|
|
150. Signs consistent with cocaine overdose include all of the following EXCEPT
A. arrhythmias
B. dysphoria
C. hyperglycaemia
D. hyperthermia
E. miosis
|
E
Best answer is Miosis. Cocaine causes maximally dilated pupils (mydriasis)
According to the Merck Manual (7th ed pg 1592) cocaine toxicity includes: hypertension, muscle twitching, tachycardia, hallucinations and paranoid delusions, maximally dilated pupils.
Cocaine has a strong sympathomimetic effect which can cause an increase in blood glucose.
Any increase in basal metabolic rate (such as that caused by cocaine) can increase body temperature
|
|
|
149. A 20 kilogram child suffered 15% full thickness burns 6 hours ago. Optimum crystalloid fluid volume resuscitation for the first hour is
A. 160 ml
B. 260 ml
C. 360 ml
D. 460 ml
E. 660 ml
|
D
Parkland - Lactated Ringer - 4 mL/kg/%TBSA burn
= 1200ml
Normally Give 0.5x1200 = 600ml over 1st 8hrs
But as 6hrs prior need to give 600ml in 2hr = 300ml
Plus need to give maintanence fluid via 4/2/1 rule = 60ml/hr
Hence total 360ml
RCH protocol suggests D however
|
|
|
148. Correct statements regarding expiratory-inspiratory flow-volume loops include all of the following EXCEPT
A. in obstructive disease the expiratory curve has a scooped
out or concave appearance
B. in restrictive disease expiratory flows are usually decreased
in relation to lung volume
C. in restrictive disease the expiratory curve has a convex
appearance
D, the expiratory curve is largely effort independent
E. the inspiratory curve is effort dependent
|
|
|
|
The formation of Compound A (a degradation product of sevoflurane) is
A. associated with significant renal dysfunction in humans
B. greater at higher fresh gas flow rates
C. lower at higher sevoflurane concentrations
D. lower at higher temperatures
E. lower when soda lime is the adsorbent compared with
baralyme
|
E
Compound A production is increased by:
• high CO2 absorber temperatures which can be caused by low flow anaesthesia
• high sevoflurane concentrations
• monovalent bases in CO2 absorber (KOH, NaOH), such as with baralyme
|
|
|
146, The LEAST useful investigation to diagnose early myocardial RE¬infarction is
A. CK-MB
B. CK-MB as a fraction of total CK
C. echocardiography
D. ECG
E. troponins
|
E
Troponin I remains elevated for 12 days.
|
|
|
145. Physiological changes with advanced age include all the following EXCEPT
A. decreased intracellular water
B. decreased total lung capacity
C. diminished baroreceptor responsiveness
D. lower maximum heart rate in response to stress
E. increased cerebrospinal fluid (CSF) volume
|
B
From Miller, M&M:
Elderly have decreased GFR, but not necessarily increased Cr due to loss of muscle mass.
FRC does not change with age.
Resting cardiac output is unchanged, but maximal CO is decreased.
Decreased LV compliance means atrial kick is important.
Stroke volume increases with age, but HR decreases.
There is decreased responsiveness to hypoxia.
There is no change in Total Lung Capacity.
|
|
|
The time to the peak analgesic effect of an intravenous bolus of morphine is approximately
A. 3 - 5 minutes
B. 5 - 10 minutes
C. 10 - 15 minutes
D. 15 - 25 minutes
E. 25 - 35 minutes
|
D
Yentis A-Z - states 15-20 mins
MIMS "peak analgesia occurring 30 to 60 minutes after intramuscular injection and 50 to 90 minutes after subcutaneous injection. Peak analgesia occurs within 20 minutes following intravenous administration"
|
|
|
143, During elective caesarean section under spinal anaesthesia
A. maternal hypotension requiring intervention is infrequent
B. the duration that the maternal systolic blood pressure is below 100 mmHg is of less importance for producing adverse cord blood acid-base measures than the degree of fall in systolic blood pressure
C. there is a significant difference between the use of rescue boluses compared to infused prophylactic ephedrine on the status of cord blood acid-base measures
D. there is less nausea and vomiting if ephedrine is prophylactically infused compared to using it as a rescue bolus to treat any maternal hypotension when it does occur
E. there is no adverse effect from maternal hypotension on cord blood acid-base values
|
D
Anaesth Intensive Care. 2002 Jun;30(3):316-20.: Effectiveness of intravenous ephedrine infusion during spinal anaesthesia for caesarean section based on maternal hypotension, neonatal acid-base status and lactate levels:
Conclusion: Ephedrine infusion prevented maternal hypotension, reduced the incidence of nausea and vomiting and led to improved umbilical blood pH during spinal anaesthesia for caesarean section
|
|
|
. Normal features of changing physiology with age include
A. increased lean body mass
B. increased basal catecholamine levels
C. earlier onset of shivering
D. increased plasma albumin
E. decreased gastric pH
|
B
http://www.asahq.org/clinical/geriatrics/PDFSyllabus5-011002.pdf
Instead, ischemia is likely due to hypertension and increased plasma concentrations of norepinephrine
|
|
|
141. Which drug is contra-indicated in a patient with chronic renal failure presenting with a fractured femur?
A. fentanyl
B. morphine
C. paracetamol
D. pethidine
E. oxycodone
|
D
Decreased elimination of nor-pethidine
|
|
|
, The normal haemoglobin (g.d1-1) for age during infancy is
A. 16 at 3 months
B. 12 at 3 months
C. 10 at 3 months
D. 8 at 3 months
E. 9 at 12 months
|
C
Stoelting edition 5 p 583 "By 2 to 3 months physiological anaemia results. After 3 months, there are progressive increases in rbc mass and Hct." Table 24.3 says at 2 months Hb is 10.7g/dL
|
|
|
139. With respect to intra-arterial cannulation and monitoring
A. following cardiopulmonary bypass, a cannula in the brachial artery will tend to give a more accurate blood pressure reading than in the radial artery
B. radial artery cannulation is not contra-indicated in Raynaud's Disease
C. the Allen's test is a reliable predictor of the adequacy of collateral flow
D. the axillary artery is not suitable for use in cardiac surgery
E. the infective rate of all cannulation sites is approximately
5%
|
A
J Cardiothorac Anesth. 1989 Feb;3(1):20-6.
A comparison of radial, brachial, and aortic pressures after cardiopulmonary bypass.
“Two minutes after separation from CPB, clinically important (greater than or equal to 10 mmHg) underestimation of systolic aortic pressures occurred in 17 of 33 (52%) radial artery catheters, while occurring in seven of 33 (21%) brachial artery catheters.”
|
|
|
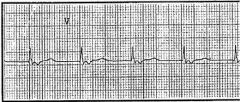
138. This ECG (Lead V5) most likely represents
A. Wolff-Parkinson-White (WPW) syndrome
B. atrial fibrillation
C. complete heart block
D. atrio-ventricular junctional rhythm
E. sinoatrial block
|
D
No P wave before QRS, regular, rate 75, retrograde P wave each QRS
|
|
|
137. Correct statements regarding medical laser hazards include all of the following EXCEPT
A. carbon dioxide lasers can cause corneal opacification
B. carbon dioxide laser energy is readily absorbed by most tissues
C. in general, the shorter wavelength lasers are more strongly absorbed by tissues and the longer wavelength lasers are more scattered
D. Nd:YAG (neodymium:yttriun-i-aluminium-garnet) lasers can injure the retina
E. the effect that a particular laser beam has on tissue depends on its wavelength and power density
|
C
• A : True. CO2 beam is TOTALLY invisible. 10.6 um wavelength can't reach the back of the eye and the retina, the eye can still be permanently damaged since the transparent tissues like the cornea and lens are sensitive to increases in local temperature - and have limited ability to sense there is a problem until it is too late. Carbon dioxide lasers can cause corneal opacification (Zuclich et al, Corneal damage induced by pulsed CO2 laser radiation. Health Phys. 1984 Dec;47(6):829-35.)
• B : True. CO2 laser causes rapid vapourisation of water which is the main constituent of most cells (molecules with two different atoms absorb infrared). VISIBLE LIGHT LASERS are transmitted by the cornea/lens and absorbed by the retina. (Oxford Handbook Anaesthesia, pg 677)
• C : False. Opposite short waves lengths scattered, long wavelengths absorbed
• D : Correct
• E : True. Effect of a laser on tissue depends on its wavelength & power density (Oxford handbook Anaesthesia, pg 675).
CO2 laser: far infrared, long wavelength, transmitted by mirrors.
Nd:YAG laser: near infrared, transmitted by optical fibre.
Argon: blue green, shorter wavelength. Significant non selective heating (useful in retina for scar formation). Not absorbed by vitreous, lens or cornea but is absorbed by Haemoglobin/pigmented tissue.
Invisible lasers (UV or IR) are absorbed readily
Visible, particularly RED penetrate most deeply.
|
|
|
135. A healthy 20 year old patient undergoing nasal surgery under general anaesthesia has the nose packed with gauze soaked in 0.5% phenylephrine and is given a submucosal injection of lignocaine with 1:100,000 adrenaline. Over the next 10 minutes the blood pressure rises from 130/80 to 220/120 mmHg and the heart rate from 60 to 100 beats per minute. The LEAST appropriate management of this situation would be to
A. administer glyceryl trinitrate
B. administer esmolol
C. administer labetalol
D. administer sodium nitroprusside
E. deepen anaesthesia with isoflurane
|
C
C better than B only because of shorter action. Though would its alpha blocking effects back this more appropriate?
Anesthesiology March 2000 - Volume 92 - Issue 3 - pp 859-864:
‘Nine case records (including the index case) dating from 1990 were found in which significant morbidity or mortality was reported after the use of a vasoconstrictor during ENT surgery. A similar death occurred a few months before the index case during an endoscopic sinus surgery and a nasal septoplasty procedure. A 26-yr-old male patient had his nose packed with cotton balls soaked in 15 ml of 0.5% phenylephrine. Lidocaine 1% with 1:100,000 epinephrine was also injected submucosally into the nose. The patient's BP increased to 220/120 mmHg, which was treated by increasing the concentration of isoflurane and administering 20 mg of labetalol. His BP decreased in response to this treatment, but bradycardia, pulmonary edema, cardiac arrest, and ultimately death also followed.’
‘6. The use of β blockers and calcium-channel blockers should be avoided when vasoconstrictive agents such as phenylephrine are used in the operating room. Case reviews, as well as a review of the medical literature, suggest that the use of β blockers, and potentially calcium-channel blockers, as treatment of hypertension secondary to a vasoconstrictor may worsen cardiac output and result in pulmonary edema.’
|
|
|
The American Heart Association guidelines for pre-operative cardiac risk assessment define poor functional capacity as being only able to exercise at a level of less than 4 METS (metabolic equivalents). An exercise capacity of 4 METS would correspond to
A. light housework such as dishwashing
B. heavy work around the house such as moving heavy objects
C. jogging for 2 kilometers
D. walking briskly on level ground (6 kilometers per hour)
E. walking slowly on level ground (3 kilometers per hour)
|
A
• A – True. At 4 MET point – see table below.
• B – False. > 4 METS.
• C – False. > 4 METS.
• D – False. > 4 METS.
• E – False. < 4 METS.
|
|
|
133. The MOST correct statement concerning lignocaine toxicity is that
A. extremely high concentrations of lignocaine will produce persistent ventricular fibrillation
B. hypercarbia increases the convulsive threshold of the drug
C. the first sign of lignocaine toxicity is cardiovascular collapse
D. the initial treatment of lignocaine induced convulsions is phenytoin
E. tonic-clonic convulsions may be preceded by symptoms such as auditory disturbances
|
E
A - False. Miller, 6th ed. p 594: "Ventricular arrhythmias were rarely seen with lidocaine, mepivacaine, or tetracaine." and "Ventricular arrhythmias and fatal ventricular fibrillation may occur more often after rapid intravenous administration of a large dose of bupivacaine but far less frequently with lidocaine."
B - False. "Hypercarbia can lower seizure threshold by several mechanisms: (1) Increased CBF with increased drug delivery to the CNS; (2) increased conversion of the drug base to the active cation in the presence of decreased intracellular pH; and (3) decreased plasma protein binding, which increases the amount of free drug available for diffusion into the brain." Goldfrank's toxicologic emergencies
C - False. "Initial symptoms are subjective and include tinnitus, lightheadedness, circumoral numbness, disorientation, confusion, auditory- and visual disturbances and lethargy." Goldfrank's toxicologic emergencies
D - False. "Treatment: supportive, with oxygenation / cardiovascular support as for CPR. Thiopental or diazepam / midazolam may be used for convulsions, although hypotension may be exacerbated." Yentis, 3rd ed., p 321.
E - True. Sequence of: "Toxicity . . . tingling . . . unconsciousness and or convulsions." Yentis, 3rd ed., p 321 and above.
|
|
|
132. The values of static vacuum and minimum gas flow recommended for satisfactory anaesthetic and surgical suction are
A. 40 Kpa and 401.min-1
B, 40 Kpa and 601.min-1
C. 50 Kpa and 301.min-1
D. 60 Kpa and 401.min-1
E. 60 Kpa and 501.min-1
|
D
Aust NZ J Surg, 1991, Sept 61(9) 687-91:
The Australian Standards guidelines state that minimum operating theatre suction should provide a flow-rate (minimum 40 L/min) and occluded negative pressure (ONP; minimum -60 kPa) and that -40 kPa achieved in less than 4 s.
|
|
|
131. A woman has an epidural placed for forceps delivery after a prolonged second stage of labour. The next day she has a right foot drop, and numbness over the anterior part of her lower leg and the dorsal surface of her right foot. The most likely cause is a
A. L4 nerve root lesion from trauma during epidural placement
B. L5 nerve root lesion from trauma during epidural placement
C. L5 nerve root lesion from an acute disc protrusion
D. right common peroneal nerve lesion from compression by lithotomy stirrups
E. right lumbar plexus lesion from compression by the fetal head
|
E
CEACCP. Brooks H, May A. 3 (4): 111. (2003). Neurological complications following regional anaesthesia in obstetrics:
“Postpartum foot drop is caused by damage to the lumbosacral nerve trunk or, less frequently, the common peroneal nerve. The lumbosacral trunk (L4 and L5) is compressed between the ala of the sacrum and the descending fetal head. It may also occur during a forceps delivery.”
|
|
|
. Clinical features of autonomic neuropathy include all of the following EXCEPT
A. increased risk of gastro-oesophageal reflux
B. postural hypotension
C. pronounced sinus arrhythmia
D. resting tachycardia
E. silent myocardial ischaemia
|
C
There is lack of HR variability but ot sinus arrhythmia
Morgan and Mikhail has a good table on autonomic neuropathy symptoms/signs on pg 739 (3rd ed) (page 805 of the 4th Ed) which includes:
• Hypertension
• Painless MI
• Orthostatic hypotension
• Lack of heart rate variability with breathing (normal heart rate variability during voluntary deep breathing is > 10 beats/min)
• Resting tachycardia
• Early satiety (due to delayed gastric emptying
• neurogenic bladder
• lack of sweating
• impotence
|
|
|
129. During elective major vascular surgery the best way to reduce the risk of acute renal failure is to maintain a normal
A. central venous pressure
B. mean arterial blood pressure
C. renal blood flow
D. systemic vascular resistance
E. urine output
|
C
Almost repeat
Main cause of renal failure post-vascular surgery will be an ischaemic (i.e. pre-renal cause)
MAP and RBF both seem kind of right – but RBF is surely more correct
The question was repeated the following year but with only CO, MAP and RBF present as same options.
|
|
|
128. Heparin Induced Thrombocytopenia (HITS)
A. is associated with antibodies to complexes of Antithrombin 3 (ATM) and heparin
B. is associated with a more rapid drop in platelet count if the patient has been exposed to heparin within the last three months
C. is not associated with the use of low molecular weight heparins
D. results in the maintenance of heparin-dependent antibody levels indefinitely after their development
E. results in thrombotic complications in most patients
|
B
o A – antibodies to heparin-PF4 immune complexes
o B – true. Rapid onset due to development of pre-existing antibodies in patient previously exposed to heparin
o C – false. Is associated, just lower incidence
o D – false. BJA 90 (5): 676. 2003
"During recovery from thrombocytopenia, heparin dependent antibodies in the serum decrease to undetectable levels by 50±85 days.78 Those with undetectable antibody but a previous proven diagnosis of HIT type II may take as long as 5 days to produce IgG antibodies and thrombocytopenia."
o E – partly true. Rates vary widely between 38-76% according to Levy in AA 2007
Stoelting: "Less than 10% of those who develop an antibody to the heparin–heparin-platelet factor 4 complex will exhibit a thrombotic event. However, the risk varies considerably with the clinical situation and can reach 40% or more in the postoperative setting when high circulating levels of both activated platelets and thrombin are present, for example, following orthopedic surgery."
|
|
|
127. Milrinone
A. prolongs conduction in Purkinje fibres
B. is contraindicated with ACE (angiotensin converting enzyme)
inhibitors
C. inhibits a phosphodiesterase iso-enzyme
D. causes nodal tachycardia
E. increases systemic and pulmonary vascular resistance
|
C
A. False. In canine fibres it sped conduction (Circulation, Vol 69, 1026-1035) not shown to induce nodal tachycardia or ventricular arrhythmia http://www.ncbi.nlm.nih.gov/pubmed/3571104
B. False. "No untoward clinical manifestations have been observed in patients in whom Primacor Injection was used concurrently with the following drugs...captopril"
C. True. Inhibits phosphodiesterase III isoenzyme.
D. True (probably not best answer). "Supraventricular arrhythmias were reported in 3.8% of the patients receiving Primacor Injection" - MIMS
E. False. Reduces pulmonary and systemic vascular resistance. (inodilator, venodilator, vasodilator)
|
|
|
126. Transient neurological syndrome (TNS) associated with subarachnoid anaesthesia
A. can be prevented by the concurrent use of a subarachnoid
opioid
B. does not occur with bupivacaine
C. is more common if a leg tourniquet is used
D. is seen with similar frequency with 2% and 5% lignocaine
E. is usually apparent within 6 to 12 hours of the procedure
|
D
A – false
B –False – mainly Lig, but has occurred with Bup
C – False – no relation
D – True
CEACCP – Spinal Anaesthesia: an update
“TNS should not be confused with the neurotoxic cauda equina syndrome seen after the administration of 5% hyperbaric lidocaine through microcatheters. Initially TNS were described after the administration of hyperbaric 5% lidocaine, but subsequent studies have suggested an equally high incidence with lower concentrations of plain lidocaine. These symptoms have also been associated with mepivacaine, but are rare with prilocaine and bupivacaine.”
E – False – 12-24hrs
|
|
|
125. In beta-thalassaemia major
A. blood transfusion prevents growth retardation in children
B. the red blood cells are hypochromic and macrocytic
C. the average age at death is 25-30 years
D. liver failure is the most common cause of death
E. iron supplementation improves peri-operative haemoglobin
levels
|
A
• A – true. Mollison’s Blood Transfusion in Clinical Medicine p 390
• B – false. should be hypochromic and microcytic
• C – true. Someone on wike says this is about right, but can live to >40 also quoted
• D – false. commonest cause of death is heart failure
• E – false. these patients suffer from iron overload
Stoelting:
Thalassemia major patients develop severe, life-threatening anemia during their first few years of life. To survive childhood, they require long-term transfusion therapy to correct their anemia and suppress their high level of ineffective erythropoiesis. Otherwise, they either die during childhood or have marked changes due to their disease and the complications of therapy.
The severity of thalassemia is remarkably variable, even among patients with seemingly identical genetic mutations. In its most severe forms, patients exhibit three defects that markedly depress their oxygen-carrying capacity: (1) ineffective erythropoiesis, (2) hemolytic anemia, and (3) hypochromia with microcytosis. The deficit in oxygen-carrying capacity produces maximum erythropoietin release, and marrow erythroblasts respond by increasing their unbalanced globin synthesis.
The accumulating unpaired globins aggregate and precipitate, forming inclusion bodies that cause membrane damage to the RBCs. Some of these defective RBCs are destroyed within the marrow, resulting in ineffective erythropoiesis. Some abnormal erythrocytes escape into the circulation, where their altered morphology can cause accelerated clearance (hemolytic anemia) or, at best, reduced capacity to transport oxygen due to their lowered Hb content (hypochromia with microcytosis).
Other features of severe thalassemia include those attributable to massive marrow hyperplasia (frontal bossing, maxillary overgrowth, stunted growth, osteoporosis), and extramedullary hematopoiesis (hepatomegaly). Hemolytic anemia may produce splenomegaly together with extreme dyspnea and orthopnea, over time resulting in congestive heart failure and mental retardation. Transfusion therapy will ameliorate many of these changes, but complications due to iron overload such as cirrhosis, right-sided heart failure, and endocrinopathy frequently require chelation therapy. Some patients demonstrate reduced transfusion requirements after splenectomy, and laparoscopic splenectomy has dramatically shortened recovery times. However, the greater risk of postsplenectomy sepsis in younger patients argues for deferment of surgery until after 5 years of age whenever possible, and for well-transfused and well-chelated patients, splenectomy may not be indicated. Bone marrow transplantation was first performed for thalassemia major in 1982 and is a therapeutic option for younger patients with HLA-identical siblings.
|
|
|
124. The peak effect of oral midazolam as a premedication in children occurs after
A. 10 - 15 minutes
B. 20 - 30 minutes
C. 35 - 45 minutes
D. 50 - 60 minutes
E. 65 - 75 minutes
|
B
"The dose of oral midazolam... usually results in a satisfactorily sedated child in approximately 10-15 min with a peak effect occurring at approximately 20-30 min, with minimal to no delay in recovery, even for brief procedures." (Cote, Preoperative preparation and premedication, BJA 1999, 83:16-28)
|
|
|
123. Pre-ganglionic sympathetic fibres pass to the
A. otic ganglion
B. carotid body
C. ciliary ganglion
D. coeliac ganglion
E. all of the above
|
D
Coeliac Plexus is the largest sympathetic plexus. It recieves pre-ganglionic fibers from the spinal segments, some of which pass through the plexus without synapsing and end in the adrenal medulla. The rest synapse within the plexus, Therefore Post ganglionic fibers originate within the plexus
|
|
|
122. The oxygen saturation of fetal haemoglobin in the fetal umbilical vein is
A. 50%
B. 60%
C. 70%
D. 80%
E. 90%
|
D
KB physiology viva says 70%
Power and Kam (p356) and Ganong both say 80%. As does Berne and Levy 8th ed P. 266. And Yentis A-Z Fig. 63 p206
|
|
|
121, The earliest sign in the development of malignant hyperthermia is
A. acidosis
B. hyperthermia
C. increased end-tidal carbon dioxide concentration
D. muscle rigidity
E. myoglobinuria
|
C
Answer C – Though note that below seems to suggest acidosis is also early, but hypercapnia probably is contributing to acisosis
British Journal of Anaesthesia. 85(1):118-28, 2000 Jul.
|
|
|
120. During a transoesophageal echocardiography (TOE) examination the end-diastolic area is found to be 15 cm2 and the end-systolic area 10 cm2. Based on these measurements one could calculate this patient's
A. area ejection fraction to be 33%
B. area ejection fraction to be 67%
C, ejection fraction to be 50%
D. ejection fraction to be 67%
E. fractional area change to be 50%
|
A
Area ejection fraction
= End diastolic area – end systolic area/ end diastolic area x 100%
= 5/15 x 100%
= 33%
|
|
|
119. Negative pressure pulmonary oedema
A. is typically seen in a patient following the relief of bronchospasm
B. is usually associated with cardiac pathology
C. should be investigated with echocardiography
D. typically requires endotracheal intubation
E. usually presents suddenly
|
|
|
|
118. The medical therapy for unstable angina which is most effective in reducing progression to myocardial infarction is
A. aspirin
B. beta-blockers
C. calcium channel blockers
D. glycerol trinitrate
E. thrombolytic therapy
|
A
AHA ACC Guidelines
This collaborative meta-analysis pooled data from 195 trials involving more than 143,000 patients and demonstrated a 22% reduction in the odds of vascular death, MI, or stroke with antiplatelet therapy across a broad spectrum of clinical presentations that included patients presenting with UA/NSTEMI
|
|
|
117. The estimated risk of infection following percutaneous exposure
(needlestick injury) to human immunodeficiency virus (HIV) is approximately
A. 1 in 30
B. 1 in 300
C. 1 in 3,000
D. 1 in 30,000
E. 1 in 300,000
|
|
|
|
116, The correct ranking of muscle:blood partition co-efficients, in order of increasing solubility in muscle, for sevoflurane (S), desflurane (D) and nitrous oxide (N20) is
A. N20 < D < S
B. D < N20 < S
C. D< S < N20
D. N20 < S < D
E. S < D < N20
|
A
Solubility in blood: H>I>S>N~>D
Solubility in fat: H>S~>I>D>N
Solubility in muscle: I>H>S>D>N
|
|
|
115. In an infant suffering from persistent vomiting
A. a plain X-ray of the abdomen is NOT likely to provide diagnostic help
B. duodenal atresia is less likely if the child has Down's syndrome
C. pyloric stenosis often presents with a hypokalaemic, hypochloraemic, metabolic acidosis
D. surgery is urgent to prevent dehydration
E. the presence of bile in the vomitus favours the diagnosis of pyloric stenosis
|
A
All seem false – perhaps A is most correct
A. could still be helpful - Plain radiographs that demonstrate a double-bubble appearance with no distal gas are characteristic of duodenal atresia. Distal bowel gas indicates stenosis, incomplete membrane, or a hepatopancreatic ductal anomaly.'
B. false -'Duodenal atresia or duodenal stenosis is most commonly associated with trisomy 21. About 22-30% of patients with duodenal obstruction have trisomy 21’ emedicine
C. false - hypokalaemic hypocholaraemic metabolic alkalosis
D. false – should receive fluid resuscitation
E. false - 'Bile-stained vomit in neonates aged 24 hours or younger is the typical presentation of atresia or severe stenosis.'
|
|
|
114. Spinal anaesthesia in infants
A. eliminates the risk of postoperative apnoea
B. has a lower failure rate than in adults
C. lasts for a shorter time than in adults
D. may be performed at a higher spinal level than in adults
E. often causes hypotension if the infant is awake
|
C
• Failure rate of 20% - higher than adults
• Proven to reduce risk of apneas – but not eliminate
• Shorter Duration - 20-60 minutes
• Spinal cord terminates more lower (L3), not higher
|
|
|
112. When intravenous magnesium sulphate is administered in the management of severe pre-eclampsia, deep tendon reflexes are lost at a serum Mg2* level of
A. 2 mmo1.1-1
B. 3.5 mmo1.1-1
C. 5 mmo1.1-1
D. 8 mmo1.1-I
E. 12 mmo1,1-1
|
C
The classic teaching is that deep tendon reflexes are LOST when [Mg+2] EXCEEDS 5 mmol/l (ie 10 mEg/l).
For a local reference, see the RWH Protocol which says LOSS of DTR occurs at >5 mmol/l.
Mg conc (mmol/L)
0.8 - 1.0 normal plasma level
1.7 - 3.5 therapeutic range
2.5 - 5.0 ECG changes (P-Q interval prolongation, widen QRS complex)
4.0 - 5.0 reduction in deep tendon reflexes
> 5.0 loss of deep tendon reflexes
7.5 sinoatrial and atrioventricular blockade. Respiratory paralysis and CNS depression
> 12 cardiac arrest
|
|
|
111. Lowering intra-ocular pressure by applying pressure to the globe (e.g. Honan balloon) is typically contraindicated in a patient having
A. a revision corneal graft
B. a revision trabeculectomy
C. an extra-capsular lens extraction
D. a redo vitrectomy
E. repeat retinal cryotherapy
|
B
(Current Opinion in Ophthalmology Issue: Volume 16(2), April 2005, pp 107-113)
"When using peribulbar and retrobulbar injections in patients with advanced glaucoma, reduced anesthetic volumes and avoiding the use of orbital Honan balloons is advisable because these can increase intraocular pressure."
Trabeculectomy is a treatment for glaucoma
|
|
|
110. Low molecular weight heparins
A. are cleared principally by the liver
B. are ineffective if only administered post-operatively
C. cross the placenta
D. have a dose-dependent half-life
E. have a longer half-life than standard (unfractionated) heparin
|
E
LMWH’s
Higher bioavailability
Bioavailability is greater. Protein binding is much less compared to unfractionated heparin, giving superior bioavailability at lower doses.
Not fully reversible with protamine unlike unfractionated heparin
Less HITS and less platelet function affect
Longer T 1/2 and more predictable kinetics
clearance by first order kinetics, through the renal route
|
|
|
109. The most effective method of deep venous thrombosis (DVT)
prophylaxis for a fifty-year-old woman presenting for anterior resection for cancer of the colon would be
A. electrical calf stimulation
B. Dextran 70 infusion
C. graduated compression stockings
D. intermittent pneumatic leg compression
E. low dose heparin (5000 units bd)
|
E
Wille-Jørgensen P, Rasmussen MS, Andersen BR, Borly L. Heparins and mechanical methods for thromboprophylaxis in colorectal surgery. Cochrane Database of Systematic Reviews 2004
Results :
• Any kind of heparin is better than no treatment or placebo (11 studies).
• Unfractionated heparin and low molecular weight heparin (4 studies) were equally effective.
• The combination of graduated compression stockings and LMWH is better than LMWH alone
Emedicine.com – perioperative DVT prophylaxis:
Heparin
Overall, heparin and LMWH are equivalent in preventing DVT, although LMWH has greater bioavailability, longer duration of anticoagulant effect in fixed doses, and little requirement for laboratory monitoring (thus is more cost-effective).
Warfarin:
Effective but cumbersome DVT prophylaxis regimen, and it is reserved for very high-risk patients who are undergoing general surgery (if the international normalized ratio [INR] is kept at 2-3). Direct comparison between warfarin (Coumadin) and other antithrombotic agents has yielded mixed results; however, warfarin is certainly more effective than aspirin or external pneumatic compression
Antiplatelet agents
Considered ineffective in preventing PE even though some recent data have suggested that antiplatelet therapy may reduce the incidence of postoperative DVT.
Dextran
Although earlier studies suggest comparable efficacy of dextran in PE prevention, with bleeding risks equivalent to those of heparin, dextran is generally considered less effective than heparin in preventing DVT; furthermore, it can lead to anaphylactoid reactions in 0.1-0.25% of patients.
Nonpharmacologic measures
Recommended for low-risk patients throughout the perioperative period until they are ambulatory. These measures are especially useful when heparin therapy is contraindicated.
|
|
|
108, In a group of subjects, the proportion vomiting is 80%. With treatment, this can be reduced to 60%. The number needed to treat (NNT) with this treatment is
A. 3
B. 4
C. 5
D. 6
E. 7
|
C
NNT = 1/absolute risk reduction
(absolute risk reduction = usual incidence - incidence post exposure)
|
|
|
107. Correct statements regarding trigeminal neuralgia include
A. Associated sensory loss is common.
B. It most frequently occurs in the second or third division of the nerve (V2 or V3).
C. Oedema of the trigeminal ganglion is usually seen on a cranial CAT scan.
D. The pain is often bilateral.
E. The pain is usually described as an intense deep ache,
|
B
Emedicine article - http://emedicine.medscape.com/article/794402-overview
A – false. usually normal examination
B – true.
C – false.
D – false. unilateral
E – false. nature of pain – brief and paroxysmal, character of which is stabbing or shocklike and typically severe
|
|
|
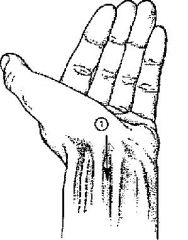
106. Blockade at the wrist of the nerve marked '1 in the figure usually results in
A. anaesthesia of the entire thumb
B. anaesthesia of the palmar aspect of the hypothenar eminence
C. anaesthesia of the palmar aspect of the radial 3 digits
D. paralysis of adductor pollicis
E. paralysis of the medial lumbrical muscles
|
Median nerve is depicted in the diagram.
Sensory loss;
radial 3 1/2 fingers, palmar surfaces, and finger tips.
Motor loss;
Pointing finger position (index finger out straight and all other fingers flexed); Weak thumb abduction (abductor pollis brevis)
FOUR muscles of the hand are supplied by the median nerve. The remainder are supplied by the Ulnar nerve.
The mnemonic LOAF is a handy reminder.
L - Lateral two lumbricals
O - Opponens pollicis
A - Abductor pollicis brevis
F - Flexor pollicis brevis
|
|
|
105. Features of paracetamol administration in children include
A. limitation of the daily dose to a maximum of 150 mg,kg-1 because of the risk of hepatotoxicity
B. reliable absorption when administered rectally with most patients achieving a therapeutic concentration with a loading dose of 20 mg,kg-1
C. peak blood levels being reached approximately 1 hour following rectal administration
D. a one hour delay between peak plasma concentration and maximum analgesia
E. a faster absoprtion of high dose rectal paracetamol compared to oral administration
|
D
• A - False. "Analgesia in children may require 90 mg/kg/day in divided doses." Sasada & Smith, 3rd ed. p. 294.
• B - False. "Rectal absorption of paracetamol is slower and less predictable, with bioavailability between 24% and 98%." Peri-operative use of paracetamol, Oscier C. Anaesthesia, 2009, 64, pages 65–72.
• C - False. "Maximal analgesic and antipyretic activity occurs 1–2 h after peak plasma levels, and the time to achieve this varies with the route of administration. Peak plasma concentration (Cmax) is achieved approximately 45 min after 1 g orally, at between 3.5 and 4.5 h after rectal administration of both 20 and 40 mg/kg, and approximately 25 min after a 1 g intravenous infusion." Peri-operative use of paracetamol, Oscier C. Anaesthesia, 2009, 64, pages 65–72.
• D - True. See quote at C.
• E - False. See quote at C.
|
|
|
104. A history of glucose-6-phosphate dehydrogenase deficiency in an
adult patient is most likely to be of relevance for anaesthesia because of
A. altered metabolism of some inhalational agents
B. increased potential for haemolysis resulting from prilocaine administration
C. increased sensitivity of blood cells to hypoxia
D. increased sensitivity to thiopentone (due to sulphur component)
E. the potential to develop jaundice
|
B
• Miller: Glucose-6-Phosphate Dehydrogenase Deficiency
o Glucose-6-phosphate dehydrogenase deficiency is an X-linked hereditary Coombs-positive hemolytic anemia. Hemolysis occurs with exposure to drugs (antipyretics, nitrates, sulfonamides), infections, hypoxia, hypothermia, blood products, or stress. The severity of the hemolysis varies among patients and the offending agent or condition. Steroids are usually effective. The preoperative history focuses on previous episodes of hemolysis, identification of predisposing factors, and determination of the current hematocrit.
• “Reduction of methaemoglobin is impaired hence avoidance of prilocaine has been suggested” p 226 Yentis
|
|
|
103, In a previously healthy multi-trauma patient, loss of 20% of blood volume would likely result in
A. minimal symptoms and signs
B. anxiety, tachycardia and decreased pulse pressure, but minimal effect on urine output
C. altered mental state, tachycardia, tachypnoea, fall in systolic blood pressure and decreased urine output
D. obtundation, marked tachycardia, markedly decreased systolic blood pressure and minimal urine output
|
B
Almost repeat
A – describes class I shock. < 15%
B – describes class II shock 15-30%
C – describes class III shock. 30-40%
D – describes class IV shock > 40%
|
|
|
102. A multi-trauma patient opens his eyes and withdraws to painful stimuli, but does not respond to voice. He is moaning but makes no comprehensible sounds. His Glasgow Coma Score is
A. 5
B. 6
C. 7
D. 8
E. 9
|
D
E2V2M4
Eyes Vocal Motor
Spontaneous Normal Conversation Obeys commands
To Voice Confused Localises to pain
To Pain Incomprehensible words Withdraws to pain
Nil Groans/sounds only Abnormal flexion
Nil Abnormal extension
Nil
|
|
|
101. A 26 year old primigravida at 39 weeks is delivering by the vertex after a protracted labour, She has received 250mg of pethidine over the previous 8 hours, The head is delivered and the neonate has thick meconium on its face and in its mouth. The most important step in the management of this neonate is
A. administration of naloxone via the umbilical vein
B. intubation of the trachea immediately on delivery
C. lavage of the trachea with sterile normal saline
D. oropharyngeal suction with a sterile catheter immediately following delivery of the head
E. oxygen by mask with intermittent positive pressure
|
B
Answer B (assuming neonate is flat) – though at the time of this question perhaps D was correct
2005 Neonatal Resuscitation Guidelines:
Clearing the Airway of Meconium
Aspiration of meconium before delivery, during birth, or during resuscitation can cause severe aspiration pneumonia. One obstetrical technique to try to decrease aspiration has been to suction meconium from the infant’s airway after delivery of the head but before delivery of the shoulders (intrapartum suctioning). Although some studies (LOE 3;4) suggested that intrapartum suctioning might be effective for decreasing the risk of aspiration syndrome, subsequent evidence from a large multicenter randomized trial (LOE 1) did not show such an effect. Therefore, current recommendations no longer advise routine intrapartum oropharyngeal and nasopharyngeal suctioning for infants born to mothers with meconium staining of amniotic fluid (Class I).
Traditional teaching (LOE 5) recommended that meconium-stained infants have endotracheal intubation immediately following birth and that suction be applied to the endotracheal tube as it is withdrawn. Randomized controlled trials (LOE 1) have shown that this practice offers no benefit if the infant is vigorous (Class I).
A vigorous infant is defined as one who has strong respiratory efforts, good muscle tone, and a heart rate >100 beats per minute (bpm). Endotracheal suctioning for infants who are not vigorous should be performed immediately after birth (Class Indeterminate).
|
|
|
100, Intra-ocular pressure may be increased by all of the following EXCEPT
A. anticholinergic drugs applied directly to the eye
B. hyperventilation
C. hypoxia
D. laryngoscopy
E. peribulbar block
|
B
A – topical anticholinergics produce mydriasis. This reduces the drainage of aqueous humor leading to increased IOP. C/I in glaucoma.
B – IOP should be reduced due to hyperventilation causing hypocarbia and in turn reducing choroidal blood flow
C – hypoxia leads to vasodilation and increased choroidal blood flow
D – laryngoscopy leads to sympathetic stimulation, raised arterial pressure, possible straining and bucking if inadequately anaesthetised leading to raised IOP
E – increased volume in orbit, hence eye will be compressed and raising IOP
|
|
|
99. In chronic obstructive pulmonary disease (COPD), the variable most closely associated with prognosis is
A. arterial carbon dioxide partial pressure (PaCO2)
B. arterial oxygen partial pressure (Pa02)
C. forced expiratory volume in one second (FEV1)
D. forced vital capacity (FVC)
E. response to bronchodilators
|
C
Australian and New Zealand COPD site:
'Spirometry is the most reproducible, standardised and objective way of measuring airflow limitation, and FEV1 is the variable most closely associated with prognosis.”
|
|
|
98. Features of Guillain-Barre Syndrome include
A. distal loss of sensation
B. extensor plantar responses
C. facial weakness
D. proximal weakness greater than distal weakness
E. pseudobulbar palsy
|
A
Though C and D seem somewhat correct
o A - True. "Sensory disturbances (e.g., paresthesias) generally precede the onset of paralysis and are most prominently in the distal extremities." Stoelting AACD
o B - False. Can occur as a rare variant. "Bickerstaff's brainstem encephalitis is an immune disorder of unknown aetiology with acute, progressive cranial nerve dysfunction, associated with cerebellar ataxia and coma... A considerable number of BBE patients have associated axonal Guillaine-Barre syndrome, indicative that the two disorders are closely related and form a continuous spectrum. Bickerstaff reported eight patients who, in addition to acute ophthalmoplegia (diplopia) and ataxia, showed drowsiness, extensor plantar responses or hemisensory loss." Guillain-Barre Overlap Syndrome.
o C - True. "Bulbar involvement most frequently manifests as bilateral facial paralysis." Stoelting AACD
o D - True. "Features of GBS include: 1. Progressive motor weakness, usually ascending from the legs (proximal more than distal)." CEACCP Vol 3 No 2 2003. GBS.
o E - False. A true bulbar palsy. "Bulbar relates to the medulla. Bulbar palsy is the result of diseases affecting the lower cranial nerves (VII - XII). A speech deficit occurs due to paralysis or weakness of the muscles of articulation which are supplied by these cranial nerves. "Example causes: Guillain-Barré syndrome. Pseudobulbar palsy results from disease of the corticobulbar tracts. Bilateral tract damage must occur for clinically evident disease as the muscles are bilaterally innervated." Bulbar and Pseudobulbar Palsy.
From Stoelting AACD:
TABLE 10C-1 -- Diagnostic Criteria for Guillain-Barré Syndrome
Features Required for Diagnosis
• Progressive bilateral weakness in legs and arms
• Areflexia
Features Strongly Supporting the Diagnosis
1. Progression of symptoms over 2–4 weeks
• Symmetry of symptoms
• Mild sensory symptoms or signs (definitive sensory level makes diagnosis doubtful)
o Cranial nerve involvement (especially bilateral facial weakness)
• Spontaneous recovery beginning 2–4 weeks after progression ceases
• Autonomic nervous system dysfunction
• Absence of fever at onset
• Increased concentrations of protein in the cerebrospinal fluid
|
|
|
97. During cardiopulmonary bypass a left ventricular vent will do all of the following EXCEPT
A. aspirate blood from the bronchial veins
B. aspirate blood from the Thebesian veins
C. aspirate blood via the right superior pulmonary vein
D. assist subendocardial flow of the cardioplegic solution
E. decrease the risk of air embolism during bypass
|
E
Miller pg. 1971:
CPB diverts blood away from both the L and R sides of the heart and lungs. However, this system alone does not effectively drain all blood that enters the heart during surgery. Systemic-to-pulmonary collaterals, systemic-to-systemic collaterals and surgical site bleeding are routes of blood return to the left side of the heart and into the surgical field that require specific drainage cannulas in the CPB pump to safely conduct CPB. Distention of the LV is an ever present risk during CPB with aortic cross-clamping. It occurs as a result of bronchpulmonary collateral flow, systemic-to-systemic pericardial collateral flow and thebesian venous return to the ventricular cavity, especially when the aorta is unclamped and there is the potential for coronary flow.
Venous return to the LV results not only in LC distention and potentially subendocardial myocardial ischaemia, but also in LV warming. Thus effective venting of the LV is an essential feature of CPB. LV can be effectively vented by cannulas placed in either the LV, LA, Right superior pulmonary vein or pulmonary artery.
|
|
|
96. Von-Willebrand's disease is
A. a common acquired defect of platelet function
B associated with an imbalance of thromboxane A2 and
pro stacyclin
C. not responsive to desmopressin (DDAVP)
D. often treated with epsilon aminocaproic acid (Amicar)
E. responsive to fresh frozen plasma
|
E
Although referred to as a single disease, von Willebrand disease (VWD) is in fact a family of bleeding disorders caused by an abnormality of the von Willebrand factor (VWF). von Willebrand disease is the most common hereditary bleeding disorder.
In recent years, desmopressin has become a mainstay of therapy for most patients with mild von Willebrand disease. At appropriate doses, DDAVP causes a 2-fold to 5-fold increase in plasma von Willebrand factor and FVIII concentrations in individuals who are healthy and patients who are responsive. Remember that in type IIB von Willebrand disease, DDAVP may cause a paradoxical drop in the platelet count and should not be used in a therapeutic setting without prior testing to see how the patient responds.
Yentis 3rd Ed pg 543 "FFP or cyro may be given prior to surgery'
|
|
|
95. In an adult with aortic stenosis the most important factor in determining the timing of aortic valve replacement is
A. a measured valve area of less than 0.8 cm2
B. a mean transvalvular gradient of greater than 50 mmHg
C. the presence of risk factors for coronary artery disease
D. the presence of significant left ventricular hypertrophy on
echocardiographic examination
E. the presence of symptoms of angina or syncope
|
E
ACC/AHA guidelines - Indications for Aortic Valve Replacement
• 1 AVR is indicated for symptomatic patients with severe AS.* (Level of Evidence: B)
• 2 AVR is indicated for patients with severe AS* undergoing coronary artery bypass graft surgery (CABG). (Level of Evidence: C)
• 3 AVR is indicated for patients with severe AS* undergoing surgery on the aorta or other heart valves. (Level of Evidence: C)
• 4 AVR is recommended for patients with severe AS* and LV systolic dysfunction (ejection fraction less than 0.50). (Level of Evidence: C)
|
|
|
94, Ehlers-Danlos Syndrome is associated with each of the following EXCEPT
A. blood vessel fragility
B. glaucoma
C. mental retardation
D. mitral valve prolapse
E. resistance to local anaesthetics
|
C
There is no cognitive impairment in Ehlers-Danlos syndrome. It is a connective tissue disorder.
A - correct = connective tissue
B - correct = secondary to venous congestion
C - wrong
D - correct = connective tissue
E - correct = Type 3 Ehlers-Danlos has resistance to LA
|
|
|
93. The commonest congenital cardiac defect is
A. coarctation of the aorta
B. patent ductus arteriosus
C. pulmonic stenosis
D. transposition of the great vessels
E. ventricular septal defect
|
E
The Incidence of Congenital Heart Disease. J Am Coll Cardiol. 2002; 39(12):1890-900:
"Isolated VSDs are by far the most common form of CHD”
|
|
|
92. Which of the following myopathies is associated with an increased risk of malignant hyperpyrexia?
A. central core disease
B. centronuclear myopathy
C. fingerprint body myopathy
D. multicore myopathy
E. nemaline myopathy
|
|
|
|
91. According to the American Heart Association Guidelines on Peri-operative Cardiac Evaluation for Non-cardiac Surgery (2002), a MAJOR predictor of increased peri-operative risk is
A. insulin dependent diabetes mellitus
B. pathological Q waves on the electrocardiograph (ECG)
C. stable angina on moderate exertion such as climbing 2 flights of stairs
D. supraventricular tachyarrhythmia with uncontrolled ventricular rate
E. uncontrolled systemic hypertension
|
|
|
|
87. Forty patients are randomly divided into two groups - one to receive induction agent A and another to receive induction agent
B. The next day they are asked to rate their anaesthetic experience on a scale of 1 (very bad) to 5 (very good), The most appropriate test to compare the anaesthetic experience of the two groups is the
A. unpaired t-test
B. Mann-Whitney test
C. Chi-square test
D. Kruskal-Wallis test
E. paired t-test
|
B
Miles & Gin:
"If there is a natural order among categories, so that there is a relative value among them... then the data can be considered ordinal data”
"The Mann-Whitney U test is the recommended test to use when comparing two groups that have data measured on an ordinal scale
|
|
|
84. A two-year-old child sustains a simple fracture of the lower end of the forearm one hour after having a full meal. The most appropriate approach is to
A. postpone surgical reduction for 12 hours and treat as an
elective case
B. allow immediate reduction using a rapid sequence
induction, cricoid pressure and intubation
C. allow immediate reduction using a regional technique
D. allow immediate reduction, after gastric emptying with a
tube followed by rapid sequence induction, cricoid pressure and intubation
E. wait 4 hours and treat as elective
|
A
Controversial
- No urgency to perform immediately
- Ideally delay 6hrs + RSI
- There should be some gastric emptying, especially if the arm is immobilized and pain controlled
|
|
|
79, Hyperventilation during neurosurgery
A. only vasoconstricts intracerebral vessels
B. protects the brain from retractor injury
C. is relatively contraindicated in severe coronary artery disease
D. can reduce cerebral blood flow by 15% of normal at its peak effect
E. may cause a "steal" phenomenon
|
C
• A - False. Generalised vasoconstriction.
• B - False. May compromise blood flow to already ischaemia areas of the brain (if compressed by the retractor
• C - True. Severe hyperventilation and alkalemia can provoke chest pain and ST-segment elevation, thereby mimicking acute myocardial infarction.
• D - False. Can be more - up to 30% (OHA p 387)
• E - False. May cause "reverse-steal" i.e. vasoconstriction diverts blood to the alrady maximally dilated ischaemic areas
|
|
|
78. Which of the following features of peri-operative ulnar nerve injury indicates a poor outcome?
A, Association with anaesthesia lasting more than 2 hours
B. Association with brachial plexus block
C. Bilateral injury
D. Onset of symptoms delayed beyond 48 hours post¬operatively
E. Presence of mixed sensory and motor deficit
|
E
• A=False
• B=False - mainly associated with GA rather than regional anaesthesia
• C=False.
• D=False - Miler 6th ed.pg. 1155 - this occurs in about 9% of cases
• E=True - Miller 6th ed. Pg. 1155 - Only 35% of patients with a mixed sensory and motor deficit recovered completely in 1 year
|
|
|
73. The anti-arrhythmic agent adenosine
A. has its actions potentiated by dipyridamole
B. has its actions potentiated by theophylline
C. is contraindicated in the presence of beta blockers
D. is contraindicated in the presence of alpha blockers
E. has the same efficacy as verapamil in terminating paroxysmal supra-ventricular tachycardia
|
A
A – True. In one study dipyridamole was shown to produce a fourfold increase in adenosine activity (MIMS)
B – False – antagonised by methylxanthines (MIMS)
C – False. Intravenous Adenocor (adenosine) has been effectively administered in the presence of other cardioactive drugs, such as digitalis, quinidine, beta-adrenergic blocking agents, calcium channel blocking agents and angiotensin converting enzyme (ACE) inhibitors, without any change in the adverse reaction profile. (MIMS) Digoxin and verapamil use may be rarely associated with ventricular fibrillation
D - False
E – Similiar - NOT the same (Ann Intern Med. 1990 Jul 15;113(2):104-10. & European Heart Journal 2004 25(15):1310-1317) – adenosine is much faster, though similiar overall efficacy
Beware carbamazepine – can ↑effect of adenosine (along with other antiarrythmics)
|
|
|
71. Regarding blood transfusion,
A. fresh blood is classified by most blood banks as blood stored for less than two weeks
B. serum sodium levels decrease with the length of storage of blood
C. a 40 micron blood filter decreases the likelihood of ARDS following massive blood transfusion
D. a saline crossmatch takes at least twenty minutes to perform
E, if type specific blood (A,B4O and Rh) is given without a
crossmatch, the chance of incompatibility is about 1 in a 1000
|
B
A - " Unrefrigerated fresh whole blood, usually defined as being less than 24 hours old” NHMRC
B - Miller's 7th Edition Table 55-4 p.1745. Serum Na at Day 0 = 169; Day 35 = 122
C - False. Microagregate filters (pore size as low as 40 to 60 microns) do not achieve substantial leukocyte reduction and the pathophysiology is complex and not due just to microaggregates
D – From wiki - "Serological crossmatching techniques have been simplified in recent years... The immediate spin crossmatch is a method involving agglutination of red cells in saline following a 2-5 minute incubation. This technique has been retained to detect ABO incompatibility”
E – Miller - "If the correct ABO and Rh blood type is given, the possibility of transfusing incompatible blood is less than 1 chance in 1000. Put in other terms, ABO-Rh typing alone results in a 99.8% chance of a compatible transfusion, the addition of an antibody screen increases the safety to 99.94%, and a crossmatch increases this to 99.95%.". But A probably more correct
|
|
|
65. Recognised features of a true anaphylactic reaction do NOT include
A. previous exposure to the drug
B. mediation by IgE antibody
C. histamine release from mast cells
D. activation of the complement system
E. intracellular influx of calcium ions
|
D
Complement activation does occur with Anaphylactoid reactions, but this is talking about anaphylactic
Exosure to drug is not always required – but the exposure has usually occurred from food/cosmetics
|
|
|
64. The sciatic nerve
A. can be readily identified during neural blockade by the production of paraesthesia on contact with a needle
B. has no sympathetic fibres
C. is formed from the dorsal branches of the anterior rami of L5 and Si to 54
D. provides motor innervation to the psoas muscle
E. provides sensory innervation from the knee joint
|
|
|
|
61. Which of the following parameters occurring during cardio-
pulmonary bypass (at 28°C) is most likely to contribute to an adverse neurological event post-operatively?
A. arterial carbon dioxide partial pressure (PaCO2) below 30 mmHg
B. arterial oxygen partial pressure (Pa02) over 400 mmHg
C. blood sugar level (BSL) over 15 mmo1.1-1
D. mean arterial blood pressure below 60 mmHg
E. pump flow less than 2.4 Lm-2.min4
|
|
|
|
59. A 46 year old brewery worker has cirrhosis of the liver with oesophageal varices and has bled from these varices on one occasion. A portacaval shunt is being considered as definitive treatment for his portal hypertension. The operation would be contraindicated if he had
A. a serum bilirubin greater than 50 micromoLlitre-1
B. a serum albumin less than 30 gram.litre-1
C. ascites
D. all of the above are true
E. none of the above are true
|
|
|
|
51, In patients with Eisenmenger's Syndrome,
A. compensation for poor oxygenation at rest is achieved by an
increase in cardiac output
B. the high pulmonary vascular resistance is usually able to be
treated with a specific vasodilator
C. an F102 of 1,0 will produce a substantial improvement in
Sa02
D. the usual clinical course includes right ventricular failure
during the 3rd or 4th decade, and subsequent death
E. venesection should be used to treat a haemoglobin greater
than 180 g.1-1 to prevent the problems of hyperviscosity
|
D
A - False.
B - False. "(high PVR is fixed, ie not treatable pharmacologically)"
C - False. "(large shunt, so high Fi02 will not make significant improvement)"
D - True. OHA, 2nd ed. p 294. "Medical treatment may prolong life into the 30's."
E - False. Stoelting, AACD. "It may be useful to perform prophylactic phlebotomy with isovolumic replacement in patients with hematocrits higher than 65%."
|
|
|
49, The preferred technique of anaesthesia for reduction of a fractured wrist in a patient with a myotonic disorder is
A. general anaesthesia with spontaneous ventilation using a
volatile agent
B. general anaesthesia with suxamethonium-induced muscle
relaxation
C. general anaesthesia with a non-depolarising relaxant
reversed by neostigmine
D. intravenous regional anaesthesia with lignocaine
E. axillary brachial plexus block with lignocaine
|
D
Anaesthesia and Myotonia—An Australian Experience. Anaesth Intensive Care 2001; 29: 34-37:
"Anaesthesia under neural or regional blockade will not protect against a myotonic response to surgical stimulation, electrocautery, or shivering. Intravenous regional anaesthesia may be the regional technique of choice due to the direct relaxant action of the local anaesthetic on muscle bundles”
|
|
|
48. A 35 year old primipara at 38 weeks gestation is admitted to hospital with abruptio placentae. The fetal heart rate is 100 beats per minute, and the cervix is unfavourable. Caesarean section is planned. The anaesthetic of choice is
A. thiopentone, succinylcholine, isoflurane and oxygen
B. spinal anaesthesia
C. thiopentone, nitrous oxide, isoflurane and oxygen
D. thiopentone, succinylcholine, nitrous oxide and oxygen
E. epidural anaesthesia
|
|
|
|
43. The dose response relationship for non-steroidal anti-inflammatory drugs is characterised by
A. a small variation in effective dose
B. an effect that increases linearly as dose increases, reaching a maximum effect
C. a minimal effective dose, and continuously increasing effect as dose increases
D. no ceiling dose with no minimal effective dose
E. a minimal effective dose and a bounded maximal effect
|
E
Katzung:
“NSAIDs have can have >50% variation in effective dose between individuals. Their effect increases exponentially to a maximum effect (when all COX blocked) and they have a minimum effective dose (blockage of sufficient COX to give effect”
|
|
|
42. The most useful tool for evaluation of the condition of a patient with an acute asthmatic attack and in assessing the response to therapy is
A. chest radiography
B. arterial blood gas measurement
C. measurement of pulsus paradoxus
D. observation of the degree of use of accessory muscles of respiration
E. measurement of peak expiratory flow or FEV1
|
|
|
|
39 Carcinoid tumours
A arise in the gastrointestinal tract in approximately 40% of cases
B. result in the carcinoid syndrome in approximately 50% of cases
C. release vasoactive agents including histamine, kallikrein and prostaglandins
D. are NOT associated with hypergylcaemia
E. do not usually result in intraoperative hypotensive episodes
|
C
A. Around 75% are gastrointestinal
B. "Carcinoid syndrome occurs in less than 10%; hepatic metastases are generally present." (Current Medical Dx and Tx)
C. "Carcinoid tumors can contain numerous GI peptides including gastrin, insulin, somatostatin, motilin, neurotensin, tachykinins (substance K, substance P, neuropeptide K), glucagon, gastrin-releasing peptide, vasoactive intestinal peptide, pancreatic peptide, other biologically active peptides (corticotropin, calcitonin, growth hormone), prostaglandins, and bioactive amines (serotonin)." (Stoelting)
D. Googel search suggests both hypo and hyperglycaemia possible
E. In manipulation of the tumour you may get carcinoid hypotnesive crises no matter where the tumour lies
|
|
|
33. When investigating a patient following severe hypotension during anaesthesia, the most specific test to determine if there was an immunological basis for the hypotension is
A. plasma histamine level
B. total IgE concentration
C. complement activation
D. mast cell tryptase
E. specific IgE levels
|
D or E
Wiki seems to suggest E is more specific, quoting specificity of allergen specific IgE = 85-94% (from hunter area pathology service NSW, http://www.haps.nsw.gov.au/research/Communique_List/Allergy_Testing_-_Specific_IgE_Reporting_Changes.aspx)
This article quotes specificity of tryptase to be 93% for peak tryptase, and 98% for serial tryptase:
Emerg Med Australas. 2004 Apr;16(2):120-4. Can serum mast cell tryptase help diagnose anaphylaxis?
|
|
|
32. In patients with phaeochromocytoma
A. paroxysmal hypertension is the most common presentation
B. initial treatment should be with beta-blockade if tachycardia is present
C. excesses of adrenaline and noradrenaline occur with equal frequency
D. urinary Vanillyl Mandelic Acid (VMA) studies may be normal
E. extra-adrenal tumours occur in 2% of patients
|
D
• A – Frequent, but probably not most common (presumably plain old HTN is most common:
o “Paroxysms of severe hypertension occur in about 50% of adults and in about 8% of children with pheochromocytoma. Other patients may be completely normotensive, may be normotensive between paroxysms, or may have stable sustained hypertension." Greenspan's Basic and Clinical Endocrinology
• B – obviously don’t want unopposed alpha blockade
• C - False, Stoelting:
o "Most pheochromocytomas secrete norepinephrine either alone or more commonly combined with a smaller amount of epinephrine in a ratio of 85:15”
• D – True, from Greenspan's Basic and Clinical Endocrinology
o "Urinary VMA determinations have an overall diagnostic sensitivity for pheochromocytoma of only about 63% and do not improve the sensitivity or specificity for the diagnosis of pheochromocytoma."
• E – False, Stoelting:
o “Twenty percent of pheochromocytomas are extra-adrenal in location”
|
|
|
28. Lower oesophageal sphincter tone is increased by
A. suxamethonium
B. pancuronium
C. metoclopramide
D. prochlorperazine
E. ergometrine
|
All True
These all increase LOS tone according to this article
The lower oesophageal sphincter and the anaesthetist, SAMJ, 70, 1986
|
|
|
23„ Oxytocin, when administered intravenously in a bolus dose of 10 units immediately postpartum
A. has a half life of approximately 30 minutes
B. commonly induces vomiting
C. commonly causes premature atrial contractions
D. often lowers blood pressure
E. causes transient bradycardia
|
D
MIMS online:
"Another pharmacological effect observed with high doses of oxytocin, particularly when administered by rapid intravenous bolus injection, is a transient direct relaxing effect on vascular smooth muscle, resulting in brief hypotension, flushing and reflex tachycardia"
|
|
|
21. Which of the following does NOT occur as a complication of diabetes mellitus in the pregnant patient?
A. increased risk of oligohydramnios
B. greater risk of fetal death in the third trimester
C. retinopathy and retinal detachment
D potentiation of hypotension when regional anaesthesia is
administered to assist delivery
E. reduced fetal oxygen delivery
|
A
Polyhydramnios with pregnancy not oligohydramnios
Complications of Diabetes mellitus for baby:
1. increased fetal malformations, persists despite better treatment of T1DM. two- to sixfold increase in major malformations. Mainly neurological (neural tube), cardiac and sacral.
2. supply demand relationship affects: maternal vasculopathy, preeclampsia, hyperglycaemia and DKA causing poor placental perfusion AND the fetus has increased metabolic needs due to hyperinsulinism and macrosomia.
3. stillbirth previously occurred in 10-30% of T1DM, usually after 36weeks, thought to be due to chronic intrauterine hypoxia.
4. fetal umbilical cord blood samples from pregnant women with type 1 diabetics have demonstrated "relative fetal erythremia and lactic acidemia."
5. macrosomic children: birth trauma, obesity when older
6. neonatal hypoglycaemia
7. respiratory distress syndrome
8. polycythaemia and jaundice
9. Ca and Mg metabolic changes
|
|
|
19, Plasma glucose concentration is approximately
A. 32% lower than blood glucose concentration
B. 14% lower than blood glucose concentration
C. the same as blood glucose concentration
D. 14% higher than blood glucose concentration
E. 32% higher than blood glucose concentration
|
D
Whole-blood values are about 10 to 15 per cent lower than those of plasma" There has to be a concentration gradient, hence plasma glucose has to be higher than blood glucose, in order to enter cells
|
|
|
18. Difficulty with tracheal intubation does not usually occur in the situation of
A. quinsy
B. Mallarnpati Class IV airway
C. acromegaly
D. bilateral fractured mandible
E. re-exploration for bleeding following carotid endarterectomy
|
D
Bilateral fracture = easier intubation
Bilateral fractures may cause mandible to fall backwards into airway and cause obstruction. Not necessarily difficult to intubate
|
|
|
16. A 68 year-old patient with chronic renal failure is scheduled to have a peritoneal dialysis catheter inserted. Her bleeding time is 11 min (N 3 to 5 min) and platelet count is 110 x 109.1-1, Preoperatively she should be
A. given 2 units fresh frozen plasma
B. given 0.3 microg.kg-1 of 1-desamino-8-d-arginine vasopressin (DDAVP) intravenously
C. given 2 units of platelets
D. cancelled and taken off salicylates for 1 week
E. accepted for surgery without any further treatment
|
E
Similar to prior questions
Presumably referring to uraemic platelet dysfunction
RACP Manual:
• “This test is largely obsolete and rarely indicated. It has been replaced in most circumstances by more reproducible and less invasive tests”
• Reference Interval - <9 minutes
• “The bleeding time should not be used as a 'screening test' for inherited or acquired bleeding disorders as it has very low sensitivity and specificity”
• “Although it may be abnormal in von Willebrand’s disease, inherited disorders of platelet function, uraemia, myeloproliferative disorders and after aspirin and NSAID use, its ability to predict surgical bleeding and/or the need for therapeutic cover in these situations is very limited”
Stoelting:
“Most patients with severe uremia have a prolonged bleeding time in excess of 30 minutes. This condition is corrected by hemodialysis. It may also relate to the patient's anemia since the bleeding time shortens with either transfusion or erythropoietin therapy. For acute bleeding episodes, DDAVP therapy can improve platelet function transiently. Infusion of conjugated estrogens (0.6 mg/kg per day) for 5 days will also shorten the bleeding time”
Leaning towards B rather than E as this has been the practice I’ve seen and doesn’t make sense to wait and see if they bleed
According to Clara: patietns with urea >20 get ddavp prior to renal biopsy or CVC
|
|
|
11. Moclobemide (Aurorix) is an antidepressant which
A. reversibly blocks mono-amine oxidase (MAO) types A and B
B. blocks MAO enzymes for 24-36 hours
C. is safe to use with pethidine
D. is safe with direct acting sympathomimetics
E. is safe with indirect acting sympathomimetics
|
D
• Moclobemide is a short acting (T 1/2=1-2 hours) RIMA (Reversible Inhibitor of MAO A)
• Directly acting sympathomimetics can be used safely in patients receiving MAOIs or moclobemide, but the dose must be titrated carefully
• Would potentiate action of indirect agents (i.e. more NA around)
|
|
|
8„ Clinical information about the likelihood of awareness during general anaesthesia CANNOT be usefully obtained using
A. somatosensory evoked spinal cord potentials
B. electroencephalogram frequency
C. lower oesophageal contractility
D. the isolated forearm technique
E. electroencephalogram latency and amplitude of evoked potentials
|
A
References for B-E on wiki
Spinal cord potentials have less correlation with anaesthesia
|
|
|
4. All of the following may be associated with ulcerative colitis EXCEPT
A. cirrhosis
B. iritis
C. psoriasis
D. arthritis
E. sclerosing cholangitis
|
A
B, D and E definitely true
A could occur by way of sclerosing cholangitis
Psoriasis is classically associated with Crohn’s. However a quick lit search suggests it is actually also associated with UC:
• J Eur Acad Dermatol Venereol. 2009 May;23(5):561-5. Epub 2009 Jan 15. Psoriasis associated with ulcerative colitis and Crohn's disease:
o “Psoriasis is associated both with Crohn's disease and ulcerative colitis. Future studies on comorbidities in patients with psoriasis should focus on ulcerative colitis”
But are the examiners looking for the classical answer and hence C?
|
![]()
![]()
![]()