![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
361 Cards in this Set
- Front
- Back
|
What is the order of teeth most frequently found missing?
|
1. Third molars
2. The mandibular second premolars 3. The maxillary lateral incisors 4. The maxillary second premolars (These make up 85% of the non-third molar congenitally missing teeth) |
|
|
What is the incidence percent of SUPERNUMERARY TEETH?
|
- 1.3%
|
|
|
What is the incidence percent of CONGENITALLY MISSING TEETH?
|
4%
|
|
|
Supernumerary teeth are most commonly found where?
|
Maxilla
|
|
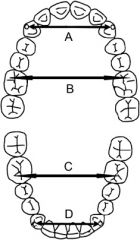
Identify A , D:
|
Inter cuspid width
|
|
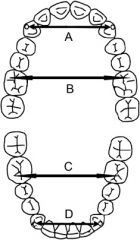
Identify B, C:
|
Intermolar width
|
|
|
Define "required"
|
amount of tooth material present, includes the mesio-distal width of the permanent teeth from 5 to 5 (erupted and unerupted)
|
|
|
Define "arch perimeter":
|
amount of space available in the arch, measured usually from the mesial of the first molar on one side to the mesial of the first molar on the other side
|
|
|
What is the Johnson-Tanaka rule and when is it used?
|
JT Rule is used if the patient is in the middle mixed dentition (3, 4, 5 are not in the mouth) and there are no periapicals of the 3,4,5 to get an approximate measurement, you use this rule to predict the size of the 3,4,5 (as a sum).
( sum of 42, 41, 31, 32 ) / 2 + 11 = sum of 3,4,5 in ONE MAXILLARY QUAD ( sum of 42, 41, 31, 32 ) / 2 + 10.5 = sum of 3,4,5 in ONE MANDIBULAR QUAD |
|
|
Which teeth predict the sum of both the mandibular and maxillary 3,4, 5's?
|
LOWER incisors
|
|
|
How does one measure arch perimeter?
|
a
|
|
|
What is the Bolton Analysis?
|
- It compares the sizes of the upper teeth ot the lower teeth.
Bolton 6 = 91% width of mand. teeth ------------------------- width of max. teeth Bolton 3 = 77% width of mand teeth ------------------------ width of max teeth |
|
|
In cases of MINIMAL CROWDING, where non-extraction is desired, one must maximize space available by using what?
|
INTRAORAL:
- Lingual holding arch - transpalatal bar or Nance arch EXTRALORAL: - headgear |
|
|
What are some perceived advantages of early orthodontic treatment?
|
- ability to modify skeletal growth
- better and more stable treatment results - less iatrogenic tooth damage - better cooperation - improved patient self esteem and parental satisfaction |
|
|
What are the perceived disadvantages of early orthodontic treatment?
|
- variation in results and stability (major)
- increased financial cost - patient "burnout" = longer duration of tx - iatrogenic problems - unpredictable dynamics of growth |
|
|
What are some problems that can be treated in the primary dentition?
|
- Digital and pacifier habits
- Space management - posterior crossbite with functional shift |
|
|
When should treatment for prolonger digital or pacifier habits be initiated?
|
4-6 years (before eruption of permanent incisors)
|
|
|
TRUE or FALSE: Anteroposterior dental and skeletal changes are more likely to self-correct than are the vertical dental changes?
|
FALSE - AP changes are LESS likely to self-correct
|
|
|
Anterior open bites resulting from digital sucking may correct spontaneously if the habit cease before what age?
|
9 years old
|
|
|
Why is it important to treat posterior crossbite with functional shift as soon as possible?
|
To prevent assymmetric positioning and growth of the condyles. Permanent facial asymmetry may result and persist
|
|
|
When should a posterior crossbite WITHOUT a functional shift be treated?
|
Less urgent. It can be treated in the early mixed dentition or even closer to adolescence
|
|
|
When is the best time to treat crowding?
|
Treatment of mild to moderate crowding cases best time is late mixed dentition, after the eruption of the first premolars.
|
|
|
Between the ages of 6 and 12, the length of the mandibular arch from the permanent left first molar to the permanent right first molar will normally
A. increase with the eruption of the permanent canines. B. increase with eruption of the premolars. C. remain the same. D. decrease with the eruption of the permanent incisors. E. decrease with the eruption of the premolars. |
E
|
|
|
The last bone in the craniofacial complex to stop growing is the
A. frontal B. nasal C. maxilla D. mandible |
MANDIBLE
|
|
|
Which tooth movement is NOT possible with a removeable appliance?
A. Crown tipping B. root uprighting C. crown rotation |
CROWN ROTATION
|
|
|
What is the rate limiting step of tooth movement?
|
bone resorption
|
|
|
What appliance is best suited to achieve rapid maxillary expansion?
|
Hyrax appliance (fixed)
|
|
|
Which appliance is suited for SLOW palatal expansion?
|
Quad-helix
|
|
|
What is the primary function of the Nance Holding Arch?
|
- space maintainer
- additional support for anterior teeth |
|
|
The most appropriate time for surgical treatment in a female patient with mandibular prognathism is
A. just before the beginning of the prepubertal growth spurt. B. just after the end of the prepubertal growth spurt. C. just before eruption of the second permanent molars. D. just after eruption of the second permanent molars. E. after the completion of growth. |
E. After completion of growth
|
|
|
Which occlusal parameter is the most useful to determine if a posterior crossbite is of skeletal or dental origin?
A. Anterior overbite. B. Sagittal molar relationship. C. Lack of space in the maxillary anterior area. D. Lack of space in the mandibular arch. E. Buccolingual angulation of affected teeth. |
Buccolingual angulation of affected teeth
|
|
|
The occlusal parameter most likely associated with maxillary anterior spacing is a/an
A. Class II Division 2 dental malocclusion. B. Class III skeletal malocclusion. C. accentuated maxillary curve of Wilson. D. reverse maxillary curve of Wilson. |
C
|
|
|
What is the purpose of the Curve of Wilson?
|
- complement paths of the condyles during mandibular movements
|
|
|
How does the Curve of Wilson grow as we move posteriorly?
|
Grows deeper posteriorly, so that molars have greater inclination than the premolars
|
|
|
What is the prevalence of malocclusion?
|
CROWDING: ~60%
CLASS II/ 1: 15-20% CLASS II/ 2: 10% CLASS III: 3% |
|
|
Define COMPETENT LIPS:
|
lips meet together at rest
|
|
|
Define INCOMPETENT LIPS
|
lips do not meet together at rest
|
|
|
Define FRANKFORT PLANE:
|
Line joining porion (superior aspect of external auditory meatus) with orbitale (lowermost point of bony orbit)
|
|
|
Define LOWER FACIAL HEIGHT;
|
Clinically, distance from the base of the nose to the point of the chin.
In a normally proportioned face is equal to middle facial third (eyebrow line to base of nose). Cephalometrically, distance from anterior nasal spine ANS to MENTON as a percentage of total face height |
|
|
Define TOTAL FACE HEIGHT:
|
Nasion to menton
|
|
|
Define BIMAXILLARY PROCLINATION:
|
Both upper and lower incisors are proclined
|
|
|
Define OVERJET
|
distance between the upper and lower incisors in the horizontal plane
|
|
|
Define OVERBITE:
|
Overlap of the incisors in the vertical plane
|
|
|
Which arch is LEEWAY SPACE greater?
|
Lower arch
|
|
|
In CEPHALOMETRICS, what is [S]?
|
Sella: mid-point of sella turcica
|
|
|
In CEPHALOMETRICS, what is [N]?
|
Nasion: most anterior point on fronto-nasal suture
|
|
|
In CEPHALOMETRICS, what is [Or]:
|
Orbitale: most inferior anterior point on margin of orbit
|
|
|
In CEPHALOMETRICS, what is [Po]?
|
Porion: uppermost outermost point on bony external auditory meatus
|
|
|
In CEPHALOMETRICS, what is [ANS]?
|
Anterior nasal spine
|
|
|
In CEPHALOMETRICS, what is [PNS]?
|
Posterior Nasal Spine
|
|
|
In CEPHALOMETRICS, what is [Go]?
|
Gonion: most inferior point on angle of mandible
|
|
|
In CEPHALOMETRICS, what is [Me]?
|
Menton: lowermost point on the mandibular symphysis
|
|
|
In CEPHALOMETRICS, what is [A]?
|
A point: position of deepest concavity on anterior profile of maxilla
|
|
|
In CEPHALOMETRICS, what is [B]?
|
B point: position of deepest concavity on anterior profile of mandibular symphysis
|
|
|
In CEPHALOMETRICS, what is FRANKFORT PLANE?
|
Po-Or
|
|
|
In CEPHALOMETRICS, what is MAXILLARY PLANE?
|
PNS-ANS
|
|
|
In CEPHALOMETRICS, what is MANDIBULAR PLANE?
|
Go-Me
|
|
|
What are three reasons for ANCHORAGE LOSS?
|
- failure to appreciate fully anchorage requirements at Rx planning stage
- Active force exceeding available anchorage (over-activation or too many teeth being moved at a time) - poor patient compliance |
|
|
What are the ADVANTAGES of removeable appliances?
|
- easier to clean
- easy to adjust, less chairside time - greater contact with mucosa = greater anchorage - can be used for o/b - can transmit forces to blocks of teeth |
|
|
What are the DISADVANTAGES OF removeable appliances?
|
- patient can leave it out
- only TIPPING movement possible - affects speech - good technician required - intermaxillary traction not possible - lower rmv appliances are dificult to tolerate - inefficient for multiple tooth movements |
|
|
What are some indications for ACTIVE RMV APPLIANCE?
|
- simple tipping movement of an individual tooth
- movement of blocks of teeth (eg. correction of buccal crossbite by expansion of arch) - interceptive treatment in the mixed dentition (eg correction of an upper incisor in crossbite) - overbite reduction - in conjunction with other appliance (eg to facilitate distal movement of upper molars with headgear, to free occlusion to allow movement of a tooth over the bite during fixed appliance Rx) |
|
|
What are some indications for PASSIVE RMV APPLIANCE?
|
- space maintainer (eg loss of an upper central due to trauma)
- retaining appliance (following fixed appliance treatment) |
|
|
Define ANCHORAGE:
|
- resistance to reaction forces from an appliance causing unwanted tooth movement
- perfect anchorage is achieving desired tooth movements in one or more teeth without inducing any auxillary or undesired tooth movement in other teeth |
|
|
What is a TAD?
|
Temporary Anchorage Device
- made of titanium or titanium alloys that is screwed into bone to provide optimal anchorage for desired tooth movements |
|
|
What are some USES of TADS?
|
- uprighting a tooth
- drawing molar teeth anterior for space closure when anteriors are already in desired position - holding 6's / molars distal in extraction cases where prevention of mesial drift is desired (no need for headgear / pt compliance) - intrusion of molars where banding and bracketing may cause supra-eruption of anteriors (gummy smile) |
|
|
What is IPR?
|
Inter Proximal Reduction
- process of removing small amounts of enamel between two adjacent teeth |
|
|
What is the max allowed removal of tooth structure for IPR?
|
0.3 mm from anterior teeth
0.6 mm from posterior teeth |
|
|
Suggest a few situation where one would consider using IPR to achieve a goal (either long/short tem):
1) treatment planning 2) esthetics 3) early mixed dent eruption 4) invisalign 5) banding |
1) Treatment option for Class I malocclusion with crowding of 1-5mm
2) Bolton's discrepancy 3) Ectopically erupted tooth, need to fit band 4) |
|
|
Suggest and explain a few treatment planning TRENDS in orthodontics?
|
INVISALIGN
- case selection is extremely important - patient compliance is key - treatment is computer-fabricated - uses TIPPING forces as opposed to sliding forces - trays are easier to clean than traditional braces - little need for ortho wax - any expansion or torquing movements are prone to relapse - IPR is very common to facilitate rotation of teeth - half of the cases will require mid-course correction or refinement stage therefore treatment is usually over 6 months - pain will still occur - optimal esthetics during treatment LINGUAL ORTHODONTICS - pleasing esthetics during treatment - help with crowding, gaps, overbites, underbites - however, tend to hurt patients tongue and make it difficult for them to speak at first - precision is a key element necessary with bends and ties because the activation of torque is FARTHER from incisal edges - treatment can take a few months longer than traditional braces - case sensitive |
|
|
When would be a good time to place a lower lingual holding arch?
|
- placing LHA is a choice to be made in the middle to end of the late mixed dentition stage (10.5-11 years old)
- before primary molars are exfoliated - it is put in place to avoid forward shift of the permanent molars to attempt to resolve crowding issues |
|
|
What are the normal eruption patterns and deviations of MAXILLA?
|
6-1-2-4-5-3-7-8
7 beats 3 = 3 gets blocked out palatally or lingually 7 beats 5 = 5 gets blocked out |
|
|
What are the normal eruption patterns and deviations of MANDIBLE?
|
6 1 2 3 4 5 7 8
7 beats 5 = 5 blocked out 4 beats 3 = 3 blocked out |
|
|
Why is the 3 on the mandible being blocked out more of a problem than the same situation on maxilla?
|
- Tissue in mandible is very thin
- will get stripping of lower canines |
|
|
When should a frenectomy be performed?
|
Well Dr. Anholt, since you asked, all maxillary frenectomies should be done after the approximation of teeth (i.e. bringing the teeth together) because if it is done before, the scar tissue that results from the surgery can inhibit future diastema closure. Usually maxillary frenectomies are done at age 12-13 years after permanent canines are fully erupted. Occasionally, if the frenum is particularly heavy/thick, intervention is required at a much earlier age (i.e. 7 or 8 years of age). Mandibular labial frenums should be managed as early as possible (when recognized). Usually this is age 7-8.
|
|
|
Why should a frenectomy be performed?
|
Maxillary frenum causes spacing of the central incisors (diastema).
Lingual frenum causes speech issues or restricted tongue movements. Mandibular Labial frenum with high attachment can cause stripping of gingiva and therefore a loss of attachement of the mandibular incisors. |
|
|
When should separators be placed?
|
ONE WEEK prior to banding appointment
|
|
|
What are some patient instructions for SEPARATORS?
|
- don't floss
- no sticky foods - call if separator falls out |
|
|
What type of cement is used for banding?
|
Fuji Ortho II
|
|
|
What is the correct height of maxillary lateral brackets?
|
3.0mm from incisal edge
|
|
|
Which archwires should be used initially?
|
Flexible - NiTi 0.014, 0.016, 0.018
|
|
|
What is the order of MOST FLEXIBLE to LEAST FLEXIBLE of archwires?
|
- Nitinol / Copper NiTi round 014, 016, 018
- NiTi rectangular 016 x 022" - Stainless Steel Round 014, 016, 018 - SS rectangular 016 x 022, 017 x 025 - SS rectangular preformed closing loops 017 x 025 |
|
|
What is the purpose of NiTi wires?
|
- initial levelling and major rotations
|
|
|
What is the purpose of SS Round AW?
|
- continues to level
- used with elastomeric chains to gather segments together (i.e. canine retraction and ant. space closure) |
|
|
What is the purpose of RECTANGULAR SS AW?
|
- major levelling of Curve of Spee
- space closure - torque control |
|
|
What are power chains used for?
|
- close spaces
- OPEN = O-O-O-O-O - CLOSED = OOOOO |
|
|
What is an OPEN COIL used for?
|
- create space
|
|
|
What is a CLOSED COIL used for?
|
- maintain space
|
|
|
What is the purposed of a GANGTIE?
|
- maintain space closure
|
|
|
What is the most common size for intraoral elastics?
|
3.5 oz - 1/4 " (chuck elastiks)
|
|
|
How are CLASS II elastics placed?
|
Max Canine to Mand Molar
|
|
|
How are CLASS III elastiks places?
|
- Mand Canine to Max Molar
|
|
|
What are the advantages of REMOVEABLE FUNCTIONAL APPLIANCES?
|
- function
- ease of fabrication - aesthetics - tissue bears most of the work rather than sound teeth being placed in stressful situations - easy to clean - do not jeopardize supporting teeth as extensively to caries/stress - do not require as much professional supervision |
|
|
What are the disadvantages of REMOVEABLE FUNCTIONAL APPLIANCES?
|
- if the patient doesnt cooperate then it is of little value
- can be lost / broken - caries susceptibility is higher if not cleaned |
|
|
What are the advantages of FIXED RETAINERS?
|
- permanence
- not easily lost/ broken - not bulky - require less patient cooperation if oral habits already good |
|
|
What are the disadvantages of FIXED RETAINERS?
|
- more chair time required
- more experience and skill necessary - susceptible to caries if OH is not good |
|
|
What are the DIAGNOSTIC FACTORS involved in SPACE MAINTENANCE?
|
- establish presence of underlying permanent tooth (periapical radiographs)
- measurements (if possible) to determine amount of space necessary or available to successional tooth - time factor: should be placed IMMEDIATELY after tooth extraction - dental age - bone overlying successional tooth - sequence of eruption |
|
|
What are the INDICATIONS for SPACE MAINTENANCE?
|
- DENTAL CARIES: severe caries involving loss of contact points initiates mesial drifting of posterior teeth
- TRAUMA - ECTOPIC ERUPTION: extraction to allow tooth to erupt - SUPPRESSED TOOTH: primary molar inhibiting normal alveolar bone development and deflecting erupting bicuspid should be extracted - DELAYED ERUPTION: when teeth are delayed either due to ectopic position, impaction, deflection - ABSENCE OF SUCCESSIONAL TOOTH: keep space in future for dental prosthesis |
|
|
What are the types of space maintainers?
|
BAND AND LOOP:
DISTAL SHOE: |
|
|
What are some uses of HEADGEAR?
|
- extrude maxillary molars
- open the bite - aid in vertical development |
|
|
What are the reasons for using a headgear?
|
- to move teeth (usually max. molars distally)
- to reinforce anchorage - for orthopedic correction |
|
|
What are the components of a HEADGEAR?
|
- facebow (inner and outer bow)
- Jhooks - neck strap - neck pad |
|
|
What are the most common adverse effects of using CERVICAL PULL HEADGEAR?
|
- extrusion and tipping of max molars
- in Class II Div I extrusion of posterior teeth tends to open the bite and rotate mandible downward and backward, aggravating facial disfigurement - depending on amount of retrognathia or increase in lower facial height, use of headgear may be contraindicated |
|
|
If you NEED extrusion of molars, what headgear will you use?
|
Cervical pull headgear
|
|
|
If you want to AVOID extrusion of first molars, what headgear would you use?
|
- HI-pull headgear
|
|
|
How do you test to see if a patient has been wearing their headgear?
|
- the 6's will be slightly mobile
- they don't need a mirror to put it in and out |
|
|
What are the indications for acrylic appliances in anterior crossbite correction?
|
- to open the bite anteriorly to allow for tooth/teeth in crossbite to move labially
- to move teeth/tooth in crossbite labially |
|
|
What are the INDICATIONS for ADAM's CLASPS?
|
- good retention on teeth to be clasped (undercuts)
- one or two teeth in crossbite and adequate room to move them labially (w or w/o deciduous teeth removal) - can deliver forces to any/all teeth in crossbite with mini-expansion screw |
|
|
What are the INDICATIONS for OVER THE TUBE CLASPS?
|
- poor retention on teeth to be clasped
- intention to use 2x4 fixed appliances in conjunction with acrylic appliance - cannot deliver forces to any/all teeth in crossbite - need to align anteriors |
|
|
What is a 2x4 fixed appliance?
|
- two bands on first molars
- brackets on incisors |
|
|
What are the indications for a 2x4 appliance?
|
- need to create space
- cases where anteriors are rotated, crowded, and/or in crossbite |
|
|
What are the CONTRAINDICATIONS of 2x4 appliance?
|
- where full braces will be used later and alignment of incisors is not going to be significantly changed at this time
- proper placement of brackets on lateral incisors will tip root distally and "burn the roots" against the canines |
|
|
What are the different ways of correcting posterior crossbite DENTALLY?
|
- through the bite elastics
- quad helix - acrylic appliance with mid-palatal expander |
|
|
What are the different ways of correcting posterior crossbite SKELETALLY?
|
- Hyrax screw (RPE)
- SARPE - Surgical narrowing of mandible and/or surgical widening of maxilla |
|
|
At what age does the mid-palatal suture start to close?
|
13-14 years
|
|
|
What are some causes of UNSUCCESSFUL ORTHODONTIC TREATMENT?
|
- poor oral hygeine
- poor compliance - missed appointments - eating sticky foods - trauma - luck of the draw |
|
|
What are the NON-SURGICAL / EXTRACTION patterns for CLASS I MALOCCLUSION?
|
ANY OF:
- NE - 4/4 - 4/5 - 5/5 - 7/7 |
|
|
What are the NON-SURGICAL / EXTRACTION patterns for CLASS II MALOCCLUSION?
|
ANY OF:
- NE - 4/ - 4/5 - 4/4 - 5/5 |
|
|
What are the NON-SURGICAL / EXTRACTION patterns for CLASS III MALOCCLUSION?
|
ANY OF:
- NE (rare) - 5/4 |
|
|
What are some ADVANTAGES of removing MAND FIRST PREMOLARS?
|
- extraction sites often closer to typical area of developing crowding (ant)
- frequent allowance for retention of second decidous molar to preserve first molar position (no mechanical space maintainer needed) - allowance for possibility of greater retraction of mand anterior teeth to reduce dental or facial protrusion - in general concordance with the dental eruption pattern of mand. dentition - avoids surgical trauma from early extraction of a second premolar (2nd premolar requires care to preserve buccal/lingual bone) - favorable eruption sequence |
|
|
What are some DISADVANTAGES of MAND FIRST MOLAR extraction?
|
- without ortho treatment, poor root paralleling between second premolar and canine
- likelihood of increased lingual migration of mandibular incisors - increased curve of spee and possibly overbite as well - increased freqeuncy of rotation of premolar and sometimes canine towards the extraction site |
|
|
What are the ADVANTAGES of SECOND MAND PREMOLAR extraction?
|
- good root parallelism between first premolar and canine retained
- limited lingual migration of mand incisors - minimal increase in curve of spee - more room for second molars in future - ability to mesialize first molar to achieve Class I molar relationship |
|
|
What are LIMITATION and DISADVANTAGES to SECOND MAND PREMOLAR extraction?
|
- contact and marginal ridge relationship between first molar and first premolar not always ideal
- early extraction of 2nd premolar requires delicate surgical intervention - space maintenance may be required to allow for eruption and distal drifting of both premolar and canine - occlusal table is radically reduced for varying periods of time |
|
|
What are ANDREWS SIX KEYS TO OCCLUSION?
|
1) Molar relationship
2) Crown angulation 3) Crown inclination 4) Rotations 5) Tight contacts 6) Occlusal plane (Curve of Spee) |
|
|
Define OLIGODONTIA:
|
missing more than 6 teeth
|
|
|
Consider the validity of the following statements:
1) Congenitally missing teeth are less common than supernumerary teeth 2) All supplemental teeth are supernumeraries 3) all supernumerary teeth are supplemental 4) including wisdom teeth, 1 in every 20 patients is congenitally missing at least one permanent tooth |
1) false
2) true 3) false 4) true 50% of children born today don't have an eighth molar |
|
|
In a normal CLASS I occlusion the transverse distance between the central fossae of the lower first permanent molars should be equal to:
|
the transverse distance between the MP cusp tips of the upper first molars
|
|
|
Suggest two plausible instances that may be present to explain a situation when the Bolton 6 calculation shows a mandibular excess but the Bolton 12 calculation shows a maxillary excess
|
- adg
|
|
|
When viewing a lateral ceph, even a patient with a perfectly symmetric mandible will appear to have a mild form of mandibular asymmetry because the lower borders of the two sides of the mandible will not be perfectly in line Why is this the case?
|
- head position
- parallax - xray source / diverging beams - this is an artifact of the x-ray |
|
|
7. Patient’s upper midline is 0.5mm to the left of the facial midline and his/her lower midline is 0.5mm to the right of the facial midline. You and the patient create a crafty plan to run an elastic at night from the hook on 23 to the hook on 43 but you don’t consult with the ortho before dismissing the patient. The patient complies and the next appointment the midlines are coincident. However certain 3D side effects can be noticed due to the fact that the canines were not tightly ligigated with steel.
|
-All 3D movements
- CANT |
|
|
Suggest rationale for interprox reduction as a modality to improve
a) esthetics b) occlusion c) treatment effeciency d) mixed dentition alignment |
a) black triangles
b) narrowing lower premolars, class I occlusion at anterior c) can't get a band on, rotating teeth easier if you have spaces for invisalign d) adjusting things to guide eruption |
|
|
Briefly talk about FOUR RECENT trends in ortho treatment. Rationalize why each may be beneficial, suggest some risks or limitations.
|
LINGUAL ORTHO
- TAD's - PATIENT DIRECTED - INVISALIGN - |
|
|
Upper 6's tend to rotate around which root(s)?
|
Palatal root
|
|
|
Which tooth in the upper arch is most likely to be blocked out and/or impacted?
|
CANINE
|
|
|
What are some of the reasons the CANINE is more likely to be blocked out in max arch?
|
- last tooth to erupt
- has the longest path of eruption |
|
|
Impacted canines most commonly erupt into which position?
|
Palatal?
|
|
|
Which dental specialists may need to be involved in impacted max canine cases?
|
ORAL SURGEON
PERIODONTIST |
|
|
Which procedure may need to be performed for impacted Max Canine?
|
- free gingival graft
- apically positioned flap |
|
|
Under what circumstance would you consider treating with braces immediately?
|
1) psychosocial
2) trauma 3) future |
|
|
ORTHO IN ADULTS - What are some special considerations that need to be taken into account?
|
- adult orthodontics is basically the same as adolescent ortho for tissue changes associated with tooth movement, stages of treatment, and goal of treatment
------------------------------------------ ISSUES TO BE CONSIDERED --------------------------- PSYCHOSOCIAL - Expectations and attitude of adult patients require different behavioural management - May demand more aesthetic appliances - Generally more co-operative in following instructions - High treatment expectations --------------------------------------------------------- TREATMENT MODALITIES AVAILABLE: - Surgical - camouflage (extraction of tooth) - growth modification appliances not applicable due to completion of growth ---------------------------- RE: EXTRACTION - extraction choice may be affected by periorestorative condition of dentition or already extracted tooth complicating treatment plan - space closure may be difficult in molar area - response of cortical bone to ortho force is significantly slow ---------------------------------------------- RE: APPLIANCE PLACEMENT - while bonding special considerations may be required due to presence of restorations such as porcelain/metallic surfaces --------------------------------------------------------- BIOMECHANICAL CONSIDERATIONS: - adult bone is less reactive to mechanical forces - greater risk of loss of attachment - bone loss and gingival recession more common in adults - less force used ---------------------------------------- RE: TOOTH MOVEMENTS - overbite of adults corrected by intrusion of anterior teeth, not extrusion of posteriors ----------------------------- RE: ANCHORAGE - anchorage may be affected by poor periorestorative status and missing teeth - headgears may not be acceptable due to esthetic reasons - two step space closure with frictionless mechanics may be used ------------------------------------ RE: ROOT RESORPTION - more vulnerable to root resorption --------------- RE: TMD - higher risk of developing TMD in adults --------------------------------- RE: TREATMENT TIME - tissue remodelling associated with tooth movement is slow, treatment time is longer -------------------------------- RE: FINAL DETAILING - higher relapse rates in adults - prolonged retention |
|
|
What is the goal of ADJUNCTIVE ORTHODONTICS in the adult?
|
- Tooth movement carried out to facilitate other dental procedures necessary to control disease, restore function and/or enhanve appearance
- primary goal usually to make it easier or more effective to replace missing teeth or damaged teeth |
|
|
What is COMPREHENSIVE ORTHODONTIC TREATMENT?
|
- To produce the best combination of dental occlusion, dental and facial appearance, stability, to maximize the benefit to the patient
|
|
|
Why take orthodontic photographic records?
|
- for proper treatment planning and follow-up
- allow study of patient's soft tissue patterns during treatment planning stage - assess lip morphology and tonicity, smile arc, smile aesthetics - degree of incisal show upon smiling |
|
|
What are the THREE MAIN TYPES of ortho records?
|
- study models
- radiographs - clinical models |
|
|
What EXTRAORAL photos are taken for ortho?
|
FACE - frontal (lips relaxed)
FACE - frontal (smiling) PROFILE - right side (lips relaxed) 3/4 PROFILE - (smiling) |
|
|
What information do we get from a FRONTAL FACE (lips relaxed) photo?
|
- general facial features
- soft tissue profile - lip competence - facial profile (long/med/short) |
|
|
What information do we get from a FRONTAL FACE (smiling) photo?
|
- visualization of smile esthetics
- soft tissue proportions during smiling - facial height |
|
|
What information do we get from a PROFILE (lips relaxed) photo?
|
- soft tissue profile
- nose/lip size - NLA - E-plane - Facial height - chin throat length - sublabial furrow - lip competence - facial characteristic (straight, convex, concave) |
|
|
What information do we get from a 3/4 PROFILE (smiling)
|
- conveys patient in social interaction
- smile esthetic changes pre - post treatment |
|
|
What are some determinants of prognosis?
|
- Patient compliance
- Luck of the draw - Age of the patient - Skeletal classification - Angle's classification - Treatment plan choice - Patient expectations |
|
|
What are some important things to discuss in INFORMED CONSENT for INVISALIGN?
|
DEVICE DESCRIPTION:
----------------------------------- They are a series of clear plastic removeable appliances that move your teeth in small increments. Aligners are customized and produced specifically for your treatment. BENEFITS --------------------- - more aesthetic than conventional ortho - nearly invisible - tooth movement can be visualized on computer software - allow for better oral hygeine - no metal wires or brackets RISKS / INCONVENIENCES --------------------------------------- - failure of compliance can lengthen treatment time and affect the ability to achieve desired results - high compliance needed - dental tenderness may be experience after new aligner - soft tissues may be scratched or irritated - teeth may shift position after treatment - faithful wearing of retainers needed - poor OH can exacerbate tooth decay, etc - aligners may temporarily affect speech - may cause temporary increase in salivation or mouth dryness - attachments may be bonded to one or more teeth during the course of treatment - teeth may require IPR - general medical conditions and use of medications can affect ortho tx - health of bone and gums may be impaired or aggravated - oral surgery may be needed to correct crowding or severe jaw imabalances - additional restorative work may be required on teeth - existing restorations (crowns) may become dislodged - root resorption |
|
|
What are some good uses of INIVISALIGN?
|
- mild to moderate crowding with IPR or expansion
- posterior dental expansion - close mild-moderate spacing - absolute intrusion (1 or 2 teeth only) - lower incisor extraction for severe crowding - tip molar distally |
|
|
What are things INVISALIGN is NOT good for?
|
- dental expansion for blocked out teeth
- extrusion of incisors - high canines - severe rotations - levelling by relative intrusion - molar uprighting - tranlastion of molars - closure of premolars extraction spaces |
|
|
Define "LOWER FACIAL HEIGHT"
|
The total face height is divided into UPPER and LOWER. Lower refers to distance from SUBNASALE to MENTON.
|
|
|
What is the normal proportion of UPPER to LOWER FACIAL HEIGHT?
|
55:45
|
|
|
What is the UPPER FACIAL HEIGHT?
|
glabella (eyebrow point) to subnasale
|
|
|
Why is it generally a poor idea to extract premolars in the lower arch only?
|
The lowers would mesialize and the upper 7' s would be left with no opposing tooth
|
|
|
What two structures demarcate the CRANIAL BASE?
|
SELLA
NASION |
|
|
Why is the cranial base important?
|
- THe plane formed by these two points represents a relatively stable anatomic structure. During growth and treatment the SN plane remains relatively constant and can be used as a reference point to measure positional change of maxilla and mandible and the associated teeth
|
|
|
What are the general limitations of cephalometrics?
|
- two dimensional view of three dimensional object
- can be errors in identification of landmarks - too many assumptions - ignores patient - cultural / geographical differences / race / sex / etc |
|
|
What is the effect of BIMAXILLARY PROTRUSION on the ANB ANGLE?
|
Bimaxillary protrusion seems to be primarily a DENTAL condition and not skeletal, so the ANB angle doesn't necessarily change. A and B point remain where they are.
|
|
|
What is the difference between PROTRUSION and PROCLINATION?
|
PROTRUSION is horizontal
PROCLINATION is angular |
|
|
What is ANNEALING?
|
- Heat and allow it to cool slowly, in order to remove internal stresses and toughen it
|
|
|
Why are wires ANNEALED?
|
- During deformation and "cold work" the AUSTENITE phase of the stainless steel wire transforms to MARTENSITE
- MARTENSITE phase is associated with creating stress and regions of varying hardness in the arch - annealing is done to homogenize the mechanical properties of the wire and relieve stress |
|
|
When is ANNEALING done?
|
- done after significant manipulation of the wire and immediately prior to placement intraorally
|
|
|
Why are NiTi wires ANNEALED?
|
NiTi wires have elastic memory
- Annealing is done when the elastic properties of the wire are needed to be removed i.e. for distal ends of the wire to resist displacement of wire |
|
|
What are the advantages of CLOSING LOOP space closure vs "elastic chain" space closure?
|
ANterior closing loop will move the anterior teeth as a single unit to where you want them, with primarily TRANSLATIONAL movement instead of tipping movements. Elastic chain closure however may tip the teeth too much and torquing will be required later to correct them.
|
|
|
What is a CLOSED COIL?
|
- it is a spring
- can move teeth to close space - can maintain a space between teeth - closed coil is STRETCHED and has force pulling inwards trying to return to original length. - exerts a PULLING force on both brackets |
|
|
Suggest some situations where FIXED RETAINERS would be desireable:
|
- prolonged retention need
- minimum patient compliance needed - orthognathic cases - good OH practice - prevent lingual incisor correction - anchorage for 6's while rotation of other teeth taking place - constriction or expansion of lower arch - as part of habit cessation - |
|
|
Why do thumb-suckers classically present with problems in all three facial dimensions?
|
Thumb-sucking has an effect in each dimension. The "suction" action has a general constriction (from the vacuum) that puts pressure to bring everything inwards. Palatal constriction is common.
There is also a vertical component which can result in posterior tooth supraeruption and an anterior open bite. |
|
|
What are SIX non-orthodontic methods/ aids to limiting thumb-sucking in a 6 year old girl that sucks her thumb while she is alone during the day and while sleeping.
|
- reinforce that hands are dirty
- use gloves/ bandage on thumb - use finger ointment or taste deterrant - tape a ruler to their arm while they sleep so they can't bend their arm - positive re-inforcement - teach them an acitivity to keep their hands busy - tell them a scary story about someone who lost his thumb from the habit - show the child the effects it is having - be positive when pointing out the behaviour rather than scolding - Have the child be in charge of placing the "thumb guard" prior to bedtime / naptime (glove, sock, splint, adhesive tape) - use bitter tasting solution NOT AS PUNISHMENT but in combination with reward system - |
|
|
Why do excessive OJ problems tend to persist even after a digit-sucking habit is eliminated?
|
Excessive OJ problems are usually due to skeletal problems rather than soft tissue / habit ones. Need to address growth/ skeletal problems to correct this.
|
|
|
Give SIX sequential sentences that you could say to a mother concerned about her 4 year old boy that sucks his thumb?
|
- Thumb sucking is a natural reflex, which calms, comforts and induces sleep in young children.
- Most children outgrow this habit by 6 years of age. - If the habit continues any later during permanent tooth eruption then there may be some problems. - Various different methods can be used to correct the problem, the earlier it is addressed the better - Psychological/behavioural modification is tried first and then appliance therapy is used if this proves not effective - Allowing the habit to continue indefinitely can result in permanent mal-occlusion and greatly affect the smile of the child making it harder to correct the older they are (more expensive treatment in the long run) |
|
|
What are the FOUR general treatment plan directions one can take with orthodontics?
|
- NON SURG - NON EXT
- NON SURG - EXT - SURG - NON EXT - SURG EXT |
|
|
What are the records used in case analysis?
|
- Pantomograph
- Lateral ceph in occlusion - Facial photos - intra-oral photos - study models - patient information on blue sheets in chart - periapicals / CMS as needed |
|
|
What questions should one ask when assessing prognosis of a treatment?
|
- What are the problems in the case that may be difficult to correct?
- What is likely to happen in treatmetn? - What is likely to happen in retention? - What is likely to happen in post-retention? - What is the overall success probability? |
|
|
EXAMPLE OF A SURGICAL WORK-UP:
|
DIAGNOSTIC SUMMARY:
------------------------------------- 1. 45 year old female 2. c.c. “can’t bite front teeth together” 3. TMJ problem 4. Class III skeletal mid-face retrusion 5. Class III Dental (Mutilated) 6. Overbite: 3 mm right central 7. Overjet: -2 mm 8. 36, 47, and 15 abscessed 9. Broad alar bases 10. Heavy maxillary frenum 11. Crossbite -- all teeth except 23, 24, and 17 12. Retroclined mandibular incisors 13. Missing 13, 34, 37, and 24 14. Mandibular incisor crowding 15. Exposure of lower anterior root structure 16. Cervical caries 17. Short chin-throat length 18. Maxillary incisors in good position 19. Large chin 20. Tendency to high mandibular plane TREATMENT OBJECTIVES: -------------------------------------- 1. Improve function and esthetics 2. Relieve TMJ problems as possible 3. Gain positive overjet 4. Treat abscessed teeth 5. Maintain perio health as possible Prevent further deterioration of mandibular incisors 6. Prevent enlargement of alar base width as possible 7. Relieve maxillary frenum 8. Procline mandibular incisors 9. Relieve mandibular crowding TREATMENT PLAN: ---------------------------- 1. Consult re: Perio 2. Consult re: Endo 3. Consult re: Surgery -- probable 3 piece maxillary advancement 4. Bond 11, 12, 21, 22, 31, 32, 41, and 42 Band remaining teeth 5. Maxillary advancement 6. Detailing and positioner PROGNOSIS: -------------------- 1. 47 may abscess further Prognosis of 36 and 15 doubtful 2. Perio condition may deteriorate -- probably better if ortho and surgery done now. If perio surgery not done, advancement of incisors may cause some loss of bone. Observe closely. 3. One-piece maxillary advancement likely not possible |
|
|
Define NASOLABIAL ANGLE:
|
- angle constructed by drawing lines from the base of the nose to the contour of the upper lip
- normal is around 102 degrees |
|
|
Obtuse NASOLABIAL ANGLE is a major indicator of what?
|
Class III midfcae retrusion
|
|
|
What is the CHIN THROAT LENGTH?
|
- Horizontal length from the throat to the chin
|
|
|
What is some useful information that can be gained from CHIN-THROAT LENGTH?
|
- good indicator of the need for any potential mandibular advancement or set back surgery where the mandible is the jaw at fault
|
|
|
What are the three different facial profiles?
|
- STRAIGHT: Class I
- CONVEX: Class II - CONCAVE: Class III |
|
|
Define SUBLABIAL FURROW?
|
- furrow made beneath the lower lip and chin
|
|
|
What is the significance of the SUBLABIAL FURROW?
|
- the deeper the furrow the lower the facial height and the greater the percentage of nasal height
|
|
|
What are the three types of FACIAL HEIGHT?
|
- MESOCEPHALIC (normal)
- DOLICO- (long) - BRACHY- (short) |
|
|
Explain ANGLE'S CLASS I:
|
Lower teeth are antero-posteriorly related to the upper teeth so that the buccal groove of the lower first permanent molar occludes with the mesio-buccal cusp of the upper first permanent molar.
- CLASS I Ideal - CLASS I Malocclusion |
|
|
Explain ANGLES CLASS II:
|
- the Lower teeth are distally related to the upper teeth to the extent of HALF the mesio-distal width of the first permanent molar, or the entire mesio-distal width of a premolar
|
|
|
What are the two divisions of ANGLES CLASS II?
|
DIV I: Upper incisors are prominent
DIV II: one or more of the upper incisors are retroclined and typically the upper centrals are retroclined |
|
|
Explain ANGLES CLASS III:
|
Lower teeth are mesially related to the upper teeth to the extent of half the mesio-distal width of the first permanent molar, or the entire mesio-distal width of a premolar, and the lower incisors occlude labially to the upper incisors.
|
|
|
What are the ANB values associated with the different skeletal patterns?
|
CLASS I: 0 - 4.5' ANB
CLASS II: > 4.5' ANB CLASS III: < 0' ANB |
|
|
DRAW OUT SASSOUNI'S TABLE:
|
a
|
|
|
What is the sequence of eruption of the PRIMARY TEETH?
|
==A==B====D===C=====E
A======B==D===C===E== 6-8==8-10==12-16-20-30 |
|
|
TRUE or FALSE: Overbite and Overjet are less in primary dentition?
|
TRUE
- if you have deep OB and OJ in primary then this will be increased in permanent |
|
|
What are the three terminal plane relationships possible?
|
MESIAL STEP (25%)
FLUSH (62%) DISTAL (13%) |
|
|
What radiographs should be taken on a 3-6 year old?
|
- upper and lower anterior occlusals or periapicals (tooth presence)
- 2 bitewings (for decay) |
|
|
What radiographs should be taken on 7-8 year old?
|
- periapicals / pantomograph of erupting incisors
|
|
|
What marks the beginning of the MIXED DENTITION PHASE?
|
Eruption of the 6's
|
|
|
EARLY MIXED DENTITION: when is it?
|
- 6-8 years
- Eruption of 6's, 1's and 2's |
|
|
MIDDLE MIXED DENTITION: When is it?
|
- 8-10 years
- end of eruption of incisors up to (but not including) exfoliation of deciduous buccal segments |
|
|
LATE MIXED DENTITION: when is it?
|
10--12 years
Permanent successors erupt and deciduous buccal segments exfoliate |
|
|
What are some solutions to ECTOPICALLY ERUPTING 6's?
|
- place separator
- slice distal of e - extract e and place space maintainer |
|
|
Define EARLY MESIAL SHIFT:
|
- may occur in early mixed dentition when 6's erupt if there is spaced dentition
- flush terminal planes may become Class I in spaced dentition |
|
|
Define LATE MESIAL SHIFT:
|
- when e's are lost and first molars move forward
- LEEWAY SPACE OF NANCE: Incoming 3,4,5 are smaller than C, D, E that are being exfoliated, results in a space. |
|
|
How much is the FREEWAY SPACE?
|
MAX: 0.9 mm per quad
MAN: 1.7 mm per quad |
|
|
What are the BIG 3?
|
- CROWDING
- RELOCATION OF UPPER / LOWER INCISORS - CURVE OF SPEE |
|
|
What are the BIG 5?
|
- Class I Molar
- Class I Cuspid - Overjet of 1-2 mm - Overbite of 1-2 mm - Coincident midlines |
|
|
What are the THREE MAIN rules for extraction cases?
|
1) If you extract in lower you MUST extract in upper
2) One can extract teeth in upper and not in lower, molars would be Class II and canines would be Class I 3) Lower incisors must be at correct angulation - 4mm @ 25' lower to NB - 4mm @ 22' upper to NA |
|
|
Define AVAILABLE ARCH PERIMETER:
|
distance around the arch perimeter from the mesial of 6 to mesial of contralateral
|
|
|
Define REQUIRED ARCH PERIMETER:
|
collective width of the teeth
- each tooth measured mesio-distally and added together |
|
|
Which extraction pattern results in MAX ANCHORAGE?
|
Extraction of FIRST PREMOLAR
|
|
|
Which extraction pattern results in MINIMAL ANCHORAGE?
|
Second premolar
|
|
|
How much slippage of the molars is there in FIRST PREMOLAR extractions?
|
2.5mm on each side (approx. 5mm)
|
|
|
How much slippage can be expected in SECOND premolar extractions?
|
5mm on each side = 10mm molar slippage
|
|
|
What are the three different classes of CURVE OF SPEE?
|
SMALL (1-2mm)
MODERATE (3-4mm) LARGE (5-6mm) |
|
|
What is the most important factor in determining whether to extract and which teeth to extract?
|
CROWDING
|
|
|
How is the CURVE OF SPEE affected during orthodontic treatment?
|
Eventually flattens as diameter of A/W increases
|
|
|
What kind of movement of teeth is NOT possible with round wires?
|
BODILY (translation)
|
|
|
Which teeth are the most common congenitally missing?
|
THIRD MOLARS
|
|
|
EXCLUDING the third molars, what percentage of the population have one or more teeth congenitally missing?
|
4%
|
|
|
What is the order of the teeth most frequently found missing?
|
THIRD MOLARS > Mand 2nd Pre > Max Lat > Max 2nd Pre
|
|
|
What is the incidence of SUPERNUMERARY TEETH?
|
1.3% - less common than congenitally missing
|
|
|
Supernumeraries are more commonly found in which arch?
|
MAXILLA
|
|
|
MISSING TEETH affect Bolton Ratios
|
Know
|
|
|
When are MAXILLARY FRENECTOMIES usually performed?
|
12-13 years after permanent canines are fully erupted
- after approximation of teeth - if done before, scar tissue may inhibit diastema closure |
|
|
How do you determine if a frenal attachment is responsible for a diastema?
|
- blanching of attachment
- high attachment - stripping of attached gingiva - lack of attached gingiva |
|
|
When should a LINGUAL FRENUM be dealt with?
|
- as early as 7 to 8 years
|
|
|
At which Moyer's stage doe the tooth start to erupt?
|
Stage 6 Nolla - crown completely formed
|
|
|
At which Moyers stage does crown pass through alveolar crest?
|
Stage 8 - 2/3 root is formed
|
|
|
How much of the root is complete when the tooth erupts into the oral cavity?
|
3/4 complete - Stage 9 Nolla
|
|
|
What resorbs roots?
|
Osteoclasts
|
|
|
Discuss PARALLAX:
|
radiograph
- used to locate impacted canines - etc |
|
|
What are some questions to ask in DIAGNOSIS?
|
- What is the stage of development?
- What are the problems? - What can be done now? - What if nothing is done now? - Is it ext/non-ext? - Is surgery necessarY? - What records required? |
|
|
What are some causes of case relapse?
|
- poor case selection
- wrong treatment plan - luck of the draw - patient compliance - third molar eruption - late growth changes - neuromuscular factors - incisors not properly placed - major derotations |
|
|
What is PERIODONTAL BIOTYPE? How does it relate to ortho?
|
Before any orthodontic treatment can begin, it is essential that the patient's periodontium be in sound condition, capable of responding to the movement of teeth in a healthy fashion. Inspection of the dentition, palpation of tissues, and careful study of adequate X-Rays are all necessary for establishing a diagnosis, but review of the depth of gingival pockets with periodontal probes is the key procedure for avoiding blunders in treatment. After periodontal health has been validated, it is vital that orthodontists determine the patient's periodontal biotype by clinical observation and periodontal probing and assess the quality of the gingival attachments of the teeth that will be affected by the expansion forces of treatment. The ensemble of these criteria will dictate what treatment paths and forces the orthodontist will employ.
|
|
|
What is a TAD?
|
TEMPORARY ANCHORAGE DEVICE
- aka: mini-implants, micro-implants, skeletal anchorage |
|
|
What are the ADVANTAGES of using TAD's?
|
- no patient cooperation required
- easy to use - shortening of treatment time - good control on tooth movements - discomfort for patient is minimal - minimal number of teeth needed as "anchors" and for indirect force - stable position throughout treatment |
|
|
What are some INDICATIONS for TAD's?
|
- where you can not afford any movement of reactive units (max anchorage cases)
- patient with several missing teeth making it difficult to engage posterior units - for difficult tooth movements eg. intrusion of anterior and posterior segments, and distalization - where asymmetrical tooth movement is needed - to treat borderline cases with non-extraction method - doing extreme orthodontics when patient is not willing to undergo orthognathic surgery |
|
|
What are some sites of placement of TAD's in MAXILLA?
|
- infrazygomatic crest area
- tuberosity area - between 1st and 2nd molars buccally - retromolar area - between 1st molar and 2nd premolar buccally - between canine and premolar buccally |
|
|
What are some sites of placement of TADs in MANDIBLE?
|
- interproximal areas buccally
- mid-palatal area |
|
|
What are the disadvantages of using HEADGEAR as anchorage?
|
- poor aesthetics
- full patient cooperation may not be possible - cooperation may be unpredictable - force is applied intermittently |
|
|
What is IPR?
|
Interproximal Reduction
|
|
|
What are some "layman" terms that can be used to describe IPR?
|
- slicing
- sectioning - stripping ends off |
|
|
What are some situations where IPR could be indicated?
|
- Bolton size discrepancy (inter-arch)
- Tooth size discrepancies - Abnormal tooth shape / dental aesthetics - Macrodontia size discrepancies - crowding of mandibular incisors - to enhance retention and stability - to simulate stone-age man's proximal attrition - normalization of gingival contour and elimination of triangular spaces above papilla - moderate dentomaxillary disharmony: up to 8mm per arch - reduced expansion and premolar extraction - camouflage of Class II and Class III malocclusions - correction of Curve of Spee |
|
|
What are some CONTRAINDICATIONS for IPR?
|
- Severe crowding (more than 8 mm per arch)
- poor oral hygeine / periodontal environment - small teeth / hypersensitivity to cold - susceptibility to decay or multiple restorations present - shape of teeth: should NOT be done on "square" teeth |
|
|
How much enamel can be reduced with IPR?
|
Approx. 0.8 mm per contact
|
|
|
What are the steps involved in IPR?
|
1) SEPARATION
2) REDUCTION 3) RECONTOURING 4) POLISHING 5) PROTECTION: fluoride |
|
|
What are the ADVANTAGES of IPR?
|
- overexpansion of arch is avoided
- extraction of teeth greatly reduced - reduced need for excessive tooth movement - treatmetn time reduced - quality of treatment significantly improved in patients with crowding and contraindications for extractions (ie closed bites) - esthetics improved - treatment of adults with slight or mod crowding is possible without ext. - greater post- treatment stability is possible |
|
|
What are some ways that LEEWAY SPACE can be "lost" or "used up"?
|
- Congenitally missing primary dentition
- large permanent teeth - no primate spacing - early crowding |
|
|
What are a few current "TRENDS" in orthodontics?
|
- TAD's
- Lingual orthodontics - Invisalign - |
|
|
When would be a good time to place a LOWER HOLDING ARCH?
|
- Placing LHA is to be made in middle to late mixed dentition stage (10-12 years old)
- before the primary molars are exfoliated - put in place to avoid forward shift of permanent molars |
|
|
What are the normal eruption patterns?
|
Maxilla: 6 1 2 4 5 3 7 8
7 beats the 3 = 3 gets blocked out (palatally or lingually) 7 beats the 5 = 5 gets blocked out Mandible: 6 1 2 3 4 5 7 8 7 beats the 5 = 5 blocked out 4 beats the 3 = 3 blocked out |
|
|
What is the 6 MONTH RULE OF THUMB?
|
Isomer / Antimer's should erupt within 6 month time span of each other
|
|
|
Define SERIAL EXTRACTION:
|
Orthodontic treatment that involves ORDERLY removal of selected deciduous and permanent teeth
|
|
|
What are some reasons for SERIAL EXTRACTION?
|
- alleviate crowding of incisor teeth
- allow unerupted teeth to guide themselves into improved positions - lessen period of active appliance therapy |
|
|
What are some justifications for SERIAL EXTRACTION?
|
Dental crowding
– The result of inade quate arch size, insufficient basal bone, and / or excessive tooth material – is epidemiologically the most common type of malocclusion. It can be eliminated by making the dental arch larger or reducing the amount of tooth material. Expansion of the dental arches by orthodontic Serial Extractions – A Review www.iosrjournals.org 41 | Page alignment may be possible if the tooth material is not too excessive. However, the stability of expansion may well be compromised by the insufficient alveolar basal bone. Physiologic tooth movement – If primary teeth are extracted p rematurely, this will influence the eruption rate and position of the permanent successors. In general, the eruption will be delayed if the primary tooth overlying the permanent tooth is extracted 1 ½ years or more from the time the primary tooth would nor mally exfoliate. Conversely, the eruption rate can be accelerated if the primary tooth overlying the permanent tooth is extracted less than a year before the primary tooth would normally exfoliate. Biologic variation in eruption rates will affect these tim e tables, as will periapical inflammation of the primary tooth. Another useful principle is that crowded teeth adjacent to an extraction site tend to align themselves. Normal dental, skeletal and profile development – influences the rationale for serial e xtraction. The work of Moorrees and Moorrees et al on arch dimensions and serial extractions indicates that there is minimal increase in mandibular intercanine width between 8 and 18 years, occurring usually around the time the permanent mandibular canines erupt. The maxillary intercanine width increases slightly more and over a longer time. The dental arch perimeter from the distal of the mandibular primary second molar to its antimere is less in the permanent dentition than in the primary. Also the princi ples of leeway space, interrelationship of overjet, overbite, axial inclinations, and mesial shift, and arch - length analysis must be considered in determining whether to institute a serial extraction procedure. The skeletal and profile factors that influe nce serial extractions are the another - posterior, vertical, and transverse relationships as well as the developmental pattern. Specifically the relation of the maxilla to the mandible and of the both to the cranial base must be determined to identify protr usions, retrusions, hyperdivergences, hypodivergences, crossbites, and asymmetries. Also rotational, vertical, and transverse growth patterns need to be integrated into the decision - making process. |
|
|
What is a list of possible clinical cues for serial extraction?
|
- premature loss of deciduous teeth
- arch-length deficiency and tooth size discrepancies - lingual eruption of lateral incisors - unilateral decidous canine loss and shift to the same side - mesial eruption of canines over lateral incisors - mesial drift of buccal segments - abnormal eruption direction - abnormal eruption sequence - flaring of incisors - ectopic eruption of mandibular first deciduous molar - abnormal resorption of deciduous molar - ankylosis - labial stripping or gingival recession of lower incisor |
|
|
What are some of the LIMITATIONS of serial extractions?
|
- Tendency of bite to close following loss of posterior teeth
- premolars fail to reach their normal occlusal level due to having to travel a long way (prolonged absence of teeth in the segment) - may develop tongue thrusting habit in the area - facial esthetics - may cause concave profile - nasal development - unrestrained extraction will accentuate its prominence by reducing skeletal development in dental area |
|
|
What are some CONTRAINDICATIONS of SERIAL EXTRACTIONS?
|
- congenital absence of teeth providing space
- mild to moderate crowding - deep or open bites - Severe Class II, III of dental/skeletal origin - cleft lip / palate - spaced dentition - anodontia / oligodontia - midline diastema - dilacerations - extensive caries - |
|
|
What are the ADVANTAGES of SERIAL EXTRACTIONS?
|
- psychological trauma can be avoided by treatment
- reduces duration of the multi-banded treatment - physiologically treatment as it involves guidance of teeth into normal positions with physiologic forces - better oral hygeine - more stable results |
|
|
What are the DISADVANTAGES of SERIAL EXTRACTIONS?
|
- patient cooperation is needed
- risk of arch length reduction is present - requires proper professional and clinical judgement - may develop tongue-thrusting - |
|
|
What is ANKYLOSIS?
|
a pathologic fusion of the cementum or dentin of a tooth root to the alveolar bone
|
|
|
How does ANKYLOSIS occur?
|
- Necrosis of PDL cellular elements by dessication, crushing, mechanical damage, disrupts normal homeostatic mechanism
- allows growth of bone across the PDL - more common following delayed replantation or severe intrusion - |
|
|
What is the best, most specific test for ANKYLOSIS?
|
Percussion / sound test
|
|
|
List some examples of INTERARCH ELASTICS and their objectives:
|
- Bilateral Class II
- Class II with Ant. Trapezoid - Class II with Ant. Cross - V Posterior with Ant. Cross - V Posterior - V Posterior with Ant. Trapezoid - Class III - Class III with Ant Trapezoid - Tent - Finishing - Finishing w/ Ant. Trapezoid - Box |
|
|
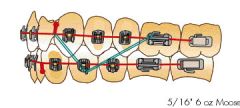
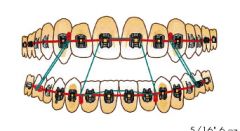
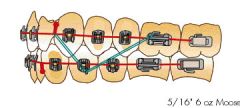
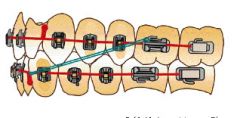
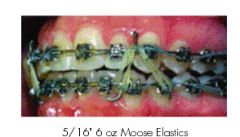
What is the OBJECTIVE of CLASS II ELASTIKS?
|
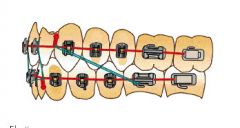
- Correct CLASS II A-P dental relationships
- use 5/16 - 6 oz |
|
|
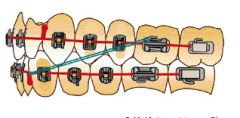
What is the OBJECTIVE of CLASS II Elastiks with ANTERIOR TRAPEZOID?
|
- Correct Class II A-P dental relationships and Anterior Openbite
|
|
|
What is the objective of CLASS II ELASTIKS WITH ANTERIOR CROSS ELASTICS?
|
- correct Class II A-P relationship
- Anterior midline discrepancy |
|
|
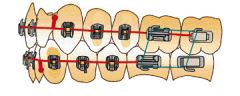
What is the OBJECTIVE of V POSTERIOR ELASTICS?
|
- Correct posterior openbite
|
|
|
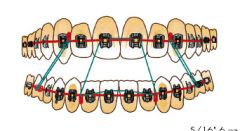
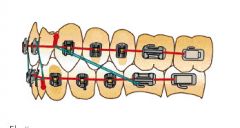
What are the OBJECTIVES of CLASS III ELASTICS?
|
- Correct Class III A-P
|
|
|
What is the OBJECTIVE of TENT ELASTIKS?
|

Correct openbite in a specific area
|
|
|
What is the OBJECTIVE of FINISHING ELASTICS?
|

Finish a case with a challenging bite to close
|
|
|
What is the OBJECTIVE of BOX ELASTICS?
|
- Correct posterior openbite in molar area
|
|
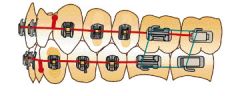
What kind of elastic design is this?
|
Class II
|
|
What kind of elastic design is this?C
|
Class II with Anterior Trapezoid
|
|
What kind of elastic design is this?
|
V Posterior
|
|
What kind of elastic design is this?
|
Class III
|
|
What kind of elastic design is this?
|
Tent
|
|

What kind of elastic design is this?
|
Finishing
|
|
What kind of elastic design is this?
|
Box
|
|
|
What is INDIRECT BONDING?
|
- Brackets are positioned on a study model, and then transfer masks are used to position the teeth intraorally
|
|
|
What are the advantages of INDIRECT BONDING?
|
- reduction in patient chair time
- more accurate braces placement - reduced composite excess around braces - reduced chair time throughout therapy because position more accurate, fewer compensatory bends needed - less need for repositioning of poorly placed brackets - less operator sensitive - little experience needed - less chance of white spot formation / plaque accumulation |
|
|
Summarize the procedure of INDIRECT BONDING:
|
- accurate stone model made
- |
|
|
Define INCISOR LIABILITY:
|
Permanent incisors are larger than the deciduous teeth.
|
|
|
How is INCISOR LIABILITY resolved with time?
|
- interdental spacing of primary dentition
- more labial inclination of permanent incisors - inter-canine arch width growth |
|
|
When should one suspect ankylosis?
|
- infra-occlusion
- deviation of occlusal plane - no permanent successor / delayed eruption - percussion |
|
|
What is "slop"?
|
Play of the wire in the bracket
|
|
|
What are the three dimensions of facial growth, in order of which finishes last?
|
WIDTH < LENGTH < HEIGHT
|
|
|
What is the average CROWN LENGTH of a MAX CENTRAL INCISOR?
|
10.5 mm
|
|
|
What is the average CROWN LENGTH of a MAX LATERAL INCISOR?
|
9.0 mm
|
|
|
What is the average CROWN LENGTH of a MAX CANINE?
|
10.0 mm
|
|
|
What is the average CROWN LENGTH of a MAX PREMOLAR?
|
8.5 mm
|
|
|
What is the average CROWN LENGTH of a MAX 1st MOLAR?
|
7.5 mm
|
|
|
What is the average CROWN LENGTH of a MAX 2nd MOLAR?
|
7.0 mm
|
|
|
What is the average CROWN WIDTH of a MAX CENTRAL INCISOR?
|
8.5 mm
|
|
|
What is the average CROWN WIDTH of a MAX LATERAL INCISOR?
|
6.5 mm
|
|
|
What is the average CROWN WIDTH of a MAX CANINE?
|
7.5 mm
|
|
|
What is the average CROWN WIDTH of a MAX PREMOLAR?
|
7.0 mm
|
|
|
What is the average CROWN WIDTH of a MAX 1st MOLAR?
|
10.0mm
|
|
|
What is the average CROWN WIDTH of a MAX 2nd MOLAR?
|
9.0 mm
|
|
|
What is the average CROWN WIDTH of a MAND CENTRAL INCISOR?
|
5.0 mm
|
|
|
What is the average CROWN WIDTH of a MAND. LAT INCISOR?
|
5.5 mm
|
|
|
What is the average CROWN WIDTH of a MAND CANINE?
|
7.0 mm
|
|
|
What is the average CROWN WIDTH of a MAND PREMOLAR?
|
7.0mm
|
|
|
What is the average CROWN WIDTH of a MAND 1st MOLAR?
|
11.0mm
|
|
|
What is the average CROWN WIDTH of a MAND 2nd MOLAR?
|
10.5mm
|
|
|
What is the average CROWN LENGTH of a MAND CENTRAL?
|
9.0 mm
|
|
|
What is the average CROWN WIDTH of a MAND LATERAL?
|
9.5mm
|
|
|
What is the average CROWN WIDTH of a MAND CANINE?
|
11.0mm
|
|
|
What is the average CROWN WIDTH of a MAND 1st PREMOLAR?
|
8.5 mm
|
|
|
What is the average CROWN WIDTH of a MAND 2nd PREMOLAR?
|
8.0 mm
|
|
|
What is the average CROWN WIDTH of a MAND 1st MOLAR?
|
7.5 mm
|
|
|
What is the average CROWN WIDTH of a MAND 2nd MOLAR?
|
7.0mm
|
|
|
Determinants of prognosis? What should be considered?
|
- Case relapse
- Poor treatment planning - Pathological conditions - Genetic variation - Hypertonus and Hypertrophy of muscles - |
|
|
What kind of bend is an INTRUSION bend?
|
Second order
|
|
|
What kind of bend is an INSET bend?
|
FIRST ORDER
|
|
|
THIRD ORDER bends accomplish what kind of movement?
|
Torque
|
|
|
What are some indications for FIXED RETAINERS post orthodontic treatment?
|
a) differential retention
b) effective and reliable c) esthetically favourable d) good patient compliance e) long term and permanent retention f) aids in patients with reduced periodontal support |
|
|
What are the main disadvantages of FIXED RETAINERS?
|
- hygeine problems
- deteriorated effectiveness - discomfort - durability - reparability - physiological harm to soft and hard tissues |
|
|
Where is hte most commonly observed failure of a FIXED RETAINER?
|
- wire / composite interface due to insufficient placement of adhesive and/or abrasion wear
|
|
|
How often should checkups be on patients with FIXED RETAINERS?
|
Every 1 year
|
|
|
When are the phases of COMP ORTHODONTIC TREATMENT generally carried out?
|
PHASE I - 7-11 years
PHASE II - After eruption of most of the adult dentition |
|
|
What are some typical PHASE I treatments?
|
SAGITTAL (antero-posterior)
- headgear - functional appliances - active retainers TRANSVERSE - expanders VERTICAL CORRECTIONS - bite plane retainers SPACING CORRECTIONS - space maintainers - Nance appliances |
|
|
CLASS II skeletal can result from what?
|
- excessive growth of maxilla
- deficient growth of mandible |
|
|
What type of headgear can be used for CLASS II CORRECTION?
|
- Cervical headgear
- high pull headgear - combination |
|
|
What type of headgear can be used to correct CLASS III?
|
- reverse pull headgear
- chin cup |
|
|
How long does a headgear need to be worn to be effective?
|
10-12 hours per day
|
|
|
What are some side effects of headgear?
|
- unwanted extrusion of maxillary molars (typically with cervical) will cause mandible to move inferiorly and posteriorly
- negates Class II correction - distal tipping of molars |
|
|
What is a side effect of REVERSE PULL HEADGEAR?
|
- downward and backward rotation of the mandible
- lingual tipping of mandibular incisors |
|
|
What are the purposes of archwires?
|
- provide the FORCE to move teeth
- act as a TRACK along which teeth move - provide a PATTERN for the shape of the arch - exert force by being ENGAGED in the slot |
|
|
What are the properties of NiTi wire?
|
- very flexible
- used in de-rotating teeth - gentle force - less discomfort - continous force - movement occurs over a long period of time |
|
|
What is the advantage of Copper NiTi wire?
|
- When it is chilled it becomes dead soft, making it much easier to insert into brackets on badly crowded teeth. Make it more resistance to permanent deformation
- when it is warm it is activated |
|
|
What is the primary use of TMA?
|
- transitional wire and for detailing
- very expensive - high-spring back with lower force than steel - permanent set when bent |
|
|
What are the properties of ROUND WIRES?
|
- solid length of wire
- medium stiffness - used in middle of treatment (working wires) - used to open/close spaces, tip teeth, and do small tooth movements - can be multi-strand / any material |
|
|
What are the properties of RECTANGULAR WIRES?
|
- solid length of wire
- more stiff - used late in treatment - gives torque control of teeth - more accurate control to the teeth - less "slop" |
|
|
When orthodontists talk about 0.018 and 0.022 brackets, what are they talking about?
|
OCCLUSO-GINGIVAL dimension of bracket slot
|
|
|
What are the key determinants of habits effect on malocclusion?
|
- Intensity
- Duration - Frequency - angle of insertion |
|
|
What are the two main approaches to finger habit cessation that should be implemented?
|
First try BEHAVIOURAL MODIFICATION
then APPLIANCE |
|
|
Suggest a few clinical dental indicators of thumb suckers:
|
- constricted upper arch
- retroclined lower incisors - anterior open bite - proclined max teeth - tongue thrust - Class II skeletal |
|
|
When should unilateral crossbite with functional shift be corrected?
|
As early as possible
|
|
|
What is usually the cause of UNILATERAL CROSSBITE with FUNCTIONAL SHIFT?
|
- Narrow upper jaw
- Upper teeth not wide enough to form a perimeter around the lower teeth |
|

What kind of clasp is this?
|
ADAM'S CLASP
|
|

What kind of clasp is this?
|
ADAM'S CLASP
|
|
What kind of clasp is this?
|
ADAM'S CLASP
|
|
|
What are 2 key concepts when deciding on how to expand the maxilla?
|
- ALWAYS overexpand (half the width of a tooth)
- overexpand and retain |
|
|
When does the mid-palatal suture begin to close?
|
13-14 years old
|
|
|
Define FUCNTIONAL SHIFT:
|
- caused by an occlusal interference that requires the mandible to shift either anteriorly and/or laterally in order to achieve maximum occlusion
|
|
|
Skeletal crossbites may be caused and/or influenced by habits and other localized deforming factors:
|
- stomach sleeping posture
- digit / pacifier sucking habits - oral respiration - low tongue position - tongue thrusting |
|
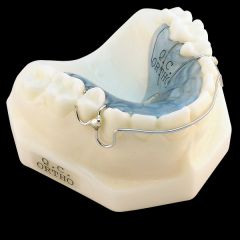
What kind of an appliance is this?
|
HAWLEY BOW
|
|

What kind of an appliance is this?
|
HAWLEY BOW
|
|

What kind of an appliance is this?
|
HAWLEY BOW
|
|
|
What are the INDICATIONS for ADAM'S CLASPS?
|
- good retention on teeth to be clasped
- one or two teeth in crossbite and adequate room to move them labially - can deliver forces to any/ all teeth in crossbite with mini-expansion screw |
|
|
What are the indications for OVER THE TUBE clasps?
|
- Poor retention on teeth to be clasped
- intention to use 2x4 fixed appliance - cannot deliver forces to any/ all teeth in crossbite - need to align anteriors |
|
|
What is the SEQUENCING for ADAMS CLASP CASES?
|
ONE
-------- Take impression and have acrylic appliance constructed with: - adam's clasps on 6's, e' or d's as required - thin posterior bite pads - mini expansion screw to move teeth in xbite labially TWO ------- insert appliance THREE ---------- Adjustment: - 1-2 quarter turns on insertion - 1 quarter turn every two to three days FOUR ------------ Monitor every 2 to 3 weeks and adjust clasps and tension of mini-expansion screw FIVE -------- Make sure that the tooth is not in traumatic occlusion before discontinuing activation or removing appliance. Overbite will hold the correction |
|
|
What is the sequencing for OVERTHETUBE CLASPS?
|
1) Place separators on M and D of 16 and 26 as required
2) fit and cement bands 3) take impression and have acrylic appliance constructed with: - OTT clasps (gingival to molar tube band) - thin post. bite pads - mini expansion screw 4) insert acrylic appliance 5) bracket four incisor teeth 6) place arch wires in progression |
|
|
When are 2x4 appliances indication?
|
- when space must be made
- cases where anteriors are rotated, crowded and/or in crossbite |
|
|
Where are 2x4 appliances contraindicated?
|
- when full braces will be used later and alignment of incisors isn't going to be significantly change at this time
- proper placement of brackets on laterals will tip roots distally and burn the roots against the canines |
|
|
How does one adjust the INNER BOW of the headgear?
|
- 4-5 mm away from incisors
- U loops facing down and aren't touching lower teeth - lips in a passive position when closed - ends of facebow fit passively into buccal tubes - anterior portion shouldnt interfere with lip posture |
|
|
How does one adjust OUTER BOW of headgear?
|
- proper force is delivered as required
- comfortable distance from face , cheeks |
|
|
How much tension is placed on headgear strap?
|
16 ounces
|
|
|
What are the steps in a COMPREHENSIVE ORTHO CASE?
|
1. DIAGNOSIS and TREATMENT PLANNING
--------------------------------------------------------------- radiographs models photos chart 2. ANCHORAGE PREPARATION --------------------------------------------- extra-oral (headgear) intra-oral (TPA, LHA) inter arch (class 2 or 3 elastics) intra arch (space gained from extractions) 3. EXTRACTION CONSIDERATIONS --------------------------------------------------- crowding incisor position curve of spee molar/cuspid OB/OJ Midlines 4. BANDING/BONDING/AW ---------------------------------------- 5. STAGE of A/W USE ------------------------------ Levelling / alignment phase 6. CANINE RETRACTION ----------------------------------- retract distally until it contacts the mesial of first premolar no retraction until placement of 0.018 SS with molar offsets (to prevent mesio-lingual movement after canine retrction complete place 0.016x0.022 for easy entry of 0.017x0.025 7. ANTERIOR CLOSURE ---------------------------------- four incisors gang-tied canines and premolars gangtied anterior closing loop opened to activate 8. POSTERIOR CLOSURE ------------------------------------ powerchair 6-6 with wire tied in individually on each tooth ant. teeth gangtied and powerchains place 9. DETAILING FINISHING ------------------------------------- 10. POST TREATMENT RECORDS ------------------------------------------------- pan, photos, models 11. RETAINERS ----------------------- positioneer acrylic Hawley fixed lingual invisible 12. RETENTION ------------------------- difficult if diagnosis and treatment plan not done properly 13. POST RETENTION -------------------------------- removal of third molars |
|
|
What are the treatment objectives in crowding cases?
|
- get the tooth into the mouth
- get tooth in non-rotated position if possible - protect labial support - prevent unwarranted iatrogenic spacing - prevent anterior crossbites from developing - prevent increase in OB - prevent retroclination of inciors - do not complicate further treatment - delay or procrastinate but act when necesary |
|
|
What are the CHIEF FACTORS when deciding a treatment plan for a case?
|
- BIG 5: molar, canine, OJ, OB, midline
- BIG 3: crowding, incisor position, curve of spee - age or development of occlusion - skeletal relationship / profile - probable options for future |

