![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
40 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Where is the sural nerve most vulnerable to entrapment?
What is the treatment? |
1.5 cm distal to tip of fibula with foot in equinus. Tx: Surgical Release.
|
|
|
|
where does the sural nerve course:?
|
Sural nerve is made of collateral branches off the common tibial and common fibular nerves (both from the sciatic division in the popliteal fossa)
Courses inferiorly between heads of gastroc, becomes superficial at middle of leg, descends with small saphenous vein, wraps inferiorly around lateral malleolus to lateral foot. |
|
|
|
course of the common fibular nerve
|
Common Fibular Nerve branches off the Sciatic (divides away from Common Tibial) travels parallel to the biceps femoris to fibular head
|
|
|
|
Function & Clinical Significance of Sural Nerve
|
Purely sensory info from the posterior lateral corner of the leg, from the lateral foot and 5th toe (but not the tip which is lateral plantar).
good for nerve bx or donor graft. |
|
|
|
Medial Plantar Nerve Entrapment
Why, Where, Tx |
aka Jogger's Foot
Compression at Knot of Henry where FDL and FHL cross MCC: Foot orthotics Tx: dc orthoses |
|
|
|
Knot of Henry
|
where FDL and FHL cross
most likely spot of Medial Plantar Nerve Entrapment (compression) aka joggers foot MCC: Foot orthotics Tx: dc orthoses |
|
|
|
Lateral Plantar Nerve Entrapment
|
Culprit is Baxter’s Nerve: 1st branch of LPN which innervates ADQ
compressed btw AHL & QP near calcaneus Tx: surgical release of abductor halluces fascia |
|
|
|
Baxter's Nerve
|
1st branch of LPN which innervates ADQ
Lateral plantar nerve entrapment caused when Baxter's nerve compressed btw AHL & QP near calcaneus Tx: surgical release of abductor halluces fascia |
|
|
|
Superficial Peroneal Nerve Entrapment
|
Paresthesia of dorsum worsened in plantarflexion/inversion
MCC: fascial defect ~12cm superior to lateral malleolus where it pierces fascia to become superficial, possibly from inversion injury Tx: Non-Op: Observation; Op: Refractory/Elite Athletes |
|
|
|
Paresthesia of foot dorsum worsened in plantarflexion/inversion
|
Superficial Peroneal Nerve Entrapment
MCC: fascial defect ~12cm superior to lateral malleolus where it pierces fascia to become superficial, possibly from inversion injury Tx: Non-Op: Observation; Op: Refractory/Elite Athletes |
|
|
|
Plantar Sessamoid Bone Anatomy
|
Two sessamoid bones within the Flexor Hallucis Brevis
|
|
|
|
Tibialis Posterior Innervation & Insertion
|
Tibial Nerve
Insertion: Navicular & Medial Cuneiform |
|
|
|
Tibialis Anterior
Innervation, Insertion, Action |
Innervation: Deep Fibular Nerve
Insertion: medial cuneiform and first metatarsal Action: Dorsiflexion and Inversion |
|
|
|
EHB
Innervation, Origin, Insertion |
Deep Fibular Nerve
Origin: Calcaneus Insertion: Proximal Phalanx (1st) |
|
|
|
Fibularis Tertius
Innervation, Course, Action |
Deep Fibular Nerve
Dorsal Surface of Fibula to Dorsal Surface of 5th Metatarsal Dorsiflexion & Eversion |
|
|
|
Dorsal interossei vs Plantar Interossei
|
Both Innervated by Lateral Plantar Nerve
Dorsal interossei muscles are bipennate Plantar interossei muscles are unipennate |
|
|
|
Flexor Hallucis Brevis
Innervation, Origin, Insertion |
Medial Plantar Nerve
Plantar Surface of Cuneiform to Medial and Lateral sessamoid bones |
|
|
|
Fibularis Longus
Nerve, Course, Action |
Superficial Fibular Nerve
Upper lateral fibular shaft to First Metatarsal, Medial Cuneiform Plantarflexion, Eversion, Arch Support |
|
|
|
Flexor Digitorum Brevis
Nerve, Origin |
Medial Plantar Nerve
Calcaneus (Plantar aponeurosis) |
|
|
|
During Rehabilitation following ACL injury/repair: what strengthening exercises are possible without endangering the graft?
|
Beynnon 1995 Am J Sports Med
Isometric Hamstrings contraction only at any angle Isometric Quadrieps contraction after 60 degrees or greater Or Active Knee motion between 35 degrees of motion or higher |
|
|
|
Strongest predictor of cutout in intertrochanteric fracture fixation with dynamic hip screw application?
|
Trip-Apex distance >25mm
Baumgartner 1995 JBJS |
|
|
|
Exchange nailing
|
Indicated for aspectic diaphyseal tibial and femoral non-unions in the absence of comminution, or segmental bone loss.
Hypertrophic non-unions have good biology and bad stability: treat with larger nail Atrophic non-unions need better biology (bone graft, flap coverage, etc) Brinker JBJS 2007 Zelle J Trauma 2004 |
|
|
|
Preoperative factors associated with postoperative improvement in shoulder function following hemiarthroplasty
|
Hetterich JBJS 2004
Most improvement: absence of glenoid erosion (pain and function) No prior surgery, intact rotator cuff (function) Osteonecrosis, DJD Least Improvement: Rheumatoid Arthritis, Capsulorrhaphy arthropathy (arthropathy 2/2 overtightening of capsule following prior surgery) |
|
|
|
Blood Volume Estimation for Pediatric Patients
|
Preme: 95mL/kg
Full Term Neonate: 85mL/kg Infants: 80 mL/kg Adult Men: 75 Adult Women: 65 |
|
|
|
Flexor tendon damage zones:
|
zone location affects healing and post-op course
Zone I: Phalanx Distal to FDS Insertion Zone II: DIP to Distal Palmer Crease (“No Man’s Land”) Zone III: Palm Zone IV: Carpal Tunnel Zone V: Wrist and forearm Thumb: TII, TII, TII |
|
|
|
FDP vs FDS
|
FDP
Origin: Ulna, Interosseus membrane Insertion: P3 Innervation: Median & Ulnar flexes DIP, assists with other flexion, common muscle belly FDS Origin: Medial Epicondyle Insertion: P2 Innervation: Median flexes PIP assists with MCP flexion, individualized muscle bellies (25% absence to 5th digit) |
|
|
|
where can you find the FPL in the carpal tunnel
|
FPL: most radial strx in carpal tunnel
|
|
|
|
most radial structure in the carpal tunnel
|
FPL
|
|
|
|
FCR
|
Origin: common flexor tendon
inserts into 2nd metacarpal, most proximal to median nerve in carpal tunnel Innervation: Median |
|
|
|
FCU
|
origin: common flexor tendon
inserts on pisiform, hook of hamate, and base of 5th metacarpal innervation: unlar nerve |
|
|
|
Phases of tendon healing:
|
Inflammatory: Days 0-5, no strength
Fibroblastic: Days 5-28, increasing strength Remodelling: Days >28, will tolerate active ROM |
|
|
|
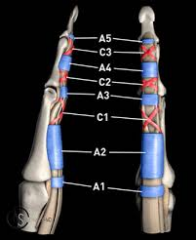
Pulley system of the digits:
|
A1 to A5 annular pullies and C1 to C3 cruciate pulleys
A2 (proxP1) and A4 (midP2) are the most important for preventing bowstringing For thumb two annular (DIP & PIP) and one oblique pulley (P1) Oblique is most important |
|
|
|
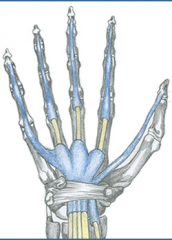
Vascular Supply to UE Flexor Tendons
|
Diffusion through Synovial Sheath when Tendon is located inside sheath (see pic)
Diffusion is most important source proximal to MCP Direct vascular supply nourishes tendons outside sheath |
|
|
|
Caring for Flexor Tendon Injuries
|
Bishop J Trauma 1986: canine model demonstrates earl motion improved outcomes
McGeorge & Stillwell J Hand Surg Br. 1992: tendons lacerated by <60% need not be repaired |
|
|
|
Median nerve lies directly ulnar to what structure
|
FCR
|
|
|
|
Extensor compartments of the wrist
|
1: AbPL, EPB
2: ECRL, ECRB 3: EPL 4: EIP, EDC (extensor indices proprius – ulnar to 1st EDC tendon, extensor digitorum communis) 5 EDM 6: ECU |
|
|
|
Extensor Zones
|
I: over DIP
II: Middle Phalanx III: over PIP IV: Proximal Phalanx V: over MCP VI: dorsum of metacarpals VII: extensor retinaculum (carpals) VIII: proximal wrist |
|
|
|
Gold standard for determining adequate blood flow for an charco ulcer to heal:
|
>30mmHg Transcutaneous O2 pressure TcpO2
-NB: ABI may be falsely elevated with calcified arteries |
|
|
|
Gold standard for relief of non-infected charcot plantar ulcerations
|
Non-infected (no fever, erythema, exudate, CRP, ESR = absolute contra’d) with good arterial supply (relative contra) = Total Contact Casting.
Once active dz complete --> CROW Charcot Restraint Orthotic Walker, followed by custom shoe with fitted orthoses. NB: ulcer recurrence most likely at 3-4 weeks |
|
|
|
Grading Diabetic Foot Ulcerations
|
Wagner Classification
0: At Risk Foot --> shoe modification, serial exams 1: Superficial ulcer --> office debridement, contact casting 2: Deeper, full thickness ulcer --> operative debridement, contact casting 3: Deep Abscess or Osteomyelitis --> operative debridement, contact casting 4: Partial Gangrene of Forefoot --> Local vs Larger Amputation 5: Extensive Gangrene --> Amputation |
Brodsky Depth-Ischemia Classification
0: At risk foot --> Education, accommodative footware, serial exams 1: superficial, noninfected ulcer --> Offload with Total Contact Cast, Walking Brace or Special Footwear 2: deep ulceration, exposing tendons or joints --> surgical debridement, wound care, off-loading, Cx specific Abx 3: Extensive ulceration or abscess --> debride or partial amputation, off-loading, Cx specific Abx A: Non-ischemic B: ischemia without Gangrene: non-invasive vasc testing, vasc recon c angioplasty/bypass C: partial forefoot gangrene: vasc recon and partial foot amputation D: complete gangrene: complete vasc eval and major extremity amputation |

