![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
78 Cards in this Set
- Front
- Back
|
150, The most important pre-operative investigation in a non-anticoagulated patient with chronic atrial fibrillation undergoing direct cardioversion is
A. chest x-ray B. electrocardiograph (ECG) C. serum digoxin level D. serum potassium level E. transoesophageal echocardiography |
E
Need to exclude intra-atrial thrombus |
|
|
149. Prior to elective surgery, an increased bleeding risk is most likely to be identified by
A. a platelet count B. a prothrombin time C. a skin bleeding time D. an accurate clinical history E. an examination for bruising |
D
Updates in perioperative coagulation: physiology and management of thromboembolism and haemorrhage. BJA 93 (2): 275–87 (2004): • “The best method to determine haemorrhagic risk with surgery is an adequate history and physical examination. This important message is based on several large trials showing that patients with a definite or suspicious history of bleeding are more likely to bleed during surgery than patients with a negative history.” • “Even in the 1980s, several studies had clearly demonstrated that no coagulation test, including PT, aPTT and bleeding time, is capable of providing this information. Newer studies have substantiated these findings.” |
|
|
148. The most important potential cause of raised intra-ocular pressure during general anaesthesia for elective anterior segment surgery is
A. endotracheal intubation B. hypercapnia C. laryngoscopy D. nitrous oxide E. suxamethonium |
A
Hypercapnia definitely does raise IOP, however there is this quote from Miller: "Laryngoscopy and endotracheal intubation are the anesthesia-related practices most likely to increase IOP significantly (i.e., at least 10 to 20 mm Hg). The mechanism is not clear but is probably related to sympathetic cardiovascular responses to tracheal intubation." So both A, B & C all seem correct. Wiki is split between A and B |
|
|
147. The partial pressure of oxygen in the blood of the fetal umbilical vein is
A. 27 mmHg B. 33 mmHg C. 40 mmHg D. 45 mmHg E. 70 mmHg |
A
pH PO2 PCO2 SaO2 Umbilical artery 7.21 18 55 45% Umbilical vein 7.32 28 40 70% |
|
|
145. The first drug to be used in the management of an intra-operative thyrotoxic crisis is
A. esmolol B. hydrocortisone C. magnesium D. potassium iodide E. propyl thiouracil |
A
Probably esmolol to control tachycardia/arrhythmia. After this the specific treatments are: Propylthiouracil 200-300mg TDS to prevent conversion of T4 to T3 1 hour after PTU give oral/NG iodide (Lugol's solution 0.5 mL PO TDS) – blocks hormone synthesis Hydrocortisone 200mg QID – high dose steroids inhibit conversion of T4 to T3 |
|
|
144. The most commonly reported cause of awareness during general anaesthesia for a non-obstetric procedure is
A. equipment failure B. faulty anaesthetic technique C. lack of premedication D. recreational drug use E. the use of total intravenous anaesthesia |
B
Similar to previous question CEACCP 2005: “Awareness is frequently associated with poor anaesthetic technique” |
|
|
143. Following trauma, aortic arch injury should be suspected in the presence of a
A. cervical spine injury B. fractured left first rib C. left-sided pneumothorax D. splenic rupture E. thoracic spine injury |
B
EMST/ATLS Manual: Signs of Aortic Dissection on CXR - Widened mediastinum - Obliteration of the aortic knob - Deviation of the trachea to the right - Depression of the left main bronchus - Deviation of the oesophagus (NG tube) to the right - Widened paratracheal stripe - Widened paraspinal interfaces - Presence of apical/pleural cap - Left haemothorax - Fractures of first/second rib or scapula |
|
|
142. A patient presents with headache, morning vomiting and double vision for three weeks. On examination nystagmus is present when the eyes are turned to either side. The most likely diagnosis is
A. acoustic neuroma B. craniopharyngioma C. frontal glioma D pituitary adenoma E. posterior fossa tumour |
E
Symptoms and their association: early morning vomiting = raised ICP double and blurred vision, nystagmus = infratentorial lesion (I,e, posterior fossa) problems with equilibrium, gait, and coordination = infratentorial lesion focal problems (eg motor or sensory deficit, speech change, seizures) = supratentorial lesion strong hand preference = supratentorial lesion neuroendocrine problems (DI, hypothyroidism) = suprasellar lesion change in visual acuity, visual field defect, Marcus Gunn pupil (afferent papillary defect), nystagmus = visual pathway lesion long nerve tract motor and/or sensory deficits, bowel and bladder deficits, and back or radicular pain = spinal cord lesion |
|
|
141. The first priority in managing a witnessed ventricular fibrillation cardiac arrest is
A. defibrillation times 3 B. endotracheal intubation C. establishment of intravenous access D. external cardiac massage E. mask ventilation with 100% oxygen |
D
Commence CPR until defibrillation can be performed |
|
|
140. The herbal medicine most likely to be associated with cardiovascular instability in the peri-operative period is
A. echinacea purpurea (echinacea) B. ephedra sinica (ma-huang) C. ginkgo biloba (ginkgo) D. hypericum perforatum (St, John's Wort) E. tanacetum parthenium (feverfew) |
B
A: the hepatotoxicity is the only thing, no major periop concerns. B: cardiovascular instability: hypertension, angina acutely and catechol depletion chronically. C: bleeding, hypoglycaemia D: P450 induction. Interaction with tramadol. Increased sensitivity to anaesthesia (along with valerian and kava). Very important is the induction of metabolism of immunosuppressants, antiretrovirals and anticonvulsants. Has caused cardiovascular collapse, but only very rarely. E: can increase bleeding |
|
|
139, Hoarseness following a total thyroidectomy may be due to damage to the
A. deep cervical plexus B. external branch of the superior laryngeal nerve C. hypoglossal nerve D. internal branch of the superior laryngeal nerve E. superficial cervical plexus |
B
The superior laryngeal nerve (SLN) has 2 divisions: internal and external. The internal branch provides sensory innervation to the larynx. It enters the larynx through the thyrohyoid membrane and therefore should not be at risk during thyroidectomy. The external branch provides motor function to the cricothyroid muscle and is at risk during thyroidectomy. This muscle is involved with elongation of the vocal folds. Trauma to the nerve results in an inability to lengthen a vocal fold and thus to create a higher-pitched sound. The external branch of the SLN is probably the most commonly injured nerve in thyroid surgery. The rate of injury to the external branch of the SLN has been estimated at 0-25%. This rate is probably underestimated, because the diagnosis is frequently missed. |
|
|
138, Management of an overdose of paracetamol could include all of the following EXCEPT
A. activated charcoal B. alkalinisation of the urine C. gastric lavage D. hepatic transplantation E. N-acetylcysteine |
B
Alkalinisation is for salicylate overdose |
|
|
137. During elective major vascular surgery the best way to reduce the risk of acute renal failure is to maintain a normal
A. cardiac output B. central venous pressure C. mean arterial blood pressure D. pulmonary capillary wedge pressure E. renal blood flow |
E
Main cause of renal failure post-vascular surgery will be an ischaemic (i.e. pre-renal cause) MAP and RBF both seem kind of right – but RBF is surely more correct The question was repeated the following year but with only CO, MAP and RBF present as same options. |
|
|
136. In a patient with myasthenia gravis undergoing a laparotomy for large bowel obstruction, the need for post-operative ventilation is significantly increased by a
A. daily dose of pyridostigmine > 180 mg B. known history of resistance to suxamethonium C. known history of sensitivity to non-depolarising muscle relaxants D. past history of prednisolone treatment > 10 mg.day-1 E. recent history of dysphagia |
E
Similar to previous question " Any degree of bulbar palsy is predictive of the need for both intra- and post-operative ventilation" Miller: Post-op ventilation is especially important in cases involving: • myasthenia gravis of more than 6 years duration • chronic obstructive lung disease • daily pyridostigmine requirement of 750 mg in association with significant bulbar weakness • vital capacity of less than 40 mL/kg |
|
|
135. Characteristics of remifentanil include all of the following EXCEPT
A. a weakly active metabolite B. high potency C. metabolism by pseudocholinesterase D. muscle rigidity following rapid bolusing E. very short context-sensitive half-life |
C
Non-specific Plasma, Red Cell & Tissue Esterases |
|
|
133. The age at which separation anxiety begins in most infants is approximately
A. 1 month B. 3 months C. 6 months D. 9 months E. 12 months |
C
A&A 2001: “In the first weeks of life, infants are able to discriminate among people, but will accept care and comfort from adults other than their parents (14). By 3 mo of age, however, infants begin to respond differently to familiar and unfamiliar people. Older infants smile more at familiar people and may even try to engage their attention (14). Separation anxiety usually begins at 7–8 mo of age and peaks around 1 yr of age” |
|
|
132. In patients with hypokalaemic periodic paralysis one should avoid
An anxiolytic drugs B. beta-adrenergic antagonists C. intravenous dextrose D. regional anaesthesia E. suxamethonium |
C
Miller: Preoperative stress should be adequately alleviated by the administration of anxiolytic drugs such as benzodiazepines...A normal response to succinylcholine is noted in these patients... Spinal anesthesia and epidural anesthesia are safe alternatives to general anesthesia in these patients. It should be noted, however, that epidural, axillary, and intercostal nerve blocks lower serum potassium 0.3 to 0.7 mmol/L on average. Administration of epinephrine with the local anesthetic accounts for a proportion of this decline Dextrose insulin release decreased K |
|
|
131, The LEAST likely complication of a peribulbar regional block for cataract surgery is
A. bradycardia B. damage to the optic nerve C. globe perforation D. ocular muscle palsy E. peribulbar haemorrhage |
B
Rubin BJA 1995 75;93 Ocular muscle palsy - temporary "common" - prolonged (6 weeks) 1% Retro or peribulbar haemorrhage 0.1 - 1.7% Vasovagal response 0.5 - 0.85 % Optic nerve penetration - 0.2% Globe perforation 0 - 0.2% Oculocardiac reflex 0% |
|
|
130, In a child with NO history of epilepsy the commonest cause of post-operative convulsions is
A. hyperthermia B. hyponatraemia C. hypoxia D. local anaesthetic toxicity E. pethidine toxicity |
C
|
|
|
129. In the management of exposure to toxic nerve agents (highly potent anticholinesterases)
A. early treatment with glycopyrrolate is more effective than atropine ketamine is contra-indicated for endotracheal intubation C. oximes (e.g. pralidoxime) in normal doses have no endogenous anticholinergic effects D. oximes reactivate acetylcholinesterase by cleavage of phosphorylated active sites E. pre-treatment with pyridostigmine prevents the effects of these agents |
D
BJA.White 89 (2): 306 (2002). Implications of chemical and biological weapons for anaesthesia and intensive care: A: False. "Atropine and oximes are effective antidotes if administered early after exposure. Atropine antagonizes muscarinic side-effects and is more beneficial than glycopyrrolate, which has a shorter half-life and does not cross the blood-brain barrier." B: False. "Ketamine may be beneficial for intubation." C: False. "They (oximes) in normal doses have an endogenous anticholinergic effect." D: True. "Administered early, oximes reactivate AChE by cleavage of phosphorylated active sites." E: False |
|
|
128. When a new diagnostic test is evaluated in a group of subjects in whom the diagnosis is known, the following results are obtained
Disease known Disease known to be present to be absent New test result positive 2 4 New test result negative 6 8 The specificity of the new test is closest to A. 25% B. 33% C. 57% D. 67% E. 75% |
D
Specificity = TN / (TN + FP) = 8 / (8+4) = 0.67 |
|
|
127. Haemodynamic responses to pneumoperitoneum include all the following EXCEPT
A. decreased cardiac output B. decreased venous vascular resistance C. increased pulmonary artery occlusion pressure D. increased systemic vascular resistance E. increased systemic blood pressure |
B
Venous resistance is increased |
|
|
126. The most appropriate intravenous fluid volume to administer to a one-year-old 10 kilogram infant, fasted for five hours having minor peripheral surgery of two hours duration (with minimal blood loss) is
A. 200 ml B. 260 ml C. 320 ml D. 410 ml E. 490 ml |
C
Fluid requirements per hour: 4ml/kg/hr first 10 kg 2ml/kg/hr next 10 kg 1ml/kg/hr each further kg 10kg child 7hr x 40ml/hr = 280ml Third space losses = 0-2ml/kg/hr for relatively atraumatic surgery or 6-8ml/kg/hr for traumatic procedures, so 2ml/kg/hr x 10kg x 2hr = 40ml Total = 320ml See Morgan and Mikhails Clinical Anesthesiology 4th ed P. 937 |
|
|
125. In the management of torsades de pointes (a type of ventricular
tachycardia), all the following drugs may be useful EXCEPT A. amiodarone B. isoprenaline C. lignocaine D. magnesium E. phenytoin |
A
Amiodarone prolongs the QT |
|
|
124. The bibliographic database of LEAST relevance to anaesthetists is
A. CINAHL B. Cochrane Library C. Embase D. Medline E. PsycINFO |
E
|
|
|
123, The dose of phenylephrine in one drop (assume one drop = 0.05 ml) of 10% phenylephrine solution is
A. 5 microgram B. 20 microgram C. 200 microgram D. I milligram E. 5 milligram |
E
10% solution = 100mg/ml So one drop = 0.05 ml = 0.05 x 100 = 5mg |
|
|
122 In patients suffering from multiple sclerosis it is better to avoid the use of
A. epidural lignocaine B. neostigmine C. pancuronium D. spinal anaesthesia E. suxamethonium |
E
Depends how severe the disease is – if mild disease then D may be true, if severe disease E more likely: Current Opinion in Anaesthesiology 2002, 15:365-370 Succinylcholine poses the risk of hyperkalemia due to the release of intracellular potassium. Hyperkalemia after depolarizing neuromuscular block represents a risk to all patients with muscle denervation pathology, and may lead to cardiac arrest. Only patients with lesions involving motor nuclei, as evidenced by flaccidity, spasticity or hyperreflexia, are at risk for hyperkalemia. Upregulation ofacetylcholine receptors even by the fourth day after the onset of symptoms leads to sensitivity to succinylcholine in multiple sclerosis patients. Patients remain at risk for hyperkalemia for months or years and succinylcholine is best avoided |
|
|
121. The American Society of Anaesthetists (ASA) Physical Status Classification rating system was designed for categorising
A. intra-operative adverse anaesthetic event risk based on physical status B. intra-operative adverse surgical event risk based on physical status C. physical status in a standardised manner D. peri-operative adverse anaesthetic event risk based on physical status E. peri-operative adverse surgical event risk based on physical status |
C
Consensus on wiki seems to be C |
|
|
120. Which of the following sequences best indicates the order of
structures in the path of a needle inserted in the midline for placement of a spinal anaesthetic? A. interspinous ligament, supraspinous ligament, ligamentum flavum, epidural space, dura mater, arachnoid mater B. supraspinous ligament, interspinous ligament, ligamentum flavum, epidural space, dura mater, arachnoid mater C. supraspinous ligament, interspinous ligament, ligamentum flavum, epidural space, dura mater, pia mater D. supraspinous ligament, ligamentum flavum, interspinous ligament, epidural space, dura mater, arachnoid mater E. supraspinous ligament, ligamentum flavum, interspinous ligament, epidural space, dura mater, pia mater |
B
1. Supraspinous ligament 2. Interspinous ligament 3. Ligamentum flavum 4. Epidural space 5. Dura mater 6. Arachnoid mater 7. Pia mater |
|
|
119. The risk of seroconversion of a non-immunised anaesthetist, after a needlestick injury with a hollow needle contaminated with blood containing Hepatitis B virus, is approximately
A. 10% B. 20% C. 30% D. 40% E. 45% |
C
"The risk of HBV seroconversion after a percutaneous injury ranges from 23% to 62% in unvaccinated persons and is dependent on the hepatitis B e antigen status of the source." Clinics in Liver Disease - Volume 14, Issue 1, February 2010 |
|
|
118. Peri-operative cardiac morbidity and mortality in patients with
coronary artery disease undergoing non-cardiac surgery is significantly reduced by A. ceasing smoking one month pre-operatively B. controlling moderate systemic hypertension pre-operatively C. delaying surgery for one month following percutaneous transluminal coronary stent insertion D. delaying surgery for three months following an uncomplicated myocardial infarction E. tight peri-operative control of blood sugar level in diabetic patients |
C
AHA guidelines: Looks like there is very high risk with surgery within 1 month of stent placement. Rare to have events after 1 month. This may have changed from prior guidelines that suggested waiting 3 months post MI |
|
|
117. Neurological outcome following traumatic brain injury is best predicted by
A. blood pressure immediately following injury B, initial Glasgow Coma Scale score C. intracranial pressure D. jugular bulb oximetry E. progress in the first 24 hours |
B
IMPACT trial – prognosis after TBI. Journal of Neurotrauma;Feb 2007;Vol. 24 (2): • “The most powerful independent prognostic variables were age, Glasgow Coma Scale (GCS) motor score, pupil response, and computerized tomography (CT) characteristics, including the Marshall CT classification and traumatic subarachnoid hemorrhage” |
|
|
116. The commonest cause of maternal convulsions in the immediate post-partum period is
A. amniotic fluid embolism B. eclampsia C. epilepsy D. local anaesthetic toxicity E. water intoxication due to syntocinon infusion |
B
CEACCP – whilst epilepsy is most common cause in pregnancy, eclampsia is most common in the per-partum period |
|
|
115. The most important characteristic of non-particulate antacids in obstetrics is their
A. inability to cross the placenta B. low cost C. pleasant taste D. reduced incidence of nausea E. speed of onset of action |
E
Sodium citrate is an antacid used as prophylaxis against aspiration pneumonitis before a rapid sequence induction. 30 ml of a .3 molar solution should be given less than 10 minutes before the start of surgery due to its limited duration of action |
|
|
114. The effect of a drop in patient core temperature from 37°C to 34°C is to
A. decrease arterial blood pressure B. decrease blood glucose concentration C. decrease blood viscosity D. impair platelet adhesion E. increase blood potassium concentration |
D
A fall from 37 to 34 will cause tachycardia, hypertension and increased SVR because of sympathetic stimulation. As the temperature falls more, bradycardia and hypotension will occur. Mild/moderate hypothermia is associated with hypoK, hypoPO4, hypoMg. At 34C platelets appear activated but aggregation and adhesion is decreased. Viscosity is increased |
|
|
113. To normalise platelet function prior to surgery, chronic diclofenac therapy should be ceased for at least
A. 12 hours B. 1-2 days C. 4 days D. 7 days E. 10 days |
B
Half-life if diclofenac is 1.1-1.8hrs. After 5 half lives (5-10hrs) plasma concentration of diclofenac should be down to 5% of steady state. But how long does it take platelet function to return to normal? - thinking it would be more than 12hrs |
|
|
112. The strongest indication for the use of transoesophageal echocardiography during major non-cardiac surgery is
A. recent myocardial infarction (less than six weeks old) B. acute significant intra-operative ST segment depression on the ECG C. massive intra-operative blood loss D. a history of severe valvular heart disease E. unexplained significant intra-operative hypotension |
E
Table in Miller has a table evaluating use of TOE and this is one of its most appropriate uses. It can differentiate causes and thereby probably is most effectively used as it will more impact on treatment |
|
|
111. Which of the following parameters occurring during cardio-
pulmonary bypass (at 28°C) is most likely to contribute to an adverse neurological event post-operatively? A. arterial carbon dioxide partial pressure (PaCO2) below 30 mmHg B. arterial oxygen partial pressure (Pa02) over 400 mmHg C. blood sugar level (BSL) over 15 mmo1,1-1 D. mean arterial blood pressure below 60 mmHg E. pump flow less than 2.4 1.m-2.min-1 |
C
Neuroprotection during cardiac surgery.Expert Rev Cardiovasc Ther. 2008 Apr;6(4):503-20 "Although a recent retrospective analysis [15] failed to demonstrate an association between maximum intraoperative glucose concentration and adverse neurological ourtcome, an earlier prospective study revealed worse neuropsychological outcome in patients exposed to hyperglycaemia." "Despite considerable research, the characteristics of ‘optimal’ CPB perfusion remain to be defined. Profound hypotension combined with prolonged cerebral hypoperfusion is clearly injurious to the brain – particularly the watershed zones. However, within the bounds of usual CPB conduct, pressure, flow rate and flow character appear to have little influence on neurological outcome. A recent retrospective study suggests, perhaps paradoxically, that higher perfusion pressure is associated with worse neurological outcome." |
|
|
110. A reflex hypertensive response to bladder dilation is common in patients with a spinal cord lesion at or above
A. seventh cervical vertebra (C7) B. fifth thoracic vertebra (T5) C. ninth thoracic vertebra (T9) D. twelth thoracic vertebra (T12) E. fourth lumbar vertebra (L4) |
B
Clinical Anesthesiology Ch 27 "Overactivity of the sympathetic nervous system is common with transections at T5 or above but is unusual with injuries below T10. Interruption of normal descending inhibitory impulses in the cord results in autonomic hyperreflexia. Cutaneous or visceral stimulation below the level of injury can induce intense autonomic reflexes: sympathetic discharge produces hypertension and vasoconstricltion below the transection and a baroreceptor-mediated reflex bradycardia and vasodilation above the transection. Cardiac arrhythmias are not unusual." |
|
|
109, In a Jehovah's Witness patient undergoing a revision of a total hip replacement, the most effective technique to minimise post¬operative anaemia would be
A. epidural anaesthesia B. induced hypotension C. intra-operative cell saving D. intra-operative intentional normovolaemic haemodilution E. pre-operative administration of recombinant erythropoietin |
E
Difficult to choose which is most effective: A - epidural anaesthesia, does reduce blood loss by up to 50%. Due to relative hypotension and possibly negative intrathoracic pressure B - induced hypotension, does reduce blood loss by a relatively minor degree C - cell saver, is effective and acceptable to most JW D - normovolaemic haemodiltion is unacceptable to many JW E - EPO will raise the pre-op hb. In "Surgery Without Blood" Crit Care Med 2003 Vol31, "Increased preop red cell mass" ranks higher than cell salvage |
|
|
108. In infants with congenital pyloric stenosis
A. dehydration is associated with early hyponatremia B. plasma chloride levels seldom fall below 85 mmo1,1-1 C. renal conservation of hydrogen and potassium ions occurs D. the urine is initially alkaline, then may become acidic E. vomiting causes a loss of potassium ions |
D
Anaesthesia & Intensive Care Medicine Volume 9, Issue 4, April 2008: "Vomiting normally results in equal loss of gastric acid and alkaline duodenal fluid. However, with gastric outlet obstruction, gastric acid along with a variable amount of Na+ and K+ is lost in vomitus without loss of HCO3− from the duodenum. The resultant systemic alkalosis overwhelms the capacity of the proximal convoluted tubule to reabsorb HCO3−, producing an alkaline urine. As extracellular fluid volume depletion increases, aldosterone is secreted, leading to renal conservation of Na+ in exchange for K+. Eventually hypokalaemia forces Na+ exchange preferentially with H+ instead of K+ in the renal tubules. This produces the characteristic ‘paradoxical acid urine’ in the face of systemic alkalosis." |
|
|
106. Side-effects of protamine include all of the following EXCEPT
A. anaphylaxis B. platelet dysfunction C. pulmonary hypertension D. pulmonary oedema E. systemic hypertension |
E
UptoDate: "Hypotension, cardiovascular collapse, noncardiogenic pulmonary edema, pulmonary vasoconstriction, and pulmonary hypertension may occur." |
|
|
105. Early complications following pneumonectomy include all of the following EXCEPT
A. broncho-pleural fistula B. respiratory failure C. right heart failure D. right to left shunt E. supraventricular arrhythmias |
A
Note: wording in 2006 Mar was "Complications, which usually present early following pneumonectomy, include all of the following EXCEPT" The point of contention is whether or not a broncho-pleural fistula represents an early or late complication • if it is early, then "right to left shunt" is the answer • right to left shunting is theoretically likely as the PVR is doubled and PFOs occur in 20% of the population • it is described intra-operatively, early, and late, but the magnitude of the problem seems to be small • you would require a very high PVR to get clinically important shunting however If it is late, then "broncho-pleural fistula" may be the answer |
|
|
104. The average expected depth of insertion of an oral endotracheal tube, from the lip, in a normal newborn infant is
A. 7.5 cm B. 8.5 cm C. 9.5 cm D. 10.5 cm E. 11.5 cm |
C
Paediatric advanced life support: Australian Resuscitation Council Guidelines 2006) in a newborn is 9.5 cm, 11.5 cm for a 6 months old infant 12 cm for a 1 year old. Thereafter, the approximate depth of oral insertion is given by the formula: age (years)/2 + 12 cm. Neonates: Weight in Kg + 6. So 3.5Kg = 9.5cm at lips |
|
|
103. The most important effect of Lugol's Iodine administration prior to thyroid surgery is
A. a reduced incidence of thyroid storm B. a reduced incidence of vocal cord palsy C. an increased chance of preservation of the parathyroid glands D. increased pigmentation to assist in gland identification E. reduced vascularity of the gland |
E
BJA article and stoelting report it decreases vascularity |
|
|
102. Acute cannabis use just prior to surgery is most likely to
A. cause intra-operative bradycardia B. decrease anaesthetic requirements C. increase the incidence of peri-operative nausea D, increase the risk of intra-operative awareness D. reduce the reliability of a BIS (bispectral index) monitor |
B
Reduced anaesthetic requirement with recent administration, however will result in higher anaesthetic requirement during withdrawal in chronic users . BJA CEPD "Abusers and anaesthesia" |
|
|
101. The use of Xenon in anaesthesia is limited because it
A. has a blood/gas solubility coefficient similar to that of ether B. is a myocardial depressant C. is less potent than nitrous oxide D. is expensive to extract E. lacks analgesic properties |
D
|
|
|
100. The first step in developing a clinical audit should be to
A. define the question to be asked B. develop the relevant clinical protocol C. draw up the audit form D. find the relevant standards E. obtain ethics committee approval |
A
The clinical audit process seeks to identify areas for service improvement, develop & carry out action plans to rectify or improve service provision and then to re-audit to ensure that these changes have an effect.-->Clinical audit can be described as a cycle or a spiral, see figure. Within the cycle there are stages that follow the systematic process of: establishing best practice; measuring against criteria; taking action to improve care; and monitoring to sustain improvement. As the process continues, each cycle aspires to a higher level of quality. Stage 1: Identify the problem or issue Stage 2: Define criteria & standards Stage 3: Data collection Stage 4: Compare performance with criteria and standards Stage 5: Implementing change |
|
|
99. The most common reason for patients complaining about their medical treatment is
A. charging of excessive fees B. patient's predisposition to complain C. poor communication with medical staff D. poor outcome of medical treatment E. poor physical environment |
C
|
|
|
98. In a patient undergoing a femoro-popliteal bypass, the most predictive independent risk factor for the development of post-operative myocardial infarction would be
A. an acute myocardial infarct 3 months ago B. an episode of intra-operative myocardial ischaemia C. an episode of post-operative myocardial ischaemia D. 50% blood volume blood loss intra-operatively E. poorly controlled diabetes mellitus |
C
Similar to previous question |
|
|
97. Twenty-four hours following a vaginal hysterectomy, a 48-year-old obese female complains of severe pain that radiates down both buttocks and thighs. She had received a spinal anaesthetic with hyperbaric lignocaine. A likely explanation for these complaints includes all of the following EXCEPT
A. a spinal abscess B. a spinal haematoma C. lumbar disc herniation D. transient neurological symptoms syndrome E. trauma due to improper positioning |
A
Too early for abscess surely |
|
|
96. Aortic valve stenosis is more likely to be severe if
A. a loud second heart sound is present B. an ejection click is heard C. a third heart sound is present D. the murmur is long in duration and peaks late in systole E. the systolic murmur is transmitted to the carotid arteries |
D
• 2nd heart sound is soft with AS. UptoDate : “S2 is soft and single since A2, which is due to aortic valve closure, is delayed and tends to occur simultaneously with P2” • Click goes away as gets severe. "In the young patient with valvular AS, a systolic ejection sound (systolic ejection click) initiates the systolic murmur but later tends to disappear as AS becomes severe” • 3rd heart sound is sign of heart failure. Could have heart failure with severe AS – but a direct marker of severity • The three most important signs indicating AS is severe in the older patients are late peaking of ejection systolic murmur, S2 that is single or A2 that is paradoxical, and the ejection systolic murmur is a seagull sound that is not frequently heard but is very specific." • Is transmitted to carotids but its presence doesn't indicate severity |
|
|
92. A 52 year old asthmatic female has a difficult intubation for
laparoscopy. After four attempts at intubation over three minutes, the saturation has decreased from 98% to 73%. The physiological change most likely to have occurred as a consequence of the above is a A. decrease in sytemic blood pressure B. decrease in cardiac output C. displacement of the Haemoglobin-oxygen dissociation curve to the left D. decrease in pulse rate E. increase in pulmonary artery pressure |
E
From NUNN: Hyperventilation once PaO2 52.5mmHg Increased pulmonary artery pressure Increased cardiac output improves regional blood flow Sympathetic activation Vasodilation in every organ except pulmonary vasculature Right shift of O2 curve by increased 2,3 DPG and acidosis if present Anaerobic metabolism |
|
|
91. The sciatic nerve
A. can be readily identified during neural blockade by the production of paraesthesia on contact with a needle B. has no sympathetic fibres C. is formed from the dorsal branches of the anterior rami of L5 and S1 to S4 D. provides motor innervation to the psoas muscle E. provides sensory innervation from the knee joint |
E
|
|
|
90. The primary duty of an expert witness called by the defence is to the
A. Court B. Defence Counsel C. defendent doctor D. medical profession E. patient taking legal action |
A
|
|
|
89. The most appropriate investigation to diagnose Type A aortic dissections in potentially unstable patients is
A. angiography B. CAT scan C. magnetic resonance imaging (MRI) D. transoesophageal echocardiography E. transthoracic echocardiography |
D
In the unstable patient this is most appropriate. TTE is not sensitive enough |
|
|
88. A dock-worker is extricated from beneath a fallen lift platform and has signs of respiratory distress. He has a jagged wound of the chest wall with blood-stained froth alternately oozing from, and sucking back into the wound. Initial treatment at the scene should be to
A. start mouth-to-mouth resuscitation B. apply large sterile packs to the wound and instruct the patient to hold these in place until he reaches hospital C. apply large sterile packs and seal the dressing with adhesive tape D. insert an intercostal drainage tube connected to an underwater seal E. pass an endotracheal tube |
D
Trauma.org: “The definitive management of the open pneumothorax is to place an occlusive dressing over the 'wound and immediately place an intercostal chest drain” |
|
|
87. Hyperosmolar non-ketotic coma is associated with
A. a normal coagulation profile B. a normal serum sodium concentration C. a normal urinary potassium concentration D. intracellular dehydration E. known diabetic patients |
D or E
Similar to some previous questions - ?which is best out of D and E though |
|
|
84. Beta-blockade has been shown to decrease the incidence of post-operative myocardial ischaemia. This is most likely due to a reduction in
A. heart rate in the post-operative period B. post-operative blood glucose level C. post-operative hypercoagulability D. systemic blood pressure in the post-operative period E. the incidence of post-operative cardiac arrhythmias |
A
Similar to 2001-2 Q79 |
|
|
82, Adverse effects of a remifentanil infusion for surgery under general anaesthesia include
A. a 10% incidence of post-operative nausea and vomiting B. delayed respiratory depression after prolonged infusions C. increased sensitivity to morphine post-operatively D. muscle rigidity with an infusion rate of 0.5 mcg.kg-1,mirr1 E. pain on bolus injection |
D
MIMS Online: "Skeletal muscle rigidity can be caused by remifentanil and is related to the dose and speed of administration. Remifentanil may cause chest wall rigidity (inability to ventilate) after single doses of > 1 microgram/kg administered over 30 to 60 seconds or infusion rates > 0.1 microgram/kg/minute. Administration of doses < 1 microgram/kg may cause chest wall rigidity when given concurrently with a continuous infusion of remifentanil." |
|
|
81. Following superficial and deep cervical plexus blockade for carotid endarterectomy, the incidence of ipsilateral phrenic nerve block is
A. less than 10% B. 20-30% C. 50-60% D. 80-90% E. nearly 100% |
C
Anaesth Intensive Care. 1998 Aug;26(4) "This study detected a 55% incidence of phrenic nerve block which is similar to the 61% incidence reported by Castresana et al for deep and superficial cervical plexus block. This incidence is lower than that reported for interscalene plexus block which was 100%, and similar to reports for supraclavicular brachial plexus block where a rate of 67% was reported." |
|
|
80. Pain continuing well after the rash of Herpes Zoster has disappeared (Post Herpetic Neuralgia)
A. has an incidence of approximately 25% B. is more common after ophthalmic than after spinal segment involvement C. is more common in the immunocompromised but is independent of age and gender D. is best treated with high dose opioids E. has been shown to occur less commonly after acyclovir (Zovirax) |
E
However now E is probably false - Most recent ANZCA pain book has reversal of recommendations: "However contrary to the previous literature the use of the antiviral agent aciclovir did not significantly reduce the incidence of post-herpetic neuralgia" |
|
|
76. Asbestos exposure is typically associated with each of the following EXCEPT
A, pleural effusions B. mesothelioma of the pleura C. laryngeal cancer D. hilar lymphadenopathy E. gastrointestinal cancer |
D
UptoDate: A - "As an example, benign asbestos pleural effusions (BAPEs) usually occur within 15 years of first exposure to asbestos (range less than 1 year to up to 50 years)" C. laryngeal cancer - true: "A weak linkage between laryngeal carcinoma and exposure to the dry cleaning agent perchloroethylene has been described. Other occupations or occupational hazards have been linked to HNC. These include asbestos" D. hilar lymphadenopathy - "Hilar and mediastinal lymphadenopathy are not seen with asbestosis and should suggest the presence of another process." |
|
|
72. The TEC 6 desflurane vaporiser provides a constant vapour pressure of
A. 1100 mmHg at 32°C B. 1380 mmHg at 38°C C. 1460 mmHg at 39°C D. 1520 mmHg at 40°C E. 1520 mmHg at 42°C |
C
"A parallel flow issues from a heated (39°C) enclosure (sump) containing liquid and gaseous desflurane, the latter at a total pressure of about 1500 mmHg (approx 2 atm)” Pharmacology of Inhaled Anaesthetics, p211 |
|
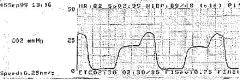
67. The following capnograph tracing is most likely to represent
A. partial obstruction of sampling tube B. sticking ventilator bellows C. incomplete neuromuscular blockade D. air entrainment into sampling tube E. partial obstruction of endotracheal tube |
D
Entrainment of air into sample line → normal flat plateau with terminal peak just before inspiration End-tidal CO2 excretion waveform and error with gas sampling line leak. Anesth Analg 1988;67: "In summary, when there is a loose connection between an end-tidal CO, sampling line and the CO, analyzer (Saracap), the CO, excretion waveform is very unusual and consists of a long plateau followed by a brief peak, rather than the usual square CO, excretion waveform. The long CO, plateau is caused by entrainment of room air through the leaky connection by the continuous CO, analyzer suction, and the brief CO, peak is caused by the next PIP, which transiently pushes undiluted end-tidal gas through the sampling line into the CO, analyzer. Because the 0, and N,O values digitally displayed by the Saracap are mean exhalation values, the 0, and N20 concentrations are a function of both the size of the leak and the PIP." |
|
|
66, The patient most likely to desaturate significantly during one lung anaesthesia is one who is having
A. a left sided thoracotomy, has reasonable Pa02 values during two-lung ventilation, but poor pre-operative spirometry B. a right-sided thoracotomy, has relatively poor Pa02 values during two-lung ventilation but good pre-operative spirometry C. a left-sided thoracotomy and has diminished perfusion but not ventilation to the operative lung on a V/Q scan D. a right-sided thoracotomy, has relatively poor Pa02 values during two-lung ventilation and poor pre-operative spirometry |
B
Singer, The Patient Intolerant of One-Lung Ventilation: The predictors of hypoxaemia with OLV: Right sided surgery Good preoperative spirometry (FEV1 or FVC) Poor PaO2 during two lung ventilation, particularly in the lateral position High percentage of ventilation or perfusion to operative lung with V/Q scan |
|
|
64. A morbidly obese patient is to have an open cholecystectomy. Compared with a patient of normal weight the
A. risk of thromboembolism is increased by 20% B. dose of patient controlled intravenous analgesia is increased and is related more closely to body surface area than weight C. recovery time from atracurium is unchanged D. Increased volume of distribution of some drugs may prolong the elimination half-life even though clearance may be unchanged or increased E. volume of the central compartment is significantly changed |
D
A : obesity is associated with increased thromboembolism - CEACCP 2008(5): "Obese patients are at increased risk of venous thromboembolism; appropriately sized compression stockings, low molecular weight heparin, and dynamic flow boots should be used from arrival in theatre until full postoperative mobilization." B: same article as above: “when using total i.v. anaesthesia, the infusion rate should be calculated on total body weight, not ideal body weight." C: Clinical Pharmacology and Therapeutics (1990) 48 "Although atracurium concentrations were consistently higher in obese patients than in nonobese patients, there was no difference in the time of recovery from neuromuscular blockade between the two groups. Consequently, the median effective concentration was higher in obese than in nonobese patients" D: above CEACCP article: "An increase in Vd prolongs the elimination half-life, despite increased clearance “ E: same article: "The volume of the central compartment is largely unchanged, but dosages of lipophilic and polar drugs need to be adjusted due to changes in volume of distribution (Vd)." So not clear – both C and D appear correct |
|
|
54, In a mechanically ventilated patient the haemodynamic parameter that correlates most closely with hypovolaemia is
A. systolic pressure variation B. central venous pressure C. pulmonary artery occlusion pressure D. pulse pressure E. cardiac output |
A
British Journal of Anaesthesia 83 (4): 550–1 (1999): "Systolic pressure variation has not become popular in the UK, despite the fact that it correlates with hypovolaemia more closely than any other measured variable, including central venous pressure, pulmonary artery occlusion or diastolic pressure, pulse pressure, cardiac output or systolic arterial pressure." |
|
|
53, A sympathetic block could be effective in treating all of the following conditions EXCEPT
A. chronic tinnitus B. quinine poisoning C. post-cardiac-surgery pain syndrome D. phantom limb pain E. compartment syndrome |
E
Stellate ganglion/lower cervical sympathetic block has been advocated for diagnostic, therapeutic and prognostic purposes for a variety of conditions, including: CRPS I & II to the upper extremities Vascular insufficiency/occlusive vascular disorders of the upper extremities Poor lymphatic drainage and edema of the upper extremity following mastectomy Postherpetic neuralgia Phantom pain CRPS of the breast & pain following mastectomy Quinine poisoning Sudden hearing loss & tinnitus Hyperhidrosis of the upper extremity Ischemic cardiac pain Bell's palsy & a variety of orofacial pain syndromes, including neuropathic orofacial pain & trigeminal neuralgia Vascular headache, including cluster and migraine headaches & sympathetically maintained headaches. Neuropathic pain syndromes in cancer pain |
|
|
48. The pain of the first stage of labour is transmitted via
A. grey rami communicantes B. T1O-L1 anterior roots C. the hypogastric plexus D. inhibitory nerves to the internal vesical sphincter E. parasympathetic nerves |
C
Update in Anaesthesia - PAIN RELIEF IN LABOUR The uterus and cervix are supplied by afferents accompanying sympathetic nerves in the uterine and cervical plexuses, the inferior, middle and superior hypogastric plexuses and the aortic plexus. The small unmyelinated 'C' visceral fibres3 transmit nociception through lumbar and lower thoracic sympathetic chains to the posterior nerve roots of the 10th, 11th and 12th thoracic and also to 1st lumbar nerves to synapse in the dorsal horn4. The chemical mediators involved are bradykinin, leukotrienes, prostaglandins, serotonin, substance P and lactic acid5. As the labour progresses severe pain is referred to the dermatomes supplied by T10 and L1. In the second stage, the direct pressure by the presenting part on the lumbosacral plexus causes neuropathic pain. Stretching of the vagina and perineum results in stimulation of the pudendal nerve (S2,3,4) via fine, myelinated, rapidly transmitting 'A delta' fibres3. From these areas, the impulses pass to dorsal horn cells and finally to the brain via the spino-thalamic tract |
|
|
41. Patients with ankylosing spondylitis usually exhibit
A. skin rash B. raised Erythrocyte Sedimentation Rate (ESR) C, positive test for Rheumatoid Factor D. HLA B27 antigen E. urethritis |
D
Stoelting: "The strong familial incidence is supported by the finding that 90% of patients with ankylosing spondylitis are HLA-B27 positive compared to only 6% of the general population." |
|
|
35. In patients with Eisenmenger's Syndrome,
A. compensation for poor oxygenation at rest is achieved by an increase in cardiac output B. the high pulmonary vascular resistance is usually able to be treated with a specific vasodilator C. an Fi02 of 1.0 will produce a substantial improvement in Sa02 D, the usual clinical course includes right ventricular failure during the 3rd or 4th decade, and subsequent death E. venesection should be used to treat a haemoglobin greater than 180 04to prevent the problems of hyperviscosity |
D
• False, I presume this would increase the shunt • "No treatment has proved effective in producing sustained decreases in pulmonary vascular resistance, although intravenous epoprostenol may be beneficial." (Stoelting) • Increasing FiO2 won’t improve oxygenation with shunt • Usually die 2nd-4th decade • "Phlebotomy with isovolemic replacement should be undertaken in patients with moderate or severe symptoms of hyperviscosity" (Stoelting), however looks like it should be done when HCT > 65% ie Hb > 210 |
|
|
32. Post-intubation croup in paediatric anaesthesia
A. rarely occurs if uncuffed endotracheal tubes are used B. is reduced if prophylactic steroids are administered intra-operatively C. occurs predominantly in children under the age of five years D. can be treated with one millilitre of aerosolysed 4% racemic adrenaline E. is less frequent if local anaesthetic lubricants are used |
C
|
|
|
30. In the hand the median nerve supplies
A. abductor pollicis brevis B. adductor pollicis C. the first dorsal interosseous D. abductor pollicis longus E. extensor indicis |
A
Median nerve supplies the LOAF muscles in the hand (for Lumbricals 1 & 2, Opponens pollicis, Abductor pollicis brevis and Flexor pollicis brevis). Anatomy for Anaesthetist: "The lateral terminal branch of the median nerve sends off a short, stout and important branch immediately distal to the flexor retinaculum and 3 cm distal to the distal wrist skin crease, which plunges into the thenar eminence, there to supply the abductor brevis, opponens and flexor brevis of the thumb." |
|
|
28. Anatomical features of the spinal cord do NOT include
A. an anterior median fissure and a posterior median septum B. thirty-two pairs of spinal nerves C. a filum terminale ending at the coccyx D. four to six spinal arteries arising from the posterior inferior cerebellar arteries E. the anterior spinal artery arising from the vertebral arteries |
B
A. "The spinal cord presents an anterior median fissure and a shallow posterior median sulcus from which a glial posterior median septum extends about halfway into the substance of the cord." B. false: "There are 31 pairs of spinal nervesaeight cervical, 12 thoracic, five lumbar, five sacral and one coccygeal. Each is formed by the fusion of an anterior and posterior spinal root." C. "Below, the spinal cord tapers into the conus medullaris, from which a glistening thread, the filum terminale, continues down to become attached to the coccyx." D. unsure, ?probably false "The posterior spinal arteries comprise one or two vessels on either side derived from the posterior inferior cerebellar arteries. They supply the posterior grey and white columns on either side. These arteries are reinforced serially by spinal branches of the vertebral, deep cervical, intercostal, lumbar, ilio-lumbar and lateral sacral arteries; the lower branches being responsible for the blood supply of the cauda equina." E. "The anterior spinal artery is a midline vessel lying on the anterior median fissure and is formed at the foramen magnum by the union of a branch from each vertebral artery." |
|
|
26. The fall in body temperature seen intra-operatively is
A minimised by thermoregulatory vasoconstriction B. greater in the elderly because basal metabolic rate increases with age C. less well controlled by forced air warming than by a circulating water mattress D. decreased by high spinal blockade E. beneficial for patients with ischaemic heart disease |
A
• A is true, though anaesthesia interferes with this effect • BMR decreases with age • C is false, forced air warmers quite effective o "One of the most effective methods is forced-air warming." (Current Anaesthesia & Critical Care (2001) 12, 79-86) • D doesn’t sound true • E certainly false |
|
|
16, The second lumbar nerve root (L2) normally contributes to the each of the following nerves EXCEPT
A. femoral nerve B. obturator nerve C. genito-femoral nerve D. lateral cutaneous nerve of the thigh E. ilio-inguinal nerve |
E
Summary of branches of the lumbar plexus Iliohypogastric L1 Ilio-inguinal L1 Genitofemoral L1, 2 Dorsal divisions 8lateral cutaneous nerve of thigh L2, 3 femoral nerve L2–4 Ventral divisions obturator nerve L2–4 accessory obturator nerve L3, 4 |
|
|
8. Thiazide diuretics may cause
A. hypernatraemia B. precipitation of acute gout C. hypoglycaemia D. hyperkalaemia E. hepatic failure |
B
Yentis: "Side effects include hypokalaemia, hyponatraemia, hyperuricaemia, hypomagnesaemia, hypochloraemic alkalosis, hyperglycaemia, hypercholesterolaemia, exacerbation of renal and hepatic impairment, impotence, and rarely rashes and thrombocytopaenia." |

