![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
81 Cards in this Set
- Front
- Back
|
Trpanosoma
Species: (1) Cruzi (2) Rangeli It is called a Chagoma (Romana's Sign) & is a sign of a bite from a reduviid. The reduviids like to feed at night near the eyes and mouth. and carry the parasite. The parasite is passed into the person by fecal matter left by the insect & rubbed into a wound or mucus membrane. |

What parasitic infection are these images a sign of?
|
|
|
Trypanosoma cruzi (protozoa). Chronic infection by trypanosoma cruzi can cause cardiomegaly through the destruction of myocardial fibers & ganglion cells. At these stages of the disease there is no cure, only supportive therapy.
|
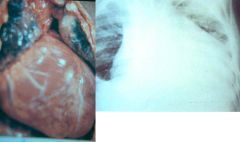
What parasitic infection are these images a sign of?
|
|
|
Trypanosoma cruzi (protozoa). Chronic infection by trypanosoma cruzi can cause apical aneurysms through the destruction of myocardial fibers & ganglion cells. At these stages of the disease there is no cure, only supportive therapy.
|

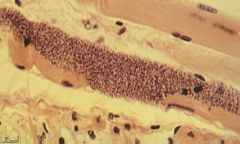
What parasitic infection is this image a sign of?
|
|
|
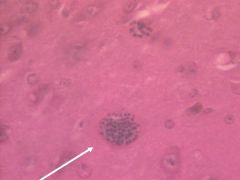
Trypanosoma Cruzi (Amastigote) in muscle.
Symptoms: Acute (4-8w): Bites near eye & mouth causing legions called Chagoma (Romana's Sign) that last for months, Fever, Progressive anemia, Edema, Lympadenopathy, Hepatosplenomegaly, EKG abnormalities, CNS involvement, Degeneration of parasitized tissue. Intermediate: Asymptomatic Chronic (Fatal): Chronic (Fatal): Fever, Constipation & Abdominal Distension (Myenteric plexus destruction), EKG abnormalities, Cardiomegaly & apical aneurysms (Destruction of myocardial fibers & ganglion cells), Pain. |
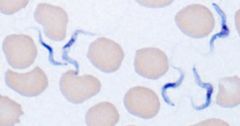
What parasite is this?
Symptoms? |
|
|
Trypanosoma Cruzi (Trypomastigote) in blood.
Hosts: Possum, Armadillo, Rodents, Humans Location: South & Central America Transfer: Reduviid Bugs (blood suckers): Triatomids, Rhodnius, Panstrongylus. Night feeders. Xfer by feces enter mucus membrane or wound. Verticle transmission. Life cycle: Reduviid (multiplies)-> Enters host-> Trypomastigote in blood-> Amastigote (multiplies) in muscle & nerve-> Trypomastigote in blood. Diagnosis: Thin smear, Thick smear, Fresh smear, Xenodiagnosis (Trypomastigote levels not high in blood, multiplies in bug as well). Symptoms & Pathology? Treatment: Benzimidazole & Nifurtimox (Older drug): Both treat all symptoms including neuroligical ones. Control: Education, Improve housing, Vector control, Screening of blood donors. |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Treatment? Control? Treatment? |
|
|
Trypanosoma cruzi (protozoa). Chronic infection by trypanosoma cruzi can cause megacolon through the destruction of the myenteric plexuses in the gut. At these stages of the disease there is no cure, only supportive therapy.
|

What parasitic infection are these images a sign of?
|
|
|
Trypanosoma (Trypomastigote) in blood.
Species: (1) Brucei Gambiense: Brain (Melarsopral), Everywhere else (Suramin) (2) Brucei Rhodiense: Brain (Melarsopral), Everywhere else (Suramin) (3) Rangeli: Asymptomatic (Benzimidazole[New] or Nifurtimox[Old]) |

What parasite is this?
Treatment? |
|
|
Trypanosoma (Trypomastigote) in blood.
Species: (1) Brucei Gambiense: Riverine Tsetse flies: Through saliva. Feed during day. Bite behind ears is extremely painful. Verticle transmission. (2) Brucei Rhodiense: Savannah Tsetse flies: Through saliva. Feed during day. Bite behind ears is extremely painful. Verticle transmission. (3) Rangeli: Reduviid Bugs (blood suckers): Triatomids, Rhodnius, Panstrongylus. Night feeders. Xfer by feces enter mucus membrane or wound. Verticle transmission. |

What parasite is this?
Transfer? |
|
|
Trypanosoma (Trypomastigote) in blood.
Species: (1) Brucei Gambiense. Hosts: Humans & Pigs main resevoirs of infection Location: West Africa (2) Brucei Rhodiense. Hosts: Gaming & Domestic animals, Humans Location: East & central Africa (3) Rangeli. Hosts: Possum, Armadillo, Rodents, Humans Location: South & Central America |
What parasite is this?
Hosts? Location? |
|
|
Trypanosoma brucei.
Species: (1) Gambiense: Riverine tsetse fly (2) Rhodiense: Savannah tsetse fly It is the Tsetse fly & feeds during the day. It's bite is very painful and normally behind the ears. |

What parasite does this insect transfer & what is it called?
|
|
|
Trypanosoma brucei.
Species: (1) Gambiense (2) Rhodiense Top picture: Trypanosoamil chancre from bite of Tstse fly. Bottom picture: Enlarged cervical lymph nodes (Winterbottom's Sign). Life cycle: All stages occur in the blood. Diagnosis: Thin smear, Thick smear, Aspirated gland juice, CSF (Centrifuged deposit), PCR/DNA. Treatment: Intravenous Suramin (Removes tryps everywhere but CNS), Melarsoprol (CNS treatment). Control: Aerial, ground, & cattle insectiside. Biconical trap for fly. |

What parasitic infection are these images a sign of?
Life cycle? Diagnosis? Treatment? Control? |
|
|
Leishmania.
Species: (1) Donavani (2) Braziliensis (3) Guyanesis (4) Tropica (5) Major It is a sand fly that lives in dry climates & is called Lutzomyia in the new world and Phlebotomus in the old world. It likes to bite at dusk and dawn, does not need water to breed, and lives in termite hills. |

What parasite does this insect transfer & what is it called?
|
|
|
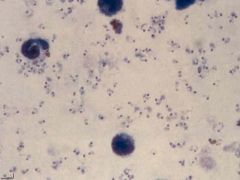
Leishmania (Amastigote) in white blood cells (macrophages) of a bone marrow aspirate.
(1) Donavani: Canids (dogs, etc.), Rodents (rarely), Humans. (2) Braziliensis: Dogs (main reservoir), Humans. (3) Guyanesis: Sloths & Rodents (main reservoir), Humans. (4) Tropica: Canids (dogs, etc.), Rodents (rarely), Humans. (5) Major: Canids (dogs, etc.), Rodents (rarely), Humans. |
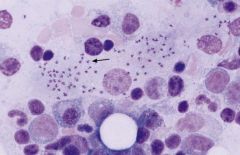
What parasite is this?
Hosts? |
|
|
Leishmania (Amastigote) that has invaded white blood cells (macrophages).
Species: (1) Donavani: East India, Africa, South Europe, South & Central America. (2) Braziliensis: South & Central America. (3) Guyanesis: South & Central America. (4) Tropica: East India, Africa, Southern Europe. (5) Major: East India, Africa, Southern Europe. Treatment: Pentavalent antimonials by IV - Pentostam (old) or Amphiteracin B (new & better but expensive). |

What parasite is this?
Location? Treatment? |
|
|
Leishamani (small cutaneous ulcers)
Species: (1) Braziliensis (2) Guyanesis They are small cutaneous ulcers that healed after a few months. Even though these ulcers have healed in 3-20 years the parasite will cause large disfiguring mucocutaneous lesions (usually around the nose & mouth) that are known as Espunda or Uta. |

What parasitic infection are these images a sign of?
|
|
|
Leishmania tropica (Dry ulcers).
Life cycle: Amastigote in skin macrophages (WBC's). Promastigote in saliva of the fly. Multiplies in vector & host. Diagnosis: History, Amastigotes in fluid aspirated (culture) from below ulcer, Serological (limited value). Symptoms: Small red papule that ulcerates after 2-4 months. Dry ulcer that will heal in 2-3 months in immunocompetent individuals. |

What parasitic infection are these images a sign of?
Life cycle? Diagnosis? Symptoms? |
|
|
Leishamani (mucocutaneous lesions)
Species: (1) Braziliensis (2) Guyanesis Life cycle: Amastigote in skin macrophages (WBC's). Promastigote in saliva of the fly. Multiplies in vector & host. Diagnosis: (Direct Only) Amastigotes in legions, Culture/lab animals. Symptoms: Small cutaneous papule. Ulcerates & heals after few months. After 3-20 years, destructive oral &/or nasal legions (Espunda or Uta [mucocutaneous leishmaniasis]). |

What parasitic infection are these images a sign of?
Life cycle? Diagnosis? Symptoms? |
|
|
Leishmaniasis (Promastigote) in saliva of the sand fly.
Species: (1) donavani: East India, Africa, South Europe, South & Central America (2) braziliensis: South & Central America (3) guyanesis: South & Central America (4) tropica: East India, Africa, South Europe (5) major: East India, Africa, South Europe |

What parasite is this?
Location? |
|
|
Leishamani (mucocutaneous lesions)
Species: (1) Braziliensis (2) Guyanesis Life cycle: Amastigote in skin macrophages (WBC's). Promastigote in saliva of the fly. Multiplies in vector & host. Diagnosis: (Direct Only) Amastigotes in legions, Culture/lab animals. Symptoms: Small cutaneous papule. Ulcerates & heals after few months. After 3-20 years, destructive oral &/or nasal legions (Espunda or Uta [mucocutaneous leishmaniasis]). |

What parasitic infection are these images a sign of?
Life cycle? Diagnosis? Symptoms? |
|
|
Leishmania tropica (Large noticable scars from healed dry ulcers).
Life cycle: Amastigote in skin macrophages (WBC's). Promastigote in saliva of the fly. Multiplies in vector & host. Diagnosis: History, Amastigotes in fluid aspirated (culture) from below ulcer, Serological (limited value). Symptoms: Small red papule that ulcerates after 2-4 months. Dry ulcer that will heal in 2-3 months in immunocompetent individuals. |

What parasitic infection are these images a sign of?
Life cycle? Diagnosis? Symptoms? |
|
|
Leishmania major (serous ulcer).
Life cycle: Amastigote in skin macrophages (WBC's). Promastigote in saliva of the fly. Multiplies in vector & host. Diagnosis: History, Amastigotes in fluid aspirated (culture) from below ulcer, Serological (limited value). Symptoms: Small red papule that ulcerates after 2 weeks. Produces serous exudate. Heals on its own in immunocompetent individuals. |

What parasitic infection is this image a sign of?
Life cycle? Diagnosis? Symptoms? |
|
|
Leishmania donavani.
Life cycle: Amastigote in visceral WBC's 4-6 days after infection. Promastigote in saliva of the fly. Multiplies in vector & host. Diagnosis: Amastigotes in marrow/spleen smears, Culture of aspirates / blood taken during febrile period, Xenodiagnosis, Serology. Symptoms: Early: Irregular fever (double daily peak), Anemia, Leucopenia, Diarrhea, Bleeding gums, Joint pain, Weight Loss. Late: Enlarged lymph nodes, Splenomegaly, Hepatomegaly. Infection reappears after treatment in immunocompromised individuals. |
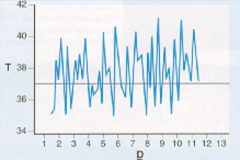
What parasitic infection is this image a sign of?
Life cycle? Diagnosis? Symptoms? |
|
|
Trichomonas vaginalis.
Hosts: Humans Location: Worldwide Transfer: Sexual intercourse Life cycle: Binary fission in: female-Vagina. male-Urethra, Epididymis, & Prostate. No protective stage. Diagnosis: Trophozoites in urine or vaginal discharge smears. Symptoms: Males: Asymptomatic. Females: Vaginitis, burning sensation, thick yellow discharge, vulvar &/or vaginal erythema. Treatment: Metronidazole (Flagly) - Sexual partners treated simultaneously. |
What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
Trichomonas vaginalis.
Hosts: Humans Location: Worldwide Transfer: Sexual intercourse Life cycle: Binary fission in: female-Vagina. male-Urethra, Epididymis, & Prostate. No protective stage. Diagnosis: Trophozoites in urine or vaginal discharge smears. Symptoms: Males: Asymptomatic. Females: Vaginitis, burning sensation, thick yellow discharge, vulvar &/or vaginal erythema. Treatment: Metronidazole (Flagly) - Sexual partners treated simultaneously. |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
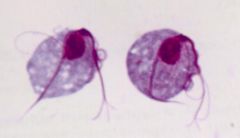
Giardia (trophozoite) not infective.
Hosts: Humans, Dogs, Cattle, Sheep, Wild mammals e.g. Beavers. Location: Worldwide Transfer: Ingestion of cysts. Trophozoites passed in diarrhea uninfective. Cysts passed in dry stools are immediately infective. Life cycle: Trophozoites divides & lives in the intestines & sloughs off in feces in bursts. Diagnosis difficult because stool sample may not contain parasite. Diagnosis: Symptoms, Stool microscopy, ELISA, Immunofluorescent (good but expensive), Therapeutic trial Symptoms: Any or All: Pale, loose, foul smelling, & fatty stools. Diarrhea 3-8 x daily. Abdominal distension. Offensive flatulence. Abdominal pain. Weight loss - anorexia. Sulphorous belching. Lasts for few days to several weeks. Treatment: Metronidazole (Flagyl). |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
Giardia (trophozoite) not infective.
Hosts: Humans, Dogs, Cattle, Sheep, Wild mammals e.g. Beavers. Location: Worldwide Transfer: Ingestion of cysts. Trophozoites passed in diarrhea uninfective. Cysts passed in dry stools are immediately infective. Life cycle: Trophozoites divides & lives in the intestines & sloughs off in feces in bursts. Diagnosis difficult because stool sample may not contain parasite. Diagnosis: Symptoms, Stool microscopy, ELISA, Immunofluorescent (good but expensive), Therapeutic trial Symptoms: Any or All: Pale, loose, foul smelling, & fatty stools. Diarrhea 3-8 x daily. Abdominal distension. Offensive flatulence. Abdominal pain. Weight loss - anorexia. Sulphorous belching. Lasts for few days to several weeks. Treatment: Metronidazole (Flagyl). |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
Giardia (trophozoite) not infective.
Hosts: Humans, Dogs, Cattle, Sheep, Wild mammals e.g. Beavers. Location: Worldwide Transfer: Ingestion of cysts. Trophozoites passed in diarrhea uninfective. Cysts passed in dry stools are immediately infective. Life cycle: Trophozoites divides & lives in the intestines & sloughs off in feces in bursts. Diagnosis difficult because stool sample may not contain parasite. Diagnosis: Symptoms, Stool microscopy, ELISA, Immunofluorescent (good but expensive), Therapeutic trial Symptoms: Any or All: Pale, loose, foul smelling, & fatty stools. Diarrhea 3-8 x daily. Abdominal distension. Offensive flatulence. Abdominal pain. Weight loss - anorexia. Sulphorous belching. Lasts for few days to several weeks. Treatment: Metronidazole (Flagyl). |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
Giardia (cystic form) immediately infective through ingestion.
|

What parasite is this?
|
|
|
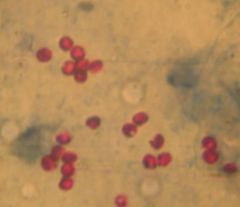
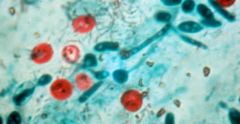
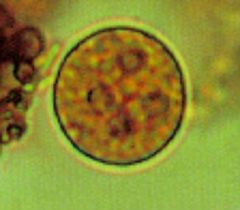
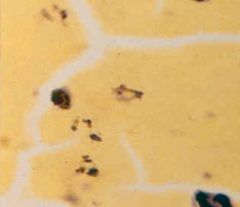
Cryptosporidium parvum (cystic form) in stool with modified Ziehl-Neelsen stain.
Hosts: Turkey, calf, lamb, kid, deer, foal, puppy, kitten, human. Location: Worldwide Transfer: Water, Food. Not killed by chlorine. Oocysts immediately infective by ingestion. Life cycle: Invades gut enterozytes (brush border of intestine). Release oocyst in feces with 4 sporozoites each. Diagnosis: Oocysts in stool (mod Ziehl-Neelsen stain), ELISA, Immunoflourescencse, Intestinal biopsy. Treatment: Don't use anti-diarrheal b/c prolongs infection. Fluid & electrolyte loss treatment. |
What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Treatment? |
|
|
Cryptosporidium parvum (cystic form) in stool with modified Ziehl-Neelsen stain.
Hosts: Turkey, calf, lamb, kid, deer, foal, puppy, kitten, human. Location: Worldwide Transfer: Water, Food. Not killed by chlorine. Oocysts immediately infective by ingestion. Life cycle: Invades gut enterozytes (brush border of intestine). Release oocyst in feces with 4 sporozoites each. Diagnosis: Oocysts in stool (mod Ziehl-Neelsen stain), ELISA, Immunoflourescencse, Intestinal biopsy. Treatment: Don't use anti-diarrheal b/c prolongs infection. Fluid & electrolyte loss treatment. |

What parasite is this?
Hosts? Location? Transfer? Life cycle? Diagnosis? Treatment? |
|
|
Cryptosporidium parvum (cystic form) in stool with modified Ziehl-Neelsen stain.
Symptoms: 1-2 weeks after exposure: Explosive, watery diarrhea that is brown-green in color. Frequency 2-10 x day for 3-10 days, complete recovery. Immunocompromised: Chronic diarrhea, Abdominal pain, Fever, Lymphadenopathy, Weight loss, Malnutrition, Villous atrophy. |
What parasite is this?
Symptoms? |
|
|
Cryptosporidium parvum (cystic form) in stool with modified Ziehl-Neelsen stain.
Symptoms: 1-2 weeks after exposure: Explosive, watery diarrhea that is brown-green in color. Frequency 2-10 x day for 3-10 days, complete recovery. Immunocompromised: Chronic diarrhea, Abdominal pain, Fever, Lymphadenopathy, Weight loss, Malnutrition, Villous atrophy. |

What parasite is this?
Symptoms? |
|
|
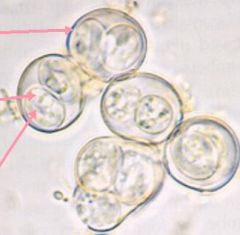
Entamoeba histolytica (cystic form) in a stool sample. Notice that 4 nuclei is characteristic of the cystic form of this parasite.
Hosts: Humans ONLY (not zoonosis) Location: Worldwide Transfer: Trophozoites passed in diarrhea uninfective. Cysts passed in dry stools are immediately infective by ingestion. |
What parasite is this?
Hosts? Location? Transfer? |
|
|
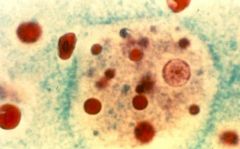
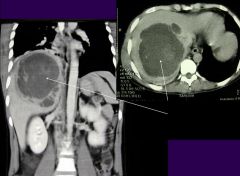
Entamoeba histolytica (invasive form, only 5% of cases). Parasite leaves the gut and invades other tissue (cardiac in this picture).
(1) Noninvasive Life cycle: Trophozoites live in lumen of large intestine. Diagnosis: Cysts in stool. Symptoms: 95% asymptomatic, Diarrhea, Flatulence, Abdominal pain, Blood & mucus in stool, Tear drop ulcers in gut. Treatment: Metronidazole (Flagyl). Fluid & electrolyte loss treatment. (2) Invasive Life cycle: Invasive: Trophozoites in RBC's, Liver, & Other organs. Diagnosis: Trophozoites in RBC's, ELISA (expensive), Aspiration, Ultrasound (liver cyst), X-ray/CT/MRI (brain & lung cyst). Symptoms: Cysts in Liver (majority), Brain, Skin, Lungs, Orbit, Spleen, Genitals -> Fever, Tender liver (pain), Hepatomegaly. Treatment: Metronidazole (Flagyl). Ultrasound guided drainage of cysts may be necessary. |
What parasite is this?
Life cycle? Diagnosis? Symptoms? Treatment? |
|
|
Entamoeba histolytica (invasive form, only 5% of cases). Parasite leaves the gut and invades other tissue. Its is a radiograph of amoebic liver abscesses.
|
What parasitic infection is this image a sign of?
|
|
|
Toxoplasma gondii (Tachyzoites) in leukocytes. They are rapidly proliferating and are transported to all organs. This form of the parasite is responsible for vertical transmission from mother to fetus and is found in raw milk. It is infective. Consuming this form of the parasite in raw milk represents the least common mean of infection.
Hosts: Definative: Cats. Intermediate: Lamb, Goat, Pork, Chicken, Rodents. |

What parasite is this?
Hosts? |
|
|
Toxoplasma gondii (Sporulated oocyst) from cat feces. This form IS infective and took 1-5 days in the environment to develop into a sporulated cyst after it had been released. The unsporulated cyst was not infective. These represent the second most frequent means of infection.
Location: Worldwide Life cycle: Cats ingest cysts (bradyzoites)-> Trophozoites-> Schizogonous & gametogonous development-> Oocysts (3-10dy)-> Unsporulated oocysts shed for 1-3wk-> Sporulate after 1-5dy in environment. Diagnosis: IgG, IgM serology. Imaging for ocular toxoplasmosis or toxoplasmic encephalitis, Isolation of parasites, Tissue biopsy. |
What parasite is this?
Symptoms? |
|
|
Toxoplasma gondii (Unsporulated oocyst) in cat feces. This form is NOT infective and takes 1-5 days to develop into a sporulated cyst after it has been released into the environment in the cat's feces. The sporulated cyst IS infective. These represent the second most frequent means of infection.
Location: Worldwide Life cycle: Cats ingest cysts (bradyzoites)-> Trophozoites-> Schizogonous & gametogonous development-> Oocysts (3-10dy)-> Unsporulated oocysts shed for 1-3wk-> Sporulate after 1-5dy in environment. Diagnosis: IgG, IgM serology. Imaging for ocular toxoplasmosis or toxoplasmic encephalitis, Isolation of parasites, Tissue biopsy. |

What parasite is this?
Location? Life cycle? Diagnosis? |
|
|
Toxoplasma gondii (Bradyzoites) in muscle tissue. There is no inflammation around the cysts and they parasite replicates slowly & indefinitely. This form of the parasite is acquired through consumption of undercooked meat containing the parasite. It is infective. Consuming this form of the parasite in meat is the most common mean of infection. Bradyzoites in our muscle can reactivate later in life.
Symptoms: Immunocompetent: Usually asymptomatic & get immunity (IgM during infection & IgG after). Immunocompromised: Invade all tissues but predeliction sites Eye (Chorioretinitis), Brain (Cysts, encephalitis: Headache, Disorientation, Coma). Fetus of recently newly infected mother: Severe: Chorioretinitis, Hydrocephalus (aqueduct block), Cerebral Necrosis, Liver failure. Less Severe: Poor cognitive skills, Jaundice, Anaemia, Convulsions, Growth retardation. Treatment: Spiramycin: Prevent verticle transmission to fetus & may be given after birth as well. TMP/SMX (Bactrim) Pyrimethamine w/ Dapsone: Prophylaxis for immunocompromised individuals. |
What parasite is this?
Symptoms? Treatment? |
|
|
Toxoplasma gondii. They are images of infants with hydrocephalus. It can occur in children who's mothers were infected with the parasite for the first time early in their pregnancy.
|

What parasitic infection are these images a sign of?
|
|
|
Toxoplasma gondii. Those are images of chorioretinitis & are indicative of an infection in an immunocompromised individual or a person who's mother was infected with the parasite for the first time early in her pregnancy.
|

What parasitic infection are these images a sign of?
|
|
|
Toxoplasma gondii. Those are images of chorioretinitis & are indicative of an infection in an immunocompromised individual or a person who's mother was infected with the parasite for the first time early in her pregnancy.
|
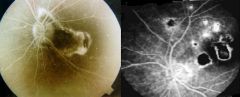
What parasitic infection are these images a sign of?
|
|
|
Toxoplasma gondii. It is an image of chorioretinitis & is indicative of an infection in an immunocompromised individual or a person who's mother was infected with the parasite for the first time early in her pregnancy.
|

What parasitic infection is this image a sign of?
|
|
|
Toxoplasma gondii. Those are images of chorioretinitis & are indicative of an infection in an immunocompromised individual or a person who's mother was infected with the parasite for the first time early in her pregnancy.
|
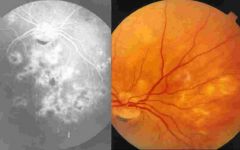
What parasitic infection are these images a sign of?
|
|
|
Toxoplasma gondii. It is picture of a brain with encephalitis and is indicative if an infection in an immunocompromised individual.
|
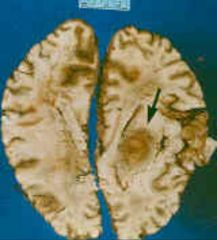
What parasitic infection is this image a sign of?
|
|
|
Toxoplasma gondii. They are pictures of a brain with encephalitis and are indicative if an infection in an immunocompromised individual.
|
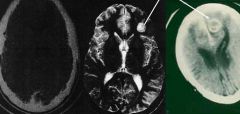
What parasitic infection are these images a sign of?
|
|
|
Plasmodium. This is a thick film with the red blood cells destroyed. The type of malaria cannot be discerned.
|
What parasite is this?
|
|
|
Plasmodium. This is a thick film with the red blood cells destroyed. The type of malaria cannot be discerned.
|
What parasite is this?
|
|
|
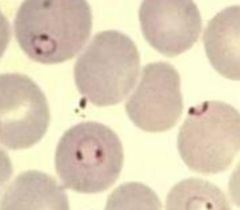
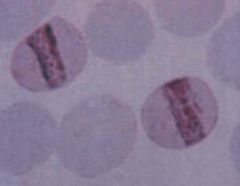
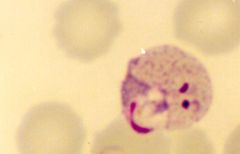
Plasmodium falciparum (Trophozoites) in sickle cell RBC's.
Notice: (1) Numerous fine ring forms (2) Double chromatin dots (3) Parasites are located near the border (margins) of the RBC (4) RBC's are not enlarged Pathogenesis: Haemolysis of RBC's. Parasite metabolites. Immune response. Cytoadherence (occlusion of capillaries-edema,organ failure) falciparum only. Cytokine increase. Malaria pigment production depletes iron stores increasing anemia. Symptoms: (looks like flu initially): Cold stage(15-60m): Mild, inappropriate cold-> leads to violent whole body shaking. Skin dry, pale, & cold. Pulse rapid & low-volume. Hot stage(2-6h): Fever. Skin flushed, dry & burining. Pulse rapid & bounding. Sweating stage(2-4h): Fever breaks. Profuse drenching sweat after patient may feel better. Can cause Diarrhea. Cerebral malaria (falciparum only): Coma, Convulsions, Abnormal posturing, Dysconjugate gaze, Retinal haemorrhages. |
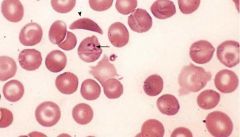
What parasite is this?
Pathogenesis? Symptoms? |
|
|
Plasmodium falciparum (Trophozoites) in RBC's.
Notice: (1) Numerous fine ring forms (2) Double chromatin dots (3) Parasites are located near the border (margins) of the RBC (4) RBC's are not enlarged Treatment: Coartem, Artemether/lumefantrine. Quinine, Quinadine (IV form of Quinine): Used on chloroquine resistant strains only (reserve drug). Control: Prophylactic drugs: Mefloquine, Doxycycline, Chloroquine, Malarone, Pauladrine. Bed nets impregnated with residual insecticide. Protective clothes, Repellent (DEET). |
What parasite is this?
Treatment? Control? |
|
|
Plasmodium falciparum (Trophozoites) in RBC's.
Notice: (1) Numerous fine ring forms (2) Double chromatin dots (3) Parasites are located near the border (margins) of the RBC (4) RBC's are not enlarged Diagnosis: Thick blood (Malaria present? Sensitivity). Thin blood (Type? Specificity). Later regular fever pattern indicitave (not as regular in falciparum b/c of RBC schizont release range). |
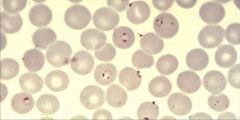
What parasite is this?
Diagnosis? |
|
|
Plasmodium falciparum (Trophozoites) in RBC's.
Notice: (1) Numerous fine ring forms (2) Double chromatin dots (3) Parasites are located near the border (margins) of the RBC (4) RBC's are not enlarged Hosts: Humans Location: Hot & wet climates. Predominant in Africa, New Guinea, & Haiti. Also present in South America & Asia. Transfer: Anopheline mosquito (saliva contains sporozoites) & feeds at night. Sporozoites in saliva mature from ingested gametocytes. Verticle transmission. Life cycle: Sporozoites ->Liver schizont(8d*40,000)->Merozites-> RBC's->Trophozoite ->RBC schizont(36-48h*8-32)->Merozites exit-> Gametocytes (mosq xfer) or Invade RBCs-> Gametocytes M&F fuse-> Zygote in mosq-> Ookinete-> Penetrate gut wall-> Oocyst-> Multiply-> Salivary gland-> Sporozoites (mosq 5d to mature). |

What parasite is this?
Hosts? Location? Transfer? Life cycle? |
|
|
Plasmodium falciparum (Gametocytes). Some merozites released from RBC's during lysis do not infect other RBC's but turn into Gametocytes to be picked up by other anopheline mosquitoes for transfer to other people.
Treatment: Coartem & Novartis (artemether/lumefantrine), Quinine, Quinadine Control: Prophylactic drugs: Mefloquine, Doxycycline, Chloroquine, Malarone, Pauladrine. Bed nets impregnated with residual insecticide. Protective clothes, Repellent (DEET). |

What parasite is this?
Treatment? Control? |
|
|
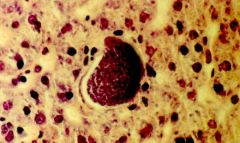
Plasmodium falciparum (schizonts adhered to endothelium of the brain). This is a picture of cerebral malaria & it can only be caused by plasmodium falciparum. Schizonts are adhered to endothelium of brain, which can cause:
(1) Coma (by definition) (2) Convulsions (3) Abnormal posturing (Decerebrate rigidity) (4) Dysconjugate gaze (5) Retinal haemorrhages It is clinically suspected when a patient with possible exposure to infection shows any reduction in consciousness. |

What parasite is this?
|
|
|
Plasmodium falciparum (schizonts adhered to endothelium of the brain). This is a picture of cerebral malaria & it can only be caused by plasmodium falciparum. Schizonts are adhered to endothelium of brain, which can cause:
(1) Coma (by definition) (2) Convulsions (3) Abnormal posturing (Decerebrate rigidity) (4) Dysconjugate gaze (5) Retinal haemorrhages It is clinically suspected when a patient with possible exposure to infection shows any reduction in consciousness. |
What parasite is this?
|
|
|
Top left: Coma (eyes open but unseeing)
Top right & bottom left: Decerebrate rigidity Bottom right: Dysconjugate gaze Plasmodium falciparum (cerebral malaria). These pictures indicate that schizonts of plasmodium falciparum are adhered to endothelium of brain, which can cause: (1) Coma (by definition) (2) Convulsions (3) Abnormal posturing (Decerebrate rigidity) (4) Dysconjugate gaze (5) Retinal haemorrhages It is clinically suspected when a patient with possible exposure to infection shows any reduction in consciousness. |

What parasitic infection are these images a sign of?
|
|
|
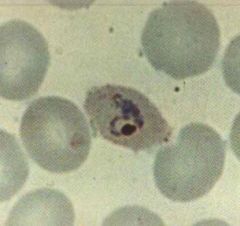
Plasmodium malariae (Trophozoites) in RBC's.
Notice: (1) Band shape (2) RBC not enlarged Hosts: Humans Location: Hot & wet climates. Replaces P. vivax in West africa because of people are resistant. Treatment: Chloroquine |
What parasite is this?
Hosts? Location? Treatment? |
|
|
Plasmodium malariae (Trophozoites) in RBC's.
Notice: (1) Band shape (2) RBC not enlarged Hosts: Humans Location: Hot & wet climates. Replaces P. vivax in West africa because of people are resistant. Treatment: Chloroquine |
What parasite is this?
Hosts? Location? Treatment? |
|
|
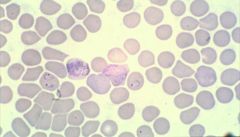
Plasmodium ovale (Trophozoites) in RBC's.
Notice: (1) "Oval" RBC (2) Enlarged RBC Hosts: Humans Location: Hot & wet climates. Widespread. Treatment: Chloroquine- Kills blood stages. Primaquine- Kills hypnozoites in liver preventing relapse & recurrence |
What parasite is this?
Hosts? Location? Treatment? |
|
|
Plasmodium ovale (Trophozoites) in RBC's.
Notice: (1) "Oval" RBC (2) Enlarged RBC Hosts: Humans Location: Hot & wet climates. Widespread. Treatment: Chloroquine- Kills blood stages. Primaquine- Kills hypnozoites in liver preventing relapse & recurrence |
What parasite is this?
Hosts? Location? Treatment? |
|
|
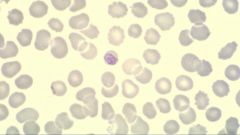
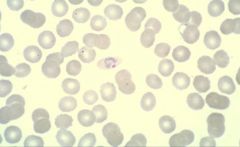
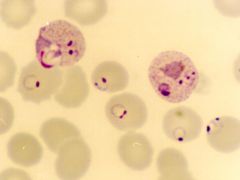
Plasmodium vivax (Trophozoites) in RBC's.
Notice: (1) Developing & thick (signet) ring forms (2) Enlarged RBC Hosts: Humans Location: Hot & wet climates. More common in S & C America, Asia. Treatment: Chloroquine- Kills blood stages. Primaquine- Kills hypnozoites in liver preventing relapse & recurrence |
What parasite is this?
Hosts? Location? Treatment? |
|
|
Plasmodium vivax (Trophozoites) in RBC's.
Notice: (1) Developing & thick (signet) ring forms (2) Enlarged RBC Hosts: Humans Location: Hot & wet climates. More common in S & C America, Asia. Treatment: Chloroquine- Kills blood stages. Primaquine- Kills hypnozoites in liver preventing relapse & recurrence |
What parasite is this?
Hosts? Location? Treatment? |
|
|
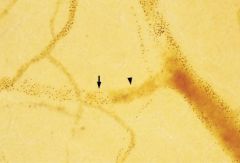
Plasmodium ovale or vivax (Hypnozoites) in the liver. If the malaria is treated and removed from the blood these hypnozoites remain dormant in the liver and may reactivate 20-30 years later. They are treated with Primaquine so that there is no recurrence of the malaria.
|
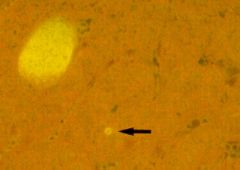
What parasite is this?
|
|
|
Plasmodium ovale or vivax (Hypnozoites) in the liver. If the malaria is treated and removed from the blood these hypnozoites remain dormant in the liver and may reactivate 20-30 years later. They are treated with Primaquine so that there is no recurrence of the malaria.
|
What parasite is this?
|
|
|
Plasmodium falciparum & Plasmodium vivax (trophozoites). Red blood cells are infected with BOTH types of malaria.
|
What parasite is this?
|
|
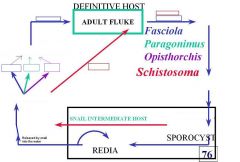
Fill in the blanks for the life cycle of the trematodes listed in this picture.
|
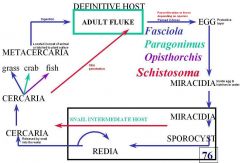
This is the answer.
|
|
|
Schistosoma mansonia (Trematoda) miracidia. The miracidia is the stage when the parasite emerges from the egg after it has entered water and infects the snail. All the schistosoma species go through this stage.
Notice: (1) Notice the tail is located laterally |

What parasite is this?
|
|
|
schistosoma (Trematoda) cercaria. The cercaria is the stage of the parasite which emerges from the snail and penetrates the skin of the definitive host.
Species: (1) Haematobium (passed in urine) (2) Mansoni (passed in feces) (3) Japonicum (passed in feces) |

What parasite is this?
|
|
|
Adult schistosoma (Trematoda) in the blood.
Species: (1) Haematobium: In urine (produced by sexual reproduction) (2) Mansoni: In feces (produced by sexual reproduction) (3) Japonicum: In feces (produced by sexual reproduction) |

What parasite is this & where does it leach?
How is it passed into the environment by the definitive host? |
|
|
Adult schistosoma (Trematoda) in the blood.
Species: (1) Haematobium: Humans only (2) Mansoni: Humans & Baboons (3) Japonicum: Humans, Oxen, Canines, Rodents Treatment: Praziquantel Control: Kill parasite to reduce morbidity & transmission, Kill snails (molluscicides), Prevent contamination, Protect from exposure. |

What parasite is this & where does it leach?
Definitive Hosts? Treatment? Control? |
|
|
Adult schistosoma (Trematoda) in the blood.
Species: (1) Haematobium: Africa, Middle East, India (2) Mansoni: Africa, Middle East, Easterb border of South America & Carribean (3) Japonicum: East Asia, Phillapines |

What parasite is this & where does it leach?
Location? |
|
|
Adult schistosoma (Trematoda) in the blood.
Species: (1) Haematobium: Bulinus (2) Mansoni: Biomphalaria (3) Japonicum: Oncomelania Intermediate hosts are all snails |

What parasite is this & where does it leach?
Intermediate hosts? |
|
|
Adult schistosoma (Trematoda) in the mesenteric veins.
Species: (1) Mansoni: Humans & Baboons (2) Japonicum: Humans, Oxen, Canines, Rodents |

What parasite is this & where does it leach?
Definitive hosts? |
|
|
Schistosoma haematobium is transferred by the Bulinus snail.
Symptoms: Clinical symptoms: Swimmer's itch (severe 0-3dy), Schistosomular pneumonitis (schisosomulae migration 3-10dy), Acute schisto or Katayama Fever (onset egg laying->immune complex syndrome 3-8wk w/ eosinophilia) Chronic syndromes: Hydronephrosis, Thickened bladder wall (> 5mm) & pollips (up chance bladder cancer), Occlusion of ureters, Haematuria --> Anemia. |

What parasite does this snail transfer & what is it called?
Symptoms? |
|
|
Schistosoma haematobium (Egg). It is transferred by the Bulinus (Snail).
Notice: (1) Tail is located at the end of the egg. Diagnosis: History, Eggs in urine, Cystoscopy, Gross haematuria (usual), Microhaematuria, Ultrasound-> morbidity assessment. |

What parasite is this?
Diagnosis? |
|
|
Top left: Normal bladder
Top right: Normal kidney Middle left: Polyp in bladder Middle right: Hydronephrosis Bottom left: Polyps in bladder and thickened bladder wall. Bottom right: Severe hydronephrosis Schistosoma haematobium infection can cause polyps and bladder wall thickening increasing the risk of bladder cancer. The damage to the kidneys and bladder are due to the release of eggs by the parasite. |
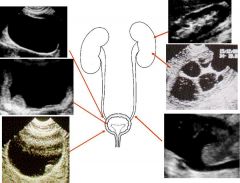
What parasitic infection are these images a sign of?
|
|
|
Schistosoma mansoni (Egg). It is transferred by the Biomphalaria (Snail).
Notice: (1) Notice the tail is located laterally Symptoms: Clinical symptoms: Swimmer's itch (severe 0-3dy), Schistosomular pneumonitis (schisosomulae migration 3-10dy), Acute schisto or Katayama Fever (onset egg laying->immune complex syndrome 3-8wk w/ eosinophilia). Chronic syndromes: (Trapped ova calcify in vessles)--> Portal hypertension, Hepatomegaly, Hematemesis (ruptured esophageal varices->anemia), Splenomegaly, Melania (blood in feces). |

What parasite is this?
Symptoms? |
|
|
Schistosoma mansoni is transferred by the Biomphalaria snail.
Diagnosis: History, Eggs in stool or in rectal biopsy, Rectoscopy & microscopy of rectal snip, Ultrasound-> morbidity assessment |

What parasite does this snail transfer & what is it called?
Diagnosis? |
|
|
Schistosoma japonicum (Egg). It is transferred by the Oncomelania (Snail).
Symptoms: Clinical symptoms: Swimmer's itch (severe 0-3dy), Schistosomular pneumonitis (schisosomulae migration 3-10dy), Acute schisto or Katayama Fever (onset egg laying->immune complex syndrome 3-8wk w/ eosinophilia). Chronic syndromes: (Trapped ova calcify in vessles)--> Portal hypertension, Hepatomegaly, Hematemesis (ruptured esophageal varices->anemia), Splenomegaly, Melania (blood in feces). |

What parasite is this?
Symptoms? |
|
|
Schistosoma japonicum is transferred by the Oncomelania snail.
Diagnosis: History, Eggs in stool or in rectal biopsy, Rectoscopy & microscopy of rectal snip, Ultrasound-> morbidity assessment |

What parasite does this snail transfer & what is it called?
Diagnosis? |
|
|
Echinococcus granulosus (Cestode) in the larval stage called a protoscolicies. This is a cross section of a hydatid cyst in a liver.
Symptoms: 85% of cases are subclinical. Can cause body wide cysts: Lung cysts (predilection): Symptomatic very quickly. Liver cysts (predilection): Symptoms longer to develop. Ocular Cystic Echinococcosis. Treatment: Surgical (not if cyst contact biliary tree): Puncture(cyst), Aspirate(parasites), Inject (alcohol), Reaspirate(fluid). Albendizole. |

What parasite is this?
Symptoms? Treatment? |

