![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
125 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What are the therapeutic effects of morphine sulfate when administered to a patient with cardiogenic pulmonary edema?
|
A: Increased venous capacitance and decreased preload
B: Increased cardiac inotropy and increased cardiac output C: Systemic venous pooling of blood and increased after load D: Decreased venous capacitance and increased inotropy |
A: Increased venous capacitance and decreased preload
|
|
|
A 66-year-old woman is diagnosed with cardiomyopathy. What does this indicate?
|
A: Progressive cardiac weakening
B: An occluded coronary artery C: Strengthening of the ventricles D: An enlarged myocardium |
A: Progressive cardiac weakening
|
|
|
You are assessing a 59-year-old woman who complains of chest pressure. When you are looking at her list of medications, you note that she takes Vasotec. What type of medication is this?
|
A: ACE inhibitor
B: Parasympathetic blocker C: Beta-blocker D: Calcium channel blocker |
A: ACE inhibitor
|
|
|
A patient’s medication regimen includes fluoxetine, Toprol, Proscar, lansoprazole, and Klonopin. Which of these medications is used to treat cardiovascular disorders? |
A: lansoprazole B: Toprol C: Proscar D: fluoxetine |
B: Toprol |
|
|
A 60-year-old female presents with confusion, shortness of breath, and diaphoresis. Her blood pressure is 70/40 mm Hg and her heart rate is 40 beats/min. The cardiac monitor reveals a slow, wide complex rhythm with dissociated P waves. After applying supplemental oxygen, you should:
|
A: start an IV and give 0.5 mg of atropine.
B: start an IV and give a rapid fluid bolus. C: begin immediate transcutaneous pacing. D: give her up to 325 mg of baby aspirin. |
C: begin immediate transcutaneous pacing.
|
|
|
You are attempting to resuscitate a 50-year-old man in cardiac arrest. The patient has a history of congestive heart failure, hypertension, and cirrhosis of the liver. The cardiac monitor reveals a slow, wide complex rhythm. CPR is ongoing and the patient has been intubated. In addition to looking for potentially reversible causes of the patient’s condition, further treatment should include:
|
A: ventilations at a rate of 8 to 10 breaths/min and 1 mg of epinephrine 1:10,000 every 3 to 5 minutes.
B: one breath every 5 to 6 seconds, 40 units of vasopressin every 5 minutes, and transcutaneous pacing. C: hyperventilation for presumed acidosis and 1 mg of epinephrine 1:10,000 every 3 to 5 minutes. D: one breath every 3 to 5 seconds, a 2-liter normal saline bolus, a vasopressor, and a dopamine infusion. |
A: ventilations at a rate of 8 to 10 breaths/min and 1 mg of epinephrine 1:10,000 every 3 to 5 minutes.
|
|
|
Which of the following signs or symptoms occurs more commonly in patients with stable angina than in those with unstable angina?
|
A: Chest pain that begins during exertion
B: ST segment elevation on the 12-lead ECG C: Chest pressure, tightness, or discomfort D: Pain that lasts more than 15 minutes |
A: Chest pain that begins during exertion
|
|
|
You are assessing the cardiac rhythm of a woman with respiratory distress. The rhythm is irregularly irregular with a rate of 120 beats/min. The QRS complexes measure 0.10 seconds in duration, the P wave to QRS ratio is 1:1, and the P waves vary in shape. This cardiac rhythm is MOST likely:
|
A: a wandering atrial pacemaker. B: multifocal atrial tachycardia.
C: atrial flutter with aberrancy. D: atrial fibrillation. |
B: multifocal atrial tachycardia.
|
|
|
A: type I second-degree AV block.
B: complete AV dissociation. C: type II second-degree AV block. D: wandering atrial pacemaker. |
A: type I second-degree AV block.
|
|
|
A transmural myocardial infarction is defined as:
|
A: an MI that involves the entire thickness of the left ventricular wall from endocardium to epicardium.
B: any area of infarcted myocardium that is caused by focal areas of acute coronary vasospasm. C: an MI that occurs without gross ST segment elevation or the presence of a pathologic Q wave. D: multiple areas of myocardial necrosis confined to the inner one third to one half of the left ventricular wall. |
A: an MI that involves the entire thickness of the left ventricular wall from endocardium to epicardium.
|
|
|
You are treating a patient with ventricular fibrillation. As the defibrillator is charging, you should:
|
A: check the defibrillator to ensure the synchronizer is activated.
B: ask your partner to ventilate the patient at 20 breaths/min. C: ensure that CPR is continuing until the defibrillator is charged. D: visually confirm that nobody is touching the patient. |
C: ensure that CPR is continuing until the defibrillator is charged.
|
|
|
A 70-year-old man presents with an acute onset of confusion, slurred speech, and left side weakness. According to his daughter, he has high blood pressure and has had several "small strokes" over the past 6 months. Your partner applies supplemental oxygen; assesses his vital signs, which are stable; and assesses his blood glucose level, which reads 35 mg/dL. You attempt to perform the Cincinnati Prehospital Stroke test, but the patient is unable to understand your instructions. After establishing IV access, you should:
|
A: monitor his cardiac rhythm, withhold glucose in case he is having a hemorrhagic stroke, and transport.
B: give 324 mg of baby aspirin, place him in a supine position, monitor his cardiac rhythm, and transport. C: administer 50% dextrose, monitor his cardiac rhythm, protect his impaired extremities, and transport. D: administer oral glucose, place him in a semi-sitting position, monitor his cardiac rhythm, and transport. |
C: administer 50% dextrose, monitor his cardiac rhythm, protect his impaired extremities, and transport.
|
|
|
A 35-year-old female experienced a syncopal episode shortly after complaining of palpitations. She was reportedly unconscious for less than 10 seconds. Upon your arrival, she is conscious and alert, denies any injuries, and states that she feels fine. She further denies any significant medical history. Her vital signs are stable and the cardiac monitor reveals a sinus rhythm with frequent premature atrial complexes. On the basis of this information, what MOST likely caused her syncopal episode?
|
A: Paroxysmal supraventricular tachycardia
B: A brief episode of ventricular tachycardia C: Aberrant conduction through the ventricles D: A sudden increase in cardiac output |
A: Paroxysmal supraventricular tachycardia
|
|
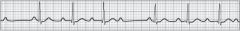
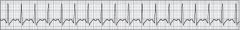
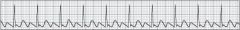
While assessing a middle-aged man who complains of nausea and weakness, he suddenly becomes unresponsive. The cardiac monitor displays the rhythm shown below. After determining that he is apneic and pulseless, you should:
|
A: perform synchronized cardioversion.
B: start an IV and give 300 mg of amiodarone. C: perform CPR for 2 minutes and defibrillate. D: start CPR and prepare to defibrillate. |
D: start CPR and prepare to defibrillate.
|
|
|
Which of the following cardiac rhythms is associated with bradycardia, and is characterized by regular R-R intervals and a greater ratio of P waves to QRS complexes? |
A: Second-degree AV block type II B: First-degree AV block C: Second-degree AV block type I D: Third-degree AV block |
D: Third-degree AV block |
|
|
A 145-pound man requires a dopamine infusion at 15 µg/kg/min for severe hypotension. You have a premixed bag containing 800 mg of dopamine in 500 mL of normal saline. If you are using a microdrip administration set (60 gtts/mL), how many drops per minute should you deliver to achieve the required dose?
|
A: 42
B: 36 C: 30 D: 48 |
B: 36
|
|
|
A 60-year-old man presents with chest discomfort, diaphoresis, and dyspnea. The 12-lead ECG reveals 4-mm ST segment elevation in leads V1 through V4. You should suspect:
|
A: anteroseptal injury.
B: anterolateral injury. C: inferoseptal ischemia. D: anterolateral infarct. |
A: anteroseptal injury.
|
|
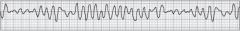
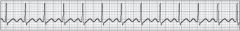
You are transporting a 44-year-old man with shortness of breath. He is conscious alert and is receiving supplemental oxygen. A patent IV line has been established. Suddenly, he develops the rhythm shown below. He is now responsive to pain only; is profusely diaphoretic; and has weak radial pulses. You should:
|
A: give 150 mg of amiodarone IV over 10 minutes.
B: perform synchronized cardioversion with 100 joules. C: give 6 mg of adenosine rapid IV push and reassess. D: assess his BP to determine if he is clinically unstable. |
B: perform synchronized cardioversion with 100 joules.
|
|
|
You are transporting a 62-year-old male who called EMS because of nausea and diarrhea. His past medical history includes high cholesterol, for which he takes Lipitor; he denies any other medical history. His blood pressure is 132/78 mm Hg, pulse is 68 beats/min, and respirations are 16 breaths/min. He is receiving oxygen via nasal cannula and has a patent IV line established. He has been in a normal sinus rhythm, but is now experiencing occasional premature ventricular complexes (PVCs). After noting the PVCs, you should:
|
A: reassess and continue monitoring him.
B: administer 1.5 mg/kg of lidocaine. C: contact the receiving facility immediately. D: give a 250–500 mL normal saline bolus. |
A: reassess and continue monitoring him.
|
|
|
Which of the following ECG findings indicates a pathologic delay at the AV node?
|
A: P-R interval less than 0.12 seconds
B: QRS complex of 0.16 seconds C: P waves of varying morphologies D: P-R interval of 0.28 seconds |
D: P-R interval of 0.28 seconds
|
|
|
When treating an adult patient with a blood pressure of 60/40 mm Hg, confusion, a heart rate of 40 beats/min, and sinus bradycardia on the cardiac monitor, you should administer supplemental oxygen, establish vascular access, and then:
|
A: begin a dopamine infusion to increase blood pressure and improve cerebral perfusion.
B: administer sequential crystalloid fluid boluses until his BP is greater than 100 mm Hg. C: acquire a 12-lead ECG, which may reveal signs of acute myocardial ischemia or injury. D: administer 0.5 mg of atropine sulfate and consider transcutaneous cardiac pacing. |
D: administer 0.5 mg of atropine sulfate and consider transcutaneous cardiac pacing.
|
|
|
A patient experiencing a right ventricular infarction would be expected to present with:
|
A: severe pulmonary edema and hemoptysis.
B: greater than 2-mm ST depression in lead V1. : hypertension and tachycardia. D: ST elevation in leads II, III, and aVF. |
D: ST elevation in leads II, III, and aVF.
|
|
|
Which of the following clinical presentations is MOST consistent with dissection of the ascending aorta?
|
A: Tearing abdominal pain unrelieved by analgesia, pulse deficit in the femoral arteries, lightheadedness, blood in the stool
B: Gradual onset of chest pressure that increases in severity over time, hypotension, tachycardia, bilaterally weak radial pulses C: Sudden onset of lower back pain that radiates to the groin, urge to defecate, pain is constant and moderate in severity D: Acute tearing pain in between the scapulae, blood pressure discrepancy between arms, maximal pain severity from the onset |
D: Acute tearing pain in between the scapulae, blood pressure discrepancy between arms, maximal pain severity from the onset
|
|
|
According to the Los Angeles Prehospital Stroke Screen (LAPSS), the likelihood that a conscious patient with an acute atraumatic neurologic complaint is experiencing a stroke is HIGHEST if he or she:
|
A: has a symmetrical face upon smiling.
B: has a blood glucose level of 750 mg/dL. C: does not have a history of seizures. D: is normally bedridden or wheelchair bound. |
C: does not have a history of seizures.
|
|
|
In the context of an acute coronary syndrome, the presence of dyspnea should make you MOST suspicious for:
|
A: severe anxiety.
B: pulmonary congestion. C: cor pulmonale. D: diffuse bronchospasm. |
B: pulmonary congestion.
|
|
|
You and your team are performing CPR on a 70-year-old male. The cardiac monitor reveals a slow, organized rhythm. His wife tells you that he goes to dialysis every day, but has missed his last three treatments. She also tells you that he has high blood pressure, hyperthyroidism, and has had several cardiac bypass surgeries. Based on the patient's medical history, which of the following conditions is the MOST likely underlying cause of his condition?
|
A: Hyperkalemia
B: Coronary thrombus C: Drug toxicity D: Hypovolemia |
A: Hyperkalemia
|
|
|
In addition to CPR, the recommended treatment sequence for an unresponsive, apneic, and pulseless patient with a regular, wide-complex cardiac rhythm at a rate of 40 beats/min includes:
|
A: transcutaneous cardiac pacing and 1 mg of epinephrine every 3 to 5 minutes.
B: 1 mg of epinephrine every 3 to 5 minutes and treating reversible causes. C: 40 units of vasopressin every 10 minutes and treating reversible causes. D: 1 mg of epinephrine every 3 to 5 minutes and 1 gram of calcium chloride. |
B: 1 mg of epinephrine every 3 to 5 minutes and treating reversible causes.
|
|
|
You are called to a local supermarket where a customer collapsed. When you arrive, two bystanders are performing CPR on the patient. You should:
|
A: perform a precordial thump and assess for a carotid pulse.
B: assess the patient to confirm pulselessness and apnea. : immediately assess the patient's cardiac rhythm. D: verify the effectiveness of the bystander’s CPR. |
B: assess the patient to confirm pulselessness and apnea.
|
|
|
ECG indicators of Wolff-Parkinson-White (WPW) syndrome include:
|
A: short PR intervals, delta waves, and QRS widening.
B: delta waves, flattened T waves, and bradycardia. C: narrow QRS complexes and peaked T waves. D: tall P waves, QT interval prolongation, and tachycardia. |
A: short PR intervals, delta waves, and QRS widening.
|
|
|
You and your team are performing CPR on a middle-aged male who presented with asystole. After 2 minutes of CPR, you reassess him and note that his cardiac rhythm has changed to ventricular fibrillation. You should:
|
A: defibrillate and then resume CPR.
B: defibrillate after 2 more minutes of CPR. C: make sure the leads are still attached. D: assess for a carotid pulse for 5 seconds. |
A: defibrillate and then resume CPR
|
|
|
When assessing a patient's pulse, you note that it is fast and has an irregularly irregular pattern. On the basis of these findings, which of the following cardiac rhythms would MOST likely be seen on the cardiac monitor?
|
A: Supraventricular tachycardia B: Ventricular tachycardia
C: Second-degree AV block type 1 D: Uncontrolled atrial fibrillation |
D: Uncontrolled atrial fibrillation
|
|
|
A middle-aged man presents with chest discomfort, shortness of breath, and nausea. You give him supplemental oxygen and continue your assessment. As your partner is attaching the ECG leads, you should:
|
A: administer 0.4 mg of nitroglycerin.
B: establish vascular access. C: administer 2 to 4 mg of morphine IM. D: administer up to 325 mg of aspirin. |
D: administer up to 325 mg of aspirin.
|
|
|
An older man is suddenly awakened in the middle of the night, gasping for air. He is extremely restless and pale, and is coughing up blood. His clinical presentation is MOST consistent with:
|
A: left side heart failure.
B: gastrointestinal bleed. C: right side heart failure. D: unstable angina. |
A: left side heart failure.
|
|
|
A 59-year-old woman presents with a regular, narrow-complex tachycardia at a rate of 180 beats/min. She is conscious and alert, but complains of chest discomfort and has a blood pressure of 86/56 mm Hg. In addition to giving her supplemental oxygen, you should:
|
A: give her up to 3 sublingual doses of nitroglycerin.
B: administer 150 mg of amiodarone over 10 min. C: administer 12 mg of adenosine rapid IV push. D: have her chew and swallow 325 mg of aspirin. |
D: have her chew and swallow 325 mg of aspirin.
|
|
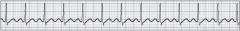
An elderly man is apneic and pulseless. The ECG shows the following rhythm, which you should interpret as:
|
A: sinus bradycardia.
B: first-degree AV block. C: sinus tachycardia. D: normal sinus rhythm. |
C: sinus tachycardia.
|
|
|
When assessing a patient with sinus tachycardia at a rate of 135 beats/min, you should recall that:
|
A: a heart rate greater than 130 beats/min often causes significant hemodynamic compromise. B: tachycardia in a patient with cardiac ischemia is beneficial in that it improves coronary perfusion.
C: the preferred treatment for tachycardia less than 150 beats/min is a calcium channel blocker. D: rate-related symptoms are uncommon in patients with a heart rate less than 150 beats/min. |
D: rate-related symptoms are uncommon in patients with a heart rate less than 150 beats/min.
|
|
|
During your SAMPLE history of an elderly man, he tells you that his cardiologist told him that he has an “irregular heartbeat.” His medications include warfarin sodium and digoxin. On the basis of this information, what underlying cardiac rhythm should you suspect?
|
A: AV heart block
B: Sinus dysrhythmia C: Atrial fibrillation D: Atrial tachycardia |
C: Atrial fibrillation
|
|
|
Which of the following electrolytes moves slowly into the cardiac cell and maintains the depolarized state of the cell membrane?
|
A: Potassium
B: Sodium C: Magnesium D: Calcium |
D: Calcium
|
|
|
A clinically unstable patient presents with an irregular narrow-complex tachycardia at a rate of 170 per minute. What is the recommended initial energy setting for synchronized cardioversion?
|
A: 120 to 200 joules
B: 200 to 300 joules C: 50 to 100 joules D: 320 to 360 joules |
A: 120 to 200 joules
|
|
|
On the 12-lead ECG, the high lateral wall of the left ventricle is viewed by leads:
|
A: V1 and V2.
B: I and aVL. C: III and aVF. D: V5 and V6. |
B: I and aVL.
|
|
|
You respond to a residence for a 68-year-old male with nausea, vomiting, and blurred vision. As you are assessing him, he tells you that he has congestive heart failure and atrial fibrillation, and takes numerous medications. The cardiac monitor reveals atrial fibrillation with a ventricular rate of 50 beats/min. Which of the following medications is MOST likely responsible for this patient's clinical presentation?
|
A: Furosemide
B: Digoxin C: Warfarin D: Vasotec |
B: Digoxin
|
|
|
A 47-year-old male took two of his prescribed nitroglycerin tablets prior to calling EMS. When you arrive at the scene, the patient tells you that he has a throbbing headache and is still experiencing chest pain. Your MOST immediate suspicion should be that:
|
A: his chest pain is probably not of a cardiac origin.
B: permanent myocardial damage has already occurred. C: his nitroglycerin is outdated or has lost its potency. D: he is experiencing continued myocardial ischemia. |
D: he is experiencing continued myocardial ischemia.
|
|
|
What are the therapeutic effects of aspirin when given to patients experiencing an acute coronary syndrome?
|
A: Prevents platelet aggregation B: Direct blood-thinning effect
C: Increases platelet production D: Dilates the coronary arteries |
A: Prevents platelet aggregation
|
|
|
Which of the following represents the correct medication sequence when treating a patient with a suspected acute coronary syndrome?
|
A: Oxygen, aspirin, nitroglycerin, and morphine
B: Oxygen, aspirin, morphine, and nitroglycerin C: Oxygen, nitroglycerin, aspirin, and morphine D: Oxygen, morphine, aspirin, and nitroglycerin |
A: Oxygen, aspirin, nitroglycerin, and morphine
|
|
|
Which of the following interventions has the greatest impact on patient survival from sudden cardiac arrest?
|
A: Early CPR and defibrillation
B: Advanced airway control C: Cardiac medication administration D: Identifying the cause |
A: Early CPR and defibrillation
|
|
|
Which of the following clinical presentations is MOST consistent with an acute ischemic stroke involving the left cerebral hemisphere?
|
A: Dysphasia, confusion, left side hemiparesis, right side facial droop
B: Aphasia, lethargy, right side hemiparalysis, right side facial droop C: Decerebrate posturing, asymmetric pupils, hypertension, bradycardia D: Dysarthria, confusion, right side hemiparesis, left side facial droop |
D: Dysarthria, confusion, right side hemiparesis, left side facial droop
|
|
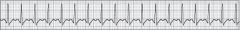
A 70-year-old woman was suddenly awakened with the feeling that she was suffocating. She is anxious, is laboring to breathe, and has dried blood on her lips. The ECG shows the cardiac rhythm below. Which of the following pathophysiologies BEST explains her clinical presentation?
|
A: Decreased stroke volume with left heart failure
B: Increased stroke volume with right heart failure C: Increased preload with left heart failure D: Decreased preload with right heart failure |
A: Decreased stroke volume with left heart failure
|
|
|
You are assessing a man with a acute chest pain. As you are inquiring about the quality of his pain, he clenches his fist. This is called __________ sign and nonverbally conveys a feeling of:
|
A: Cullen’s, dullness.
B: Beck’s, impending doom. C: Levine’s, pressure. D: Grey-Turner’s, fluttering |
C: Levine’s, pressure.
|
|
|
If a patient was experiencing acute injury involving the interventricular septum and anterior wall of the left ventricle, you would expect the 12-lead ECG to reveal:
|
A: Inverted T waves in all of the precordial leads.
B: ST segment elevation in leads V5, V6, I, and aVL. C: ST segment elevation in leads V1 through V4. D: ST segment depression in leads II, III, and aVF. |
C: ST segment elevation in leads V1 through V4.
|
|
|
Immediately following return of spontaneous circulation, the paramedic should:
|
A: assess the patient’s blood pressure.
B: induce therapeutic hypothermia. C: reassess the patient’s ventilatory status. D: provide a bolus of normal saline solution. |
C: reassess the patient’s ventilatory status.
|
|
|
You are assessing a middle-aged female who complains of chest discomfort. She is conscious, alert, and oriented. Her skin is diaphoretic. Her blood pressure is 122/72 mm Hg, her pulse rate is 120 beats/min, and her respirations are 20 breaths/min. On the basis of her chief complaint, which of your assessment findings is the MOST significant?
|
A: Diaphoresis
B: Mental status C: Pulse rate of 120 beats/min D: Elevated respiratory rate |
C: Pulse rate of 120 beats/min
|
|
|
What occurs at the beginning of ventricular contraction?
|
A: Increased ventricular pressure causes the ventricular walls to stretch.
B: Additional blood fills the ventricles secondary to atrial kick. C: The pulmonic and aortic valves close and the tricuspid and mitral valves open. D: The atrioventricular valves close and the semilunar valves are forced open. |
D: The atrioventricular valves close and the semilunar valves are forced open.
|
|
A 56-year-old man presents with the cardiac rhythm shown below. He complains of chest discomfort, shortness of breath, and is profusely diaphoretic. His blood pressure is 84/64 mm Hg and his radial pulses are barely palpable. You should:
|
A: defibrillate with 200 biphasic joules.
B: prepare for immediate cardiac pacing. C: give 150 mg of amiodarone over 10 minutes. D: consider sedation and perform cardioversion. |
D: consider sedation and perform cardioversion.
|
|
|
A 54-year-old man presents with chest pressure, confusion, and profuse diaphoresis. As your partner administers supplemental oxygen, you apply the cardiac monitor. In lead II, you observe a wide QRS complex rhythm with dissociated P waves and a ventricular rate of 35 beats/min. You should:
|
A: begin transcutaneous pacing at once.
B: obtain a complete set of vital signs. C: start an IV and give 0.5 mg of atropine. D: immediately obtain a 12-lead ECG. |
A: begin transcutaneous pacing at once.
|
|
|
When attempting transcutaneous cardiac pacing (TCP), you will know that electrical capture has been achieved when:
|
A: you see an increase in the number of narrow QRS complexes.
B: each pacemaker spike is followed by a wide QRS complex. C: the patient’s inherent heart rate spontaneously increases. D: the milliamp setting is at least 40 and the patient is in pain. |
B: each pacemaker spike is followed by a wide QRS complex.
|
|
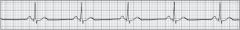
The MOST appropriate initial action for a 54-year-old man who presents with the following cardiac rhythm should consist of:
|
A: administering 0.5 mg of atropine sulfate.
B: assessing the patient’s clinical status. C: preparing for transcutaneous pacing. D: quickly establishing vascular access. |
B: assessing the patient’s clinical status.
|
|
A 70-year-old man presents with the cardiac rhythm shown below. He is confused, is slow to answer your questions, and is profusely diaphoretic. His blood pressure is 76/54 mm Hg, his pulse is rapid and weak, and his respirations are 22 breaths/min and labored. He is receiving high-flow oxygen and your partner has established a patent IV line. You should:
|
A: Administer 150 mg of amiodarone over 10 minutes
B: Attempt vagal maneuvers and then consider adenosine C: Administer a 500-mL normal saline bolus and reassess D: Consider sedation and then cardiovert with 100 joules |
D: Consider sedation and then cardiovert with 100 joules
|
|
|
You are treating a 68-year-old woman with chest pressure and shortness of breath that started 2 days ago. Her BP is 76/52 mm Hg and her pulse is 130 beats/min and weak. The cardiac monitor reveals sinus tachycardia with occasional PVCs and auscultation of her lungs reveals diffuse coarse crackles. Which of the following treatment interventions is MOST appropriate for this patient?
|
A: Dopamine, 2 to 20 µg/kg/min.
B: Normal saline, 20 mL/kg rapid bolus. C: Amiodarone, 150 mg over 10 min. D: Nitroglycerin, 10 to 20 µg/min. |
A: Dopamine, 2 to 20 µg/kg/min.
|
|
|
A 56-year-old man has had chest pain for the past 2 days, but refused to go to the hospital. His wife called EMS when she noticed that he was not acting right. He is conscious, but confused, and is diaphoretic. His BP is 80/40 mm Hg and his pulse is rapid and weak. The patient's history and your assessment findings are MOST consistent with:
|
A: cardiogenic hypoperfusion.
B: unstable angina pectoris. C: acute ischemic stroke. D: acute myocardial infarction. |
A: cardiogenic hypoperfusion.
|
|
|
What is the correct initial dose and rate of administration of amiodarone for a patient with refractory ventricular fibrillation?
|
A: 150 mg given over 10 minutes B: 300 mg given over 10 minutes C: 150 mg via rapid IV or IO push D: 300 mg via rapid IV or IO push
|
D: 300 mg via rapid IV or IO push
|
|
|
Ventricular ejection fraction is defined as the:
|
A: percentage of blood in the ventricle pumped out during a contraction.
B: volume of blood pumped into the left ventricle from the left atrium. C: amount of blood pumped from either ventricle each minute. D: amount of blood pumped out from either ventricle per contraction. |
A: percentage of blood in the ventricle pumped out during a contraction.
|
|
|
Which of the following causes of pulseless electrical activity (PEA) would be the MOST likely to respond to immediate treatment in the prehospital setting?
|
A: Hypokalemia
B: Lactic acidosis C: Drug overdose D: Hypovolemia |
D: Hypovolemia
|
|
|
In contrast to unstable angina, stable angina occurs when a patient:
|
A: complains of chest pain at the same time of the day for more than 2 weeks.
B: experiences chest discomfort after a certain, predictable amount of exertion. C: needs more than two nitroglycerin treatments to relieve his or her chest pain. D: presents with chest pain or discomfort during periods of low oxygen demand. |
B: experiences chest discomfort after a certain, predictable amount of exertion.
|
|
|
A 56-year-old man has had chest pain for the past 2 days, but refused to go to the hospital. His wife called EMS when she noticed that he was not acting right. He is conscious, but confused, and is diaphoretic. His BP is 80/40 mm Hg and his pulse is rapid and weak. The patient's history and your assessment findings are MOST consistent with:
|
A: unstable angina pectoris.
B: acute myocardial infarction. C: cardiogenic hypoperfusion. D: acute ischemic stroke. |
C: cardiogenic hypoperfusion.
|
|
|
Sudden cardiac arrest in the adult population is MOST often secondary to:
|
A: a cardiac dysrhythmia.
B: accidental electrocution. C: respiratory failure. D: massive hypovolemia. |
A: a cardiac dysrhythmia.
|
|
|
You are evaluating a regular cardiac rhythm in lead II. The rate is 90 beats/min, the QRS complexes consistently measure 0.16 seconds, and inverted P waves are seen immediately following each QRS complex. The rhythm described is MOST characteristic of a/an:
|
A: second-degree AV block with abnormal ventricular conduction. B: accelerated junctional rhythm with ventricular aberrancy.
C: wandering atrial pacemaker with a bundle branch block. D: ectopic atrial rhythm with a ventricular conduction delay. |
B: accelerated junctional rhythm with ventricular aberrancy.
|
|
|
A 39-year-old female presents with an acute onset of lightheadedness. The cardiac monitor reveals a tachycardic rhythm at 170 beats/min with QRS complexes that measure 0.08 seconds in duration. Despite vagal maneuvers and adenosine, her cardiac rhythm remains unchanged. She is conscious and alert, has a blood pressure of 118/72 mm Hg, and denies shortness of breath or chest discomfort. You should:
|
A: perform synchronized cardioversion with 50 joules.
B: administer 150 mg of amiodarone over 10 minutes. C: consider that her rhythm is ventricular in origin. D: transport immediately and monitor her en route. |
D: transport immediately and monitor her en route.
|
|
|
A 49-year-old male complains of generalized weakness that began about a week ago. He is conscious and alert and is breathing adequately. His blood pressure is 138/78 mm Hg, pulse is 130 beats/min and irregular, and respirations are 14 breaths/min. You administer supplemental oxygen and apply the cardiac monitor, which reveals atrial fibrillation; a 12-lead ECG tracing reveals the same. The patient denies any significant medical problems and takes no medications. After establishing IV access, you should:
|
A: sedate with midazolam and perform synchronized cardioversion.
B: administer 0.25 mg/kg of diltiazem and transport for evaluation. C: give 150 mg of amiodarone over 10 minutes and transport. D: attempt vagal maneuvers and then give 6 mg of adenosine IV push. |
B: administer 0.25 mg/kg of diltiazem and transport for evaluation.
|
|
|
In older adults, an S3 heart sound:
|
A: is generally very pronounced. B: indicates mitral valve closure. C: signifies moderate heart failure.
D: is considered a normal variant. |
C: signifies moderate heart failure.
|
|
|
Atropine sulfate exerts its therapeutic effect by:
|
A: increasing cardiac contractility.
B: stimulating alpha receptors. C: opposing the vagus nerve. D: blocking sympathetic activity |
C: opposing the vagus nerve.
|
|
|
Which of the following statements regarding the use of vasopressin in cardiac arrest is correct?
|
A: Vasopressin is highly effective in treating pediatric cardiac arrest patients
B: Vasopressin is superior to epinephrine and should be used when possible C: Vasopressin should be given every 3 to 5 minutes throughout the arrest D: Vasopressin can be used to replace the first or second dose of epinephrine |
D: Vasopressin can be used to replace the first or second dose of epinephrine
|
|
|
When assessing a patient with suspected cardiac-related chest pain, which of the following questions would be MOST appropriate to ask?
|
A: Is the pain crushing or dull in nature?
B: Does the pain move to your arms? C: Can you describe the quality of the pain? D: Were you at rest when the pain began? |
C: Can you describe the quality of the pain?
|
|
|
Where is the point of maximal impulse (PMI) located in most people?
|
A: Left anterior chest, on the left sternal border, at the fourth intercostal space
B: Left anterolateral chest, in the midaxillary line, at the fifth intercostal space C: Left anterior chest, in the midclavicular line, at the fifth intercostal space D: Directly over the sternum, approximately 1” to the left of the angle of Louis |
C: Left anterior chest, in the midclavicular line, at the fifth intercostal space
|
|
|
When administering epinephrine to a patient in cardiac arrest, the MAIN desired effect is:
|
A: vasoconstriction, which improves coronary and cerebral perfusion.
B: bronchodilation, which facilitates positive-pressure ventilation. C: beta-1 receptor stimulation, which increases cardiac contractility. D: coronary artery dilation, which decreases the myocardial workload. |
A: vasoconstriction, which improves coronary and cerebral perfusion.
|
|
|
In which of the following situations is transcutaneous cardiac pacing (TCP) clearly indicated?
|
A: Pulseless electrical activity at a rate of 50 beats/min.
B: Asystole, but only after 10 minutes of adequate CPR. C: Third-degree AV block in a patient with pulmonary edema. D: First-degree AV block in a patient with abdominal pain. |
C: Third-degree AV block in a patient with pulmonary edema.
|
|
|
What is the therapeutic effect of aspirin when administered to a patient experiencing an acute coronary syndrome (ACS)?
|
A: Decreased platelet production and coronary artery vasoconstriction
B: Destruction of a blood clot in a coronary artery by destroying fibrin C: Destruction of platelets by increasing thromboxane A2 production D: Decreased thromboxane A2 production, which inhibits platelet aggregation |
D: Decreased thromboxane A2 production, which inhibits platelet aggregation
|
|
|
During resuscitation of a 60-year-old man with ventricular fibrillation, you restore spontaneous circulation following CPR, defibrillation, two doses of epinephrine, and one dose of amiodarone. The patient remains unresponsive and apneic. Which of the following represents the MOST appropriate post-arrest care for this patient?
|
A: Ventilate at a rate of 20 breaths/min, begin an epinephrine infusion to maintain perfusion, and keep the patient warm
B: Ventilate at a rate of 8 to 10 breaths/min, support blood pressure, and give 150 mg of amiodarone over 10 minutes C: Ventilate at a rate of 10 to 12 breaths/min, support blood pressure, and consider therapeutic hypothermia D: Hyperventilate the patient, administer a normal saline bolus, and begin an amiodarone infusion at 0.5 mg/min |
C: Ventilate at a rate of 10 to 12 breaths/min, support blood pressure, and consider therapeutic hypothermia
|
|
|
Which of the following 12-lead ECG findings signifies a left bundle branch block?
|
A: QRS duration of 122 ms; terminal S wave in lead V6
B: QRS duration of 124 ms; terminal S wave in lead V1 C: QRS duration of 126 ms; terminal S wave in lead aVL D: QRS duration of 128 ms; terminal R wave in lead V1 |
B: QRS duration of 124 ms; terminal S wave in lead V1
|
|
|
A 61-year-old male presents with chest pressure that woke him up from his nap 30 minutes ago. He is diaphoretic, anxious, and rates his pain as an an 8 over 10. His past medical history is significant for hypertension, type II diabetes, and coronary stent placement 2 months ago. He takes lisinopril, Plavix, and Glucophage, and is wearing a medical alert bracelet stating "allergic to salicylates." His blood pressure is 160/100 mm Hg, pulse is 110 beats/min, and respirations are 22 breaths/min. The 12-lead ECG shows sinus tachycardia with 3-mm ST segment elevation in leads V1 through V5. Which of the following treatment modalities is MOST appropriate for this patient?
|
A: 325 mg of baby aspirin, supplemental oxygen, vascular access, up to three doses of nitroglycerin, and up to 10 mg of morphine if his systolic BP is greater than 120 mm Hg and he is still in pain
B: High-flow oxygen via nonrebreathing mask, a right-sided 12-lead ECG, vascular access, 0.25 mg/kg of diltiazem, and application of pacing pads in case he becomes bradycardic C: 325 mg of baby aspirin; high-flow oxygen via nonrebreathing mask; vascular access; and 1 µg/kg of fentanyl to relieve his pain, treat his anxiety, and lower his BP D: Supplemental oxygen, vascular access, up to three 0.4 mg doses of nitroglycerin, and 2 to 4 mg of morphine sulfate if his systolic BP is greater than 90 mm Hg and he is still experiencing pain |
D: Supplemental oxygen, vascular access, up to three 0.4 mg doses of nitroglycerin, and 2 to 4 mg of morphine sulfate if his systolic BP is greater than 90 mm Hg and he is still experiencing pain
|
|
|
A 30-year-old man complains of nausea and one episode of vomiting. He is conscious and alert and states that he has a slight headache. He denies chest pain or shortness of breath, and his skin is pink, warm, and dry. His BP is 136/88 mm Hg, pulse is 44 beats/min and strong, and respirations are 14 breaths/min and unlabored. The cardiac monitor reveals sinus bradycardia. Treatment for this patient should include:
|
A: high-flow oxygen and 0.5 mg atropine IV push.
B: supportive care and transport to the hospital. C: high-flow oxygen and a 20 mL/kg fluid bolus. D: 2 to 10 µg/min of epinephrine via IV infusion. |
B: supportive care and transport to the hospital.
|
|
|
Which of the following represents the MOST appropriate initial drug and dose that is given to all adult patients in cardiac arrest?
|
A: 40 units of vasopressin every 3 to 5 minutes
B: 0.1 mg/kg of epinephrine every 3 to 5 minutes C: 10 mL of epinephrine 1:10,000 every 3 to 5 minutes D: 1 mg of epinephrine 1:1,000 every 3 to 5 minutes |
C: 10 mL of epinephrine 1:10,000 every 3 to 5 minutes
|
|
|
Which of the following is an absolute contraindication for fibrinolytic therapy?
|
A: BP of 170/100 mm Hg on presentation
B: Current use of anticoagulant medication C: Subdural hematoma 3 years ago D: Ischemic stroke within the last 6 months |
C: Subdural hematoma 3 years ago
|
|
|
Which of the following findings is MOST suggestive of right-sided heart failure?
|
A: Persistent orthopnea
B: Engorged jugular veins C: Nocturnal dyspnea D: Blood-tinged sputum |
B: Engorged jugular veins
|
|
|
You are preparing to defibrillate a patient in cardiac arrest with a manual biphasic defibrillator, but are unsure of the appropriate initial energy setting. What should you do?
|
A: Deliver one shock with 200 joules and resume CPR.
B: Deliver three sequential shocks with 120 joules. C: Contact medical control for further guidance. D: Continue CPR and shock with 360 joules in 2 minutes. |
A: Deliver one shock with 200 joules and resume CPR.
|
|
|
A middle-aged man is found unresponsive, pulseless, and apneic. His cardiac arrest was not witnessed, although his skin is still warm to the touch. You should:
|
A: begin immediate high-quality CPR.
B: insert an advanced airway device. C: assess his need for defibrillation. D: administer a precordial thump. |
A: begin immediate high-quality CPR.
|
|
|
The appropriate second dose and method of administration of amiodarone for a patient with refractory ventricular fibrillation is:
|
A: 150 mg given over 10 minutes. B: 150 mg via rapid IV/IO push.
C: 300 mg given over 10 minutes. D: 300 mg via rapid IV/IO push. |
B: 150 mg via rapid IV/IO push.
|
|
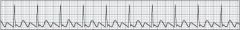
You should interpret the following cardiac rhythm as:
|
A: uncontrolled atrial fibrillation.B: atrial flutter with a variable block.
C: atrial flutter with a fixed block.D: second-degree AV block type II. |
C: atrial flutter with a fixed block.
|
|
|
Assessment and treatment of a responsive adult with a suspected acute coronary syndrome (ACS) might include all of the following, EXCEPT:
|
A: obtaining a 12-lead electrocardiogram.
B: administering 2 to 5 mg of morphine sulfate. C: asking the patient if she has a cardiac history. D: administering lidocaine at a dose of 1.5 mg/kg. |
D: administering lidocaine at a dose of 1.5 mg/kg.
|
|
|
The initial dose of diltiazem for a 165-pound patient is approximately:
|
A: 17 mg.
B: 19 mg. C: 22 mg. D: 25 mg. |
B: 19 mg.
|
|
|
You are assessing a 75-year-old male who experienced a sudden onset of slurred speech, a right-sided facial droop, and left-sided hemiparesis approximately 45 minutes ago. His blood pressure is 170/94 mm Hg, pulse rate is 68 beats/min and irregular, and respirations are 14 breaths/min and unlabored. His oxygen saturation is 94% on room air. The MOST appropriate treatment for this patient includes:
|
A: 160 to 325 mg of aspirin, supplemental oxygen via nasal cannula, cardiac monitoring, blood glucose assessment, an IV of an isotonic crystalloid, and transport.
B: assisted ventilation with a bag-mask device, cardiac monitoring, an IV of normal saline, IV dextrose if his blood glucose level is less than 80 mg/dL, and transport. C: supplemental oxygen via nasal cannula, cardiac monitoring, blood glucose assessment, an IV of normal saline set to keep the vein open, and prompt transport. D: oxygen via nonrebreathing mask, an IV of normal saline, cardiac monitoring, 5 mg of labetalol to lower his BP, blood glucose assessment, and rapid transport. |
C: supplemental oxygen via nasal cannula, cardiac monitoring, blood glucose assessment, an IV of normal saline set to keep the vein open, and prompt transport.
|
|
|
What are the physiologic effects of nitroglycerin when given to patients with cardiac-related chest pain, pressure, or discomfort?
|
A: Smooth muscle relaxation and decreased preload
B: Analgesia, vasoconstriction, and increased preload C: Increased afterload and vascular constriction D: Increased venous return to the right side of the heart |
A: Smooth muscle relaxation and decreased preload
|
|
|
You arrive approximately 8 minutes after a 51-year-old male collapsed at a family event. After determining that he is unresponsive and apneic, you should:
|
A: give 2 rescue breaths and check for a pulse.
B: immediately assess the patient's cardiac rhythm. C: assess for a carotid pulse for 5 to 10 seconds. D: begin CPR, starting with chest compressions. |
C: assess for a carotid pulse for 5 to 10 seconds.
|
|
|
Which of the following statements regarding right ventricular failure (RVF) is correct?
|
A: Fluid boluses are contraindicated in patients with RVF.
B: RVF most often leads to pulmonary hypertension. C: Morphine is the drug of choice for patients with RVF. D: Sacral and pedal edema are common signs of RVF. |
D: Sacral and pedal edema are common signs of RVF.
|
|
After determining that an elderly man is pulseless and apneic, you and your team begin CPR and briefly pause to assess his cardiac rhythm, which is shown below. After resuming CPR, you should:
|
A: give 1 mEq of sodium bicarbonate to rule out acidosis.
B: establish vascular access and give 1 mg of epinephrine. C: prepare to cardiovert the patient at 50 to 100 joules. D: insert an advanced airway as CPR is briefly paused. |
B: establish vascular access and give 1 mg of epinephrine
|
|
|
A 72-year-old male presents with an acute onset of confusion, slurred speech, and decreased movement of his right arm. The patient’s wife tells you that this began about 20 minutes ago, and that he was fine before that. He has type II diabetes, hypertension, and atrial fibrillation. Given this patient’s clinical presentation and past medical history, you should be MOST suspicious that he has:
|
A: acute hypoglycemia.
B: a space-occupying intracranial lesion. C: an acute epidural hemorrhage. D: an occluded cerebral artery. |
D: an occluded cerebral artery.
|
|
|
You and your team are attempting to resuscitate a 66-year-old man in cardiac arrest. The cardiac monitor reveals a slow, wide-complex rhythm. The patient has been successfully intubated and an IV line has been established. As CPR is ongoing, you should:
|
A: administer 10 mL of epinephrine 1:10,000 IV.
B: ventilate the patient at a rate of 24 breaths/min. C: attempt transcutaneous pacing to increase the heart rate. D: give 40 units of vasopressin every 3 to 5 minutes. |
A: administer 10 mL of epinephrine 1:10,000 IV.
|
|
|
You are transporting a 60-year-old woman with chest discomfort and diaphoresis. The 12-lead ECG indicates an acute anterior wall MI. The patient is receiving oxygen and an IV has been established. You have administered 324 mg of aspirin, 3 sublingual nitroglycerin, and 5 mg of morphine. Which of the following should concern you the MOST during transport?
|
A: Respiratory depression
B: Completely relieving her pain C: Severe hypotension D: An acute cardiac dysrhythmia |
D: An acute cardiac dysrhythmia
|
|
|
Which of the following represents the correct adult dosing regimen for adenosine?
|
A: 6 mg, followed by 6 mg in 2 minutes if needed
B: 12 mg, followed by 12 mg in 2 minutes if needed C: 36 mg, divided in 12 mg increments 2 minutes apart D: 6 mg, followed by 12 mg in 2 minutes if needed |
D: 6 mg, followed by 12 mg in 2 minutes if needed
|
|
A 44-year-old man presents with the rhythm shown below. He complains of nausea, but denies vomiting. He is conscious and alert with a BP of 122/62 mm Hg, a pulse rate of 98 beats/min, and respirations of 16 breaths/min and unlabored. Treatment for this patient would MOST likely include:
|
A: cardioversion.
B: diltiazem, 0.25 mg/kg. C: ondansetron, 4 mg. D: amiodarone, 150 mg. |
C: ondansetron, 4 mg.
|
|
|
You are assessing a 67-year-old female with chest discomfort when she becomes unresponsive, apneic, and pulseless. The cardiac monitor reveals coarse ventricular fibrillation. You achieve return of spontaneous circulation after 6 minutes and the cardiac monitor now reveals a narrow complex rhythm. The patient is still unresponsive, has occasional respirations, a blood pressure of 70/40 mm Hg, and a weak pulse of 70 beats/min. The MOST appropriate postresuscitation care for this patient includes:
|
A: insertion of an airway adjunct, assisted ventilation, vascular access, a 500-mL crystalloid bolus, an antidysrhythmic, and consideration for induced hypothermia.
B: prompt insertion of a multilumen airway device, ventilatory assistance, vascular access, 150 mg of amiodarone over 10 minutes, and 0.5 mg of atropine sulfate. C: preoxygenation with a bag-mask device and high-flow oxygen, endotracheal intubation, vascular access, 300 mg of amiodarone, and a dopamine infusion. D: high-flow oxygen via nonrebreathing mask, vascular access, a lidocaine infusion, and an adequate volume of normal saline solution to increase her blood pressure. |
A: insertion of an airway adjunct, assisted ventilation, vascular access, a 500-mL crystalloid bolus, an antidysrhythmic, and consideration for induced hypothermia.
|
|
|
A 50-year-old woman is pulseless and apneic. Your partner and an emergency medical responder are performing well-coordinated CPR. After 2 minutes of CPR, the cardiac monitor reveals coarse ventricular fibrillation. You should:
|
A: defibrillate at once and then reassess the rhythm and pulse.
B: assess for a carotid pulse for no longer than 10 seconds. C: shock the patient three times with 360 monophasic joules. D: deliver a single shock and immediately resume CPR. |
D: deliver a single shock and immediately resume CPR.
|
|
|
A 59-year-old male with a monomorphic wide-complex tachycardia at a rate of 220/min, a blood pressure of 80/50 mm Hg, and a decreased level of consciousness, should be treated with:
|
A: synchronized cardioversion.
B: 2 g of magnesium sulfate. C: 150 mg of amiodarone IV. D: monophasic defibrillation. |
A: synchronized cardioversion.
|
|
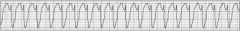
A patient with acute chest discomfort displays the cardiac rhythm shown below. Which of the following is the MOST detrimental effect that this rhythm can have on the patient?
|
A:Increased nervousness and anxiety
B: Increased myocardial oxygen demand C: Decreased myocardial irritability D: Decreased myocardial contractility |
B: Increased myocardial oxygen demand
|
|

You should interpret the following cardiac rhythm as:
|
A: third-degree AV block.
B: first-degree AV block. C: second-degree AV block type II. D: second-degree AV block type I |
A: third-degree AV block.
|
|
|
You are assessing a 50-year-old man with acute chest pressure, diaphoresis, and nausea. The 12-lead ECG tracing reveals 3-mm ST segment elevation in leads V3 through V6. This indicates:
|
A: anteroseptal ischemia.
B: anterolateral injury. C: inferior injury. D: lateral ischemia. |
B: anterolateral injury
|
|
|
When administering a sympathomimetic medication, you must be alert for:
|
A: acute hypotension.
B: cardiac arrhythmias. C: severe bradycardia. D: acute respiratory failure |
B: cardiac arrhythmias.
|
|
|
Appropriate treatment for asystole includes:
|
A: supraglottic airway placement and antidysrhythmic therapy.
B: transcutaneous cardiac pacing and epinephrine 1:10,000. C: epinephrine 1:10,000 and advanced airway management. D: vasopressin every 3 to 5 minutes and tracheal intubation |
C: epinephrine 1:10,000 and advanced airway management.
|
|
|
Which of the following ECG lead configurations is correct?
|
A: To assess lead I, place the positive lead on the right arm and the negative lead on the left arm.B: To assess lead III, place the negative lead on the left leg and the positive lead on the right arm.C: To assess lead II, place the negative lead on the right arm and the positive lead on the left leg.D: To assess lead III, place the negative lead on the right arm and the positive lead on the left leg.You
|
C: To assess lead II, place the negative lead on the right arm and the positive lead on the left leg.
|
|
|
You have defibrillated a patient who presented with ventricular fibrillation. After 2 minutes of CPR, you reassess the patient's cardiac rhythm and see a wide-complex tachycardia. You should:
|
A: cardiovert with the energy setting you used to defibrillate.
B: check for a carotid pulse and defibrillate if a pulse is absent. C: administer 300 mg of amiodarone via rapid IV or IO push. D: defibrillate and then immediately resume chest compressions. |
B: check for a carotid pulse and defibrillate if a pulse is absent.
|
|
|
When assessing lead II in a patient with a heart rate of 70 beats/min, the Q-T interval is considered prolonged if it is:
|
A: consistently greater than 0.20 seconds.
B: greater than one half of the R-R interval. C: three times the length of the P-R interval. D: twice the width of the QRS complex. |
B: greater than one half of the R-R interval.
|
|
|
The main purpose of listening to heart sounds is to:
|
A: assess for an S4 sound, which indicates a weak left ventricle.
B: evaluate the location of the point of maximal impulse (PMI).C: determine if the cardiac valves are functioning properly. D: assess the rate, regularity, and quality of the heartbeat. |
C: determine if the cardiac valves are functioning properly.
|
|
|
Cardioversion involves delivering a shock that is synchronized to occur during the:
|
A: upslope of the T wave.
B: P wave. C: R wave. D: downslope of the T wave. |
C: R wave
|
|
|
Unlike a second-degree AV block type I, a second-degree AV block type II is characterized by:
|
A: consistent P-R intervals following conducted P waves.
B: dissociation of the P waves and QRS complexes. C: a ventricular rate that is less than 50 beats/min. D: a progressive lengthening of the P-R interval. |
A: consistent P-R intervals following conducted P waves.
|
|
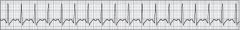
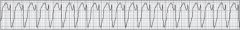
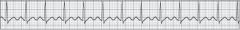
A 65-year-old man with difficulty breathing and palpitations presents with the cardiac rhythm shown below, which you should interpret as:
|
A: supraventricular tachycardia.B: ventricular tachycardia.
C: uncontrolled atrial fibrillation.D: atrial flutter with a fixed block. |
A: supraventricular tachycardia.
|
|
|
Which of the following represents the MOST appropriate initial drug and dose that is given to all adult patients in cardiac arrest?
|
A: 1 mg of epinephrine 1:1,000 every 3 to 5 minutes
B: 0.1 mg/kg of epinephrine every 3 to 5 minutes C: 10 mL of epinephrine 1:10,000 every 3 to 5 minutes D: 40 units of vasopressin every 3 to 5 minutes |
C: 10 mL of epinephrine 1:10,000 every 3 to 5 minutes
|
|
|
A 27-year-old female complains of palpitations. The cardiac monitor reveals a narrow-complex tachycardia at 180/min. She denies any other symptoms, and states that this has happened to her before, but it typically resolves on its own. Her blood pressure is 126/66 mm Hg, pulse is 180 beats/min, and respirations are 16 breaths/min. After attempting vagal maneuvers and giving two doses of adenosine, her cardiac rhythm and vital signs remain unchanged. You should:
|
A: transport at once, reassess her frequently, and perform synchronized cardioversion if necessary.B: administer 5 mg of midazolam and perform synchronized cardioversion starting with 50 joules.
C: infuse 150 mg of amiodarone over 10 minutes, reassess her, and repeat the amiodarone if needed. D: administer 0.35 mg/kg of diltiazem over 2 minutes and then reassess her hemodynamic status. |
A: transport at once, reassess her frequently, and perform synchronized cardioversion if necessary.
|
|
|
Immediately after establishing a return of spontaneous circulation in a woman with ventricular fibrillation of short duration, you should:
|
A: assess her ventilatory status and treat accordingly.
B: assess her blood pressure and treat if needed. C: obtain a 12-lead ECG to assess for cardiac damage. D: establish vascular access and give amiodarone. |
A: assess her ventilatory status and treat accordingly.
|
|
|
Which of the following pain descriptions is MOST consistent with a cardiac problem?
|
A: Sharp
B: Intermittent C: Tearing D: Crushing |
D: Crushing
|
|
|
ECG indicators of Wolff-Parkinson-White (WPW) syndrome include:
|
A: narrow QRS complexes and peaked T waves.
B: short PR intervals, delta waves, and QRS widening. C: tall P waves, QT interval prolongation, and tachycardia. D: delta waves, flattened T waves, and bradycardia. |
B: short PR intervals, delta waves, and QRS widening.
|
|
|
A 71-year-old male presents with chest pain and shortness of breath. He is conscious, but confused, and is profusely diaphoretic. He has weakly palpable radial pulses, a BP of 70/40 mm Hg, and diffuse crackles in all lung fields. You administer high-flow oxygen and apply the cardiac monitor, which reveals sinus tachycardia. The closest appropriate hospital is 40 miles away. Which of the following is the MOST appropriate next action?
|
A: Give 20 mL/kg fluid boluses.
B: Begin an infusion of dopamine. C: Perform a head-to-toe exam.D: Obtain a 12-lead ECG tracing. |
B: Begin an infusion of dopamine.
|
|
|
After performing synchronized cardioversion on an unstable patient with a wide-complex tachycardia, you look at the monitor and see coarse ventricular fibrillation. The patient is unresponsive, apneic, and pulseless. You should:
|
A: begin CPR, establish vascular access, and give amiodarone.
B: prepare to intubate the patient as your partner begins CPR.C: start CPR, ensure the synchronize mode is off, and defibrillate.D: perform CPR for 2 minutes and then cardiovert with 100 joules. |
C: start CPR, ensure the synchronize mode is off, and defibrillate.
|
|
|
In addition to CPR, the recommended treatment sequence for an unresponsive, apneic, and pulseless patient with a regular, wide-complex cardiac rhythm at a rate of 40 beats/min includes:
|
A: transcutaneous cardiac pacing and 1 mg of epinephrine every 3 to 5 minutes.
B: 40 units of vasopressin every 10 minutes and treating reversible causes. C: 1 mg of epinephrine every 3 to 5 minutes and 1 gram of calcium chloride. D: 1 mg of epinephrine every 3 to 5 minutes and treating reversible causes. |
D: 1 mg of epinephrine every 3 to 5 minutes and treating reversible causes.
|
|
|
Occlusion of the right coronary artery would MOST likely result in:
|
A: ectopic ventricular complexes.B: sudden cardiac arrest.
C: an increase in atrial kick. D: sinoatrial node failure. |
D: sinoatrial node failure.
|
|
|
Side effects of atropine sulfate may include:
|
A: hypotension.
B: acute urinary retention. C: pupillary constriction. D: hypersalivation. |
B: acute urinary retention.
|
|
|
When obtaining a 12-lead ECG, lead V1 should be placed:
|
A: approximately 1 inch to the right of the angle of Louis.
B: on the upper right shoulder just above the clavicle. C: in the fourth intercostal space just to the right of the sternum.D: in the second intercostal space just inferior to the second rib. |
C: in the fourth intercostal space just to the right of the sternum.
|

