![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
406 Cards in this Set
- Front
- Back
|
LIST 6 type of soft tissue injuries that can occur as complications:
|
- mucosal tears
- puncture - heat injury - abrasion/ avulsion - inadvertant incisions - crush injury |
|
|
MUCOSAL TEAR injuries usually result because of:
|
- careless retraction of a flap
- inadequate size of flap - uncontrolled pressure with elevator |
|
|
MUCOSAL TEAR injury is treated with:
|
- careful suture closure
- flaps survive because vascular perfusion of area is very rich |
|
|
PUNCTURE injuries usually occur because of:
|
- using sharp instrument (ie 301)
- slips off tooth and penetrates tissue - most commonly palatal tissues in maxilla and lingual tissues in mandible |
|
|
Treatment of PUNCTURE injury involves:
|
- irrigation of the wound and close f/u until the area heals (usually by secondary intention)
- leaving wound open allows drainage from the depth of the wound |
|
|
INADVERTANT INCISIONS usually results because of:
|
- lack of attention
Treated by suturing and appropriate wound care |
|
|
LIST SOME DENTOALVEOLAR COMPLICATIONS:
|
- root displacement
- damage to adjacent bone (tuberosity fracture, alveolar fracture) - damage to adjacent teeth - extraction of wrong tooth - root fracture - aspiration - swallowing of tooth - injury to regional nerves - injury to TMJ - oroantral communication - hemorrhage - |
|
|
What are radiographic predictors of 3rd molar proximity to IAN?
|
- darkening of the root
- deflection of the root - diversion of the canal - narrowing of the root - interruption of the white lines |
|
|
What are some indications for removal of a tooth (exodontia)?
|
- caries
- pulpal necrosis - perio disease - orthodontics - pathology - malposed teeth - cracked/fractured teeth - impacted teeth - radiation therapy - financial issues - teeth involved with jaw fractures |
|
|
What are some SYSTEMIC contraindications to exodontia?
|
- Uncontrolled leukemia / lymphoma
- Uncontrolled metabolic diseases - Uncontrolled cardiac issues - Radiation therapy - Severe / uncontrolled dysrhythmias - pregnancy - bleeding disorders - corticosteroids / bisphosphanates / immunosuppressors / cancer agents |
|
|
What are some LOCAL contraindications to exodontia?
|
- infection
- malignancy - pericoronitis - radiation therapy |
|
|
What things do you want to assess clinically and radiographically before extracting a tooth?
|
- access to the tooth
- mobility of the tooth - condition of the crown - Adjacent teeth - Relationship to vital structures (IAN, mental nerve, sinus) - configuration of roots - condition of surrounding bone - |
|
|
What are the three mechanical principles used in oral surgery?
|
- lever
- wedge - wheel and axle |
|
|
What are the five major MOTIONS used to luxate teeth and expand bony sockets?
|
- apical pressure
- buccal / palatal pressure - buccal force - rotation - traction |
|
|
On the MAXILLA which bone is THICKER / THINNER ?
|
Palatal (thick) -> Buccal (thinner)
|
|
|
On the MANDIBLE which bone is THICKER / THINNER?
|
Buccal (thicker) > Lingual (thinner) (from midline to premolars)
|
|
|
Describe the 5-STEP PROGRAM for extraction a tooth:
|
1. loosening of the soft tissue attachment
2. luxation with dental elevator 3. adaptation of the forceps to the tooth 4. luxation of the tooth with the forceps 5. removal of the tooth from socket |
|
|
Define "BIOPSY":
|
Biopsy is the removal of a representative section of living tissue from a lesion for microscopic examination 'ex viva' and histopathologic diagnosis
|
|
|
What is the purpose of a BIOPSY?
|
to determine whether a lesion is inflammatory, developmental, reactive, systemic or neoplastic (benign of malignant).
|
|
|
List the criteria FOR DOING A BIOPSY:
|
1. Anything that doesn't respond to local treatment within 7-14 days
2. lesions that interfere with local function 3. Lesions that show slow enlargement or sudden growth 4. Lesions with no apparent etiology 5. Longstanding white or red lesions 6. Radiolucent or Radiopaque bone lesions 7. Lesions associated with pain, parasthesia, anaesthesia of unknown etiology 8. Deep masses (tongue, buccal mucosa, lip) |
|
|
List the criteria for NOT DOING A BIOPSY:
|
1. Normal anatomic structures -> leukoedema, fordyce granules, etc.
2. Traumatic lesions 3. Inflammatory lesions which may respond to local treatment 4. Lesions that require biopsy techniques beyond your surgical ability -> ie difficult anatomy |
|
|
What are the three types of BIOPSY techniques?
|
- fine needle aspiration
- incisional biopsy - excisional biopsy |
|
|
What are 3 INDICATIONS for doing ASPIRATION BIOPSY?
|
1. determine the presence and type of fluid within a lesion
2. exploration of an intraosseous lesion indicated 3. initial diagnosis of subcutaneous masses |
|
|
What are the 3 indications for doing an INCISIONAL BIOPSY?
|
1. Size limitations > 1cm in diameter
2. Hazardous location of the lesion 3. Great suspicion of malignancy |
|
|
How would you determine normal soft tissue margins during biopsy?
|
- NORMAL tissue on deep surface - extend ~ 2 mm
- IRREGULAR or indistinct margins should go ~ 5 mm |
|
|
One should NEVER do incisional biopsy on what two types of lesions?
|
- PIGMENTED - may stimulate malignant transformation or seed into normal tissues
- VASCULAR - life threatening hemorrhage |
|
|
What are the 3 indications for EXCISIONAL BIOPSY?
|
- small lesions < 1 cm
- Lesions on clinical exam seem benign - complete excision with a margin of normal tissue without mutilation |
|
|
What shape is used to do EXCISIONAL BIOPSY? Why?
|
wedge "canoe" shape - to approximate the tissues better and have better wound closure
|
|
|
What is the SAAAAAB rule?
|
- Size
- Appearance - Anesthetic - Anatomic considerations - Avoid (excess trauma) - Adequate disposition - Blade |
|
|
When is an OPEN / SURGICAL technique warranted during extraction?
|
- used for removing roots that were fractured
- removal of multiple teeth - ankylosed teeth - hypercementosis / widely divergent roots - impacted teeth (GENERALLY if there is a need for excessive force then do OPEN) |
|
|
What are the FIVE basic principles of incisions for flaps?
|
1. sharp blade / proper size
2. continuous firm stroke 3. avoid cutting vital structures 4. should be properly placed: sound bone 5. Should be held perpendicular to the epithelial surface |
|
|
What are the FIVE characteristics of a flap?
|
1. outlined by surgical incision
2. carries its own blood supply 3. allows access to underlying tissues 4. can be replaced in the original positions 5. can be maintained with sutures - heal |
|
|
What are the DESIGN parameters of a flap?
|
1. base of flap must be broader than free margin
2. must be adequate size 3. full thickness mucoperiosteal 4. incisions should be made over intact bone 5. avoid injury to vital structures 6. |
|
|
How long does the canine have to travel to erupt into normal position?
|
~22 mm
|
|
|
What is the most important first step when dealing with impacted canine?
|
LOCALIZATION - using any technological means to figure out the exact position of the impacted tooth.
|
|
|
What is the most common site of IMPACTED CANINE?
|
Palatal
|
|
|
What are the main problems associated with impacted canines?
|
1. Adjacent teeth migrate due to canine pressure on central and laterals
2. Root resorption of adjacent teeth 3. Cystic degeneration of follicle 4. Cleft palate 5. Edentulous patient 6. Pain |
|
|
What is the most commonly used blade in oral surgery?
|

No. 15
|
|

Name this instrument and it's uses:
|
No. 11 Blade - for puncturing / stabbing incisions
|
|

Name this instrument and it's uses:
|
No. 12 Blade - for maxillary tuberosity area
|
|

Name this instrument and its function:
|
Molt No. 9 Periosteal elevator
- To elevate papillae and soft tissue flaps |
|

Name this instrument:
|
Minnesota retractor
|
|

Name this instrument and its use:
|
Weider retractor - for retracting the tongue
|
|

Name these instruments:
|
Adson forceps - with and without teeth
|
|

Name these instruments:
|
Rangeurs - for cutting / smoothing bone
|
|

Name this instrument:
|
bone file - used in pulling motion
|
|

Name this instrument:
|
Curette
|
|
Name this instrument and it's components;
|
Dental elevator (straight)
Handle Shank Blade |
|

Name these instruments:
|
Triangular dental elevator - for removing root tips
|
|

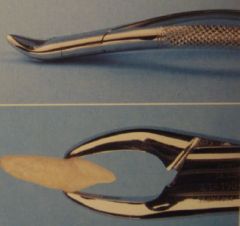
Name this instrument and its components:
|
Dental forceps
Handle Hinge Beak |
|
Identify this forcep and what teeth it is generally used for:
|
No. 150
Universal forceps for use with maxillary teeth (conical roots, no bifurcations). |
|

Identify these forceps and their use:
|
No. 53 L or R
For Maxillary Molars - buccal bifurcation and palatal conical |
|

Name this instrument and it's uses:
|
No 151. and 151A
For mandibular teeth and mandibular premolars (conical) |
|

Name this instrument and its uses:
|
No. 17 for mandibular molars (buccal and lingual bifurcation)
|
|

Name this instrument and its uses:
|
No. 87 - for Mandibular molars (buccal and lingual bifurcation)
|
|
|
What is the MAXIMUM RECOMMENDED DOSE of 2% Lidocaine for a NORMAL patient?
|
4.4 mg / kg
|
|
|
What is the MAXIMUM RECOMMENDED DOSE of 2% Lidocaine w 1:100,000 epinephrine for a NORMAL patient?
|
7.2 mg / kg
|
|
|
What is the MAXIMUM RECOMMENDED DOSE of epinephrine for a normal patient?
|
0.2 mg
|
|
|
What is the MAXIMUM RECOMMENDED DOSE of epinephrine for an ASA 3 or 4 patient?
|
0.04 mg
|
|
|
What are the terminal branches of the PTERYGOPALATINE NERVE?
|
- greater and lesser palatine
- pharyngeal nerve - nasopalatine - orbital |
|
|
What are the 5 different designs of FTMP flaps?
|
- envelope
- 3 cornered - 4 cornered - semilunar - Y shaped |
|
|
How does healing by PRIMARY INTENTION occur?
|
- Involves epidermis and dermis without total penetration of the dermis healing. This is when wounds are approximated together.
|
|
|
How does healing by SECONDARY INTENTION occur?
|
The wound is allowed to granulate. Takes much longer and forms more of a scar.
|
|
|
The INFERIOR MEATUS receives from which structure?
|
Nasolacrimal duct
|
|
|
The MIDDLE MEATUS receives from which?
|
- frontal sinus
- maxillary sinus - ethmoidal sinus (anterior and middle) |
|
|
The SUPERIOR MEATUS receives from where?
|
- posterior ethmoidal sinuses
|
|
|
The SPHENOIDAL SINUS drains into where?
|
- spheno-ethmoidal recess
|
|
|
What are the most common areas of litigation for dentists?
|
1. Extraction of wrong tooth
2. Nerve damage (ie lingual nerve) 3. Failure to diagnose a lesion/condition/disease/etc 4. Implant complications 5. Failure to refer adequately 6. TMJ injury |
|
|
What are some things that should be discussed with a patient as part of informed consent?
|
1. Their specific problem / diagnosis
2. The proposed treatment 3. Common/possible side effects 4. Common/possible complications 5. Treatment alternatives 6. No guarantee of treatment outcome 7. Risk of refusing treatment |
|
|
What are the 4 main purposes of doing adequate informed consent ?
|
- engaging the patient in his/her own health
- creating a better patient/practitioner relationship - encourages physician to thoroughly review patients treatment options - avoid litigation and discontent when complications arise |
|
|
What are the borders of the INFRATEMPORAL FOSSA?
|
ANTERIORLY: by the infratemporal surface of the maxilla and the ridge which descends from its zygomatic process
POSTERIORLY: by the articular tubercle of the temporal and the spinal angularis of the sphenoid SUPERIORLY: by the greater wing of the sphenoid below the infratemporal crest, and by the under surface of the temporal squama, containing the foramen ovale, which transmits the mandibular branch of the trigeminal nerve, and the foramen spinosum, which transmits the middle meningeal artery INFERIORLY: by the medial pterygoid muscle attaching to the mandible MEDIALLY: by the lateral pterygoid plate LATERALLY: by the ramus of mandible, which contains the mandibular foramen, leading to the mandibular canal through which the inferior alveolar nerve passes. This also contains the lingula, a triangular piece of bone that overlies the mandibular foramen antero-medially. Finally, the mylohyoid groove descends obliquely transmitting the mylohyoid nerve the only motor branch of the anterior division of the trigeminal nerve. |
|
|
What are some preventative measures one would undertake to prevent maxillary tuberosity fracture during extraction?
|
- examination of pre-operative radiographs
- use of controlled forces - support the alveolus - removal of buccal bone - section the tooth to be extracted |
|
|
What are the steps one would undertake if the maxillary tuberosity happens to fracture off when trying to extract the third molar?
|
IF BONE IS COMPLETELY REMOVED:
- it should NOT be replaced - careful repositioning of soft tissue flap - smooth any sharp edges that may have been caused by fracture - DO NOT PROBE the socket if apex was near sinus floor IF BONE IS STILL ATTACHED TO PERIOSTEUM: - tooth stabilized and buccal bone carefully detached from the tooth - if soft tissue is elevated from the bone the blood supply will be severed and cause necrosis |
|
|
You are extracting #26 when it suddenly falls into the throat and the patient starts violently coughing, what do you do in this unfortunate incident?
|
adf
|
|
|
What are the components of GELFOAM?
|
gelatin
|
|
|
What is SURGICEL made of?
|
oxidized cellulose
|
|
|
Write a prescription for AMICAR:
|
dasfa
|
|
|
Patient who has well-controlled asthma falls into which ASA category?
|
ASA 2 (II)
|
|
|
What does THROMBIN do and what is it's factor number?
|
Thrombin helps convert Fibrinogen to Fibrin.
It is factor IIa. |
|
|
You get an oroantral communication during oral surgery. What do you do?
|
adfad
|
|
|
What is the most common blood condition?
|
Von Willebrands disease
|
|
|
What are the 5 main motions during luxation of a tooth?
|
- apical pressure
- buccal / palatal pressure - traction - rotation - elevation |
|
|
How would you biopsy 2x2 cm lesion on the lateral border of the tongue?
|
INCISION vs EXCISION?
|
|
|
The membrane of the maxillary sinus is called?
|
Schneiderian membrane
|
|
|
What are the 4 different tests used to test coagulability?
|
- Bleeding time
- Platelet count - PT - aPTT |
|
|
What is the normal platelet count?
|
150,000 - 450,000 per uL (microliter)
|
|
|
What are some predisponsing factors for impacted canine?
|
adfadf
|
|
|
What are some problems associated with having impacted canines?
|
adf
|
|
|
Someone with Hemophilia will have deficiency in what pathway of the coagulation cascade?
|
INTRINSIC
|
|
|
What are four indications for patients who could benefit from nitrous oxide sedation?
|
1) anxious / fearful patients
2) those with low coping ability (e.g. behaviour mgmt problems, dental fear, anxiety and needle phobic, prominent gag reflex, etc) 3) special needs patients that COMMUNICATE 4) those with special treatment needs (e.g. emergency, complicated and prolonged tx, minor oral surgery, special procedures, etc) |
|
|
What are the main contraindications for N2O sedation in patients?
|
1) Inability to communicate
2) Inability to nose breathe 3) severe psychiatric and/or behavioural/personality disorders 4) Vit B12 or folate deficiency/disorders 5) COPD 6) neuromuscular disorders (e.g. MS) 7) cancer undergoing chemotherapy with Bleomycin drugs 8) Patients during first trimester of pregnancy |
|
|
What are HEAT INJURIES usually caused by?
|
- "hot out of the autoclave" instruments
- allow instruments to cool before use, or immerse in cold saline to get rid of heat |
|
|
What is the management of a HEAT INJURY?
|
- no treatment
- vaseline, bacitracin, neosporin - if burn is significant then refer |
|
|
How does one prevent ABRASION/AVULSION INJURIES?
|
- lip retraction
- being aware of surroundings ABRASION - wound care AVULSION - primary closure vs graft |
|
|
CRUSH INJURIES are usually due to:
|
- uncontrolled forces and improper placement of instruments
|
|
|
Fracture of MAXILLARY ALVEOLUS occurs in which three situations most often?
|
- lone standing molars
- canines - distal molars (3rd molars/ tuberosity) |
|
|
How does one prevent FRACTURE OF MAXILLARY ALVEOLUS?
|
- examination of pre-operative radiographs
- use of controlled forces - support the alveolus - removal of buccal bone and sectioning of teeth |
|
|
You are performing an extraction on a lone standing #18 and the maxillary alveolus fractures - what do you do?
|
- if bone has been COMPLETELY REMOVED it should NOT be replaced
- careful repositioning of soft tissue flap - smooth any sharp edges that may have been caused by the fracture - if portion of fractured bone is at apex near sinus floor then DO NOT PROBE THE SOCKET IF THE BONE IS STILL ATTACHED TO PERIOSTEUM - tooth stabilized and buccal bone carefully detached from tooth - if soft tissue is elevated off the bone then blood supply will be severed - if segment can't be detached from the tooth then splint for 6-8 weeks , tooth then can be extracted with open technique |
|
|
What is the most common injury to adjacent teeth during EXODONTIA?
|
- fracture or dislodgement of an adjacent restoration
|
|
|
Which conditions increase risk of fracture/dislodgement of an adjacent restoration?
|
- large restorations
- severely carious teeth - teeth in opposing arch - crowns |
|
|
What do you do if an adjacent tooth is mobile after extraction?
|
- reposition tooth
- stabilize - check occlusion |
|
|
What is the most common cause of malpractice lawsuits against dentists?
|
Extraction of wrong tooth
- inadequate attention to pre-op assessment - improper communication - ortho cases must be very careful |
|
|
What is the treatment of a WRONGLY EXTRACTED TOOTH?
|
- quick replacemtn into socket
- if orthodontic then call orthodontist and ask if tooth extracted can be substituted - defer correct tooth extraction for 4-5 weeks - if not recognized immediately then inform the patient and see if the tx plan can be altered, offer implant free of charge |
|
|
How does one prevent extraction of wrong tooth?
|
- focus attention on procedure
- check with patient and assistant to ensure that correct tooth is being extracted - check, recheck, images, and records to confirm correct tooth |
|
|
What type of roots are more likely to be fractured?
|
- long
- curved - divergent roots that lie in dense bone |
|
|
Which is the tooth root most commonly displaced? and where?
|
- maxillary molar root
- maxillary sinus |
|
|
What do you check if you displace a root tip into the sinus?
|
- identify size of root lost in sinus
- was there any infection of tooth or periapical tissues? - is the sinus healthy? |
|
|
What is the treatment of a displaced root tip into maxillary sinus?
|
- if displaced tooth fragment is small (2-3mm) and the tooth and sinus have no pre-existing infection, then surgeon should make a brief attempt at removing the root
- FIRST take xray - IRRIGATE through the small opening in the socket apex and suction irrigating solution from the sinus via the socket. This occasionally flushes the root from the sinus through the socket. - CHECK suction solution and CONFIRM radiographically that tooth has been removed - If NOT SUCCESSFUL no additional treatment should be done through socket apex, and root tip should be left in the sinus - patient should be notified of decision and given proper follow-up instructions for regular monitoring of root and sinus - if a LARGE or ENTIRE tooth displaced into sinus, it should be removed via CALDWELL LUC approach by an OMFS. |
|
|
Impacted third molars are more commonly displaced into which space?
|
INFRATEMPORAL SPACE
- elevator may force tooth posteriorly through periosteum into the infratemporal fossa - tooth usually lateral to lat. pterygoid plate and inferior to lateral pterygoid muscle |
|
|
You are performing tooth extraction when tooth suddenly falls into the patients throat? What do you do?
|
- Turn towards the surgeon and place patient in position with mouth towards floor
- encouraged to cough and spit tooth out onto the floor - suction - tooth has the potential to be swallowed or aspirated NO COUGH / NO RESP DISTRESS : most likely tooth was swallowed and has travelled down esophagus into stomach COUGHING / SOB: tooth aspirated into trachea BOTH CASES: should be transported to emergency room |
|
|
What is the management if your patient aspirates the extracted tooth?
|
- Maintain airway and breathing
- supplemental O2 may be necessary - Consult for removal via bronchoscope |
|
|
Which nerves are most likely to be injured during exodontia?
|
- mental nerve
- lingual nerve - buccal nerve - nasopalatine nerve - inferior alveolar nerve |
|
|
What are RADIOGRAPHIC PREDICTORS of NERVE PROXIMITY?
|
- darkening of root
- deflection of root - narrowing of root - interruption of white lines - diversion of canal |
|
|
Your patient complains of pain in TMJ following the procedure, what do you do?
|
- moist heat
- rest for the jaw - soft diet - 600-800mg Ibuprofen q4-6h x 48hrs then prn - APA 500-1000mg q4-6h if cannot take NSAIDS |
|
|
What do you do if you get an OROANTRAL COMMUNICATION following surgery?
|
IF <2MM OPENING:
- no additional surgical tx - ensure high quality clot (gauze pressure, pack hemostatic agent like gelfoam/spongostan. - SINUS PRECAUTIONS IF 2-6MM OPENING: - blood clot - gelfoam / surgicel - figure eight suture - sinus precautions - antibiotics - decongestants IF 7MM OR GREATER: - refer to OMFS for primary closure flaps - may need buccal advancement flap w/wout fat graft - palatal pedicle flap |
|
|
What are SINUS PRECAUTIONS:
|
- no nose blowing for 1 week
- no violent sneezes - no spitting or vigorous rinsing - NO SMOKING - cover with amox or with clav, cipro and azithromycin |
|
|
PROTHROMBIN TIME measures with system?
|
EXTRINSIC
|
|
|
Which factors are tested for in PROTHROMBIN TIME?
|
- II
- VII - IX - X |
|
|
What is the NORMAL PROTHROMBIN TIME?
|
11-13seconds
|
|
|
What is a NORMAL INR?
|
0.8 - 1.2
|
|
|
List three conditions that will PROLONG PROTHROMBIN TIME?
|
- warfarin
- Vit K deficiency - Liver disease |
|
|
PARTIAL THROMBOPLASTIC TIME tests which system?
|
INTRINSIC CLOTTING
|
|
|
Which test detects patients with some hereditary forms of coagulopathy?
|
PTT
|
|
|
What is the normal platelet count?
|
150,000 - 450,000 platelets / uL
|
|
|
Which platelet count will cause bleeding issues?
|
< 50,000 / uL
|
|
|
Describe the difference between hemorrhage in the three main types of vessels:
|
ARTERY: bright red, pumping
VENOUS: steady flow, dark red CAPILLARY: slow flow |
|
|
How can PRIMARY HEMORRHAGE be avoided?
|
- good vision
- clean incisions - flap reflection - good suctioning - knowledge of anatomy - tying off vessels - removal of excess granulation tissue |
|
|
Secondary hemmorhage may result because of what?
|
infection breaking down initial clot
>24 hours following surgery - poor initial closure of wound, trauma of rinsing, chewing, vigorous tooth brushing |
|
|
Which part of the brain is responsible for the vomiting sensation?
|
Area postrema
|
|
|
What are some contraindications to morphine?
|
ABSOLUTE: allergy
RELATIVE: head injury, pts with convulsive disorders, hypotension, asthma, hypothyroidism, Addison's disease, severe renal or hepatic dysfunction, COPD |
|
|
What are the four main routes of sedation?
|
- oral
- rectal - IM - IV |
|
|
What is our goal with patient sedation in dentistry?
|
light level of sedation that lessens anxiety and stress, and makes local delivery more effective
|
|
|
What is the most important thing to remember when placing a patient under sedation?
|
- patient should remain:
- cooperative - entirely responsive to direction - no resp or CV depression |
|
|
What are the characteristics of an ideal sedative agent?
|
- ameliorate a transient anxiety state without depression of vital functions
- wide safety range - should be effective after single dose - rapid uptake and absorption (rapid onset) - adequate duration with rapid recovery - relaxation of skeletal muscles is desireable (not mandatory) - minimal toxicity and side effects - antiemetic properties are desireable - inexpensive - suitably long shelf life - not habituating or addicting - should potentiate the desired effects of a concomitantly used agent without significant depressive effects |
|
|
What are the objectives with patient sedation?
|
- pt's mood should be altered to allay apprehension, anxiety or fear
- elevation of pain threshhold - consciousness intact, cooperative, respond rationally to verbal command - amnesia is desireable |
|
|
Sedation may be helpful to affect what physiological things?
|
- control excessive secretions from salivary glands
- help control gagging - help control motor disturbances - relaxation |
|
|
What are some factors that modify dosage of sedatives?
|
- pain threshhold
- weight - age - presence of a pathologic condition - concomitant meds - absorption from GI tract |
|
|
PAIN THRESHOLD can vary depending on what thigs?
|
- emotional state
- degree of fatigue - age - sex - past experiences - pain - etc |
|
|
How are children different than adults?
|
- increased C.O. to vessel-rich group
- decreased redistribution due to decreased muscle and fat - decreased binding to plasma protein - increased BMR and increased BBB penetrance |
|
|
How are elderly generally different from adults?
|
- decreased GI absorption
- alteration in number and character of receptor sites - change in body fat; decrease total body water - decrease in plasma albumin - decreased liver biotransformation and renal excretion rates |
|
|
What are the routes of administration for sedative drugs?
|
- inhalational
- oral + sublingual - rectal - subcutaneous - IM and intralingual |
|
|
What is the most convenient route of sedative administration?
|
oral / sublingual
|
|
|
What is the oldest and most common route of administration of sedatives?
|
oral/sublingual
|
|
|
What are the advantages of ORAL/SUBLINGUAL route of sedative admin?
|
- almost universal acceptability
- easy of administration - low cost - decreased incidence and severity of adverse reactions - no needles, syringes, equipment |
|
|
What are the DISadvantages of ORAL/SUBLINGUAL route of sedative admin?
|
- reliance on patient compliance
- prolonged latent period - erratic and incomplete absorption of drugs from GI tract - inability to titrate - inability to lighten or deepen - prolonged duration of action |
|
|
When is the RECTAL route of admin. used?
|
- uncooperative children who refuse to take oral meds
|
|
|
What types of drugs is RECTAL route reserved for?
|
analgesics
antiemetics |
|
|
IM and intralingual route avoids which metabolism?
|
- FIRST PASS METABOLISM
|
|
|
What are the Advantages of IM drug admin?
|
- more rapid onset vs PO (~ 15 min)
- shorter time to maximal clinical effect (15-30min) - more reliable absorption than oral/rectal - pt cooperative not as essential as with IV (poor veins, disruptive pt's) |
|
|
What are the DISAdvantages of IM drug admin?
|
- inability to titrate
- inability to reverse - prolonged duration of drug effect - injection needed - possible local tissue injury |
|
|
Why is injection a disadvantage of IM admin?
|
- specialized equipment needed
- knowledge - skill to adminsiter injection and monitor pt |
|
|
What are the four main sites for IM drug admin?
|
- gluteal area
- ventrogluteal area - vastus lateralis - deltoid area |
|
|
Which is the least well perfused area for IM administration?
|
- gluteal region
|
|
|
Where is the largest reservoir for IM administration?
|
- vastus lateralis
|
|
|
Define GENERAL ANAESTHESIA
|
a state of unrousable unconciousness to which analgesia and muscle relaxation is added to produce balanced anaesthesia
|
|
|
Define ANALGESIA:
|
absence of pain
|
|
|
Define SEDATION:
|
an altered level of consciousness in which the patient, although awake, has a decreased level of fear and anxiety
|
|
|
When is LOCAL ANAESTHETIC contra-indicated?
|
- unco-operative patients
- infection around the injection site - patients with a major bleeding diathesis - most major surgery |
|
|
What are some CONTRA-INDICATIONS for CONSCIOUS SEDATION?
|
- cardiorespiratory, renal, liver, or psychiatric pathology
- an unescorted patient or one unable or unwilling to conform to the requirements of conscious sedation - a demonstrated adverse reaction to sedative agents - pregnancy, during which BENZO's should be avoided |
|
|
NITROUS OXIDE has what properties?
|
- analgesic
- sedative (greater) |
|
|
Why does NITROUS OXIDE have very rapid distribution?
|
- poorly insoluble
- does not enter any of the body's metabolic pathways |
|
|
What is the indication for NITROUS OXIDE?
|
- anxious patients
- children |
|
|
What are the contraindications for NITROUS OXIDE?
|
- upper airway obstruction (ie cold, emphysema)
- Pregnancy (first trimenster) - complex medical history |
|
|
A NITROUS OXIDE machine will not deliver any less than how much oxygen?
|
30% O2
|
|
|
What is the dose of THIOPENTONE?
|
4mg / kg
|
|
|
What is the dose of PROPOFOL?
|
2.5 mg / kg
|
|
|
What is the dose of KETAMINE?
|
1-2mg / kg
|
|
|
What are the steps of a SIMPLE TOOTH EXTRACTION?
|
- test effectiveness of LA with pointed end of periosteal elevator
- sever gingivodental fibers with same end of elevator - Elevate the tooth - Luxate and extract - Examine the root for complete extraction - carefully palpate the apical region with a curette - remove periodontal granulation tissue with Lucas curette or rongeur - Palpate the alveolar process for sharp edges and undercuts / perform alveoloplasty as necessary - suture gingival tissues if necessary - place guaze dressing, check for hemostasis prior to dismissing patient - give post-op instructions, analgesic prescription, and follow up appointment if necessary |
|
|
What are the phases of bone healing following extraction of a tooth?
|
- hemorrhage and clot formation
- organization of clot by formation of granulation tissue - replacement of granulation tissue by connective tissue and epithelialization of the site - replacement of connective tissue by fibrillar bone - remodelling of the alveolar bone and bone maturation |
|
|
What are POST-OP instructions following extraction?
|
- bite on gauze for 20 min, if bleeding persists place another piece of gauze for another 20 min
- be careful not to bite cheek, lip, or tongue while anaesthesized - do not rinse mouth today - red-colored saliva may be apparent for 12-24 hours - if necessary, take NSAIDS prn pain - drinking (but not rinsing) is encourage, try to stay away from hot liquids first day - try to eat a soft diet (soup, jello) - slight swelling may be expected to accompany removal of teeth - sinus precautions (only if oro-antral communcation occurs): don't blow nose, sneeze through mouth, no smoking, no sucking through straws - call if questions or concerns |
|
|
What is the mechanism of action of ASPIRIN?
|
- suppresses production of prostaglandins and thromboxanes due to irreversible inactivation of cyclooxygenase (COX) enzyme
|
|
|
What is the average lifespan of a platelet?
|
5- 9 days
|
|
|
How does WARFARIN work?
|
- blocks Vit K epoxide to Vit K reduced form
- Reduced Vit K is essential for activation of certain factors - has NO effect on previously formed thrombus |
|
|
What are the Vit K dependent factors?
|
Factor II, VII, IX, X
|
|
|
When can the PEAK anticoagulant effect be achieved with WARFARIN?
|
72-96 hours
|
|
|
Define PROTHROMBIN TIME:
|
Time required for blood to coagulate
|
|
|
How is PT test performed?
|
- adding mixture of calcium and thromboplastin to citrated plasma
|
|
|
What is the average optimal treatment range for WARFARIN?
|
2.0 - 3.0 INR
|
|
|
What is the normal PT time?
|
10 - 12 seconds
|
|
|
What is the normal PTT time?
|
30-45 seconds
|
|
|
What is the normal INR range?
|
1-2
|
|
|
What are the two components to PAIN?
|
- pain perception
- pain reaction |
|
|
What are some mediators of inflammation that are released during tissue damage?
|
- bradykinin
- serotonin - histamine - eicossanoids - cytokines - substance P |
|
|
Pain receptors (nociceptors) record what kind of stimuli?
|
- bare nerve endings record:
- occurence - duration - location of sensation |
|
|
Define ANALGESIC:
|
drug capable of reducing or eliminating pain on systemic administration without ordinarily impairing consciousness
|
|
|
What are the differences of NARCOTICS vs NON-NARCOTICS?
|
- MOA
- Relative efficacy against severe pain - presence of anti-inflammatory effects - relative incidence and types of adverse effects - drug dependence / abuse liability |
|
|
What are the 3 main actions of NARCOTICS?
|
1) elevation of pain threshold
2) modifying the reaction to pain 3) induction of lethargy and sleep |
|
|
What is the mechanism of action of NARCOTICS?
|
- centrally via opioid receptors (some peripheral analgesic effects)
- usually act at Mu receptors - all opioid receptors have analgesic effects |
|
|
What are some general effects when MU receptors are activated?
|
- resperitary depression
- euphoria - addictive potential |
|
|
What are some general effects when KAPPA receptors are activated?
|
- miosis
- sedation - dysphoria - psychomimetic effects |
|
|
What are the general effects of DELTA receptors?
|
- behaviroural
- epileptogenic |
|
|
Where are OPIOID RECEPTORS primarily located?
|
- substantia gelatinosa
- trigeminal nucleus - brainstem solitary nucleus and area postrema - infundibulum of hypothalamus - medial thalamus - limbic system (HIGHEST CONCENTRATION) - periaqueductal grey matter of mesencephalon |
|
|
Where is the highest concentration of OPIOID RECEPTORS?
|
Limbic system
|
|
|
What are ENDORPHINS?
|
endogenous opiates
|
|
|
What are the three classes of NARCOTIC ANALGESICS?
|
1) NATURAL constituents of opium (Morphine, Codeine, Heroin)
2) SEMI-SYNTHETIC modifications of the morphine molecule (Oxycodone, hydromorphone) 3) SYNTHETIC (meperidine, fentanyl, methadone, propoxyphene) |
|
|
TRUE or FALSE: There is a ceiling doseage for narcotics?
|
FALSE
|
|
|
What is the prototype / gold standard MU agonist?
|
MORPHINE
|
|
|
What are the general effects that morphine has?
|
- analgesic
- sedative - antitussive - constipative - histamin releasing - miotic - convulsive - respiratory depressant effects |
|
|
What are the ABSOLUTE contraindications for morphine?
|
ALLERGY
|
|
|
What are the RELATIVE contraindications for MORPHINE?
|
- head injury
- Pts with convulsive disorder - hypotension, asthma, hypothyroidism, Addison's disease, severe renal or hepatic dysfunction, COPD |
|
|
With MORPHINE useage tolerance develops to WHICH effects?
|
- analgeic
- euphoric - respiratory depressant - hypotensive - emetic DOES NOT DEVELOP TO: - miosis - constipation - bradycardia |
|
|
What are the standard doses of morphine?
|
5-10 mg IV
10 mg Morphine IV = 60mg Morphine PO not as effective orally due to poor absorption |
|
|
How potent is MEPERIDINE?
|
1/10 as potent as morphine
0.1 of MORPHINE |
|
|
What kind of receptors does MEPERIDINE target?
|
Mu agonist
|
|
|
How potent is CODEINE?
|
1/12 as potent as MORPHINE
|
|
|
What is a problem with CODEINE use in general population?
|
7-10% of population is deficient in Cytochrome CYP2D6 which converts codeine into active analgesic metabolites
|
|
|
What receptors does OXYCODONE affect?
|
- MU and mild KAPPA agonist
|
|
|
WHat is one advantage of OXYCODONE over MORPHINE?
|
- more oral bioavailability
- oral oxycodone more potent than morphine |
|
|
What is FENTANYL primarily used for?
|
- IV sedation
- General anaesthesia |
|
|
What is the potency of FENTANYL?
|
100x more potent than parenteral morphine
|
|
|
What are the effects of NALOXONE?
|
- primary therapeutic indication is treatment of NARCOTIC-INDUCED RESPIRATORY DEPRESSION
- also reverse euphoric, analgesic, sedative, miotic and GI effects - when given in presence of narcotic will: - prevent opioid effects if given just before or at same time - reverse effects if given after - can precipitate withdrawal syndrome **SHORT DURATION OF ACTION** |
|
|
What is the DOSING of NALOXONE?
|
ADULTS: 0.4mg IV, IM or SC
CHILDREN: 0.01mg / kg Repeat q2-3min If no response after 10mg - differential for resp. depression |
|
|
What are the properties of NSAIDS?
|
- reduce or control pain primarily by directly inhibiting the biochemical mediators of pain at the site of injury
- all NSAID's share common properties: ANALGESIC, ANTI-INFLAMMATORY, and ANTI-PYRETIC |
|
|
TRUE or FALSE: There is a correlation between the anti-inflammatory and analgesic effects of NSAIDS.
|
FALSE : no correlation
|
|
|
What are the pharmacodynamics of NSAIDS?
|
- inhibition of COX1 and COX2
- blocks Prostaglandin cascade that follows tissue damage and would otherwise stimulate and sensitize peripheral nociceptors - spinal inhibitory action on sensitization of pain induced by the activation of glutamate and substance P - central analgesic effect in the brain (less understood) |
|
|
What is the "housekeeping " enzyme?
|
- expressed in most tissues but variably
- regulates normal cellular processes (gastric cytoprotection, vascular homeostasis, platelet aggregation, and kidney function) |
|
|
TRUE or FALSE: Combining NSAIDs is not recommended.
|
TRUE
|
|
|
TRUE or FALSE: NSAIDs have a ceiling dose for pain control and therefore are more useful in severe pain.
|
FALSE: Have a higher ceiling dose which makes it LESS useful in severe pain
|
|
|
How long does the decrease in platelet aggregation that follows NSAID use take to reverse/
|
within 24 hours
|
|
|
What is the advantage of using COX2 inhibitor NSAID?
|
- reduce risk of serious GI adverse effects (gi ulceration, bleeding)
- spare platelet function - share same potential as nonselective NSAIDs for renal toxicity - increased incidence of CV thrombotic events, edema, HTN |
|
|
TRUE or FALSE: COX 2 inhibitors when used eliminate the GI adverse effects normally associated with non-selective NSAIDs?
|
FALSE - reduce the risk but dont eliminate them
|
|
|
What are the RISK GROUPS associated for NSAID induced ulcers?
|
- Age > 65yrs
- history of recent peptic ulcer or previous GI bleed - coexisting significant disease (CV, hepatic, renal impairment) - concomitant therapy w corticosteroids, anticoagulants, or ASA (incl. low dose for prophylaxis) |
|
|
What are the risk groups for NEPHROTOXICITY for NSAID use?
|
- age > 65 yrs
- previous renal insufficiency - HTN - hepatic cirrhosis - CHF - AHD - Concurrent diuretic or ACEI - protracted dehydration |
|
|
NSAIDS should be avoided when?
|
- if patient is allergic to ASA
- severe history of asthma - third trimester - pts on lithium, anticoagulants, digoxin - recent peptic ulcer - past history of GI bleed - bleeding dyscrasia or anticoagulants - history of asthma - kidney disease - elderly (esp >75) - HTN, cardiac disease |
|
|
What are the CNS adverse effects of NSAID use?
|
- HA
- tinnitus - dizziness |
|
|
What are the CV adverse effects of NSAIDs?
|
- fluid retention
- HTN - edema - rarely CHF |
|
|
What are the GI adverse effects of NSAIDs?
|
- abdominal pain
|
|
|
What are the hemotologic adverse effects of NSAIDs?
|
- rare thrombocytopenia
- neutropenia - aplastic anemia |
|
|
What are the HEPATIC adverse effects of NSAID use?
|
- abnormal LFt's
- rare liver failure |
|
|
What are the PULMONARY adverse effects of NSAID?
|
- asthma
|
|
|
What are the RENAL adverse effects of NSAID?
|
- renal insufficiency
- renal failure - hyperkalemia - proteinuria |
|
|
Write out a prescription for TYLENOL:
|
Rx: Tylenol 325 mg
Disp: Twenty Sig: 1-2 tablets q4-6h prn pain |
|
|
Write out an IBUPROFEN Rx:
|
Rx: Ibuprofen 400mg (600mg)
Disp: twenty Sig: 1 tab q4-6h prn pain |
|
|
Write out a NAPROXEN Rx:
|
Rx: Naprosyn 250mg (500mg)
Disp: 20 (Twenty) Sig: 1 tablet tid (bid) prn pain |
|
|
Write out Tylenol #2 prescription:
|
Rx: Tylenol #2 (300mg Acetominophen/15mg Codeine)
Disp: 20 (Twenty) Sig: 1-2 tablets q4-6h prn pain |
|
|
Write out TYLENOL #3 prescription:
|
Rx: Tylenol #3 (300mg Acetominophen/30mg Codeine)
Disp: 20 (Twenty) Sig: 1 tablet q4-6h prn pain |
|
|
Write out a PERCOCET prescription:
|
Rx: Percocet (5mg Oxycodone/325mg Acetominophen)
Disp: 20 (Twenty) Sig: 1-2 tablets q4-6h prn pain |
|
|
Write out a DILAUDID prescription?
|
Rx: Dilaudid 1mg (2mg)
Disp: 20 (Twenty) Sig: 1-2 tablets q4-6h prn pain |
|
|
What are Peterson's 5 principles of antibiotic prophylaxis?
|
1. Surgical procedure should have a significant risk of infection
2. the correct antibiotic for the surgical procedure should be selected 3. antiobiotic level should be high 4. the timing of the antibiotic administration must be correct 5. the shortest antibiotic exposure must be used |
|
|
What are the classifications of WOUNDS?
|
- clean
- clean/ contaminated - contaminated - dirty |
|
|
What are some factors that contribute to the risk of surgical site infection?
|
- co-morbid conditions
- age - quality of tissue at the surgical site - skill of the surgeon |
|
|
What is the infection rate of a CLASS I wound?
|
(CLASS I = clean wound)
<1-2 % without pre-op Abx |
|
|
What are the characteristics of a CLASS I wound?
|
(CLASS I = clean wound)
- atraumatic - without inflammation - without break in asepsis - closed PRIMARILY |
|
|
What are the characteristics of a CLASS 2 wound?
|
(Clean contaminated = Class 2)
- mucosal barrier is crossed or communication with the oral cavity - eg. orthognathic surgery, implants, bone grafting, non-infected - prophylactic Abx may be of benefit |
|
|
What is the infection rate of a CLASS II wound?
|
Clean contaminated = Class 2
Infection rate 10-15% |
|
|
What is the infection rate of CLASS 3 wound?
|
- 20-30% w/o Abx
(Contaminated wound = Class 3) |
|
|
What are the characteristics of CLASS 3 wounds?
|
Contaminated
- traumatic injury involving oral mucosa - usually managed with only pre-op Abx unless other risk factors present |
|
|
What are the characteristics of Class 4 wound?
|
- actively infected OR
- result of trauma in which there has been a delay in tx and there is communication with the oral cavity and the possible presence of devitalized tissue or foreign bodies - may have 50% rate of infection and are often managed with pre- and post-op Abx |
|
|
A patient of yours is undergoing Implant surgery. What are the chances that they will have an infection if you don't prescribe prophylactic Abx?
|
10-15%
|
|
|
A patient of yours is undergoing Orthognathic surgery. What are the chances that they will have an infection if you don't prescribe prophylactic Abx?
|
10-15%
|
|
|
Oral antitiobics should be given how soon before/after surgery?
|
ORAL abx 60min BEFORE
PARENTERAL abx 30 min BEFORE |
|
|
Majority of infective endocarditis cases are caused by what bacteria?
|
Streptococci
Staphylococci |
|
|
What are some factors that affect microbial flora?
|
- host immune system
- anatomic region - relative humidity - presence or lack of oxygen - local surface characteristics - available nutrition - interaction between the microbes |
|
|
What are the indications for OPEN EXTRACTION?
|
- need for excessive force
- excessive bone loss - fracture of tooth and root - initial attempts at forceps have failed - patient with short clinical crowns - radiographic examination |
|
|
Why can patients with short clinical crowns due to attrition / bruxism be an indication for OPEN EXTRACTION?
|
- usually surrounded by dense bone with strong PDL attachments
|
|
|
What are some RADIOGRAPHIC indicators for OPEN EXTRACTION?
|
- hypercementosis of roots
- bulbous apices - divergent / dilacerated - dense bone - pneumatization - caries - restorations |
|
|
What are the steps for trying to remove a root fragment?
|
- Irrigation - suction technique first
- THEN tease root apex with root tip pick - THEN small straight elevator wedged in PDL |
|
|
What are some possible justifications for leaving root fragments?
|
1) 4-5mm
2) deeply imbedded - not superficial 3) without infection - risk of surgery GREATER than benefit - endangering important structures - potential displacement into unwanted spaces |
|
|
What must you do if you choose to leave a root tip in?
|
- inform the patient
- radiographic evidence - follow-up - advised to return if symptoms arise in the area of fragment / tip |
|
|
What are some indications for REMOVAL OF IMPACTED TEETH?
|
- prevention of periodontal disease
- prevention of caries - prevention of pericoronitis - prevention of root resorption - impacted teeth under prosthesis - pain of unexplained origin - prevention of jaw fractures - facilitation of orthodontic treatment - prevention of cysts / tumours |
|
|
What are some CONTRA-indications for removal of impacted teeth?
|
1) Extremes of age (young and old)
- retained in alveolar process for years - without perio disease, caries, cystic degeneration, etc - radiographically detected layer of overlying bone - check tooth radiographically every 1-2 yrs 2) cmopromised medical status 3) excessive damage to adjacent structures |
|
|
What is the MOST COMMON impaction of third molars?
|
Mesioangular
|
|
|
What is the EASIEST third molar impaction to remove?
|
Mesioangular
|
|
|
What is the MOST DIFFICULT third molar impaction to extract?
|
DISTOANGULAR > Vertical > horiz > mesio
|
|
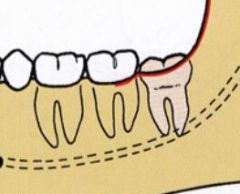
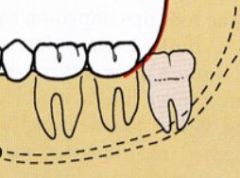
What kind of classification of third molar impaction is this?
|
Pell and Gregory CLASS 1
|
|
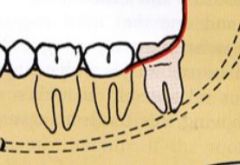
What kind of classification of third molar impaction is this?
|
Pell and Gregory CLASS 2
- Approx half is covered by anterior portion of ramus of mandible |
|
What kind of classification of third molar impaction is this?
|
Pell and Gregory CLASS 3
- completely embedded in bone of ramus |
|
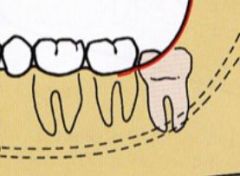
What Class is this?
|
Pell and Gregory CLASS A
- occlusal plane is at same level as occlusal plane of 2nd molar |
|
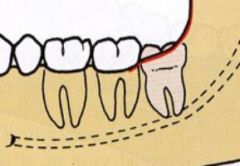
What Class is this?
|
Pell and Gregory CLASS B
- occlusal plane of impacted tooth between occlusal plane and cervical line of 2nd molar |
|

What class of impaction is this?
|
Pell and Gregory Class B
- occlusal plane of tooth is below cervical line of 2nd molar |
|
|
What are some factors that make IMPACTION SURGERY LESS DIFFICULT?
|
- mesioangular position
- Class 1 ramus - Class A depth - Roots one third to two thirds formed - Fused conical roots - Wide PDL - Large follicle - elastic bone - separated from 2nd molar - separated from inferior alveolar nerve - soft tissue impact |
|
|
Which "FAACTORS THAT MAKE IMPACTION LESS DIFFICULT" are usually present in young patients?
|
- roots one third to two thirds formed
- large follicle - wide PDL - elastic bone - separated from IAN |
|
|
What are the factors that make impaction surgery MORE DIFFICULT?
|
- distoangular
- class 3 ramus - class C depth - long, thin roots - divergent curved roots - narrow PDL - thin follicle - dense, inelastic bone - contact with second molar - close to IAN - complete bony impaction |
|
|
Which "FACTORS THAT MAKE IMPACTION SURGERY MORE DIFFICULT" are usually present in older patients?
|
- long, thin roots
- thin follicle - dense, inelastic bone - complete bony impaction |
|
|
What are the goals of physical and psychological evaluation of the patient?
|
1) determine patient's physical and psychological ability to tolerate the planned dental treatment
2) are there treatment modifications needed to enable the patient to better tolerate the stresses of the dental treatment? 3) is psychosedation indicated? 4) to determine which technique of sedation is most appropriate for the patient |
|
|
What does the "minimum physical exam" for all potential patients consist of?
|
- vital signs
- visual inspection |
|
|
What information is gathered for VITAL SIGNS?
|
- blood pressure
- heart rate / rhythm - respiratory rate - temperature - height - weight |
|
|
What things are examined as part of VISUAL INSPECTION?
|
- posture
- body movement - speech - skin |
|
|
What are the different ASA classifications?
|
CLASS 1
- healthy patient CLASS 2 - mild systemic disease without limitation of daily activities CLASS 3 - pt with severe systemic disease that limits activity but is not incapacitating CLASS 4 - incapacitating systemic disease which is a constant threat to life CLASS 5 - moribund pt not expected to survive 24hrs with or without the operation CLASS 6 - brain dead - organ donation |
|
|
What are some things that constitute ASA 2?
|
- healthy pregnant female
- healthy >60yrs - healthy but extreme phobia - Atopic pt - HTN - Non-Insulin DDiabetes (Type 2) - WELL CONTROLLED: epilepsy, asthma, thyroid condition |
|
|
What are some things that constitute ASA 3?
|
- Well controlled INSULIN DDiabetes
- Symptomatic thyroid diagnosis - MI > 6 months ago wtih no residual complications - CVA > 6 months ago with no residual complications - 160-199 / 95-115 - less well-controlled epilepsy - more severe asthma - stable angina - HF - orthopnea, ankle edema - COPD |
|
|
What are some things that constitute ASA 4?
|
- unstable angina
- MI < 6 months ago - CVA < 6 months ago - 200/115 - uncontrolled dysrhythmias - severe HF or COPD - uncontrolled epilepsy or IDDM - |
|
|
What are some STRESS-REDUCTION PROTOCOLS?
|
- recognition of medical risk/med consult prn before treatment
- recognition of anxiety - premedication - morning appointment - minimization of office waiting time - psychosedation during treatment - adequate pain control during tx - length of appt - post-op pain and anxiety control |
|
|
What are some imporatnt questions to ask about in the HEALTH QUESTIONNAIRE?
|
- general health, hospitalizations, physicals
- pain? - chest pain? - swelling of ankles? SOB? - recent weight loss? fever? nightsweats? - cough? blood? - bleeding problems? - sinus problems? - nausea, vomiting, diarrhea - dizziness? headaches? fainting? blurred vision? - seizures? - heart disease? attacks? murmurs? stroke? HTN? RF? - asthma? tb? COPD? - hepatitis? - arthritis? - allergies? - anemia - kidney? thyroid? adrenal? - psych care? - prosthetic heart vales? joints? - drugs? alcohol? tobacco? - pregnancy? |
|
|
What is the goal of SEDATIVE use?
|
- achieve LIGHT level of sedation that lessens anxiety and stress, and makes LA more effective
|
|
|
What are the importants things that must be maintained in regards to the patient during psychosedation?
|
- should remain awake
- cooperative - entirely responsive to direction - no RESP or CV depression |
|
|
What are the characteristics of an ideal sedative agent?
|
- ameliorate a transient anxiety state without depression of vital functions
- wide safety range - should be effective after single doses - rapid uptake and absorption (rapid onset) - adequate duration with rapid recovery - relaxation of skeletal muscles is desireable, but not mandatory - minimal toxicity and side effects - anti-emetic properties are desireable - inexpensive - suitably long-shelf life - not habituating or addicting - should potentiate the desired effects of a concomitantly used agent without significant depressive effects |
|
|
TRUE or FALSE: Objective of sedation is to decrease the pain threshold.
|
FALSE; want to ELEVATE the threshold
|
|
|
What are some specific situations where sedation may be helpful?
|
- control excessive secretions from salivary glands
- help control gagging - help control motor disturbances - relaxation |
|
|
What are the important FACTORS that will modfiy the dosing of sedatives?
|
1) PAIN THRESHOLD: varies depending on:
- emotional state - degree of fatigue - age - sex - past experience - pain 2) WEIGHT 3) AGE - special attention to young and elderly 4) PRESENCE OF PATHOLOGIC CONDITION: - liver, kidney, hypothyroidism, Addison's, COPD, etc 5) CONCOMITANT MEDS 6) ABSORPTION FROM GI TRACT |
|
|
How are CHILDREN different than adults? (re: drug use)
|
- increase C.O to vessel-rich group
- decreased redistribution due to decreased muscle and fat - decreased binding to plasma protein - increased BMR and increased BBB penetrance |
|
|
What is CLARK'S RULE?
|
PEDIATRIC DOSE = [weight of child (lb) / 150] x adult dose
|
|
|
What is YOUNG's RULE?
|
PEDIATRIC DOSE = [Age of child (yr) / age + 12 ] x adult dose
|
|
|
How do ELDERLY differ from adults in terms of drug use?
|
- decreased GI absorption
- alteration in number and character of receptor sites - change in body fat; decrease in total body water - decrease in plasma albumin - decreased liver biotransformation and renal excretion rates |
|
|
What are the different routes of ADMINISTRATION FOR SEDATIVE DRUGS?
|
- inhalational
- oral + sublingual - rectal - subcutaenous - IM , intralingual - IV |
|
|
What is the MOST CONVENIENT / ECONOMIC route of administration of sedative?
|
ORAL and sublingual
|
|
|
What are the advantages of IV sedation?
|
1) RAPID ONSET: Arm -> Brain 30sec
2) TITRATION 3) PATENT VEIN W IV ACCESS 4) DEPTH OF SEDATION 5) RECOVERY TIME SHORTER |
|
|
What are the disadvantages of IV SEDATION>?
|
1) VENIPUNCTURE REQUIRED with possible complications
2) INABILITY TO REVERSE ACTION OF SOME DRUGS 3) RAPID ONSET OF ACTION - need rapid recognition and tx 4) MONITORING 5) SPECIALIZED TRAINING 6) NPO, ESCORT, POST-OP LIMITATIONS |
|
|
What are some common VENIPUNCTURE sites?
|
- cephalic vein
- basilic vein - median cubital vein - dorsal venous arch |
|
|
What are some general PRE-SEDATION guidelines?
|
- NPO 6 hrs pre-op OR
- light meal if nitrous only - escort - sedation depth is patient-med-dose-dependent |
|
|
What are some POST-SEDATION guidelines?
|
- sit patient up slowly
- walk with escort - restful day at home (with escort) - verbal and written instructions |
|
|
What are some importants SEDATION RECORDS to make?
|
1) VITAL SIGNS - pre/ intra/ post-op. Ideally EVERY 5 MIN during procedure. Sp02, BP, HR, RR, ECG
2) Meds, dose + time of admin 3) Responsiveness 4) Recovery adequate for discharge recorded |
|
|
List some ORAL SEDATIVE AGENTS:
|
- Diazepam
- Lorazepam - Triazolam - Midazolam - Diphenhydramine - Chloral hydrate - NON-BZD's - anxiolytics/hypnotics - BA |
|
|
What doseages does DIAZEPAM come in?
|
2, 5, 10mg pills
|
|
|
What is the half-life of DIAZEPAM?
|
20-70 hours
|
|
|
What are some contraindications to DIAZEPAM use?
|
- MG
- allergy - pregnancy - acute narrow angle glaucoma |
|
|
What are your instructions for DIAZEPAM use if prescribed?
|
Rx. Diazepam 2-10mg PO
Mitte: i night before, i morning of procedure |
|
|
What dosing would you give for LORAZEPAM?
|
2-4 mg
1 hour prior to appointment |
|
|
What is the half life of LORAZEPAM?
|
9-16 hours
|
|
|
Peak levels with LORAZEPAM USE would be reached in how much time?
|
2 hours
|
|
|
Peak plasma levels would be reached how long after oral use of TRIAZOLAM?
|
60-90 min
|
|
|
What is the half-life of TRIAZOLAM?
|
1.5 - 5.5 hours
|
|
|
What is the standard dosing of TRIAZOLAM in adults?
|
0.125 - 0.5mg
|
|
|
Which anxiolytic can be used safely in pediatrics?
|
MIDAZOLAM 0.3-0.6mg/kg PO 1hour prior to procedure
|
|
|
What is the ADULT dosing for MIDAZOLAM?
|
7.5 - 15 mg
|
|
|
What are Petersons 5 principles of antibiotic prophylaxis.
|
fgh
|
|
|
Define ANALGESIC:
|
drug capable of reducing or eliminating pain on systemic administration
|
|
|
What is the difference b/w NARCOTICS vs NON-NARCOTICS?
|
- Mechanism of action
- relative efficacy against severe pain - presence of anti-inflammatory effects - relative incidence and types of adverse effects - drug dependence / abuse liability |
|
|
What are the three actions of NARCOTICS?
|
- elevation of pain threshold
- modifying the reaction to pain - induction of lethargy and sleep |
|
|
What is the MECHANISM OF ACTION of narcotics?
|
- centrally via opioid receptors
- some peripheral analgesic effects - usually act at Mu receptors - all opioid receptors have analgesic effects |
|
|
What effects happen when MU receptors are activated?
|
- respiratory depression
- euphoria - addictive potential |
|
|
What effects happen when KAPPA receptors are activated?
|
- mioisis
- sedation - dysphoria - psychomimetic effects |
|
|
What effects do DELTA RECEPTORS have when activated?
|
- behavioural
- epileptogenic |
|
|
What does opiate-receptor activation do on the synaptic level?
|
INHIBITS pre-synaptic release and post-synaptic response to excitatory neurotransmitters
|
|
|
Where are OPIOID RECEPTORS primarily located in?
|
- substantia gelatinosa
- trigeminal nucleus - brainstem solitary nucleus and area postrema - infundibulum of hypothalamus - medial thalamus - limbic system ****** HIGHEST CONCENTRATION ***** - Periaqueductal grey matter (PAG) of mesencephalon |
|
|
Which areas that control emotions can have an effect on pain perception?
|
- medial thalamus
- limbic system |
|
|
What are ENDORPHINS?
|
- endogenous opiates
|
|
|
What are the three classes of NARCOTIC ANALGESICS?
|
NATURAL: Morphine, codeine, heroin
SEMI-SYNTHETIC: modifications of morphine: Oxycodone, hydromorphone SYNTHETIC: meperidine, fentanyl, methadone, propoxyphene |
|
|
TRUE or FALSE: There is a ceiling doseage for narcotics?
|
FALSE: no ceiling dose
|
|
|
Define CEILING DOSE:
|
In pharmacology, the term ceiling effect refers to the property of increasing doses of a given medication to have progressively smaller incremental effect (an example of diminishing returns). Mixed agonist-antagonist opioids, such as nalbuphine, serve as a classic example of the ceiling effect; increasing the dose of a narcotic frequently leads to smaller and smaller gains in relief of pain. In many cases, the severity of side effects from a medication increases as the dose increases, long after its therapeutic ceiling has been reached.
|
|
|
TRUE or FALSE: Respiratory depressant effects may last longer than adequate analgesic effects.
|
TRUE
|
|
|
What are all the effects of MORPHINE?
|
- analgesic
- sedative - anti-tussive - constipative - histamine-releasing - miotic - convulsive - respiratory depressant effects (directly depresses the responsiveness of the medullary respiratory centres to CO2 as well as the pontine and medullary centres responsible for resp. rhythm) |
|
|
What are ABSOLUTE CONTRAINDICATIONS to morphine use?
|
Allergy
|
|
|
What are the RELATIVE contraindications for MORPHINE?
|
- head injury
- pts with convulsive disorders - hypotension, asthma, hypothyroidism, Addison's dz, severe renal or hepatic, COPD |
|
|
With MORPHINE use tolerance develops to WHICH effects / and to which does it not develop?
|
TOLERANCE:
- analgesic - euphoric - resp - hypotensive - emetic NO TOLERANCE: - miosis - constipation - bradycardia |
|
|
What is the doseage for MORPHINE?
|
5-10mg IV
(not as effective orally due to poor absorption) 10mg MORPHINE IV = 60mg MORPHINE PO |
|
|
Which NARCOTICS are pure MU agonists?
|
- Morphine
- Meperidine - Codeine - Hydromorphone - Fentanyl |
|
|
What is the potency of MEPERIDINE?
|
1/10 as potent as morphine
less constipating less anti-tussive |
|
|
What are the effects of MEPERIDINE?
|
- less constipating
- less anti-tussive - minimal oral bioavailability - decreases seizure threshold |
|
|
What is the potency of CODEINE?
|
1/12 of MORPHINE
|
|
|
What enzyme converts CODEINE into ACTIVE ANALGESIC METABOLITES?
|
Cytochrome CYP2D6
|
|
|
What is the ANTITUSSIVE DOSE of CODEINE is?
|
15-20mg
|
|
|
What is the PO ANALGESIC DOSE of CODEINE?
|
30-60mg
|
|
|
Which NARCOTIC is both a MU and milk KAPPA agonist?
|
OXYCODONE
|
|
|
Which drugs have oxycodone in them?
|
PERCOCET
PERCODAN |
|
|
What is the usual HYDROMORPHONE dose PO?
|
1-2 mg
q4-6h |
|
|
Which two narcotics are very structurally similar?
|
FENTANYL + MEPERIDINE
|
|
|
Which narcotic is most commonly used for IV SEDATION and GEN. ANAESTHESIA?
|
FENTANYL
|
|
|
What are the MIXED AGONIST/ANTAGONIST narcotics?
|
- Pentazocine
- Nalbuphine - Butorphanol |
|
|
What is TRAMADOL?
|
- centrally acting analgesic
|
|
|
What is the dosing of TRAMADOL?
|
50-100mg QID
|
|
|
What is the contraindication for TRAMADOL?
|
Pts with seizure / epilepsy history
|
|
|
What is a narcotic antagonist?
|
NALOXONE
|
|
|
What is the PRIMARY THERAPEUTIC INDICATION for use of NALOXONE?
|
Narcotic-induced respiratory depression
- reverses euphoric, analgesic, sedative, miotic, and GI effects |
|
|
What is the dosing of NALOXONE?
|
ADULT: 0.4mg IV, IM, SC
CHILDREN: 0.01mg/kg REPEAT q2-3min If no response after 10mg = DD for resp. depression **short duration of action** |
|
|
What are the common properties of ALL NSAIDs?
|
- analgesic
- anti-inflammatory - anti-pyretic |
|
|
Why may NSAIDs be less useful for severe pain?
|
NSAIDs have a ceiling dose
|
|
|
What is the life of a platelet?
|
5-9 days
|
|
|
Acetyl Salicylic Acid (ASA) is longer lasting of the NSAIDs why?
|
Irreversibly damages COX1 for life of the platelet
|
|
|
What are the benefits of COX2 inhibitors?
|
- reduce risk of serious GI adverse effects (such as gastric ulceration/bleeding)
- spare platelet function - share the same potential as NSAIDs for renal toxicity - increased incidence of CV thrombotic events (edema, HTN) |
|
|
Risk groups for NSAID induced ulcers:
|
- age > 65 years
- history of recent peptic ulcer disease or previous GI bleed - coexisting significant disease (CV, hepatic or renal impairment) - concomitant therapy w/ corticosteroids, anticoagulants, or ASA |
|
|
When should NSAIDs be avoided?
|
- allergic to ASA
- history of severe asthma - third trimester - pts on lithium, anticoagulants, antineoplastic doses of methotrexate, digoxin, renal disease |
|
|
What is your choice of prescription for MILD TO MODERATE PAIN?
|
- full therapeutic dose of ibuprofen or tylenol if NSAID is contraindicated
- OR - Tylenol #3 with 325mg acetaminophen ================================ Rx: 400-600mg q4-6h DO NOT EXCEED 2400mg ================================ |
|
|
Primary biotransformation of ACETAMINOPHEN?
|
In liver
|
|
|
What is the usual dose of ACETAMINOPHEN?
|
- 325-1000mg q4-6h
(1/2 life 2-3 hours) |
|
|
Healthy patients should not exceed how much acetaminophen per day?
|
4g per day
|
|
|
Which NSAID has the longest half life?
|
NAPROXEN (14 hours)
|
|
|
What factors will affect your choice in choosing an effective analgesic?
|
- expected pain (mild/mod/severe)
- psychology of the patient - has pt tried narcotics / nsaids for pain? What was dose? Effect? Side effects? - MOST CASES DENTAL/OS PAIN RESPONDS WELL TO NSAID |
|
|
What is the general rule of thumb for combining NSAID with narcotic?
|
- Narcotic given IN ADDITION to NSAID
- Use narcotic that is well-absorbed orally (Oxycodone / Dilaudid) |
|
|
What are some ADVERSE EFFECTS of NSAIDs?
|
CNS: HA, tinnitus, dizziness
CV: fluid retention, HTN, edema, rarely CHF GI: abdominal pain Heme: Rare thrombocytopenia, neutropenia, aplastic anemia HEPATIC: abnormal LFTs, rare liver failure PULP: Asthma RASHES: all types, pruritis RENAL: renal insufficiency, renal failure, hyperkalemia, proteinuria |
|
|
Write a prescription for TYLENOL:
|
Rx: Tylenol 325mg
Disp: 20 (Twnty) Sig: 1-2 tablets q4-6h prn pain |
|
|
Write out a prescription for NAPROXEN:
|
Rx: Naprosyn 250mg (500mg)
Disp: 20 (Twenty) Sig: 1 tablet TID prn pain |
|
|
Write a prescription for TYLENOL #2:
|
Rx: Tylenol #2 (300mg Acetaminophen / 15mg Codeine)
Disp: 20 (Twenty) Sig: 1-2 tablets q4-6h prn pain |
|
|
Write out a prescription for TYLENOL #3:
|
Rx: Tylenol #3 (300mg Acetaminophen / 30 mg Codeine)
Disp: 20 (twenty) Sig: 1 tablet q4-6h prn pain |
|
|
Write out a prescription for PERCOCET:
|
Rx: PERCOCET (5mg oxycodone / 325mg acetaminophen)
Disp: 20 Sig: 1-2 tablets q4-6h prn pain |
|
|
Write out a prescription for DILAUDID:
|
Rx: DILAUDID 1mg
Disp 20 Sig: 1-2 tablets q4-6h prn pain |
|
|
What does "prn" stand for?
|
Pro re nata
"as and when necessary" |
|
|
The majority of post-operative hemorrhage (>90%) results from what causes?
|
- excessive operator trauma
- poor compliance with post-op instructions - interference with extraction socket or pocket site (sucking, tongue pushing) - inflammation at extraction/op site - inappropriate use of analgesia with aspirin or other NSAID |
|
|
How does WARFARIN work?
|
- Binds to enzyme VitK2,3 epoxide reductaste
- antagonizes vit-K dependent synthesis of Fac II, VII, IX, X PT and aPTT time are prolonged |
|
|
What is the timing of warfarin effects?
|
- delayed for 8-12 hours
- maximal @ 36hours - persist for 72 hours HALF LIFE = 37 hours |
|
|
WARFARIN is metabolized primarily where?
|
LIVER
|
|
|
The effect of WARFARIN is reversible or irreversible?
|
Reversible with Vit K
|
|
|
What is the usual therapeutic range for deep vein thrombosis?
|
2-3 INR
|
|
|
Patients on warfarin:
Should be referred to hospital in which situations? |
INR > 3.5
Need of more than simple surgical procedure Presence of additional bleeding risk factors or logistic difficulties |
|
|
If surgery on WARFARIN patient performed in office, what materials should be used?
|
- absorbable packing hemostatic agents
- sutures - hemostatic mouthwashes |
|
|
Which drugs can ENHANCE warfarin effect?
|
ANTIBACTERIALS
- if infection present, no elective surgery should be done until patient has been treated with Abx and is free from acute infection ANTIFUNGALS - treatments with azoles ANTIVIRALS - |
|
|
What are the guidelines for WARFARIN THERAPY prior to/ during / after surgery?
|
DAY 1: Obtain baseline INR
Warfarin 10mg dose on night of surgery. Alternatively, can use patients known usual maintenance dose. DAY 2: Check INR (reflects first dose ONLY) If INR < 1.5 give same dose If INR > 1.5, give lower dose DAY 3: Check INR (reflects first 2 doses) If INR < 1.5 - higher than avg maintenance dose If INR 1.5-2.0 - average maintenance dose (approx 5mg) needed If INR > 2.0 lower dose needed |
|
|
Most NSAID induced inhibition of thromboxane synthesis leads to a decrease in platelet aggregation, how long does it take for this effect to reverse?
|
24 hours
|
|
|
What is the reversal agent for heparin?
|
Protamine sulfate
|
|
|
What is the reversal agent for WARFARIN?
|
Vit K?
|
|
|
What is the reversal agent for acetaminophen?
|
N-acetyl-cysteine
|
|
|
Which drug should one be careful if alcohol is used?
|
ACETAMINOPHEN
|
|
|
What are the factors that affect microbial flora?
|
- host immune system
- anatomic region - relative humidity - presence / lack of oxygen - local surface characteristics - available nutrition - interaction between microbes |
|
|
What is the environment of the SKIN like?
|
- mildly acidic pH
- desquamates - inhospitable -types and number relatively constant |
|
|
What is the ORAL environment like?
|
- warm, constant temp
- wet / dark - aerobic and anaerobic - constant source of nutrition - newbourn mouth initially aerobic - mostly Strep. |
|
|
What are some environmental agents that can alter microflora?
|
- alcohol
- tobacco smoke - medications - radiation therapy - caries - periodontitis |
|
|
What are some of the most common INDIGENOUS NASAL / PARANASAL sinus flora?
|
- Haemophilus influenzae
- Moraxella species - Strep pneumoniae |
|
|
What is the ratio of ANAEROBES:AEROBES in odontogenic infections?
|
2:1
most frequently Alpha-hemolytic STREPTOCOCCI |
|
|
Bites from humans most commonly involve what organisms?
|
- streptococcus viridans
- bacteroides - peprostrep - enterococcus corrodens |
|
|
Bites from animals usually involves which bacteria?
|
- staph aureus
- strep viridans - bacteroides - |
|
|
Which are BACTERICIDAL antibiotics?
|
B-lactams (penicillins, cephalo, carbapenams, mono)
Aminoglycosides Vancomycin Metronidazole Fluoroquin |
|
|
What are BACTERIOSTATIC antibiotics?
|
Macrolides
Clindamycin Tetracycline Sulfa abx |
|
|
Which are the CONCENTRATION dependent anti-biotics?
|
FLUOROQUINOLONEs
AMINOGLYCOSIDES |
|
|
What are the TIME-DEPENDENT ANTIBIOTICS?
|
dag
|
|
|
Which antibiotics should be avoided in children less than 8 years?
|
- tetracyclines
- fluoroquinolones - carbapenams |
|
|
Which antibiotics are the WORST for pregnancy?
|
AMINOGLYCOSIDES
TETRACYCLINES DOXYCYCLINE |

