![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
89 Cards in this Set
- Front
- Back
|
91. A 4-year-old child with obstructive sleep disorder presenting for
tonsillectomy A. is likely to suffer from daytime somnolence B. is unlikely to have a history of snoring C. is suitable for day-case surgery D. has a 40% chance of postoperative vomiting without anti-emetic treatment E. is likely to lose 5% of their blood volume during surgery |
E
Adults and teenagers with OSA are often obese and have daytime somnolence; younger children may have normal weight or failure to thrive and behavior disorders such as hyperactivity, attention problems, and enuresis A history of snoring is a sensitive, though not specific, symptom that supports the diagnosis of OSA Patients with mild-to-moderate obstructive disease (defined as AHI <10) and no comorbidities can usually be discharged home the same day if they are >3-yr-of-age – not specific enough to make this answer correct Some Contenetion on Anaesthesia MCQ, but: "Tonsillectomy is one of the most frequently performed ambulatory surgical procedures in children and is associated with an incidence of postoperative vomiting ranging between 40% and 73%." (Dexamethasone reduces postoperative vomiting and pain after pediatric tonsillectomy, in CJA Volume 50, Number 4, April, 2003) – perhaps 40% is too low “Microdebrider IT resulted in more intraoperative bleeding than ET (27.9 versus 8.7 mL, p = 0.003; and 1.2 versus 0.2 mL/kg, p <0.001). The median and maximum blood losses, respectively” Comparison of intraoperative bleeding between microdebrider intracapsular tonsillectomy and electrocautery tonsillectomy 2009 A google search finds multiple other references with intra-op blood loss low Seems it is actually E, but this would no longer be the case now |
|
|
90. When compared with non-selective non-steroidal anti-inflammatory drugs
(NSAIDs), the COX-2 selective drugs A. are less likely to induce bronchospasm in aspirin sensitive patients B. cause significantly fewer adverse renal effects C. have less effect on platelet function D. have lower analgesic efficacy E. have a similar incidence of gastrointestinal side-effects |
C & A
ANZCA pain book – A is also correct |
|
|
89. The syndrome known as transient radicular irritation, or transient
neurologic symptoms, following spinal anaesthesia occurs only in patients A. given intrathecal lignocaine B. having surgery performed in the lithotomy position C. given hyperbaric intrathecal solutions D. who experience an initial full recovery from spinal blockade E. who experience complete motor blockade with their spinal block |
D
Some studies and systematic reviews have found that mepivacaine and lidocaine at a range of dilutions cause more frequent symptoms than bupivacaine and prilocaine do."(Miller Ch 30) – i.e. but not the only cause "Transient neurologic symptoms after spinal anesthesia develop most frequently after ambulatory procedures, especially in patients placed in the lithotomy or knee arthroscopy positions." (Miller Ch51) – i.e but not only Dilution of spinal lidocaine does not alter the incidence of transient neurologic symptoms. Anesthesiology 90 (1999), pp. 445–449.37 "Transient neurologic symptoms (TNS) are symptoms of pain in the gluteal region that can radiate down both legs and appear within a few hours to 24 hours after an uneventful spinal anesthetic." (Miller Ch 70) |
|
|
88. When ketamine is used for management of acute post-operative pain
A. analgesia is usually accompanied by hallucinations B. a starting dose of 0.05 to 0.1 mg.kg-1.hour-1 is appropriate C. benzodiazepines are ineffective in decreasing dysphoric reactions D. morphine is contraindicated as respiratory depressant effects are additive E. the intravenous route is recommended because absorption is more reliable than via the subcutaneous route |
B
|
|
|
87. A 30 year old female requires drainage of a large wound abscess following
an abdominoplasty 1 week ago. She has been on enoxaparin (Clexane) 40 mg once a day for 8 days. She would probably have A. a prolonged prothrombin time (PT) B. a prolonged activated partial thromboplastin time (aPPT) C. normal coagulation, 12 hours after the last dose of enoxaparin D. a risk of bleeding, which would NOT be predicted by her antiXa activity E. her haemostatic function restored to normal after administration of 6 units of FFP (fresh frozen plasma) pre-operatively |
D
"The anti-Xa level is not predictive of the risk of bleeding and is, therefore, not helpful in the management of patients undergoing neuraxial blocks." (ASRA Consensus statement) |
|
|
86. During one-lung ventilation, hypoxic pulmonary vasoconstriction in the
non-ventilated lung A. is increased with high pulmonary artery pressures B. is decreased by applying CPAP (continuous positive airway pressure) to the non-ventilated lung C. reduces the shunt fraction by approximately 40% D. is reduced significantly by isoflurane E. is unaffected by hyperventilation |
C
A. is increased with high pulmonary artery pressures - false B. is decreased by applying CPAP to the non-ventilated lung - maybe true; CPAP will decrease the amount of shunted blood definitely, but does its application actually recruit alveoli and improve V/Q ratio?? C. reduces the shunt fraction by approximately 40% - maybe true: 50% is quoted figure D. is reduced significantly by isoflurane - false E. is unaffected by hyperventilation - probably false: pulmonary vessel tone is affected by hyper/hypocapnoea. Factors which inhibit HPV (and hence worsen shunt) Very high or very low PA Pressures Hypocapnoea High or low mixed venous PO2 Vasodilators e.g. SNP Pulmonary infection Inhalational anaesthetic agents (from: Morgan & Mikhail 3rd ed p528) |
|
|
85. The MAC (minimum alveolar concentration) and blood:gas partition co-
efficient of xenon are A. 71% and 0.14 respectively B. 45% and 0.24 respectively C. 101% and 0.24 respectively D. 45% and 0.42 respectively E. 71% and 0.47 respectively |
A
|
|
|
84. When investigating a patient following anaphylaxis during anaesthesia,
the test most widely applicable and least likely to produce false positive results, in identifying the responsible drug or drugs is A. skin prick testing B. I125 radiommunoassay (RIA) to specific circulating IgE C. RIA inhibition D. intradermal skin testing E. assessment of basophil degranulation and histamine release from leukocytes |
A
Skin tests are most useful for latex, beta lactam antibiotics and NMBAs. They are also useful for induction agents, protamine and chlorhexidine. Intradermal testing may be more reliable for propofol [2]. Skin tests are not usually performed for opioids because false positive results are common. However, skin prick testing appears to be informative for the synthetic opioids fentanyl and remifentanil. Skin tests are not useful for NSAIDs, dextrans or iodinated radiological contrast media because anaphylaxis to these agents is not usually IgE-mediated |
|
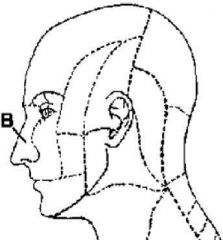
83. Sensory nerves supplying the territory marked "B" in the figure below, are derived from the nasal branch of the
A. anterior ethmoidal nerve B. infra-trochlear nerve D. infra-orbital nerve E. lacrimal nerve F. nasopalatine nerve |
A
The nasociliary nerve supplies the tip of the nose through the EXT NASAL BRANCH OF THE ANT ETHMOIDAL NERVE and the root of the nose through the infratrochlear nerve |
|
|
82. The most correct statement regarding intra-operative glucose
management in children is that A. 5% dextrose should be used B. there is a higher incidence of hypoglycaemia in children following overnight fasting than in children fasting during the daytime C. blood glucose monitoring is mandatory D. hyperglycaemia is harmless E. most children do not require glucose intra-operatively |
E
By elimination as well as Paediatr Anaesth. 2008 May;18(5) "Hypoglycemia is known to induce brain damage especially in newborn infant. However, the risk of preoperative hypoglycemia has been demonstrated to be low in normal healthy infants and children (1–2%), despite prolonged fasting periods (18–25). Thus, it would appear that in the vast majority of patients there is no need to administer glucose in the perioperative period nor there is a need to monitor blood glucose in these patients." |
|
|
81. The most correct statement concerning thyroid diseases is that
A. thyrotoxicosis has the same incidence in men and women B. thrombocytopaenia is associated with thyrotoxicosis C. the half life of T4 (thyroxine) is 2 days D. beta-blockers are contraindicated in acute thyrotoxicosis E. carbimazole acts within 2-3 days to reduce T^4 synthesis |
B
• Thyrotoxicosis has the same incidence in men and women - False Female:Male – 9:1 • Thrombocytopenia is associated with thyrotoxicosis - True May be associated - Uptodate • The half life of T 4 (thyroxine) is 2 days - False 7 Days Stoelting • Beta-blockers are contraindicated in acute thyrotoxicosis - False Indicated for immediate symptom control OHOCM 6th Edition • Carbimazole acts within 2-3 days to reduce T4 synthesis - False Noticable improvements may be seen in 1 – 2 days. Stoelting |
|
|
79. In Australia the current leading cause of direct maternal mortality is
A. cardiac disese B. complications of anaesthesia C. embolism D. pre-eclampsia and eclampsia E. post-partum haemorrhage |
C
Perinatal and Reproductive Epidemiology Research Unit http://www.preru.unsw.edu.au/ The leading causes of direct maternal deaths were: amniotic fluid embolism, thromboembolism and hypertension. Cardiac disease, psychiatric related causes and nonobstetric haemorrhage were the main indirect causes of maternal deaths |
|
|
78. In the pre-operative preparation of patients with phaeochromocytoma
A. phenoxybenzamine blocks alpha-1-adrenergic receptors only B. side-effects of phenoxybenzamine include drowsiness and nasal congestion C. labetalol can be used as the sole agent to control blood pressure D. 10 mg daily of phenoxybenzamine is usually sufficient to control blood pressure E. postural hypotension is an unwanted side-effect |
B
CEACCP - Phaeochromocytoma “Phenoxybenzamine is commonly started at least 14 days before 0surgery and continued until 1–2 days before surgery. It is thought that α-blockade is required for a minimum of 2 weeks in order torestore normovolaemia and myocardial function. Therefore, some advise treatment for months; stopping the drug a couple of days before surgery reduces the risk of postoperative hypotension. Starting dose is 10 mg twice daily and increased, depending on BP control, postural hypotension and nasal stuffiness, to 60–200 mg daily” Is E talking about unwanted side effect of phaeo or of phenoxybenzamine? Does phenoxybenzamine cause drowsiness? |
|
|
77. Serious post-operative epidural infection
A. is rarely due to Staphylococcal species B. is associated with epidural catheter disconnection C. occurs with an incidence in the range 1-2 per 10,000 D. is usually reported in obstetric cases E. mandates surgical drainage if an abscess is present |
C
Epidural Abscesses – BJA 2006: • Staph in 53-97% of cases • "reconnection is safe within 8 hr provided that the fluid inside the catheter is static and does not move when lifted above the level of the patient" • Incidence between 1:1000 to 1:100000 • “Estimating the true incidence of a rare complication from such disparate reports is not easy, but there is some suggestion that it might be of the order of 1 in 1000 in surgical, and 1 in 2000 in obstetric” • Medical Mx may be appropriate for small abscesses |
|
|
76. Carbon monoxide poisoning results in hypoxic injury by
A. binding to mitochondrial cytochrome oxidase B. decreasing alveolar ventilation C. occupying oxygen binding sites on haemoglobin D. reducing the arterial partial pressure of oxygen (PaO2) E. shifting the oxygen-haemoglobin dissociation curve to the right |
A & C
Also binds to cytochrome-c oxidase interfering with cellular respiration |
|
|
74. Chronic post-operative pain
A. in a phantom limb is reduced in incidence by administration of chemotherapy B. after thoracotomy has an incidence of approximately 50% C. following thoracotomy does NOT have its severity predicted by the severity of acute post-operative pain D. following mastectomy combined with implantation of a prosthesis is LESS likely to occur than following mastectomy alone E. following cholecystectomy is MORE likely if there is a history of classic gallbladder pain pre-operatively |
B
Chronic pain as an outcome of surgery. A review of predictive factors: "Long-term pain after thoracotomy, the postthoracotomy pain syndrome (PTPS), may have an incidence of more than 50%." |
|
|
73. Risk factors for post-operative delirium include all the following EXCEPT
A. age greater than 70 years B. history of alcohol abuse C. perioperative morphine administration D. electrolyte disturbance E. benzodiazepine administration |
C
Miller: "Opioids other than meperidine have not been associated with development of postoperative delirium" |
|
|
72. An INCORRECT statement regarding the management of hypocalcaemia
is that A. correcting a respiratory or metabolic alkalosis increases the level of ionised calcium B. undiluted calcium should be administered via a central vein as it is irritant to peripheral veins C. acidosis will decrease calcium binding to albumin and therefore increase ionised calcium D. when calcium alone is not sufficient for control of hypocalcaemia, Vitamin D metabolites can be added E. calcium chloride has been shown to be superior to calcium gluconate |
E
Miller: “When equivalent calcium doses are administered, both preparations are equally efficacious in restoring the calcium level to normal. In this regard, calcium gluconate is especially advantageous in peripheral venous administration because extravasated calcium chloride solution can result in severe tissue destruction." |
|
|
71. With respect to general anaesthesia for caesarean section
A. ketamine is NOT appropriate as an intravenous induction agent B. rapacuronium has a similar onset of action to suxamethonium C. awareness can be reduced by use of bispectral index monitoring D. inhalational anaesthetics should be discontinued after delivery E. fetal outcome is significantly improved by the use of 100% oxygen at emergency caesarean section |
C
B-aware trial – BIS monitoring reduced risk of awareness by 82% in GA caesarians Rapacuronium does have a similar onset time to sux though |
|
|
70. Which of the following alternatives is correct regarding the range of values
that odds ratios (OR) and relative risks (RR) can take? A. OR (0 to positive infinity); RR (0 to positive infinity) B. OR (negative infinity to positive infinity); RR (negative infinity to positive infinity) C. OR (0 to 1); RR (0 to 1) D. OR (0 to positive infinity); RR (negative infinity to positive infinity) E. OR (negative 1 to positive 1); RR (negative 1 to positive 1) |
A
|
|
|
69. Recognised factors that predispose upper limb nerves to compression
under anaesthesia include A. forearm extension and supination B. extreme flexion of elbows across the chest C. internal rotation of the abducted arm D. the lateral position with the uppermost arm flexed in an arm support E. the prone position with arms by the side and fingers flexed |
A
Iatrogenic upper limb nerve injuries: a systematic review – ANZJSurg 2011 Perioperative peripheral nerve injuries – CEACCP 2012 Brachial Plexus “A brachial plexus stretch injury is more likely if the arms are abducted beyond 90° and externally rotated with the elbow extended and the forearm fully supinated. The use of shoulder braces in a head-down (Trendelenburg) position, lateral flexion of the neck to the opposite side and depression of the shoulder have also been implicated” “This results from compression, stretching, or a direct injury as a result of a regional technique. Compression against the clavicle may occur during retraction of a median sternotomy or in the lateral decubitus position with compression against the thorax and humeral head. Arm abduction, external rotation with posterior shoulder displacement, causes considerable stretch on the upper brachial plexus roots. The same effect is seen when there is extreme abduction of the arm >90 degreees” Ulnar Nerve “Direct pressure on the ulnar groove in the elbow and prolonged forearm flexion are cited as the most common causes of injury” Radial Nerve “Tourniquets/arterial pressure cuffs, compression against a patient screen or an arm board positioned at an incorrect height creating a step, are the most common perioperative reasons cited for this nerve injury.” Median Nerve “Direct nerve damage from regional techniques, invasive procedures around the elbow, and compression in the carpal tunnel are usually responsible for injury to this nerve.” |
|
|
68. In unselected patients the risk of herpes simplex labialis in the
puerperium is A. approximately 10% after caesarean delivery using epidural or intrathecal morphine B. approximately 5% after normal vaginal delivery without epidural analgesia C. approximately 3% after caesarean delivery using parenteral, but not epidural or intrathecal morphine D. greater after caesarean delivery using epidural or intrathecal fentanyl, than without using fentanyl E. none of the above |
A
Neuraxial Morphine and Oral Herpes Reactivation in the Obstetric Population – AA 2010: Rates for reactivation vary in studies between 2.6-14.6% for epidural morphine Reactivation with systemic opioids 0-0.5% |
|
|
67. The pulmonary artery catheter
A. provides a sensitive monitor for myocardial ischaemia by measurement of pulmonary capillary wedge pressure (PCWP) B. may be safely inserted 7 days after transvenous pacemaker wire placement C. is contraindicated in patients with bifascicular conduction block on the ECG D. frequently causes significant tricuspid valve regurgitation E. when wedged, enables reliable detection of mitral valve regurgitation by noting the presence of ‘v’ waves |
E
Miller – Cardiovascular monitoring: Complete heart block is a complication of PA catheterization – presumably more likely if already in bifasicular block PAC can dislodge temporary pacing wires “Although myocardial ischemia will often be detectable as a rise in pulmonary artery diastolic, mean, or systolic pressure, these changes are generally less striking than the accompanying change in wedge pressure and the new appearance of tall a and v waves” “None of the current methods for detecting perioperative myocardial ischemia are perfectly sensitive or specific. Although patients with left ventricular ischemia are likely to have higher mean wedge pressure than those without ischemia, these differences are small and may be difficult to detect clinically” Mitral Regurgitation does produce a prominent v-wave in the wedge waveform “wedge pressure v waves are neither sensitive nor specific indicators of the severity of mitral regurgitation… Prominent wedge pressure v waves may exist in the absence of mitral regurgitation when LAP is high” |
|
|
66. To rule out raised intracranial pressure in an awake patient, the most
reliable finding is A. absence of papilloedema B. presence of retinal vein pulsation C. absence of headache D. absence of diplopia E. absence of vomiting |
B
J Neurol Neurosurg Psychiatry 2003;74:7-9: Spontaneous retinal venous pulsation: aetiology and significance “as the intracranial pressure rises the intracranial pulse pressure rises to equal the intraocular pulse pressure and the spontaneous venous pulsations cease. Thus it is shown that cessation of the spontaneous venous pulsation is a sensitive marker of raised intracranial pressure” |
|
|
65. When stimulating the ulnar nerve at the wrist to monitor neuromuscular
blockade, A. supramaximal currents in excess of 80mA will stimulate the adductor pollicis directly B. the sensitivity for assessment of neuromuscular blockade is the same as when stimulating the facial muscles C. adult size large ECG dot electrodes require the same current as paediatric size ECG dot electrodes D. monitoring in the presence of an upper motor neuron lesion will underestimate the neuromuscular block E. double burst stimulation is a reliable way to estimate the degree of blockade |
D
Stoelting p200: UMN → resistance to NMB because of upregulation of AChRc's |
|
|
64. Post-dural puncture headache
A. does NOT recur following discharge from hospital B. may be associated with hearing loss C. is more likely if a catheter has entered the subarachnoid space D. is reduced in incidence by prophylactic bed rest for 24 hours E. is worse if the patient is nursed in the prone position |
B
BJA 2003 PDPH "Other symptoms associated with dural puncture headache include nausea, vomiting, hearing loss,78 tinnitus, vertigo, dizziness and paraesthesia of the scalp, and upper108 and lower limb pain" |
|
|
63. With respect to hepatitis C (HCV), which of the following is FALSE?
A. the incidence of HCV in blood donors varies from 0.01% to 1.5% B. HCV infection persists after initial infection in about 80% of cases C. alanine aminotransferase (ALT) is used to monitor HCV infection and to detect chronic persistent infection D. long term follow-up shows 20 - 30% of HCV infected individuals develop cirrhosis E. interferon can halve the incidence of HCV viraemia |
C & E
Chronic viraemia in 85-90% of infected individuals 70% of those with chronic HCV develop some degree of chronic liver injury 20% of those develop cirrhosis within 20yrs Risk of cirrhosis is 15x higher in HCV infected individuals that abuse ETOH Risk of hepatocellular carcinoma in those with cirrhosis is 1-4% per year HCV RNA is the gold standard for monitoring treatment ALT can be normal in chronically infected GCV individuals Peg-Interferon + ribavirin can produce sustained response in around 56% |
|
|
62. Patients with sickle-cell trait
A. are usually anaemic B. never sickle C. sickle at very low haemoglobin saturations D. sickle with hypercarbia E. sickle with hyperthermia |
C
From Millers’: Sickle cell trait should not be considered a disease because hemoglobin AS cells begin to sickle only when the oxygen saturation of hemoglobin is below 20%. No difference has been found between normal persons (those with hemoglobin AA) and those with hemoglobin AS regarding survival rates or the incidence of severe disease, with one exception: patients with hemoglobin AS have a 50% increase in pulmonary infarction." (Miller 7th Ed Ch 35) |
|
|
61. Factors which do NOT contribute to the increased risk of aspiration
pneumonitis during pregnancy include A. increased gastrin production B. a tendency for the stomach to be pushed up against the left diaphragm C. increased acidity of gastric secretion D. increased volume of gastric secretion E. decreased secretion of the hormone motilin |
A
Do have increased gastric secretions and acidity, and it’s not related to gastrin production |
|
|
60. The primary factor controlling the rate of production of albumin is
A. colloid osmotic pressure B. serum atrial natriuretic factor concentration C. serum cortisol concentration D. serum growth hormone concentration E. serum sodium concentration |
A
Apparently A - Anaesthesia, Volume 53 Issue 8 Page 789-803, August 1998. Serum albumin: touchstone or totem? M. P. Margarson & N. Soni: “The primary factor controlling the rate of production is a change in the colloid osmotic pressure and the osmolality of the extravascular liver space. Synthesis is also stimulated by raised concentrations of insulin, thyroxine and cortisol . Growth hormone, despite its effects on reducing total urinary nitrogen loss, has no measurable effect on albumin synthesis in patients.” |
|
|
59. Factors contributing to carbon monoxide accumulation in a circle
absorber anaesthetic circuit include A. fresh baralyme B. sevoflurane C. exhausted baralyme D. halothane E. desflurane |
E
|
|
|
58. A healthy young adult suffering trauma involving pelvis and lower extremities presents to your emergency department. A MAST suit is in place and one litre of a colloid solution has already been given intravenously. The patient has a pulse rate of 140 beats.min-1, is anxious,
confused and hypotensive. Estimated blood loss as a percentage of blood volume is A. 10% B. 20% C. 30% D. 40% E. 50% |
E
History suggests ATLS Class IV haemorrhage (>40%) |
|
|
57. If the tracheal diameter measured on a PA chest x-ray at the level of the
sternoclavicular joint is between 16mm and 18mm, the best choice of double lumen tube would be A. 41 Fr B. 39 Fr C. 37 Fr D. 35 Fr E. 33 Fr |
B
Size of DLT to pick = (2 x trachea) + 5 |
|
|
56. When placing a patient in the lithotomy position
A. the femoral nerve is unlikely to be damaged B. the common peroneal nerve is not at risk of injury C. flexion at the hips of greater than 90 degrees will protect the obturator nerve D. damage to the sciatic nerve may be prevented by exaggerated external rotation of the hips E. damage to peripheral nerves is more commonly due to compression of blood supply, rather than direct pressure |
E
No clear right answer, probably right |
|
|
55. Complications of an intra-orbital local anaesthetic block are minimised if
A. the eye is oriented in a supero-medial direction for an infero-lateral injection B. the anaesthetic solution is placed posteriorly where the nerves are close together C. a shallow bevel (Atkinson-type) rather than a sharp intravenous ¬type needle is used D. the injection site is medial rather than supero-medial |
D
Anaesthesia MCQ answer |
|
|
54. For personnel working in an operating room environment
A. levels of volatile anaesthetic agents of less than 5 parts per million are considered safe B. chronic exposure to trace levels of anaesthetic agents causes significant cognitive impairment C. the risk of spontaneous abortion is increased D. the risk of cancer is increased in males E. none of the above |
E
Miller "The National Institute for Occupational Safety and Health has recommended that the upper limits in the atmosphere of operating rooms be 25ppm for nitrous oxide and 2ppm for halogenated anesthetics (or 0.5ppm for halogenated anesthetics used in combination with nitrous oxide)." (Miller 6th ed p.3151) The rest surely can’t be true |
|
|
53. A patient with severe liver disease is scheduled to have a portacaval
shunt for portal hypertension. Recommended features of the anaesthetic management include A. use of vecuronium as the relaxant of choice B. care with the dose of suxamethonium because it may have a prolonged effect C. avoidance of fentanyl as an analgesic D. avoidance of all volatile anaesthetic agents including isoflurane E. reduction of the induction dose of thiopentone |
E
Reduced levels of plasma-cholinesterase – but ?clinical significance |
|
|
52. At a late stage in severe septic shock
A. the myocardium becomes increasingly sensitive to catecholamines B. adrenaline should not be infused as it is predominantly an alpha agonist at low doses C. the infusion of endogenously occurring catecholamines is futile as blood levels are already too high D. the infusion of dopamine is strongly recommended as it exerts its effects in high doses via different receptors than in low doses E. inadequate catecholamine synthesis may contribute to the poor circulation |
E
|
|
|
51. The passage of an appropriately sized endotracheal tube in a neonate
suffering from the idiopathic respiratory distress syndrome (hyaline membrane disease) will A. impair oxygenation by making grunting impossible B. impair oxygenation by increasing airway resistance C. improve oxygenation by reducing dead space D. improve oxygenation by eliminating laryngeal obstruction E. have no effect on oxygenation |
A
Anaesthesia MCQ suggests A as these will be loss of auto-PEEP |
|
|
50. The most appropriate method for improving oxygenation during one lung
anaesthesia, after institution of an FiO2 of 1.0, is application of A. 5 cm H2O CPAP to the non-dependent lung B. 10 cm H2O CPAP to the non-dependent lung C. 5 cm H2O PEEP to the dependent lung D. 5 cm H2O CPAP to the non-dependent and 5 cm H2O PEEP to the dependent lung E. intermittent re-inflation of the non-dependent lung |
C
see CEACCP or Millers – Hypoxaemia and OLA |
|
|
49. When performing laser surgery on the airway
A. instruments with high reflectance are desirable B. poly-vinyl chloride (PVC) endotracheal tubes are more easily penetrated by the laser beam than red rubber tubes C. PVC tubes are more flammable than red rubber tubes D. the volatile anaesthetic agents support combustion E. the CO2 laser beam is reflected by moistened cotton swabs |
B & C
Miller – Anaesthesia for laser surgery “PVC tubes seem to be ignited much more easily by CO2 lasers than red rubber tubes [52] [58] [59] and to produce more toxic combustion products” Note:PVC more easily ignited – but flammability (judged by flammability index) is less (also from miller) |
|
|
48. Expected adverse drug effects in a geriatric population receiving a high
dose of a selective serotonin reuptake inhibitor for depression would include all of the following EXCEPT A. hyponatraemia caused by inappropriate secretion of ADH B. impairment of platelet aggregation caused by depletion of 5HT (serotonin) stores C. withdrawal symptoms characterised by anxiety, agitation and increased sweating D. sedation, dry mouth, orthostatic hypotension and cardiac conduction defects E. gastro-intestinal effects (nausea, vomiting, diarrhoea) |
D
These are more anticholinergic effects and not seen with SSRI’s |
|
|
47. According to the American College of Cardiology /American Heart
Association (ACA/AHA) Guidelines for Perioperative Cardiovascular Evaluation for Noncardiac Surgery, intermediate clinical predictors of increased perioperative cardiovascular risk include all of the following EXCEPT A. uncontrolled systemic hypertension B. diabetes mellitus C. prior myocardial infarct (over 6 weeks ago) D. compensated or prior congestive cardiac failure E. mild angina pectoris (Canadian Class I or II) |
A
From the guidelines |
|
|
46. Penetrating cardiac injury will most commonly produce damage to the
A. right atrium B. sino-atrial node C. left ventricle D. right coronary artery E. right ventricle |
E
Consider orientation of the heart |
|
|
The J-point of the ECG waveform is altered by all of the following EXCEPT
A. hypothermia B. tachycardia C. myocardial ischaemia D. calcium channel blockers E. digoxin |
D
J-point: where the QRS meets the ST segment |
|
|
44. Effects of volatile anaesthetic agents on the brain include
A. maintenance of cerebral blood flow when used with hypocapnia B. uncoupling of autoregulation, with a consequent rise in intracranial pressure C. reduction of cardiac output and cerebral blood volume when used at concentrations of 1.3 MAC D. maintenance of cerebral metabolic rate, but reduction of cerebral electrical activity E. equal depression of all neurons of the brain at 1.3 MAC concentration |
A
autoregulation isn’t uncoupled, it is the uncoupling of flow to CMRO2. Thinking A by process of exclusion |
|
|
43. The treatment LEAST likely to be useful for torsades de pointes is
A. defibrillation B. procainamide C. magnesium D. electrical pacing E. isoprenaline |
B
|
|
|
42. You are called to see a 30 year old man with rapidly deteriorating asthma.
Following appropriate medical management an endotracheal tube is inserted and he is ventilated with a mechanical ventilator with a tidal volume of 600 ml and a rate of 12 breaths per minute. Five minutes later the blood pressure is unrecordable and external cardiac massage is commenced. Arterial blood is taken and shows pH 7.08, pCO2 96 mmHg, pO2 36 mmHg, oxygen saturation 46% and bicarbonate 27 mmol.L-1. He is administered adrenaline, salbutamol, pancuronium, bicarbonate and calcium gluconate. The ECG shows sinus rhythm at a rate of 60 beats per minute. The patient remains pulseless and cyanosed with fixed dilated pupils and distended neck veins. The most appropriate continuing management is A. cease resuscitation B. administer further adrenaline C. insert bilateral intercostal drains D. cease ventilation for 30 seconds and resume at a slower rate E. increase peak inspiratory pressure |
D
|
|
|
41. A 24 year old female with mitral valve prolapse develops atrial flutter
during a diagnostic laparoscopy. The drug most likely to revert this arrhythmia is A. digoxin B. amiodarone C. verapamil D. esmolol E. Adenosine |
B
Who knows, probably b or c or d |
|
|
40. The presence of small bubbles of air in an invasive arterial pressure
monitoring system will always decrease the A. damping coefficient of the system B. resonant frequency of the system C. recorded systolic pressure D. recorded mean pressure E. extinction coefficient of the system |
B
Bubbles being compressible always cause an increase in damping coefficient AND a decrease in resonant frequency However, shouldn’t bubbles lead to increased damping, leading to decreased SBP.? |
|
|
39. The end-tidal CO2 partial pressure (PetCO2) may be greater than the
arterial CO2 partial pressure (PaCO2). Causes of this do NOT include A. transitory variations in V/Q matching and deadspace B. breathing with small tidal volumes C. PaCO2 fluctuations during the respiratory cycle D. exercise E. slow emptying of long time constant alveoli containing CO2 levels approximating mixed venous CO2 levels |
B
Anaesthesia & Intensive Care, 1994, Capnography article "Reasons for this include slow emptying of long-time constant alveoli containing CO2 levels approximating mixed venous CO2, transitory variations in V°/Q° matching and deadspace, the use of low frequency ventilation and PaCO2 fluctuations during the respiratory cycle". |
|
|
38. The power of a statistical test can be expected to decrease, if there is an
increase in A. the sample size B. the size of the treatment effect C. the chance of making a Type 1 error D. the variability of the population E. none of the above |
D
Power uses beta value, not alpha (see option C) |
|
|
37. Complications of coeliac plexus block include
A. hypertension B. failure of erection C. constipation D. paraplegia E. dysaesthesia along L3-4 |
D
|
|
|
36. When anaesthetising a patient with an acute pericardial tamponade,
A. the patient may be safely induced with a dose of 3-5 mg.kg-1 of thiopentone B. it is important to limit intravenous fluid infusion, to prevent further compression of the heart C. it is important to reduce afterload D. a slow heart rate allows time for optimal filling of the ventricle E. awareness is a potential problem after release of the tamponade |
E
All the rest are false. Cardiac output becomes HR dependents as ventricular filling in reduced |
|
|
35. Recognised features of malignant carcinoid syndrome do NOT include
A. hypotension B. bronchospasm C. diarrhoea D. arthralgia E. hypoglycaemia |
E
Though arthralgia also seems rare |
|
|
34. When paracetamol is used in infants and children,
A. a dose of 10 mg.kg-1 is more effective than placebo for relief of symptoms of tonsillitis B. the bioavailability of rectal suppositories is less than 50% of that from an equivalent oral dose C. a rectal loading dose of 45 mg.kg-1 will reliably produce therapeutic plasma levels with a peak concentration after 1 hour D. the elimination half life is 2 - 2.3 hours E. a far greater proportion of unmetabolised paracetamol is excreted by the kidney, compared to adults |
D
|
|
|
33. During anaesthesia for Magnetic Resonance Imaging,
A. any ferromagnetic items outside the 30 Gauss line will not be strongly attracted to the magnetic core B. any battery-powered monitor of non-ferromagnetic construction can be safely placed close to the magnetic core without risk of attraction to the magnet C. the most commonly used MRI contrast medium, gadopentetate dimeglumide (Magnevist) induces a similar incidence of side effects as does the iodinated contrast media used in radiology D. it is essential to limit the use of halogenated agents as halogen atoms exhibit the property of nuclear magnetic resonance and may interfere with image quality |
A
Australian Anaesthesia 2005 - Don’t Get Sucked in: Anaesthesia for Magnetic Resonance Imaging |
|
|
32. The clinical sign which has the highest correlation with awareness in a
spontaneously breathing patient under general anaesthesia is A. patient movement in response to a stimulus B. an increase in blood pressure and heart rate C. increased lacrimation and sweating D. pupillary dilation E. an increase in respiratory rate |
A
|
|
|
31. When a new diagnostic test is evaluated in a group of subjects in whom the diagnosis is known, the following results are obtained
Disease known Disease known to be present to be absent New test result positive 2 4 New test result negative 6 8 The specificity of the new test is closest to A. 25% B. 33% C. 57% D. 67% E. 75% |
D
Specificity = TN / (TN + FP) = 8 / (8+4) = 0.67 |
|
|
30. In a clinical trial, 3 out of 10 patients develop a complication in the
control group, and 1 of 10 patients develops the complication in the treated group. To assess whether this is a statistically significant difference the most appropriate statistical test to use would be the A. Chi-square Test B. Chi-square Test with Yates correction C. Student's t-test D. Fisher’s Exact Test E. Mann-Whitney Test |
D
Non-parametric, sample size <50, 2x2 table |
|
|
29. You are assessing the circulation of a patient using a pulmonary artery catheter. The mean arterial blood pressure is 100 mmHg, CVP is 5 mmHg. The pulmonary capillary wedge pressure is 15 mmHg and the cardiac output is 5 L.min-1. In this patient the systemic vascular resistance (in dynes.sec.cm-5) is
A. 3.2 B. 3.8 C. 150 D. 1280 E. 1520 |
E
SVR = (MAP-CVP)/CO x 80 |
|
|
28. When working with surgical lasers
A. the eyes can be protected from YAG laser emission by ordinary glasses with side shields B. the reflected laser beam is safe to view C. the emission from the CO2 laser is invisible D. protective eyewear is needed for all Class 1 lasers |
C
Wiki – Laser Safety: A Class 1 laser is safe under all conditions of normal use |
|
|
27. With respect to latex allergy
A. immediate IgE mediated hypersensitivity is thought to be due to polysaccharides retained within finished latex products B. it is possible to distinguish between contact dermatitis and IgE mediated hypersensitivity on the basis of history C. no further testing is required if a latex RAST or EAST (enzyme linked) test is positive D. intradermal tests are used to make a diagnosis, because anaphylaxis has been reported with skin prick testing E. less than 5% of atopic health workers are likely to skin test positive to latex |
C
RAST is highly specific. B sounds correct also, but perhaps the broad range of ways in which type I hypersensitivity presents means history won’t always be able to differentiate |
|
|
26. Non-steroidal anti-inflammatory drugs (NSAIDs) are NOT
A. known to cause reversible renal impairment B. known to cause a clinically significant increase in average operative blood loss C. recognised as a cause of renal papillary necrosis D. known to induce life-threatening asthma in atopic patients with aspirin sensitivity |
B
Not clear – significant blood loss rare, so maybe B. Apparently does cause papillary necrosis |
|
|
25. A male with stable angina treated with atenolol (a beta blocker) is
scheduled for a semi-elective bowel resection. The most appropriate postoperative management of his coronary artery disease would be to A. re-commence his oral atenolol once he is tolerating oral intake, if he has no angina before this time B. use a parenteral form of nitroglycerin until atenolol can be re-commenced orally C. use intravenous atenolol (at approximately 10% of the oral dose) until atenolol can be re-commenced orally D. use intravenous atenolol (at approximately 30% of the oral dose) until atenolol can be re-commenced orally E. monitor his ECG and re-commence his oral atenolol once he is tolerating oral intake, if he has no ST changes suggesting myocardial ischaemia before this time |
A
|
|
|
24. The risk of Hepatitis B infection after a needlestick injury from a Hepatitis
B E-Antigen positive patient is A. less than 1% B. 10% C. 20% D. 35% E. 50% |
D
Table 101-2 Miller HBsAg+/HBeAg+ Clinical hepatitis 22-31 Seroconversion 37-62 HBsAg+/HBeAg- Clinical hepatitis 1-6 Seroconversion 23-37 |
|
|
23. Desflurane
A. has a boiling point of 29.2º C at 1 atmosphere B. has a blood:gas partition coefficient higher than isoflurane C. has been reported as a triggering agent for malignant hyperthermia D. is associated with a low incidence of reflex airway responses when used for gaseous induction E. increases cerebral blood flow at 1 MAC |
C
|
|
|
22. The most appropriate strategy for the management of post-operative pain
following a remifentanil-propofol based anaesthetic for a patient undergoing a laparotomy is to A. cease the remifentanil infusion as wound closure commences, having given morphine intravenously 10 minutes earlier B. cease the remifentanil infusion once the wound is closed, having given morphine intravenously 20 minutes earlier C. cease the propofol 10 minutes prior to ceasing the remifentanil at the end of the case, and titrating intravenous morphine for analgesia on patient request D. continue intravenous remifentanil at a lower infusion rate in the recovery room and ceasing 30 minutes later E. give morphine intravenously at the same time as ceasing the remifentanil infusion in patients who have received neostigmine |
B
|
|
|
21 A patient with idiopathic hypertrophic subaortic stenosis becomes
hypotensive following induction of anaesthesia. An acceptable therapeutic regime would be A. calcium chloride by bolus injection B. isoprenaline by infusion C. dopamine by infusion D. nitroglycerine by infusion E. phenylephrine by bolus injection |
E
i.e. maintain DPP, don’t increase myocardial O2 demand |
|
|
20. In a patient who has a plasma tricyclic antidepressant level greater than
1000 ng.mL-1 the most likely E.C.G. finding is A. a prolonged PR interval B. deepened Q waves C. a prolonged QRS duration D. a prolonged ST segment E. the appearance of U waves |
C
|
|
|
19. With a back-pressure compensated ball flowmeter
A. a 25 degree tilt from vertical will cause an over-reading of approximately 50% B. increasing the outlet resistance will decrease the flow reading without affecting the flow C. the flow control spindle is on the inlet side of the float chamber D. accuracy of the reading is dependent on using a gas supply with the correct inlet pressure E. a leak in the outer chamber will NOT influence the accuracy of the flow reading |
D
|
|
|
18. Optimal conditions for accurate invasive blood pressure monitoring
include A. a large bore cannula, a system with a damping coefficient of 0.7 and a resonant frequency of 50 Hz B. wide bore tubing, a transducer with a frequency response range of 0 to 7 Hz, and a system with a resonant frequency of 3 Hz C. low compliance tubing, a system with a resonant frequency of 40 Hz and a damping coefficient of 1.0 D. high compliance tubing, a system with a resonant frequency of 10 Hz and a maximum phase lag E. a system with a minimum volume of fluid, a damping coefficient of 0.1 and a resonant frequency of 14 Hz |
A
Ideal specifications for IABP monitoring: Natural frequency of system > frequency of arterial waveform (which is 16-24Hz) A dampening coefficient of 0.6-0.7 is optimal. Minimise tubing length, eliminating stop cocks, removing air bubles and use low compliance tubing. Small catheters lower natural frequencies (bad), but improve underdampened systems and result in less complications |
|
|
17. The average expected depth of insertion of an oral endotracheal tube,
from the lip, in a normal newborn infant is A. 7.5 cm B. 8.5 cm C. 9.5 cm D. 10.5 cm E. 11.5 cm |
C
Paediatric advanced life support: Australian Resuscitation Council Guidelines 2006) in a newborn is 9.5 cm, 11.5 cm for a 6 months old infant 12 cm for a 1 year old. Thereafter, the approximate depth of oral insertion is given by the formula: age (years)/2 + 12 cm. Neonates: Weight in Kg + 6. So 3.5Kg = 9.5cm at lips |
|
|
16. A patient has suffered flash burns of the upper half of the left upper limb,
all of the left lower limb and the anterior surface of the abdomen. The approximate percentage of the body surface which has been burned is A. 18% B. 23% C. 32% D. 41% E. 48% |
C
Rule of 9’s: 4.5 + 18 + 9 |
|
|
15. In the management of drug-induced anaphylaxis
A. the first priority is the correction of diminished intra-vascular volume using intravenous colloid B. adrenaline is contra-indicated in the presence of a ventricular arrhythmia or the concurrent administration of halothane C. metaraminol is the treatment of choice for hypotension D. calcium is contra-indicated because of potential enhancement of mediator release E. lignocaine is the treatment of choice for arrhythmias |
D
|
|
|
14. In a patient being ventilated under general anaesthesia, end tidal CO2
monitoring would allow detection of all of the following EXCEPT A. circuit disconnection B. a malfunctioning inspiratory valve C. venous air embolism D. hypovolaemic shock E. endobronchial intubation |
E
|
|
|
13. A patient undergoing suprapubic prostatectomy appears to be bleeding
excessively. In an attempt to exclude primary hyperfibrinolysis as a possible cause the most useful test is A. plasma fibrinogen estimation B. euglobulin-lysis time C. whole blood clotting time D. prothrombin ratio E. clot retraction time |
B
Euglobin-lysis time measures fibrinolysis, the rest don’t |
|
|
12. In patients with portal hypertension undergoing surgery, laboratory
results associated with an increase in postoperative mortality include A. an elevated aPTT (activated partial thromboplastin time) B. a total bilirubin over 25 micromol.l-1 (normal range 3 - 17) C. a serum albumin less than 30 g.l-1 (normal range 35 - 50) D. an ALT (alanine transaminase) of 80 (normal range < 55) E. a serum albumin greater than 55 g.l-1 (normal range 35 - 50) |
C
C and D are both elements in Child-Pugh, but is this what the question is asking? |
|
|
11. Induced hypothermia to below 30o C
A. decreases blood viscosity B. decreases the transfer of oxygen from blood to the tissues C. decreases the solubility of oxygen in arterial blood D. produces systemic vasodilation E. will produce amnesia |
B
i.e. left shift in OHDC |
|
|
10. Complex regional pain syndrome Type 1 (Reflex Sympathetic Dystrophy)
can follow A. a high velocity injury to a nerve trunk B. a brachial plexus avulsion C. minor trauma D. all of the above |
C
See CEACCP article – Complex regional pain sysndrome CRPS I—symptoms preceded by tissue injury, most commonly limb trauma (absence of nerve injury) |
|
|
9. Following the intravenous injection of 1 mg.kg-1 of suxamethonium the
serum potassium concentration increase is A. typically 0.8 to 1.5 mmol.litre-1 in normal adults B. largely prevented by pretreatment with 0.04 mg.kg-1 of d-tubocurarine C. NOT exaggerated by renal failure D. higher in patients with atypical cholinesterase E. none of the above |
C
|
|
|
8. The most important factor in reducing peri-operative morbidity in
diabetic patients undergoing peripheral vascular surgery is A. tight control of blood sugar level in the peri-operative period B. frequent blood sugar level estimations C. use of regional rather than general anaesthesia D. stabilisation of co-existing disease E. the use of an insulin infusion rather than a subcutaneous sliding scale regimen |
D
|
|
|
7. Precautions when providing anaesthesia for surgery using a Nd-YAG
laser should include all of the following EXCEPT A. avoidance of nitrous oxide B. scavenging of smoke particles because they may contain viral DNA C. awareness that gas embolism is possible from cooling gas down laser conduit D. use of sunglasses to protect eyes E. avoidance of an FiO2 above 0.4 |
D
Miller: Anaesthesia for laser surgery Nd:YAG lasers require special green-tinted goggles, which make assessment of patient skin color difficult, or clear lenses (Nd:YAG Protection Glass; Surgical Laser Technologies, Malvern, PA), which have a special coating opaque to near infrared The role of the smoke plume as a viral vector is controversial. Viral DNA has been detected in plume from condylomas [18] [19] and skin warts,[20] but not from laryngeal papillomas.[21] Human immunodeficiency virus (HIV) was not detected in electrosurgical smoke plume[22] in one study, and only noninfectious DNA fragments were found in a CO2 laser plume from HIV-infected tissue pellets.[23] Competent transmission of any viral infection by a smoke plume has yet to be shown.[24] The laser plume does not seem to contain viable eukaryotic cells (i.e., tumor cells), [25] [26] but it may contain viable bacterial spores. [27] [28] CO2 lasers seem to produce the most smoke because of vaporization of tissue, and Nd:YAG contact probes produce much less |
|
|
6. Carbon dioxide is the most common gas used for insufflation for
laparoscopy because it A. is cheap and readily available true B. is slow to be absorbed from the peritoneum and thus safer false C. is not as dangerous as some other gases if inadvertently given intravenously true D. provides the best surgical conditions for vision and diathermy true E. will not produce any problems with gas emboli as it dissolves rapidly in blood false |
C
CEACCP - Laparoscopic abdominal surgery: “Carbon dioxide is used as the insufflation gas as it is non-flammable, colourless and has a higher blood solubility than air, thus reducing the risk of complications after venous embolism.” |
|
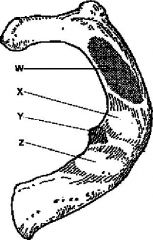
5. In this diagram of the superior surface of a first rib
A. label 'W' represents the insertion point of scalenus posterior B. label 'X' represents the groove for the subclavian vein C. a supraclavicular brachial plexus block needle is inserted posterior to the point labeled 'Y' D. label 'Z' represents the insertion point of scalenus anterior E. label 'W' represents the groove for the subclavian artery |
C
Anatomy for Anaesthetists, Page 300-301 |
|
|
4. The respiratory effects of morbid obesity include all of the following
EXCEPT A. hypoxaemia B. decrease in functional residual capacity C. decrease in residual volume D. an abnormal ventilation - perfusion ratio E. decrease in chest wall compliance |
C
See Can Respir J. 2006 May-Jun;13(4):203-10. Altered respiratory physiology in obesity |
|
|
3. The Visual Analogue Scale for assessment of post-operative pain
A. is considerably less reliable if the line is less than 50mm long B. is best used as a once-only measurement after the surgical procedure C. gives best results if the patient is instructed to make one clear mark parallel to the line D. should be used 60 minutes after each administration of an analgesic E. should have indicator marks at one quarter, one half and three quarters of the scale |
A
CEACCP Article – Measuring Pain – “Lines less than 100mm may be less accurate” |
|
|
2. In carbon monoxide poisoning
A. the severity of poisoning correlates well with carboxyhaemoglobin levels B. recovery occurring within 24 hours will be permanent C. toxicity is due solely to reduction in tissue oxygenation resulting from binding of carbon monoxide to haemoglobin False – “also disrupts oxidative metabolism, increases nitric oxide concentrations, causes brain lipid peroxidation, generates oxygen free radicals, and produces other metabolic changes that may result in neurologic and cardiac toxicity” D. cyanosis is a more common presentation than cherry-red discoloration E. pulse oximetry can be used to monitor patient recovery False – “pulse oximetry cannot distinguish carboxyhemoglobin from oxyhemoglobin. SpO2 values may, therefore, be quite misleading” |
D
Stoelting ACED – CO poisoning |
|
|
1. In a patient with porphyria, the drug most likely to cause an acute
episode is A. morphine B. propofol C. propanidid D. phenytoin E. atropine |
D
Miller chapter 35 – Metabolic Diseases “Drugs used in anesthetic management that are reported to be safe for patients with porphyria include neostigmine (Prostigmin), atropine, gallamine, succinylcholine, d-tubocurarine, pancuronium, nitrous oxide, procaine, propofol, propanidid, etomidate, meperidine, fentanyl, morphine, droperidol, promazine, promethazine, and chlorpromazine” “sensitizing drugs include barbiturates, meprobamate, chlordiazepoxide, glutethimide, diazepam, hydroxydione, phenytoin, imipramine, pentazocine, birth control pills, ethyl alcohol, sulfonamides, griseofulvin, and ergotamine” See also table 13-11 in Stoelting ACED |

