![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
21 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
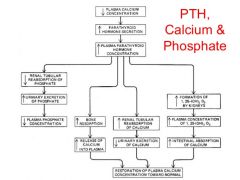
Describe the physiology of calcium and parathyroid |
|
|
|
|
What are the non-modifiable risk factors for osteoporosis? |
1. Age (post-menopausal) 2. Female 3. Family history 4. Caucasian/Asian 5. Early onset of menopause 6. low peak bone mass in early adulthood |
red ones are in FRAX calculator |
|
|
What are the modifiable risk factors for osteoporosis? |
1. dietary insufficiency 2. renal disease --> lower vit D production 3. gut malabsorption 4. endocrine causes: hyperthyroidism/hyperparathyroidism/cushing's/hypogonadism 5. RA 6. disuse osteoporosis 7. corticosteroids, anticonvulsants, excessive thyroxine 8. thyroxine and anticonvulsants 9. alcohol > 3units/day 10. smoking 11. low BMI 12. congenital conditions (OI, neuromuscular diseases) 13. COPD 14. Prolonged immobilization |
red ones are in FRAX calculator |
|
|
What is the FRAX calculator? |
The FRAX® algorithms give the 10-year probability of fracture. The output is a 10-year probability of hip fracture and the 10-year probability of a major osteoporotic fracture (clinical spine, forearm, hip or shoulder fracture). |
|
|
|
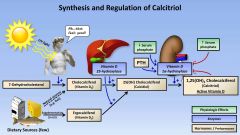
1. Define Vitamin D deficiency and treatment 2. Define Vitamin D insufficiency and treatment 3. Define normal Vitamin D level and treatment |
1. 25(OH)vit D <12 ug/L ----- 8 week calcium and vit D two tab OM + Lynae, followed by maintainance dose of Calcium/Vit D 2 tab OM 2. 25(OH)vit D 12-19 ug/L ----- 4 week calcium and vit D two tab OM + Lynae, followed by maintainance dose of Calcium/Vit D 2 tab OM 3. 25(OH)vit D >20 ug/L ----- maintainance dose of Calcium/Vit D 2 tab OM, if high risk of fall/osteoporosis |
|
|
|
1. Define normal bone density 2. Define osteopenia 3. Define osteoporosis 4. Define severe osteoporosis |
1. T-score of -1 SD or above 2. T-score between -1 SD and -2.5 SD 3. T-score of 2.5 SD or below 4. T-score of 2.5 SD or below, with at least 1 associated fracture |
|
|
|
When should pharmacological treatment be initiated for osteoporosis? |
1. Confirmed to be osteoporotic via DEXA scan 2. Previous fragility fractures 3. Increased fracture risk, guided by FRAX score 4. Prophylaxis for long term steroids (>7.5mg/day for >6 months) |
|
|
|
What are the pharmacological treatment options for osteoporosis? |
*** All therapy requires calcium (1200mg/day) and vit D supplementation (800 IU/day) First-line: Alendronate or Risedronate (Biphosphonates) Second-line: Strontium renelate or IV Zoledronic acid (Biphosphonates) Third-line: Etidronate (Biphosphonates) Fourth-line: Teriparatide (PTH recombinant form) others: - Raloxifene (SERMs) - Denosumab (RANKL inhibitor) |
|
|
|
What is the danger of starting bisphosphonate too early in osteoporotic patients? |
- Bisphophosnates reduces the activity of osteoclasts. - Vit D deficiency leads to impaired calcium uptake by the GIT - Thus, in the state of vitamin D deficiency, uninhibited action of osteoblasts > osteoclasts will lead to further deterioration in Calcium levels. (bone remodelling requires calcium) --> This leads to the risk of hypocalcaemia and osteomalacia |
|
|
|
What should the vitamin D level be before initiating bisphosphonate therapy? |
25-hydroxyvitamin D levels > 20 ug/L |
|
|
|
What are the side effects and risk factors for Alendronate/Risedronate? (and bisphosphonates in general) How should it be taken? What is the MOA? |
SE: - esophagitis/gastritis - osteonecrosis of jaw - ocular pain/BOV/conjunctivitis - associated with long bone fracture after 5 years CI: - Creatinine clearance <30 ml/min (stage 4 CKD) - Hypocalcaemia - Ensure Vit D level is normal before administration - Unable to remain upright for 30 mins - Unable to swallow pill/water How to take the medication? - First thing in the morning, take with water orally, on an empty stomach - stand/sit upright for 30 mins (to prevent esophagitis/gastritis) - don't take anything for the next 1.5 hours - calcium can only be taken 2 hours after bisphosphonates - stop/switch medication after 5 years, maximum MOA: - inhibit osteoclast acitivity |
|
|
|
What are the side effects and CI of zoledronic acid? How to take zoledronic acid? |
SE: - Flu-like reaction CI: - Creatinine clearance <30 ml/min (stage 4 CKD) - Hypocalcaemia - Ensure Vit D level is normal before administration How to take the medication? - 5mg IV, once a year - Give paracetamol before infusion, and continue till 48 hours after infusion, to reduce flu symptoms - Drink 500ml of water before infusion (to minimize gastritis/esophagitis?) |
|
|
|
What are the side effects and CI of strontium renelate? How to take strontium renelate? What is the MOA? |
SE: - SJS/TEN (main reason why it is 2nd line) - Nausea - Diarrhea CI: - creatinine clearance <30 ml/min (stage 4 CKD) how to take? - 2g sachet, taken at bedtime, 2hrs after eating MOA: - inhibit osteoclast acitivity |
|
|
|
What are the side effects and CI of raloxifen? What is the MOA? |
SE: - hot flushes - arthralgia - dizziness - leg cramps and oedema CI: - history of venous thrombo-embolic event, cholestasis, hepatic impairment, severe renal impairment - unexplained AUB/endometrial CA - be cautious if pt have CVS risk factors MOA: - selective estrogen receptor modulator |
|
|
|
What are the side effects and CI of teriparatide? How to take teriparatide? What is the MOA? |
SE: - hypercalcaemia - nausea and vomiting - headaches - very expensive CI: - bone malignancy (due to osteosarcoma in rats) - hypercalcaemia - hyperparathyroidism how to take? - 20 mg subcutaneous injection daily - maximum course is 18 months What is the MOA? - PTH recombinant --> activates osteoblasts, inhibits osteoclasts - if given daily, will have predominantly osteoblastic action and bone remodelling |
|
|
|
SE of Denosumab? How to take Denosumab? What is the MOA of Denosumab? |
SE: - SJS, TEN - Expensive How to take?: - Every 6 months, IV injection MOA: - RANK-Ligand inhibitor, leading to reduction in development of osteoclasts |
|
|
|
What are other lifestyle methods in managing osteoporosis? |
1. weight bearing exercise 2. Smoking cessation 3. fall prevention strategies 4. Calcium 1000mg/day 5. Vitamin D (ergocalciferol 50,000U once a week for 6-8weeks, then cholecalciferol 1000U daily) |
|
|
|
What are the bloods to do for fracture in elderly? |
1. Calcium and phosphate levels 2. FBC, ESR, UECr, Vit D 3. TFT, LFT, tumor markers, myeloma panel, skull x-ray (if suspected) 4. DEXA scan |
|
|
|
Common areas for fragility fracture? |
1. Vertebral compression fracture 2. Hip fracture 3. Forearm fracture (colles) |
|
|
|
Investigations for newly diagnosed osteoporosis? |
1. Calcium, phosphate levels 2. Vitamin D (25 OH cholecalciferol) 3. FBC, RP 4. ESR others if suspected secondary osteoporosis: - TFT - LFT - Tumor markers - Myeloma screen (FBC, ESR, urine electrophoresis, skull x-ray, BMA) |
|
|
|
Abnormal T score, normal Z score = primary osteoporosis |
Abnormal T and Z score = secondary osteoporosis |
|

