![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
179 Cards in this Set
- Front
- Back
|
Trpanosoma
Species: (1) Cruzi (2) Rangeli It is called a Chagoma (Romana's Sign) & is a sign of a bite from a reduviid. The reduviids like to feed at night near the eyes and mouth. and carry the parasite. The parasite is passed into the person by fecal matter left by the insect & rubbed into a wound or mucus membrane. |

What parasitic infection are these images a sign of?
|
|
|
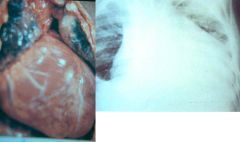
Trypanosoma cruzi (protozoa). Chronic infection by trypanosoma cruzi can cause cardiomegaly through the destruction of myocardial fibers & ganglion cells. At these stages of the disease there is no cure, only supportive therapy.
|
What parasitic infection are these images a sign of?
|
|
|
Trypanosoma cruzi (protozoa). Chronic infection by trypanosoma cruzi can cause apical aneurysms through the destruction of myocardial fibers & ganglion cells. At these stages of the disease there is no cure, only supportive therapy.
|

What parasitic infection is this image a sign of?
|
|
|
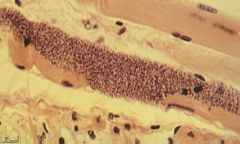
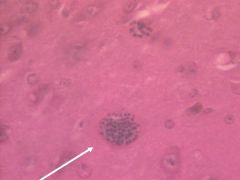
Trypanosoma Cruzi (Amastigote) in muscle.
Symptoms: Acute (4-8w): Bites near eye & mouth causing legions called Chagoma (Romana's Sign) that last for months, Fever, Progressive anemia, Edema, Lympadenopathy, Hepatosplenomegaly, EKG abnormalities, CNS involvement, Degeneration of parasitized tissue. Intermediate: Asymptomatic Chronic (Fatal): Chronic (Fatal): Fever, Constipation & Abdominal Distension (Myenteric plexus destruction), EKG abnormalities, Cardiomegaly & apical aneurysms (Destruction of myocardial fibers & ganglion cells), Pain. |
What parasite is this?
Symptoms? |
|
|
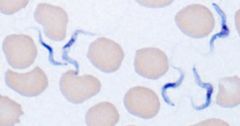
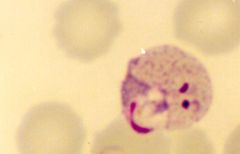
Trypanosoma Cruzi (Trypomastigote) in blood.
Hosts: Possum, Armadillo, Rodents, Humans Location: South & Central America Transfer: Reduviid Bugs (blood suckers): Triatomids, Rhodnius, Panstrongylus. Night feeders. Xfer by feces enter mucus membrane or wound. Verticle transmission. Life cycle: Reduviid (multiplies)-> Enters host-> Trypomastigote in blood-> Amastigote (multiplies) in muscle & nerve-> Trypomastigote in blood. Diagnosis: Thin smear, Thick smear, Fresh smear, Xenodiagnosis (Trypomastigote levels not high in blood, multiplies in bug as well). Symptoms & Pathology? Treatment: Benzimidazole & Nifurtimox (Older drug): Both treat all symptoms including neuroligical ones. Control: Education, Improve housing, Vector control, Screening of blood donors. |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Treatment? Control? Treatment? |
|
|
Trypanosoma cruzi (protozoa). Chronic infection by trypanosoma cruzi can cause megacolon through the destruction of the myenteric plexuses in the gut. At these stages of the disease there is no cure, only supportive therapy.
|

What parasitic infection are these images a sign of?
|
|
|
Trypanosoma (Trypomastigote) in blood.
Species: (1) Brucei Gambiense: Brain (Melarsopral), Everywhere else (Suramin) (2) Brucei Rhodiense: Brain (Melarsopral), Everywhere else (Suramin) (3) Rangeli: Asymptomatic (Benzimidazole[New] or Nifurtimox[Old]) |

What parasite is this?
Treatment? |
|
|
Trypanosoma (Trypomastigote) in blood.
Species: (1) Brucei Gambiense: Riverine Tsetse flies: Through saliva. Feed during day. Bite behind ears is extremely painful. Verticle transmission. (2) Brucei Rhodiense: Savannah Tsetse flies: Through saliva. Feed during day. Bite behind ears is extremely painful. Verticle transmission. (3) Rangeli: Reduviid Bugs (blood suckers): Triatomids, Rhodnius, Panstrongylus. Night feeders. Xfer by feces enter mucus membrane or wound. Verticle transmission. |

What parasite is this?
Transfer? |
|
|
Trypanosoma (Trypomastigote) in blood.
Species: (1) Brucei Gambiense. Hosts: Humans & Pigs main resevoirs of infection Location: West Africa (2) Brucei Rhodiense. Hosts: Gaming & Domestic animals, Humans Location: East & central Africa (3) Rangeli. Hosts: Possum, Armadillo, Rodents, Humans Location: South & Central America |
What parasite is this?
Hosts? Location? |
|
|
Trypanosoma brucei.
Species: (1) Gambiense: Riverine tsetse fly (2) Rhodiense: Savannah tsetse fly It is the Tsetse fly & feeds during the day. It's bite is very painful and normally behind the ears. |

What parasite does this insect transfer & what is it called?
|
|
|
Trypanosoma brucei.
Species: (1) Gambiense (2) Rhodiense Top picture: Trypanosoamil chancre from bite of Tstse fly. Bottom picture: Enlarged cervical lymph nodes (Winterbottom's Sign). Life cycle: All stages occur in the blood. Diagnosis: Thin smear, Thick smear, Aspirated gland juice, CSF (Centrifuged deposit), PCR/DNA. Treatment: Intravenous Suramin (Removes tryps everywhere but CNS), Melarsoprol (CNS treatment). Control: Aerial, ground, & cattle insectiside. Biconical trap for fly. |

What parasitic infection are these images a sign of?
Life cycle? Diagnosis? Treatment? Control? |
|
|
Leishmania.
Species: (1) Donavani (2) Braziliensis (3) Guyanesis (4) Tropica (5) Major It is a sand fly that lives in dry climates & is called Lutzomyia in the new world and Phlebotomus in the old world. It likes to bite at dusk and dawn, does not need water to breed, and lives in termite hills. |

What parasite does this insect transfer & what is it called?
|
|
|
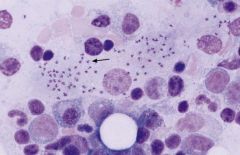
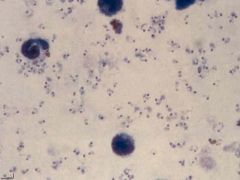
Leishmania (Amastigote) in white blood cells (macrophages) of a bone marrow aspirate.
(1) Donavani: Canids (dogs, etc.), Rodents (rarely), Humans. (2) Braziliensis: Dogs (main reservoir), Humans. (3) Guyanesis: Sloths & Rodents (main reservoir), Humans. (4) Tropica: Canids (dogs, etc.), Rodents (rarely), Humans. (5) Major: Canids (dogs, etc.), Rodents (rarely), Humans. |
What parasite is this?
Hosts? |
|
|
Leishmania (Amastigote) that has invaded white blood cells (macrophages).
Species: (1) Donavani: East India, Africa, South Europe, South & Central America. (2) Braziliensis: South & Central America. (3) Guyanesis: South & Central America. (4) Tropica: East India, Africa, Southern Europe. (5) Major: East India, Africa, Southern Europe. Treatment: Pentavalent antimonials by IV - Pentostam (old) or Amphiteracin B (new & better but expensive). |

What parasite is this?
Location? Treatment? |
|
|
Leishamani (small cutaneous ulcers)
Species: (1) Braziliensis (2) Guyanesis They are small cutaneous ulcers that healed after a few months. Even though these ulcers have healed in 3-20 years the parasite will cause large disfiguring mucocutaneous lesions (usually around the nose & mouth) that are known as Espunda or Uta. |

What parasitic infection are these images a sign of?
|
|
|
Leishmania tropica (Dry ulcers).
Life cycle: Amastigote in skin macrophages (WBC's). Promastigote in saliva of the fly. Multiplies in vector & host. Diagnosis: History, Amastigotes in fluid aspirated (culture) from below ulcer, Serological (limited value). Symptoms: Small red papule that ulcerates after 2-4 months. Dry ulcer that will heal in 2-3 months in immunocompetent individuals. |

What parasitic infection are these images a sign of?
Life cycle? Diagnosis? Symptoms? |
|
|
Leishamani (mucocutaneous lesions)
Species: (1) Braziliensis (2) Guyanesis Life cycle: Amastigote in skin macrophages (WBC's). Promastigote in saliva of the fly. Multiplies in vector & host. Diagnosis: (Direct Only) Amastigotes in legions, Culture/lab animals. Symptoms: Small cutaneous papule. Ulcerates & heals after few months. After 3-20 years, destructive oral &/or nasal legions (Espunda or Uta [mucocutaneous leishmaniasis]). |

What parasitic infection are these images a sign of?
Life cycle? Diagnosis? Symptoms? |
|
|
Leishmaniasis (Promastigote) in saliva of the sand fly.
Species: (1) donavani: East India, Africa, South Europe, South & Central America (2) braziliensis: South & Central America (3) guyanesis: South & Central America (4) tropica: East India, Africa, South Europe (5) major: East India, Africa, South Europe |

What parasite is this?
Location? |
|
|
Leishamani (mucocutaneous lesions)
Species: (1) Braziliensis (2) Guyanesis Life cycle: Amastigote in skin macrophages (WBC's). Promastigote in saliva of the fly. Multiplies in vector & host. Diagnosis: (Direct Only) Amastigotes in legions, Culture/lab animals. Symptoms: Small cutaneous papule. Ulcerates & heals after few months. After 3-20 years, destructive oral &/or nasal legions (Espunda or Uta [mucocutaneous leishmaniasis]). |

What parasitic infection are these images a sign of?
Life cycle? Diagnosis? Symptoms? |
|
|
Leishmania tropica (Large noticable scars from healed dry ulcers).
Life cycle: Amastigote in skin macrophages (WBC's). Promastigote in saliva of the fly. Multiplies in vector & host. Diagnosis: History, Amastigotes in fluid aspirated (culture) from below ulcer, Serological (limited value). Symptoms: Small red papule that ulcerates after 2-4 months. Dry ulcer that will heal in 2-3 months in immunocompetent individuals. |

What parasitic infection are these images a sign of?
Life cycle? Diagnosis? Symptoms? |
|
|
Leishmania major (serous ulcer).
Life cycle: Amastigote in skin macrophages (WBC's). Promastigote in saliva of the fly. Multiplies in vector & host. Diagnosis: History, Amastigotes in fluid aspirated (culture) from below ulcer, Serological (limited value). Symptoms: Small red papule that ulcerates after 2 weeks. Produces serous exudate. Heals on its own in immunocompetent individuals. |

What parasitic infection is this image a sign of?
Life cycle? Diagnosis? Symptoms? |
|
|
Leishmania donavani.
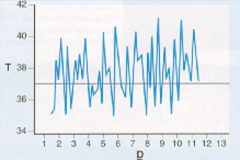
Life cycle: Amastigote in visceral WBC's 4-6 days after infection. Promastigote in saliva of the fly. Multiplies in vector & host. Diagnosis: Amastigotes in marrow/spleen smears, Culture of aspirates / blood taken during febrile period, Xenodiagnosis, Serology. Symptoms: Early: Irregular fever (double daily peak), Anemia, Leucopenia, Diarrhea, Bleeding gums, Joint pain, Weight Loss. Late: Enlarged lymph nodes, Splenomegaly, Hepatomegaly. Infection reappears after treatment in immunocompromised individuals. |
What parasitic infection is this image a sign of?
Life cycle? Diagnosis? Symptoms? |
|
|
Trichomonas vaginalis.
Hosts: Humans Location: Worldwide Transfer: Sexual intercourse Life cycle: Binary fission in: female-Vagina. male-Urethra, Epididymis, & Prostate. No protective stage. Diagnosis: Trophozoites in urine or vaginal discharge smears. Symptoms: Males: Asymptomatic. Females: Vaginitis, burning sensation, thick yellow discharge, vulvar &/or vaginal erythema. Treatment: Metronidazole (Flagly) - Sexual partners treated simultaneously. |
What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
Trichomonas vaginalis.
Hosts: Humans Location: Worldwide Transfer: Sexual intercourse Life cycle: Binary fission in: female-Vagina. male-Urethra, Epididymis, & Prostate. No protective stage. Diagnosis: Trophozoites in urine or vaginal discharge smears. Symptoms: Males: Asymptomatic. Females: Vaginitis, burning sensation, thick yellow discharge, vulvar &/or vaginal erythema. Treatment: Metronidazole (Flagly) - Sexual partners treated simultaneously. |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
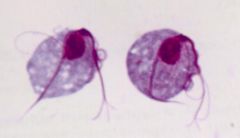
Giardia (trophozoite) not infective.
Hosts: Humans, Dogs, Cattle, Sheep, Wild mammals e.g. Beavers. Location: Worldwide Transfer: Ingestion of cysts. Trophozoites passed in diarrhea uninfective. Cysts passed in dry stools are immediately infective. Life cycle: Trophozoites divides & lives in the intestines & sloughs off in feces in bursts. Diagnosis difficult because stool sample may not contain parasite. Diagnosis: Symptoms, Stool microscopy, ELISA, Immunofluorescent (good but expensive), Therapeutic trial Symptoms: Any or All: Pale, loose, foul smelling, & fatty stools. Diarrhea 3-8 x daily. Abdominal distension. Offensive flatulence. Abdominal pain. Weight loss - anorexia. Sulphorous belching. Lasts for few days to several weeks. Treatment: Metronidazole (Flagyl). |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
Giardia (trophozoite) not infective.
Hosts: Humans, Dogs, Cattle, Sheep, Wild mammals e.g. Beavers. Location: Worldwide Transfer: Ingestion of cysts. Trophozoites passed in diarrhea uninfective. Cysts passed in dry stools are immediately infective. Life cycle: Trophozoites divides & lives in the intestines & sloughs off in feces in bursts. Diagnosis difficult because stool sample may not contain parasite. Diagnosis: Symptoms, Stool microscopy, ELISA, Immunofluorescent (good but expensive), Therapeutic trial Symptoms: Any or All: Pale, loose, foul smelling, & fatty stools. Diarrhea 3-8 x daily. Abdominal distension. Offensive flatulence. Abdominal pain. Weight loss - anorexia. Sulphorous belching. Lasts for few days to several weeks. Treatment: Metronidazole (Flagyl). |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
Giardia (trophozoite) not infective.
Hosts: Humans, Dogs, Cattle, Sheep, Wild mammals e.g. Beavers. Location: Worldwide Transfer: Ingestion of cysts. Trophozoites passed in diarrhea uninfective. Cysts passed in dry stools are immediately infective. Life cycle: Trophozoites divides & lives in the intestines & sloughs off in feces in bursts. Diagnosis difficult because stool sample may not contain parasite. Diagnosis: Symptoms, Stool microscopy, ELISA, Immunofluorescent (good but expensive), Therapeutic trial Symptoms: Any or All: Pale, loose, foul smelling, & fatty stools. Diarrhea 3-8 x daily. Abdominal distension. Offensive flatulence. Abdominal pain. Weight loss - anorexia. Sulphorous belching. Lasts for few days to several weeks. Treatment: Metronidazole (Flagyl). |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
Giardia (cystic form) immediately infective through ingestion.
|

What parasite is this?
|
|
|
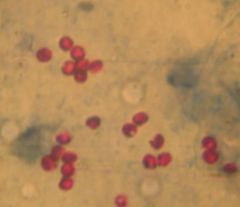
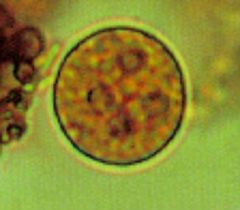
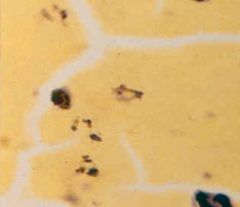
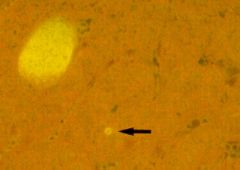
Cryptosporidium parvum (cystic form) in stool with modified Ziehl-Neelsen stain.
Hosts: Turkey, calf, lamb, kid, deer, foal, puppy, kitten, human. Location: Worldwide Transfer: Water, Food. Not killed by chlorine. Oocysts immediately infective by ingestion. Life cycle: Invades gut enterozytes (brush border of intestine). Release oocyst in feces with 4 sporozoites each. Diagnosis: Oocysts in stool (mod Ziehl-Neelsen stain), ELISA, Immunoflourescencse, Intestinal biopsy. Treatment: Don't use anti-diarrheal b/c prolongs infection. Fluid & electrolyte loss treatment. |
What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Treatment? |
|
|
Cryptosporidium parvum (cystic form) in stool with modified Ziehl-Neelsen stain.
Hosts: Turkey, calf, lamb, kid, deer, foal, puppy, kitten, human. Location: Worldwide Transfer: Water, Food. Not killed by chlorine. Oocysts immediately infective by ingestion. Life cycle: Invades gut enterozytes (brush border of intestine). Release oocyst in feces with 4 sporozoites each. Diagnosis: Oocysts in stool (mod Ziehl-Neelsen stain), ELISA, Immunoflourescencse, Intestinal biopsy. Treatment: Don't use anti-diarrheal b/c prolongs infection. Fluid & electrolyte loss treatment. |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Treatment? |
|
|
Cryptosporidium parvum (cystic form) in stool with modified Ziehl-Neelsen stain.
Symptoms: 1-2 weeks after exposure: Explosive, watery diarrhea that is brown-green in color. Frequency 2-10 x day for 3-10 days, complete recovery. Immunocompromised: Chronic diarrhea, Abdominal pain, Fever, Lymphadenopathy, Weight loss, Malnutrition, Villous atrophy. |
What parasite is this?
Symptoms? |
|
|
Cryptosporidium parvum (cystic form) in stool with modified Ziehl-Neelsen stain.
Symptoms: 1-2 weeks after exposure: Explosive, watery diarrhea that is brown-green in color. Frequency 2-10 x day for 3-10 days, complete recovery. Immunocompromised: Chronic diarrhea, Abdominal pain, Fever, Lymphadenopathy, Weight loss, Malnutrition, Villous atrophy. |

What parasite is this?
Symptoms? |
|
|
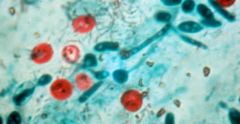
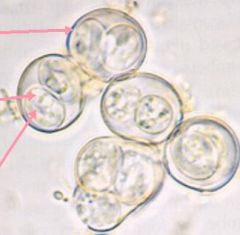
Entamoeba histolytica (cystic form) in a stool sample. Notice that 4 nuclei is characteristic of the cystic form of this parasite.
Hosts: Humans ONLY (not zoonosis) Location: Worldwide Transfer: Trophozoites passed in diarrhea uninfective. Cysts passed in dry stools are immediately infective by ingestion. |
What parasite is this?
Hosts? Location? Transfer? |
|
|
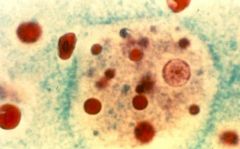
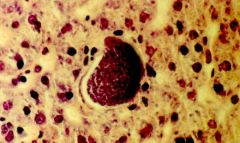
Entamoeba histolytica (invasive form, only 5% of cases). Parasite leaves the gut and invades other tissue (cardiac in this picture).
(1) Noninvasive Life cycle: Trophozoites live in lumen of large intestine. Diagnosis: Cysts in stool. Symptoms: 95% asymptomatic, Diarrhea, Flatulence, Abdominal pain, Blood & mucus in stool, Tear drop ulcers in gut. Treatment: Metronidazole (Flagyl). Fluid & electrolyte loss treatment. (2) Invasive Life cycle: Invasive: Trophozoites in RBC's, Liver, & Other organs. Diagnosis: Trophozoites in RBC's, ELISA (expensive), Aspiration, Ultrasound (liver cyst), X-ray/CT/MRI (brain & lung cyst). Symptoms: Cysts in Liver (majority), Brain, Skin, Lungs, Orbit, Spleen, Genitals -> Fever, Tender liver (pain), Hepatomegaly. Treatment: Metronidazole (Flagyl). Ultrasound guided drainage of cysts may be necessary. |
What parasite is this?
Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
Entamoeba histolytica (invasive form, only 5% of cases). Parasite leaves the gut and invades other tissue. Its is a radiograph of amoebic liver abscesses.
|
What parasitic infection is this image a sign of?
|
|
|
Toxoplasma gondii (Tachyzoites) in leukocytes. They are rapidly proliferating and are transported to all organs. This form of the parasite is responsible for vertical transmission from mother to fetus and is found in raw milk. It is infective. Consuming this form of the parasite in raw milk represents the least common mean of infection.
Hosts: Definative: Cats. Intermediate: Lamb, Goat, Pork, Chicken, Rodents. |

What parasite is this?
Hosts? |
|
|
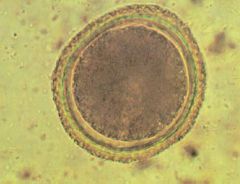
Toxoplasma gondii (Sporulated oocyst) from cat feces. This form IS infective and took 1-5 days in the environment to develop into a sporulated cyst after it had been released. The unsporulated cyst was not infective. These represent the second most frequent means of infection.
Location: Worldwide Life cycle: Cats ingest cysts (bradyzoites)-> Trophozoites-> Schizogonous & gametogonous development-> Oocysts (3-10dy)-> Unsporulated oocysts shed for 1-3wk-> Sporulate after 1-5dy in environment. Diagnosis: IgG, IgM serology. Imaging for ocular toxoplasmosis or toxoplasmic encephalitis, Isolation of parasites, Tissue biopsy. |
What parasite is this?
Symptoms? |
|
|
Toxoplasma gondii (Unsporulated oocyst) in cat feces. This form is NOT infective and takes 1-5 days to develop into a sporulated cyst after it has been released into the environment in the cat's feces. The sporulated cyst IS infective. These represent the second most frequent means of infection.
Location: Worldwide Life cycle: Cats ingest cysts (bradyzoites)-> Trophozoites-> Schizogonous & gametogonous development-> Oocysts (3-10dy)-> Unsporulated oocysts shed for 1-3wk-> Sporulate after 1-5dy in environment. Diagnosis: IgG, IgM serology. Imaging for ocular toxoplasmosis or toxoplasmic encephalitis, Isolation of parasites, Tissue biopsy. |

What parasite is this?
Location? Life cycle? Diagnosis? |
|
|
Toxoplasma gondii (Bradyzoites) in muscle tissue. There is no inflammation around the cysts and they parasite replicates slowly & indefinitely. This form of the parasite is acquired through consumption of undercooked meat containing the parasite. It is infective. Consuming this form of the parasite in meat is the most common mean of infection. Bradyzoites in our muscle can reactivate later in life.
Symptoms: Immunocompetent: Usually asymptomatic & get immunity (IgM during infection & IgG after). Immunocompromised: Invade all tissues but predeliction sites Eye (Chorioretinitis), Brain (Cysts, encephalitis: Headache, Disorientation, Coma). Fetus of recently newly infected mother: Severe: Chorioretinitis, Hydrocephalus (aqueduct block), Cerebral Necrosis, Liver failure. Less Severe: Poor cognitive skills, Jaundice, Anaemia, Convulsions, Growth retardation. Treatment: Spiramycin: Prevent verticle transmission to fetus & may be given after birth as well. TMP/SMX (Bactrim) Pyrimethamine w/ Dapsone: Prophylaxis for immunocompromised individuals. |
What parasite is this?
Symptoms? Treatment? |
|
|
Toxoplasma gondii. They are images of infants with hydrocephalus. It can occur in children who's mothers were infected with the parasite for the first time early in their pregnancy.
|

What parasitic infection are these images a sign of?
|
|
|
Toxoplasma gondii. Those are images of chorioretinitis & are indicative of an infection in an immunocompromised individual or a person who's mother was infected with the parasite for the first time early in her pregnancy.
|

What parasitic infection are these images a sign of?
|
|
|
Toxoplasma gondii. Those are images of chorioretinitis & are indicative of an infection in an immunocompromised individual or a person who's mother was infected with the parasite for the first time early in her pregnancy.
|
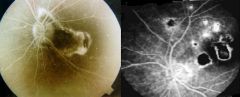
What parasitic infection are these images a sign of?
|
|
|
Toxoplasma gondii. It is an image of chorioretinitis & is indicative of an infection in an immunocompromised individual or a person who's mother was infected with the parasite for the first time early in her pregnancy.
|

What parasitic infection is this image a sign of?
|
|
|
Toxoplasma gondii. Those are images of chorioretinitis & are indicative of an infection in an immunocompromised individual or a person who's mother was infected with the parasite for the first time early in her pregnancy.
|
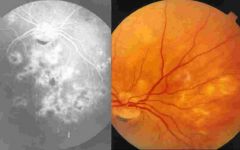
What parasitic infection are these images a sign of?
|
|
|
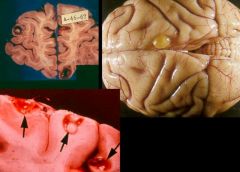
Toxoplasma gondii. It is picture of a brain with encephalitis and is indicative if an infection in an immunocompromised individual.
|
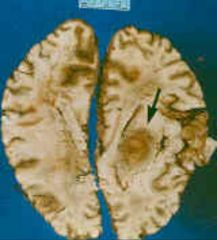
What parasitic infection is this image a sign of?
|
|
|
Toxoplasma gondii. They are pictures of a brain with encephalitis and are indicative if an infection in an immunocompromised individual.
|
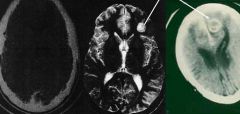
What parasitic infection are these images a sign of?
|
|
|
Plasmodium. This is a thick film with the red blood cells destroyed. The type of malaria cannot be discerned.
|
What parasite is this?
|
|
|
Plasmodium. This is a thick film with the red blood cells destroyed. The type of malaria cannot be discerned.
|
What parasite is this?
|
|
|
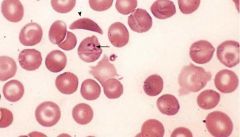
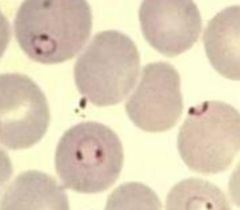
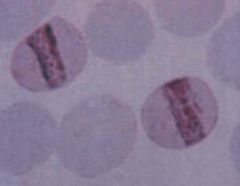
Plasmodium falciparum (Trophozoites) in sickle cell RBC's.
Notice: (1) Numerous fine ring forms (2) Double chromatin dots (3) Parasites are located near the border (margins) of the RBC (4) RBC's are not enlarged Pathogenesis: Haemolysis of RBC's. Parasite metabolites. Immune response. Cytoadherence (occlusion of capillaries-edema,organ failure) falciparum only. Cytokine increase. Malaria pigment production depletes iron stores increasing anemia. Symptoms: (looks like flu initially): Cold stage(15-60m): Mild, inappropriate cold-> leads to violent whole body shaking. Skin dry, pale, & cold. Pulse rapid & low-volume. Hot stage(2-6h): Fever. Skin flushed, dry & burining. Pulse rapid & bounding. Sweating stage(2-4h): Fever breaks. Profuse drenching sweat after patient may feel better. Can cause Diarrhea. Cerebral malaria (falciparum only): Coma, Convulsions, Abnormal posturing, Dysconjugate gaze, Retinal haemorrhages. |
What parasite is this?
Pathogenesis? Symptoms? |
|
|
Plasmodium falciparum (Trophozoites) in RBC's.
Notice: (1) Numerous fine ring forms (2) Double chromatin dots (3) Parasites are located near the border (margins) of the RBC (4) RBC's are not enlarged Treatment: Coartem, Artemether/lumefantrine. Quinine, Quinadine (IV form of Quinine): Used on chloroquine resistant strains only (reserve drug). Control: Prophylactic drugs: Mefloquine, Doxycycline, Chloroquine, Malarone, Pauladrine. Bed nets impregnated with residual insecticide. Protective clothes, Repellent (DEET). |
What parasite is this?
Treatment? Control? |
|
|
Plasmodium falciparum (Trophozoites) in RBC's.
Notice: (1) Numerous fine ring forms (2) Double chromatin dots (3) Parasites are located near the border (margins) of the RBC (4) RBC's are not enlarged Diagnosis: Thick blood (Malaria present? Sensitivity). Thin blood (Type? Specificity). Later regular fever pattern indicitave (not as regular in falciparum b/c of RBC schizont release range). |
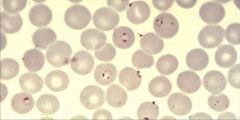
What parasite is this?
Diagnosis? |
|
|
Plasmodium falciparum (Trophozoites) in RBC's.
Notice: (1) Numerous fine ring forms (2) Double chromatin dots (3) Parasites are located near the border (margins) of the RBC (4) RBC's are not enlarged Hosts: Humans Location: Hot & wet climates. Predominant in Africa, New Guinea, & Haiti. Also present in South America & Asia. Transfer: Anopheline mosquito (saliva contains sporozoites) & feeds at night. Sporozoites in saliva mature from ingested gametocytes. Verticle transmission. Life cycle: Sporozoites ->Liver schizont(8d*40,000)->Merozites-> RBC's->Trophozoite ->RBC schizont(36-48h*8-32)->Merozites exit-> Gametocytes (mosq xfer) or Invade RBCs-> Gametocytes M&F fuse-> Zygote in mosq-> Ookinete-> Penetrate gut wall-> Oocyst-> Multiply-> Salivary gland-> Sporozoites (mosq 5d to mature). |

What parasite is this?
Hosts? Location? Transfer? Life cycle? |
|
|
Plasmodium falciparum (Gametocytes). Some merozites released from RBC's during lysis do not infect other RBC's but turn into Gametocytes to be picked up by other anopheline mosquitoes for transfer to other people.
Treatment: Coartem & Novartis (artemether/lumefantrine), Quinine, Quinadine Control: Prophylactic drugs: Mefloquine, Doxycycline, Chloroquine, Malarone, Pauladrine. Bed nets impregnated with residual insecticide. Protective clothes, Repellent (DEET). |

What parasite is this?
Treatment? Control? |
|
|
Plasmodium falciparum (schizonts adhered to endothelium of the brain). This is a picture of cerebral malaria & it can only be caused by plasmodium falciparum. Schizonts are adhered to endothelium of brain, which can cause:
(1) Coma (by definition) (2) Convulsions (3) Abnormal posturing (Decerebrate rigidity) (4) Dysconjugate gaze (5) Retinal haemorrhages It is clinically suspected when a patient with possible exposure to infection shows any reduction in consciousness. |

What parasite is this?
|
|
|
Plasmodium falciparum (schizonts adhered to endothelium of the brain). This is a picture of cerebral malaria & it can only be caused by plasmodium falciparum. Schizonts are adhered to endothelium of brain, which can cause:
(1) Coma (by definition) (2) Convulsions (3) Abnormal posturing (Decerebrate rigidity) (4) Dysconjugate gaze (5) Retinal haemorrhages It is clinically suspected when a patient with possible exposure to infection shows any reduction in consciousness. |
What parasite is this?
|
|
|
Top left: Coma (eyes open but unseeing)
Top right & bottom left: Decerebrate rigidity Bottom right: Dysconjugate gaze Plasmodium falciparum (cerebral malaria). These pictures indicate that schizonts of plasmodium falciparum are adhered to endothelium of brain, which can cause: (1) Coma (by definition) (2) Convulsions (3) Abnormal posturing (Decerebrate rigidity) (4) Dysconjugate gaze (5) Retinal haemorrhages It is clinically suspected when a patient with possible exposure to infection shows any reduction in consciousness. |

What parasitic infection are these images a sign of?
|
|
|
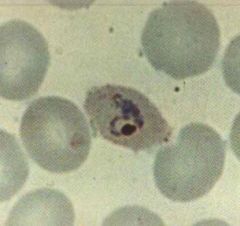
Plasmodium malariae (Trophozoites) in RBC's.
Notice: (1) Band shape (2) RBC not enlarged Hosts: Humans Location: Hot & wet climates. Replaces P. vivax in West africa because of people are resistant. Treatment: Chloroquine |
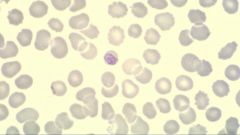
What parasite is this?
Hosts? Location? Treatment? |
|
|
Plasmodium malariae (Trophozoites) in RBC's.
Notice: (1) Band shape (2) RBC not enlarged Hosts: Humans Location: Hot & wet climates. Replaces P. vivax in West africa because of people are resistant. Treatment: Chloroquine |
What parasite is this?
Hosts? Location? Treatment? |
|
|
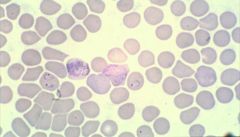
Plasmodium ovale (Trophozoites) in RBC's.
Notice: (1) "Oval" RBC (2) Enlarged RBC Hosts: Humans Location: Hot & wet climates. Widespread. Treatment: Chloroquine- Kills blood stages. Primaquine- Kills hypnozoites in liver preventing relapse & recurrence |
What parasite is this?
Hosts? Location? Treatment? |
|
|
Plasmodium ovale (Trophozoites) in RBC's.
Notice: (1) "Oval" RBC (2) Enlarged RBC Hosts: Humans Location: Hot & wet climates. Widespread. Treatment: Chloroquine- Kills blood stages. Primaquine- Kills hypnozoites in liver preventing relapse & recurrence |
What parasite is this?
Hosts? Location? Treatment? |
|
|
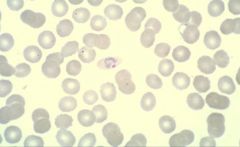
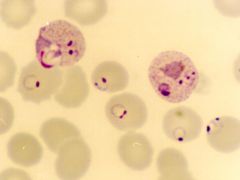
Plasmodium vivax (Trophozoites) in RBC's.
Notice: (1) Developing & thick (signet) ring forms (2) Enlarged RBC Hosts: Humans Location: Hot & wet climates. More common in S & C America, Asia. Treatment: Chloroquine- Kills blood stages. Primaquine- Kills hypnozoites in liver preventing relapse & recurrence |
What parasite is this?
Hosts? Location? Treatment? |
|
|
Plasmodium vivax (Trophozoites) in RBC's.
Notice: (1) Developing & thick (signet) ring forms (2) Enlarged RBC Hosts: Humans Location: Hot & wet climates. More common in S & C America, Asia. Treatment: Chloroquine- Kills blood stages. Primaquine- Kills hypnozoites in liver preventing relapse & recurrence |
What parasite is this?
Hosts? Location? Treatment? |
|
|
Plasmodium ovale or vivax (Hypnozoites) in the liver. If the malaria is treated and removed from the blood these hypnozoites remain dormant in the liver and may reactivate 20-30 years later. They are treated with Primaquine so that there is no recurrence of the malaria.
|
What parasite is this?
|
|
|
Plasmodium ovale or vivax (Hypnozoites) in the liver. If the malaria is treated and removed from the blood these hypnozoites remain dormant in the liver and may reactivate 20-30 years later. They are treated with Primaquine so that there is no recurrence of the malaria.
|
What parasite is this?
|
|
|
Plasmodium falciparum & Plasmodium vivax (trophozoites). Red blood cells are infected with BOTH types of malaria.
|
What parasite is this?
|
|
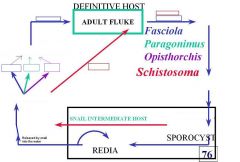
Fill in the blanks for the life cycle of the trematodes listed in this picture.
|
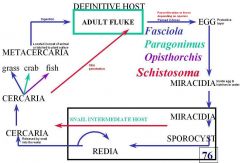
This is the answer.
|
|
|
Schistosoma mansonia (Trematoda) miracidia. The miracidia is the stage when the parasite emerges from the egg after it has entered water and infects the snail. All the schistosoma species go through this stage.
Notice: (1) Notice the tail is located laterally |

What parasite is this?
|
|
|
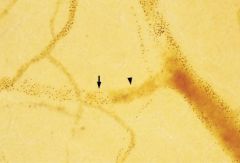
schistosoma (Trematoda) cercaria. The cercaria is the stage of the parasite which emerges from the snail and penetrates the skin of the definitive host.
Species: (1) Haematobium (passed in urine) (2) Mansoni (passed in feces) (3) Japonicum (passed in feces) |

What parasite is this?
|
|
|
Adult schistosoma (Trematoda) in the blood.
Species: (1) Haematobium: In urine (produced by sexual reproduction) (2) Mansoni: In feces (produced by sexual reproduction) (3) Japonicum: In feces (produced by sexual reproduction) |

What parasite is this & where does it leach?
How is it passed into the environment by the definitive host? |
|
|
Adult schistosoma (Trematoda) in the blood.
Species: (1) Haematobium: Humans only (2) Mansoni: Humans & Baboons (3) Japonicum: Humans, Oxen, Canines, Rodents Treatment: Praziquantel Control: Kill parasite to reduce morbidity & transmission, Kill snails (molluscicides), Prevent contamination, Protect from exposure. |

What parasite is this & where does it leach?
Definitive Hosts? Treatment? Control? |
|
|
Adult schistosoma (Trematoda) in the blood.
Species: (1) Haematobium: Africa, Middle East, India (2) Mansoni: Africa, Middle East, Easterb border of South America & Carribean (3) Japonicum: East Asia, Phillapines |

What parasite is this & where does it leach?
Location? |
|
|
Adult schistosoma (Trematoda) in the blood.
Species: (1) Haematobium: Bulinus (2) Mansoni: Biomphalaria (3) Japonicum: Oncomelania Intermediate hosts are all snails |

What parasite is this & where does it leach?
Intermediate hosts? |
|
|
Adult schistosoma (Trematoda) in the mesenteric veins.
Species: (1) Mansoni: Humans & Baboons (2) Japonicum: Humans, Oxen, Canines, Rodents |

What parasite is this & where does it leach?
Definitive hosts? |
|
|
Schistosoma haematobium is transferred by the Bulinus snail.
Symptoms: Clinical symptoms: Swimmer's itch (severe 0-3dy), Schistosomular pneumonitis (schisosomulae migration 3-10dy), Acute schisto or Katayama Fever (onset egg laying->immune complex syndrome 3-8wk w/ eosinophilia) Chronic syndromes: Hydronephrosis, Thickened bladder wall (> 5mm) & pollips (up chance bladder cancer), Occlusion of ureters, Haematuria --> Anemia. |

What parasite does this snail transfer & what is it called?
Symptoms? |
|
|
Schistosoma haematobium (Egg). It is transferred by the Bulinus (Snail).
Notice: (1) Tail is located at the end of the egg. Diagnosis: History, Eggs in urine, Cystoscopy, Gross haematuria (usual), Microhaematuria, Ultrasound-> morbidity assessment. |

What parasite is this?
Diagnosis? |
|
|
Top left: Normal bladder
Top right: Normal kidney Middle left: Polyp in bladder Middle right: Hydronephrosis Bottom left: Polyps in bladder and thickened bladder wall. Bottom right: Severe hydronephrosis Schistosoma haematobium infection can cause polyps and bladder wall thickening increasing the risk of bladder cancer. The damage to the kidneys and bladder are due to the release of eggs by the parasite. |
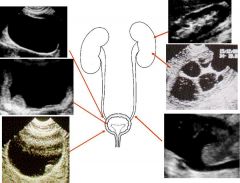
What parasitic infection are these images a sign of?
|
|
|
Schistosoma mansoni (Egg). It is transferred by the Biomphalaria (Snail).
Notice: (1) Notice the tail is located laterally Symptoms: Clinical symptoms: Swimmer's itch (severe 0-3dy), Schistosomular pneumonitis (schisosomulae migration 3-10dy), Acute schisto or Katayama Fever (onset egg laying->immune complex syndrome 3-8wk w/ eosinophilia). Chronic syndromes: (Trapped ova calcify in vessles)--> Portal hypertension, Hepatomegaly, Hematemesis (ruptured esophageal varices->anemia), Splenomegaly, Melania (blood in feces). |

What parasite is this?
Symptoms? |
|
|
Schistosoma mansoni is transferred by the Biomphalaria snail.
Diagnosis: History, Eggs in stool or in rectal biopsy, Rectoscopy & microscopy of rectal snip, Ultrasound-> morbidity assessment |

What parasite does this snail transfer & what is it called?
Diagnosis? |
|
|
Schistosoma japonicum (Egg). It is transferred by the Oncomelania (Snail).
Symptoms: Clinical symptoms: Swimmer's itch (severe 0-3dy), Schistosomular pneumonitis (schisosomulae migration 3-10dy), Acute schisto or Katayama Fever (onset egg laying->immune complex syndrome 3-8wk w/ eosinophilia). Chronic syndromes: (Trapped ova calcify in vessles)--> Portal hypertension, Hepatomegaly, Hematemesis (ruptured esophageal varices->anemia), Splenomegaly, Melania (blood in feces). |

What parasite is this?
Symptoms? |
|
|
Schistosoma japonicum is transferred by the Oncomelania snail.
Diagnosis: History, Eggs in stool or in rectal biopsy, Rectoscopy & microscopy of rectal snip, Ultrasound-> morbidity assessment |

What parasite does this snail transfer & what is it called?
Diagnosis? |
|
|
Fasciola (Trematoda) in the bile ducts.
Species: (1) Hepatica Definitive hosts: Humans, Sheep, Cattle Location: S America, Europe, Africa, Australia, New Zealand Diagnosis: Eggs in feces. Symptoms: Young flukes (damage liver): Severe headache, Backache, Chills, Fever. Adult flukes (cause atrophy of portal vessels, hemorrhage, secondary pathological conditions that may be lethal): Enlarged tender/cirrhotic liver, Diarrhea, Anemia -> Indicate advanced infection Treatment: Triclabendazole Control: Anthelmintics expel helminths from body |

What parasite is this & where does it leach?
Definitive hosts? Location? Diagnosis? Symptoms? Treatment? Control? |
|
|
Opisthorchis (Trematoda) in the bile ducts.
Species: (1) Sinensis Definitive hosts: Humans, Reptiles, Birds, Mammals incl. Dogs. Location: East Asia, Japan Diagnosis: Eggs in feces?????? Symptoms: Usually asymptomatic. Mechanical & toxic irritation of the bile ducts, especially with heavy infection (up to 6000 flukes). Can cause diarrhea. Treatment: Praziquantel |

What parasite is this & where does it leach?
Definitive hosts? Location? Diagnosis? Symptoms? Treatment? |
|
|
It is a radiograph of a bile duct obstruction by flukes. The species responsible may be one of the following:
(1) Opisthorchis sinensis (2) Fasciola hepatica |

What parasitic infection is this image a sign of?
|
|
|
Paragonimus (Trematoda) in the lungs.
Species: (1) Westermani Definitive hosts: Humans, Cats, Dogs Location: East Asia, Parts West Africa, South & Central America Diagnosis: Eggs in sputum or feces Symptoms: Cough, Blood stained sputum. Treatment: Praziquantel |

What parasite is this & where does it leach?
Definitive hosts? Location? Diagnosis? Symptoms? Treatment? |
|
|
Paragonimus (Trematoda) in the lungs.
Species: (1) Westermani Definitive hosts: Humans, Cats, Dogs Location: East Asia, Parts West Africa, South & Central America Diagnosis: Eggs in sputum or feces Symptoms: Cough, Blood stained sputum. Treatment: Praziquantel |

What parasite is this & where does it leach?
Definitive hosts? Location? Diagnosis? Symptoms? Treatment? |
|
|
It is indicative of a Paragonimus (Trematoda) infection in the lungs.
Species: (1) Westermani |

What parasitic infection is this image a sign of?
|
|
|
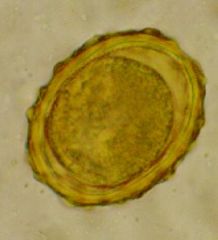
Taenia or Echinococcus (embryophore) which are Cestodes in the family Cyclophyllidea.
Notice: (1) Radially striated hardened shell (2) Inside the outer shell is the onocsphere Species: (1) Taenia saginata (2) Taenia solium (3) Echinococcus granulosus (4) Echinococcus multilocularis |

What parasite is this?
|
|
|
This is an oncosphere. It is an early larval stage of the following species that belong to cestodes in the family cyclophyllidea:
(1) Taenia (2) Echinococcus (3) Diplylidium |

What parasite is this?
|
|
|
This is one of the larval stages of Taenia (Cestode-cyclophyllidea) called a cysticerus.
Species: (1) Saginata (2) Solium |

What parasite is this?
|
|
|
This is a proglottid of Taenia (Cestode-cyclophyllidea).
Species: (1) Saginata (2) Solium |

What parasite is this?
|
|
|
Taenia (Cestode-Cyclophyllidea).
Species: (1) Solium (2) Saginata |

What parasite is this?
|
|
|
Taenia (Cestode-Cyclophyllidea).
Species: (1) Solium (2) saginata |
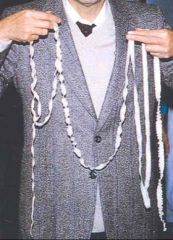
What parasite is this?
|
|
|
Taenia (Cestode-Cyclophyllidea).
Species: (1) Solium (2) Saginata |

What parasite is this?
|
|
|
Taenia saginata (Cestode-Cyclophyllidea).
Notice: (1) The scolex does NOT have an armed rostellum with a double row of hooks Hosts: Definitive: Humans Intermediate: Cows Location: Worldwide Transfer: Ingest cyst in beef-> Tapeworm (small intestine) Life cycle: Humans defacate proglottids-> Release embryophore-> Cow ingest-> Oncosphere released-> Cysticercus in cow muscle Diagnosis: Proglottids in feces. Symptoms: Usually asymptomatic but may be undesirable because proglottids released in feces & can also crawl out when not defecating. Treatment: Praziquantel. Control: Education, Sanitation, Treatment, Meat inspection, Proper cooking. |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? Control? |
|
|
Taenia saginata (Cestode-Cyclophyllidea) proglottid.
Notice: (1) The uterus of the proglottid Has MORE than 13 lateral branches Hosts: Definitive: Humans Intermediate: Cows Location: Worldwide Transfer: Ingest cyst in beef-> Tapeworm (small intestine) Life cycle: Humans defacate proglottids-> Release embryophore-> Cow ingest-> Oncosphere released-> Cysticercus in cow muscle Diagnosis: Proglottids in feces. Symptoms: Usually asymptomatic but may be undesirable because proglottids released in feces & can also crawl out when not defecating. Treatment: Praziquantel. Control: Education, Sanitation, Treatment, Meat inspection, Proper cooking. |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? Control? |
|
|
Taenia saginata (Cestode-Cyclophyllidea) proglottid.
Notice: (1) The uterus of the proglottid Has MORE than 13 lateral branches Hosts: Definitive: Humans Intermediate: Cows Location: Worldwide Transfer: Ingest cyst in beef-> Tapeworm (small intestine) Life cycle: Humans defacate proglottids-> Release embryophore-> Cow ingest-> Oncosphere released-> Cysticercus in cow muscle Diagnosis: Proglottids in feces. Symptoms: Usually asymptomatic but may be undesirable because proglottids released in feces & can also crawl out when not defecating. Treatment: Praziquantel. Control: Education, Sanitation, Treatment, Meat inspection, Proper cooking. |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? Control? |
|
|
Taenia saginata (Cestode-Cyclophyllidea).
Notice: (1) The scolex does NOT have an armed rostellum with a double row of hooks Hosts: Definitive: Humans Intermediate: Cows Location: Worldwide Transfer: Ingest cyst in beef-> Tapeworm (small intestine) Life cycle: Humans defacate proglottids-> Release embryophore-> Cow ingest-> Oncosphere released-> Cysticercus in cow muscle Diagnosis: Proglottids in feces. Symptoms: Usually asymptomatic but may be undesirable because proglottids released in feces & can also crawl out when not defecating. Treatment: Praziquantel. Control: Education, Sanitation, Treatment, Meat inspection, Proper cooking. |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? Control? |
|
|
Taenia solium (Cestode-Cyclophyllidea).
Notice: (1) The scolex does has an armed rostellum with a double row of hooks Hosts: Definitive: Humans Intermediate: Humans, Pigs Location: Worldwide Transfer: Ingest cyst in pork-> Tapeworm (small intestine). Ingest embryophore-> Cysticercosis with prediliction sites in the brain & eye. Life cycle: Humans defacate proglottids-> Release embryophore-> Pig ingest-> Oncosphere released-> Cysticercus in pig muscle Diagnosis: Proglottids in feces. Cysticercosis: Biopsy of sub Q nodules, calcified cysticercosis by x-ray & CAT scan, Serology. Symptoms: Usually asymptomatic but may be undesireable because proglottids released in feces and can also crawl out when not defacating. Embryophore ingestion can cause body wide cysts: Neurocysticercosis (Headache, Visual hallucinations, Seizures, Coma), Ocularcysticercosis. Treatment: Tapeworm: Niclosamide Cysticercosis: Albendizole (newer & kills less aggressively). Corticosteroids (reduce inflammation from dying parasite). Control: Education, Sanitation, Treatment, Meat inspection, Proper cooking. |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? Control? |
|
|
Taenia solium (Cestode-Cyclophyllidea)
Notice: (1) The scolex does has an armed rostellum with a double row of hooks Hosts: Definitive: Humans Intermediate: Humans, Pigs Location: Worldwide Transfer: Ingest cyst in pork-> Tapeworm (small intestine). Ingest embryophore-> Cysticercosis with prediliction sites in the brain & eye. Life cycle: Humans defacate proglottids-> Release embryophore-> Pig ingest-> Oncosphere released-> Cysticercus in pig muscle Diagnosis: Proglottids in feces. Cysticercosis: Biopsy of sub Q nodules, calcified cysticercosis by x-ray & CAT scan, Serology. Symptoms: Usually asymptomatic but may be undesireable because proglottids released in feces and can also crawl out when not defacating. Embryophore ingestion can cause body wide cysts: Neurocysticercosis (Headache, Visual hallucinations, Seizures, Coma), Ocularcysticercosis. Treatment: Tapeworm: Niclosamide Cysticercosis: Albendizole (newer & kills less aggressively). Corticosteroids (reduce inflammation from dying parasite). Control: Education, Sanitation, Treatment, Meat inspection, Proper cooking. |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? Control? |
|
|
Taenia solium (Cestode-Cyclophyllidea) Proglottid.
Notice: (1) The uterus of the proglottid Has LESS than 13 lateral branches Hosts: Definitive: Humans Intermediate: Humans, Pigs Location: Worldwide Transfer: Ingest cyst in pork-> Tapeworm (small intestine). Ingest embryophore-> Cysticercosis with prediliction sites in the brain & eye. Life cycle: Humans defacate proglottids-> Release embryophore-> Pig ingest-> Oncosphere released-> Cysticercus in pig muscle Diagnosis: Proglottids in feces. Cysticercosis: Biopsy of sub Q nodules, calcified cysticercosis by x-ray & CAT scan, Serology. Symptoms: Usually asymptomatic but may be undesireable because proglottids released in feces and can also crawl out when not defacating. Embryophore ingestion can cause body wide cysts: Neurocysticercosis (Headache, Visual hallucinations, Seizures, Coma), Ocularcysticercosis. Treatment: Tapeworm: Niclosamide Cysticercosis: Albendizole (newer & kills less aggressively). Corticosteroids (reduce inflammation from dying parasite). Control: Education, Sanitation, Treatment, Meat inspection, Proper cooking. |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? Control? |
|
|
Taenia solium (Cestode) infection. It has caused cysticercosis.
Transfer: Ingestion of embryophore Treatment: Albendizole (newer & kills less aggressively) & Corticosteroids (reduce inflammation from dying parasite) to treat the cysticercosis. |

What parasitic infection is this image a sign of?
Transfer? Treatment? |
|
|
Taenia solium (Cestode) infection. It has caused neurocysticercosis.
Transfer: Ingestion of embryophore Treatment: Albendizole (newer & kills less aggressively) & Corticosteroids (reduce inflammation from dying parasite) to treat the cysticercosis. |
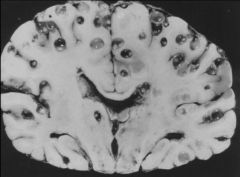
What parasitic infection is this image a sign of?
Transfer? Treatment? |
|
|
Taenia solium (Cestode) infection. It has caused neurocysticercosis..
Transfer: Ingestion of embryophore Treatment: Albendizole (newer & kills less aggressively) & Corticosteroids (reduce inflammation from dying parasite) to treat the cysticercosis. |
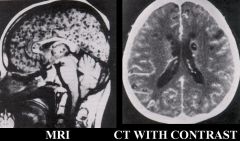
What parasitic infection are these images a sign of?
Transfer? Treatment? |
|
|
Taenia solium (Cestode) infection. It has caused neurocysticercosis..
Transfer: Ingestion of embryophore Treatment: Albendizole (newer & kills less aggressively) & Corticosteroids (reduce inflammation from dying parasite) to treat the cysticercosis. |
What parasitic infection are these images a sign of?
Transfer? Treatment? |
|
|
Diplylidium (Cestode - Cyclophyllidea) egg.
Species: (1) Caninum |
What parasite is this?
|
|
|
Diplylidium (Cestode - Cyclophyllidea) egg.
Species: (1) Caninum |
What parasite is this?
|
|
|
Diplylidium (Cestode-cyclophyllidea) one of the larval stages called a cysticercoid.
Species: (1) Caninum |
What parasite is this?
|
|
|
Diplylidium caninum.
Hosts: Definitive: Dogs, Humans. Intermediate: Fleas & Lice. Location: Worldwide Transfer: Humans infected by accidentally eating fleas from infected dogs. Life cycle: Tapeworm lives in small intestine Diagnosis: Proglottids in feces. Symptoms: Usually asymptomatic. May have: Abdominal pain, Diarrhia, Anal pruritis. Treatment: Niclosamide or Praziquantel |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
Echinococcus (tapeworm)
Species: (1) Granulosus- Intermediate hosts: Humans, wild herbivores (Esp. Sheep) (2) Multilocularis- Intermediate hosts: Humans, rodents Definitive Hosts: Dogs Location: Worldwide Transfer: Dog w/ tapeworm defacate egg-> Human/Animal eat egg-> Cysts-> Dogs eat cysts get tapeworm Life cycle: Definitive host: Lives in small intestine Intermediate host: Hydatid cysts in all organs w/ predilection sites in liver then lungs. Diagnosis: Ultrasound is gold standard for locating hydatid cysts, CT, MRI, X-ray. ELISA. Control: Education, Control dog population, Treat dogs, Meat inspection. |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Control? |
|
|
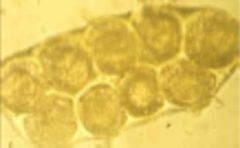
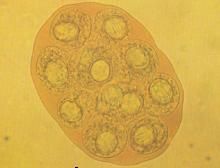
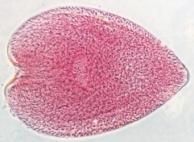
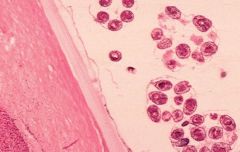
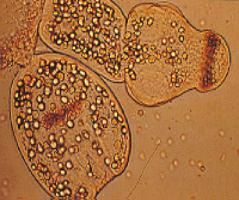
Echinococcus granulosus (Cestode) in the larval stage called a protoscolicies. This is a cross section of a hydatid cyst in a liver.
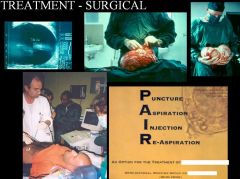
Symptoms: 85% of cases are subclinical. Can cause body wide cysts: Lung cysts (predilection): Symptomatic very quickly. Liver cysts (predilection): Symptoms longer to develop. Ocular Cystic Echinococcosis. Treatment: Surgical (not if cyst contact biliary tree): Puncture(cyst), Aspirate(parasites), Inject (alcohol), Reaspirate(fluid). Albendizole. |

What parasite is this?
Symptoms? Treatment? |
|
|
Echinococcus granulosus (Cestode) in the larval stage called a protoscolicies. This is a cross section of a hydatid cyst in a liver.
Symptoms: 85% of cases are subclinical. Can cause body wide cysts: Lung cysts (predilection): Symptomatic very quickly. Liver cysts (predilection): Symptoms longer to develop. Ocular Cystic Echinococcosis. Treatment: Surgical (not if cyst contact biliary tree): Puncture(cyst), Aspirate(parasites), Inject (alcohol), Reaspirate(fluid). Albendizole. |
What parasite is this?
Symptoms? Treatment? |
|
|
Echinococcus granulosus (Cestode) infection. This surgical procedure is used to excise the hydatic cysts caused by the parasite.
P - Puncture A - Aspirate (remove fluid from cyst) I - Inject (alcohol to disinfect) R - Reaspirate(remove fluid) This procedure can't be used on small secondary cysts or if the cyst is in contact with the biliary tree. The only treatment for those is Albendazole. |
What parasitic infection is being treated in the surgical procedure in the picture?
|
|
|
Echinococcus granulosus (Cestode) infection, which is also called "Cystic hytadid disease".
|

What parasitic infection are these images a sign of?
|
|
|
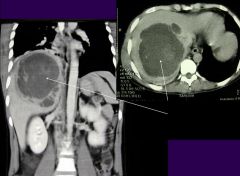
Echinococcus granulosus infection with hydatic cysts in the liver.
Notice: That the cysts are of different sizes. The larger cyst can be treated surgically while the smaller ones can't and must be treated with Albendizole. |

What parasitic infection is this image a sign of?
|
|
|
Infection by ecchinococcus granulosus. The larval stage of the parasite called protoscolicies have caused the formation of hydatid cysts in the liver & lung.
|

What parasitic infection is this image a sign of?
|
|
|
Echinococcus granulosus (Cestode)
|
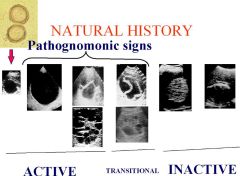
What parasitic infection are the pathognomonic signs in this picture a sign of?
|
|
|
Echinococcus granulosus infection with hydatic cysts in the lung.
|

What parasitic infection is this image a sign of?
|
|
|
Echinococcus multilocularis (Cestode) infection, which is also called "Alveolar Hydatid Disease". Infection results in inoperable hydatic cysts.
Symptoms: 85% of cases are subclinical. Can cause body wide cysts: Lung cysts (predilection): Symptomatic very quickly. Liver cysts (predilection): Symptoms longer to develop. Treatment: Albendazole for life |
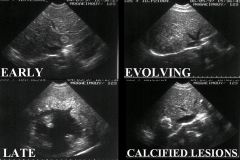
What parasitic infection is this progression of ultrasound images a sign of?
Symptoms? Treatment? |
|
|
Echinococcus multilocularis (Cestode) in the larval stage. This is a cross section of a hydatid cyst.
Symptoms: 85% of cases are subclinical. Can cause body wide cysts: Lung cysts (predilection): Symptomatic very quickly. Liver cysts (predilection): Symptoms longer to develop. Treatment: Albendizole for the life of the patient (surgery not an option because of the cyst size). |
What parasite is this?
Symptoms? Treatment? |
|
|
Diphylobothrium latum (Cestode)
Hosts: Definitive: Dogs, Cats, Bears, Humans. Intermediate: Fresh water flea->Fish Location: Worldwide, but major in north hemisphere near fresh water lakes. Transfer: Definitive host defecates eggs->fresh water flea->fresh water fish-> New host eats fish with parasite & develops tapeworm Life cycle: Adult worms live in small intestine. Diagnosis: Detection of eggs in feces Symptoms: May lead to megaloblastic anemia because tapeworm can outcompete the host for vitamin B12. Treatment: Praziquantel, Treat anemia. |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
It is the Cyclops fresh water flea & it transfers:
(1) Dracunculus medinensis (Nematode-Human Subcutaneous Filaria) "Guinea worm" (2) Diphyllobothrium latum (Cestode). The cyclops & other fresh water fleas with the disease are eaten by fish, which are then eaten by humans & other definitive hosts, which results in infection. |

What parasites are transfered by the creature in this picture & what is it called?
|
|
|
Diphyllobothrium latum (Cestode) can cause the megaloblastic anemia in the picture because the parasite outcompetes the host for vitamin B12. The lack of B12 leads to megologlastic anemia.
Treatment: Praziquantel, Treat anemia. |
What parasitic infection is this images a sign of?
Treatment: |
|
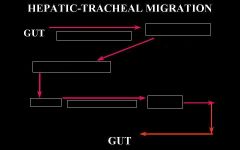
Fill in the blanks for the hepatic-tracheal migration of a nematode.
|
This is the answer.
|
|
|
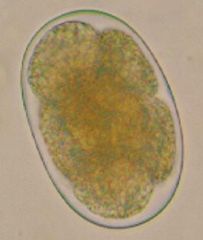
Hookworm (Nematoda) egg. This is the egg before L1 because the larva is out of the egg at the beginning of L1.
Species: (1) Ancylostoma duodenale (2) Necator americanus Transfer: Human defecates egg-> Larva leaves egg before L1-> L1-L2(24-36h)-> L2-L3(1w) infective-> Skin penetration Life cycle: L3 larva infective (out of egg). Undergoes hepatotracheal migration. Adults live in small intestine. |
What parasite is this?
|
|
|
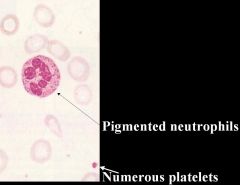
Hookworm (Nematoda)
Species: (1) Ancylostoma duodenale (2) Necator americanus Hosts: Humans Location: Worldwide but more concentrated in the tropics Transfer: Human defecates egg-> Larva leaves egg before L1-> L1-L2(24-36h)-> L2-L3(1w) infective-> Skin penetration Life cycle: L3 larva infective (out of egg). Undergoes hepatic tracheal migration. Adults live in small intestine. Diagnosis: Salt floatation (eggs). Symptoms: Skin penetration (Ground itch). Larval migration to lungs-> Mild pneumonitis. Suck blood in intestines-> Anemia (Tiredness, Edema, Myalgia, Pallor, Breathlessness). May cause iron deficiency anemia (Hypochromic, Microcytic, Pigmented neutrophils, Many platelets). Treatment: Albendazole: Kills worm. Treat anemia. Control: Education (hygiene), Sanitation, Treatment |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Treatment? Control? |
|
|
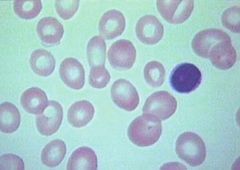
Hookworm (Nematoda) which can cause the microcytic anemia pictured because they can cause iron deficiency.
Species: (1) Ancylostoma duodenale (2) Necator americanus Notice: (a) Hypochromic (b) Microcytic (c) Pigmented neutrophils (d) Many platelets |
What parasitic infection is this image a sign of?
|
|
|
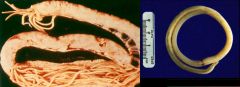
Hookworm (Nematoda)
Species (you don't need to differentiate b/t 2 species): (1) Ancylostoma duodenale (top 2 worms) (2) Necator americanus (bottom 2 worms) Hosts: Humans Location: Worldwide but more concentrated in the tropics Transfer: Human defecates egg-> Larva leaves egg before L1-> L1-L2(24-36h)-> L2-L3(1w) infective-> Skin penetration Life cycle: L3 larva infective (out of egg). Undergoes hepatic tracheal migration. Adults live in small intestine. Diagnosis: Salt floatation (eggs). Symptoms: Skin penetration (Ground itch). Larval migration to lungs-> Mild pneumonitis. Suck blood in intestines-> Anemia (Tiredness, Edema, Myalgia, Pallor, Breathlessness). May cause iron deficiency anemia (Hypochromic, Microcytic, Pigmented neutrophils, Many platelets). Treatment: Albendazole: Kills worm. Treat anemia. Control: Education (hygiene), Sanitation, Treatment |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Treatment? Control? |
|
|
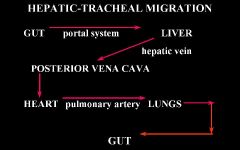
Ascaris lumbricoides (Nematoda) egg-L2. Larva is still within the egg. This IS the infective stage and infection occurs by ingestion of the egg.
Transfer: Human defecates egg-> L1-L2(3w) infective-> Ingestion of L2 larva still in egg. Life cycle: L2 larva infective (still in egg). Sexual repo. 200,000eggs/day. |

What parasite is this?
Transfer? Life cycle? |
|
|
Ascaris lumbricoides (Nematoda) egg-L1. Larva is still within the egg & is NOT infective.
Transfer: Human defecates egg-> L1-L2(3w) infective-> Ingestion of L2 larva still in egg. Life cycle: L2 larva infective (still in egg). Sexual repo. 200,000eggs/day. |
What parasite is this?
Transfer? Life cycle? |
|
|
Ascaris lumbricoides (Nematoda)
Host: Humans Location: Worldwide Transfer: Human defecates egg-> L1-L2(3w) infective-> Ingestion of L2 larva still in egg. Life cycle: L2 larva infective (still in egg). Sexual repo. 200,000eggs/day. Diagnosis: Salt flotation (eggs). Adult worms in diarrhea, out of mouth, nose, & ear. Symptoms: Loeffler's syndrome (pulmonary eosinophilia), Larvae fever, Cough, Wheeze, Rapidly changing X-ray picture. Adult worms: Biliary obstruction, Jaundice, Appendicitis, Pancreatitis, Asphyxia, Diarrhea. Treatment: Albendazole Control: Education (hygiene), Sanitation, Treatment |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? Control? |
|
|
Ascaris lumbricoides (Nematoda)
Host: Humans Location: Worldwide Transfer: Human defecates egg-> L1-L2(3w) infective-> Ingestion of L2 larva still in egg. Life cycle: L2 larva infective (still in egg). Sexual repo. 200,000eggs/day. Diagnosis: Salt flotation (eggs). Adult worms in diarrhea, out of mouth, nose, & ear. Symptoms: Loeffler's syndrome (pulmonary eosinophilia), Larvae fever, Cough, Wheeze, Rapidly changing X-ray picture. Adult worms: Biliary obstruction, Jaundice, Appendicitis, Pancreatitis, Asphyxia, Diarrhea. Treatment: Albendazole Control: Education (hygiene), Sanitation, Treatment |
What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? Control? |
|
|
Trichuris trichuria (Nematoda) egg in the L1 stage. It takes 2 weeks in the environment to mature before it is infective.
Transfer: Human defecates egg-> Maturation to L1(2w) infective-> Ingestion of L1 larva still in egg Life cycle: L1 larva is infective (still in egg). No HT migration. Adult lives in cecum. |

What parasite is this?
Transfer? Life cycle? |
|
|
Trichuris trichuria (Nematoda)
Host: Humans Location: Worldwide but mostly in tropics Transfer: Human defecates egg-> Maturation to L1(2w) infective-> Ingestion of L1 larva still in egg Life cycle: L1 larva is infective (still in egg). No HT migration. Adult lives in cecum. Diagnosis: Salt flotation (eggs). Symptoms: Most infections are asymptomatic. Heavy infection: Bloody diarrhea, Abdominal pain, Prolapse of the rectum, Anemia, Impaired growth, Reduced cognitive function. Treatment: Mebendazole Control: Education (hygiene), Sanitation, Treatment |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? Control? |
|
|
Trichuris trichuria (Nematoda)
Host: Humans Location: Worldwide but mostly in tropics Transfer: Human defecates egg-> Maturation to L1(2w) infective-> Ingestion of L1 larva still in egg Life cycle: L1 larva is infective (still in egg). No HT migration. Adult lives in cecum. Diagnosis: Salt flotation (eggs). Symptoms: Most infections are asymptomatic. Heavy infection: Bloody diarrhea, Abdominal pain, Prolapse of the rectum, Anemia, Impaired growth, Reduced cognitive function. Treatment: Mebendazole Control: Education (hygiene), Sanitation, Treatment |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? Control? |
|
|
Trichuris trichuria (Nematoda). It is a prolapsed rectum and is indicative of a HEAVY infection.
|

What parasitic infection is this images a sign of?
|
|
|
Strongyloides stercoralis (Nematoda)
Hosts: Humans & Dogs Location: Worldwide, but more in concentrated in tropics. Transfer: Human defecates L1 larva-> L3 infective-> Skin penetration. Autoinfection (can maintain > 30years). Life cycle: L3 larva infective. Undergoes hepatic tracheal migration. Sexual repo (does not follow 1 egg-> 1 adult rule for nematodes). Produce 5 eggs/day. Diagnosis: Stool microscopy & culture (female doesn't produce many larvae), ELISA, Eosinophilia, Larva currens. Symptoms: Early: Itchy eruption at site of penetration, Cough & wheeze, Upper abdominal pain & diarrhea, Weight loss, Larva currens. Established infection: Intestinal symptoms, Flattening of villi, Malabsorption, Smelly yellow stool, Diarrhea, Larva currens. Treatment: Thiabendazole Control: Difficult because it is a zoonosis. |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Treatment? Symptoms? Control? |
|
|
Strongyloides stercoralis (Nematoda). It is a larva current and is a raised wiggly line that comes & goes in a few hours, is very itchy and is confined to the trunk.
|

What parasitic infection is this image a sign of?
|
|
|
Ancylostoma (Nematoda). They are cutaneous larva migrans.
Species: (1) Caninum: Dog hookworm (Definitive hosts) (2) Braziliense: Cat hookworm (Definitive hosts) Intermediate hosts: Humans Location: Worldwide Transfer: Skin penetration by L3. Require humid & moist soil. Life cycle: L3 larva penetrate skin in humans but can't migrate any farther. Some make it to intestines but don't produce eggs. Diagnosis: Cutaneous larva migrans Symptoms: Cutaneous larva migrans (feet), Intense pruritis, Secondary infections, Eosinophilic enteritis when some L3 make it to intestines but they do not produce eggs. Treatment: Thiobendazlole |

What parasitic infection are these images a sign of?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
Ancylostoma (Nematoda). They are cutaneous larva migrans.
Species: (1) Caninum: Dog hookworm (Definitive hosts) (2) Braziliense: Cat hookworm (Definitive hosts) Intermediate hosts: Humans Location: Worldwide Transfer: Skin penetration by L3. Require humid & moist soil. Life cycle: L3 larva penetrate skin in humans but can't migrate any farther. Some make it to intestines but don't produce eggs. Diagnosis: Cutaneous larva migrans Symptoms: Cutaneous larva migrans (feet), Intense pruritis, Secondary infections, Eosinophilic enteritis when some L3 make it to intestines but they do not produce eggs. Treatment: Thiobendazlole |

What parasitic infection are these images a sign of?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
Ancylostoma (Nematoda). It is eosinophilic enteritis. In humans the parasite is not able to lay eggs if it does manage to migrate into the intestines.
Species: (1) Caninum: Dog hookworm (Definitive hosts) (2) Braziliense: Cat hookworm (Definitive hosts) |

What parasitic infection is this images a sign of?
|
|
|
Enterobius vermicularis (Nematoda)
Hosts: Humans Location: ?????? Transfer: Females lay eggs-> L1-L3(4-6h) infective-> Ingestion of L3 Life cycle: L3 larva infective. No HT migration. Adult lives in intestines. Female migrates to rectum to lays eggs & dies. Diagnosis: Itchy anus, especially @ night. Find eggs in stool (Graham slide). Symptoms: Itchy anus, especially at night. Treatment: Albnedazole |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
Enterobius vermicularis (Nematoda)
Hosts: Humans Location: ?????? Transfer: Females lay eggs-> L1-L3(4-6h) infective-> Ingestion of L3 Life cycle: L3 larva infective. No HT migration. Adult lives in intestines. Female migrates to rectum to lays eggs & dies. Diagnosis: Itchy anus, especially @ night. Find eggs in stool (Graham slide). Symptoms: Itchy anus, especially at night. Treatment: Albnedazole |
What is this parasite?What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
Enterobius vermicularis (Nematoda)
Hosts: Humans Location: ?????? Transfer: Females lay eggs-> L1-L3(4-6h) infective-> Ingestion of L3 Life cycle: L3 larva infective. No HT migration. Adult lives in intestines. Female migrates to rectum to lays eggs & dies. Diagnosis: Itchy anus, especially @ night. Find eggs in stool (Graham slide). Symptoms: Itchy anus, especially at night. Treatment: Albnedazole |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
Enterobius vermicularis (Nematoda) egg. The parasite is transfered by ingestion of the L3 larva. Development from L1-L3 only takes 4-6 hours.
|

What parasite is this?
|
|
|
Enterobius vermicularis (Nematoda) egg. The parasite is transfered by ingestion of the L3 larva. Development from L1-L3 only takes 4-6 hours.
|

What parasite is this?
|
|
|
Enterobius vermicularis (Nematoda) egg. The parasite is transfered by ingestion of the L3 larva. Development from L1-L3 only takes 4-6 hours.
|

What parasite is this?
|
|
|
Enterobius vermicularis (Nematoda)
|

What parasite is this?
|
|
|
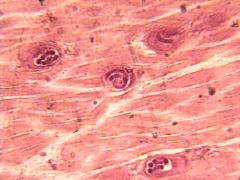
Trichinella (nematoda) L1 larva. The larva of the parasite lives in muscle.
Species: (1) Spiralis: North & South America, Europe (2) Nelsoni: Sub-saharan Africa (3) Nativa: Arctic circle |

What parasite is this?
Location? |
|
|
Trichinella (nematoda) L1 larva. The larva of the parasite lives in muscle.
Species: (1) Spiralis: Domestic pigs & horses, rodents (2) Nelsoni: Hyenas, warthogs, & other carnivores (3) Nativa: Polar bears, arctic foxes, bears |
What parasite is this?
Definitive hosts? |
|
|
Trichinella (Nematoda)
Species: (1) Spiralis: Domestic pigs & horses, Rats (Definitive hosts). N & S America, Europe (Location) (2) Nelsoni: Hyenas, warthogs, & other carnivores (Definitive hosts). Sub-saharan Africa (Location). (3) Nativa: Polar bears, arctic foxes, bears (Definitive hosts). Arctic circle (Location). Intermediate host: Humans Transfer: Ingestion of L1 larva in meat. Life cycle: L1 is infective stage. Larvae live in striated muscle. Adult lives in small intestine of definitive host. In humans a few larva mature to adulthood, many remain larva. Diagnosis: ELISA, Muscle biobsy (Microscopy or Rapid PCR) Symptoms: Enteric phase (usually mild): Nausea, Vomitting, Colic, Diarrhea, Sweating. Migratory (invasive) phase: Periorbital edema, Eosinophilia (large infection), Myalgia, Fever. Encystment Phase: Myalgia, Edema, Dehydration, Fever, (Usually subsides 2mo after infection), Eosinophilia (subsides but stays elevated). Treatment: Mebendazole (kills larvae off very slowly) Control: Education, Prop meat cooking, Meat inspection, Freeze meat (does not work for nativa), Rat free piggeries |
What is this parasite?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? Control? |
|
|
Trichinella (Nematoda). It is an image of periorbital edema, which is a classic symptom of the parasite during the migratory (invasive) phase.
Species: (1) Spiralis (2) Nelsoni (3) Nativa |

What parasitic infection is this images a sign of?
|
|
|
Toxocara canis (Nematoda) egg.
Transfer: Dogs defecate egg (usually start 3w after birth)-> L1-L2(2w) infective-> Ingestion of L2 larva still in egg. Life cycle: L2 larva infective. Migrates to eye & liver in humans. Does not lay eggs in humans. |
What parasite is this?
Transfer? Life Cycle? |
|
|
Toxacara canis (nematoda). They are ocular larva migrans and causes blindness.
Hosts: Definitive: Dogs (puppies main excretors) Intermediate: Humans Transfer: Dogs defecate egg (usually start 3w after birth)-> L1-L2(2w) infective-> Ingestion of L2 larva still in egg. Life cycle: L2 larva infective. Migrates to eye & liver in humans. Does not lay eggs in humans. Diagnosis: History, Symptoms, Serology. Symptoms: Ocular larva migrans (OLM) cause blindness. Visceral larva migrans (VLM) cause hepatomegaly. Treatment: Thiabnedazole Control: Deworm dogs. Properly control dog feces. |

What parasitic infection are these images a sign of?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? Control? |
|
|
Loa Loa (Nematode-Human Subcutaneous Filaria)
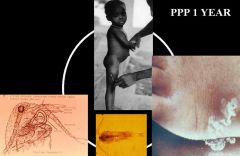
Hosts: Definitive: Humans Intermediate: Chrysops fly Location: Rain forests of Africa Transfer: L3 larva (infective) innoculated by chrysops fly (day biter). Life cycle: L1 larva (MF) released into water by adult. L1-L3 larva stages occur in Chrysops fly. PPP of 1 year. Worms mature at harvest time. Sexual repo. Diagnosis: Calabar swellings. Patients can see worms in eyes. Symptoms: Calabar swellings (Pain) caused by worm migration. Patient can see worm crawling in front of eyes. Swelling on the back of the arms. Treatment: Ivermectin. Surgical removal of worms. |

What parasitic infection are these images a sign of?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
Loa Loa (Nematode-Human Subcutaneous Filaria). It is the day biting Chrysops fly and is the intermediate host for the parasite.
Transfer: L3 larva (infective) inoculated by chrysops fly (day biter). Life cycle: L1 larva (MF) released into water by adult. L1-L3 larva stages occur in flea. PPP of 1 year. Worms mature at harvest time. Sexual repo. |

What parasite does this insect transfer & what is it called?
Transfer? Life cycle? |
|
|
Dracunculus medinensis (Nematode-Human Subcutaneous Filaria) "Guinea worm"
|
What parasitic infection are these images a sign of?
|
|
|
Dracunculus medinensis (Nematode-Human Subcutaneous Filaria) "Guinea worm"
Hosts: Definitive: Humans Intermediate: Cyclops water flea (microscopic) Location: Central Africa (esp. Sudan), India, Bangladesh Transfer: L3 larva (infective) innoculated by ingestion of cyclops flea (drinking). Life cycle: L1 larva (MF) released into water by adult. L1-L3 larva stages occur in flea. PPP of 1 year. Worms mature at harvest time. Sexual repo. Diagnosis: Foot pain & ulcers with worm visible. Symptoms: Migration of female to foot cause intense pain (relieved by water immersion), Ulcer, Secondary bacterial infection, Disability. Dead worm-> cellulites. Treatment: Albendazole, Thiabendazole, Moist bandages (don’t' kill, make easier to remove). Removed by slowly winding around stick. Control: Clean water (filters). Abate kills cyclops. Infected no enter water. |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? Control? |
|
|
Dracunculus medinensis (Nematode-Human Subcutaneous Filaria) "Guinea worm"
Treatment: Albendazole, Thiabendazole, Moist bandages (don’t' kill, make easier to remove). Removed by slowly winding around stick. Control: Clean water (filters). Abate kills cyclops. Infected no enter water. |

What parasitic infection is being treated in the surgical procedure in the picture?
Treatment? Control? |
|
|
Onchocerca volvuls (Nematode-Human Subcutaneous Filaria) "River Blindness" and is transferred by the Simulium fly.
Transfer: L3 larva (infective) inoculated into skin (slashing that enters subQ tissue but does not cause bleeding) by Simulium fly. Life cycle: L1 larva (MF) in skin. L1-L3 in simulium fly. Adult in onchocerc-omata (near bone). MF contain Wolbachia [gram(-) bacteria]-> need to survive & main cause of inflam. Sexual repo. |

What parasite does this insect transfer & what is it called?
Transfer? Life cycle? |
|
|
Onchocerca volvuls (Nematode-Human Subcutaneous Filaria) "River Blindness". The pictures show adult worms in onchocercomata. Onchocercomata are located throughout the body near bones but can be visible externally if they are located near a bony prominence.
Note: Even though the picture shows a nodule on the head the adult worm is NOT in the brain, nor does it affect the brain. |

What parasitic infection are these images a sign of?
|
|
|
Onchocerca volvuls (Nematode-Human Subcutaneous Filaria) "River Blindness"
Hosts: Definitive: Humans. Intermediate: Simulium fly Location: Central Africa. North part of South America, C America (near flowing rivers) Transfer: L3 larva (infective) inoculated into skin (slashing that enters subQ tissue but does not cause bleeding) by Simulium fly. Life cycle: L1 larva (MF) in skin. L1-L3 in simulium fly. Adult in onchocerc-omata (near bone). MF contain Wolbachia [gram(-) bacteria]-> need to survive & main cause of inflam. Sexual repo. Diagnosis: Skin snips, ELISA plate. Symptoms: Adult worms: Little pathology. Some onchocercomata visible over bony prominences. Microfilariae in skin: Pruritus (itch never stops), Papular dermatitis, Lichenification (lizard skin), Depigmentation, Dermal atrophy (tissue-paper skin)-> Hanging groin, Sclerosing keratitis-> blindness. Dying MF: Allergic reaction. Treatment: Ivermectin. Surgical removal of worms. Doxycylcine. Control: Vector control, Treatment, Relocation of villages. |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? Control? |
|
|
Onchocerca volvuls (Nematode-Human Subcutaneous Filaria) "River Blindness". The picture shows an allergic reaction because of the death of microfilaria in the skin. Many scratches are also apparent because of the microfilaria cause incessant & severe pruritus. This itch is constant throughout the day & night.
|

What parasitic infection are these images a sign of?
|
|
|
Onchocerca volvuls (Nematode-Human Subcutaneous Filaria) "River Blindness". These pictures show lichenification (lizard skin). It is due to presence of microfilaria in the skin.
|

What parasitic infection are these images a sign of?
|
|
|
Onchocerca volvuls (Nematode-Human Subcutaneous Filaria) "River Blindness". These pictures show dermal atrophy which can lead to hanging groins and loose skin. It is due to presence of microfilaria in the skin.
|
What parasitic infection are these images a sign of?
|
|
|
Onchocerca volvuls (Nematode-Human Subcutaneous Filaria) "River Blindness". These pictures show Sclerosing keratitis, which progressively lead to blindness. It is due to presence of microfilaria in the eye.
|
What parasitic infection are these images a sign of?
|
|
|
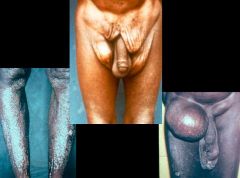
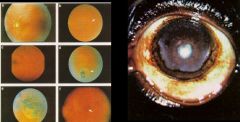
Wuchereria bancrofti (Nematode-Human Lymphatic Filaria).
Hosts: Definitive: Humans Intermediate: Mosquitoes Location: Africa, Middle East, Asia, Philippines Transfer: L3 larva (infective) inoculated by mosquito. Rural areas: Anopholes, Mansonia mosquitoes Urban areas: Culex mosquito Life cycle: L1 larva (MF) in blood (@ night). L1-L3 in mosquito (10dy-no multiplication). PPP of 13mo. Adults initially in lymph & migrate to nodes causing damage. Predilection site in males (spermatic cord). Sexual repo. Diagnosis: ICT card test (Gold standard-detect female worm antigens), Thick blood film, Membrane filter concentration. Symptoms: Usually contracted in childhood->manifest later. Adult worms: Lymphatic damage-> Lymphoedema-> Recurrent infection-> Elephantiasis, Hydrocoele (men), & Chyluria (early symptom). Micro Filaria: Filarial fever (secondary infections->acute inflammatory episodes) Treatment: Micro Filaria: DEC clears 95% up to 1yr, Ivermectin & Albendazole 99% up to 1yr. Hydrocoele: Surgery. Lymphoedema/Elephantiasis: Hygiene, Elevation, Skin care. Exercise) Control: Guyana/China DEC fortified salt. Mass drug administration. Doxycycline (new->kills wolbachia->kills MF). |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? Control? |
|
|
Wuchereria bancrofti (Nematode-Human Lymphatic Filaria).
Hosts: Definitive: Humans Intermediate: Mosquitoes Location: Africa, Middle East, Asia, Philippines Transfer: L3 larva (infective) inoculated by mosquito. Rural areas: Anopholes, Mansonia mosquitoes Urban areas: Culex mosquito Life cycle: L1 larva (MF) in blood (@ night). L1-L3 in mosquito (10dy-no multiplication). PPP of 13mo. Adults initially in lymph & migrate to nodes causing damage. Predilection site in males (spermatic cord). Sexual repo. Diagnosis: ICT card test (Gold standard-detect female worm antigens), Thick blood film, Membrane filter concentration. Symptoms: Usually contracted in childhood->manifest later. Adult worms: Lymphatic damage-> Lymphoedema-> Recurrent infection-> Elephantiasis, Hydrocoele (men), & Chyluria (early symptom). Micro Filaria: Filarial fever (secondary infections->acute inflammatory episodes) Treatment: Micro Filaria: DEC clears 95% up to 1yr, Ivermectin & Albendazole 99% up to 1yr. Hydrocoele: Surgery. Lymphoedema/Elephantiasis: Hygiene, Elevation, Skin care. Exercise) Control: Guyana/China DEC fortified salt. Mass drug administration. Doxycycline (new->kills wolbachia->kills MF). |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? Control? |
|
|
Wuchereria bancrofti (Nematode-Human Lymphatic Filaria). The ICT card test detects antigens from the female worm, can be used even when micro filaria aren't in the blood, & is the current gold standard for diagnosing an infection.
|
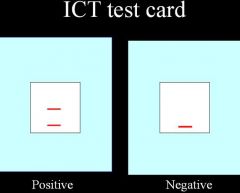
What parasite is this diagnostic test used to detect?
|
|
|
Wuchereria bancrofti (Nematode-Human Lymphatic Filaria). Adult worms migration from the lymphatics to the lymph nodes can cause Lymphatic damage. Lymphoscintigraphy is use to determine if lymphatic damage has occurred so that precautions can be taken to prevent the progression of the disease from lymphoedema to elephantiasis.
|
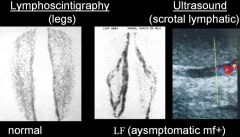
These diagnostic tests used to detect damage from what parasite?
|
|
|
Wuchereria bancrofti (Nematode-Human Lymphatic Filaria). They are images of lymphoedema, which is a result of damage to the lymphatic system caused by the migration of adult worms migration from the lymphatics to the lymph nodes. If precautionary steps aren't taken lympeodema can progress to elephantiasis.
|

What parasitic infection are these images a sign of?
|
|
|
Wuchereria bancrofti (Nematode-Human Lymphatic Filaria). They are images of lymphoedema & chyluria (chyle in urine), which are a result of damage to the lymphatic system caused by the migration of adult worms migration from the lymphatics to the lymph nodes. If precautionary steps aren't taken lympeodema can progress to elephantiasis.
|
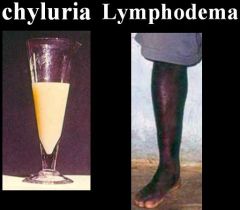
What parasitic infection are these images a sign of?
|
|
|
Wuchereria bancrofti (Nematode-Human Lymphatic Filaria). This is an image of elephantiasis. It was caused by damage to the lymphatic system because of the migration of adult worms from the lymphatics to the lymph nodes which resulted in lymphoedema. Repeated infections, cuts, & scratches then exacerbate the condition into elephantiasis.
|
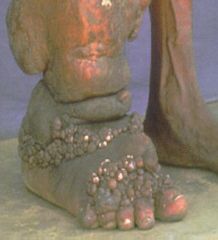
What parasitic infection is this image a sign of?
|
|
|
Wuchereria bancrofti (Nematode-Human Lymphatic Filaria). This is an image of a hydrocoele. It was caused by damage to the lymphatic system because of the migration of adult worms from the lymphatics to the lymph nodes. The adult worm has a predilection site in the spermatic cord of males which can lead to to the formation of a hydrocoele.
|

What parasitic infection is this image a sign of?
|
|
|
Wuchereria bancrofti (Nematode-Human Lymphatic Filaria). These are images of a hydrocoeles. They are caused by damage to the lymphatic system because of the migration of adult worms from the lymphatics to the lymph nodes. The adult worm has a predilection site in the spermatic cord of males which can lead to to the formation of a hydrocoele. The bottom right picture shows the surgical removal of a hydrocoele.
|

What parasitic infection are these images a sign of?
|
|
|
Nematode life cycle
|
(1) 5 moult stages (L1-L5) with L5 being the adult
(2) Different nematodes are infective at different moult stages (3) One larva->On adult (except for strongyloides stercoralis) (4) Larva will or will not undergo hepatotracheal in the definitive host migration depending on the species (5) Sexes are separate |
|
|
Direct nematode life cycle
|
First two moults are on the ground or in the egg
|
|
|
Indirect nematode life cycle
|
First two moults are in the insect
|
|
|
What are the different ways in which nematodes pass their eggs or larvae?
|
(1) Unsegmented ovum
(2) A dividing ovum (3) Developed larvae in the egg (oviparous) (4) Larvae hatch in utero (viviparous) |
|
|
Characteristics of human filariasis (Nematoda)?
|
(1) Pre-patent period (PPP) usually about 1 year.
(2) They don't multiply in the vector (3) None are zoonotic (4) All adults are long slender worms (5) L1 microfilariae are produced by the adult female & the L3 larvae are then ingested, inoculated, or drunk. |

