![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
111 Cards in this Set
- Front
- Back
|
immune response to a foreign substance, based on the specific memory of a past exposure to that same foreign substance; the second, acquired immune response is quicker than the initial response |
acquired immune response |
|
|
any substance able to induce a specific immune response |
antigen |
|
|
a disease where parts of an individual's own body become antigens |
autoimmune disease |
|
|
What is another word for antigen? |
immunogen |
|
|
when the body no longer recognizes certain antigens as foreign |
immunodeficiency |
|
|
the body overreacts to what it sees as foreign, creating a multitude of complications |
hypersensitivity |
|
|
chemical mediators produced by cells involved in the immune response |
cytokines |
|
|
What are the primary white blood cells involved in the immune response? |
lymphocytes
*mobile antigen-sensitive cells with a long life* |
|
|
What are the three main types of lymphocytes? |
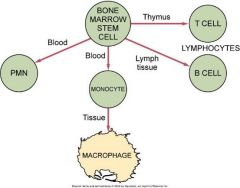
|
|
|
Type of lymphocyte that develops in lymphoid tissue other than the thymus, and that can later develop into a plasma cell that produces antibody, the main initiator of humoral immunity |
B-Cell Lymphocyte |
|
|
Tissue composed of lymphocytes supported by a meshwork of connective tissue; includes tonsillar tissue, lymph nodes, and lymphatic organs |
lymphoid tissue |
|
|
What are the two main types of B cells that develop when stimulated by an antigen? |
|
|
|
cell that retains a memory of the antigen |
B-Memory Cell; duplicates itself in the presence of an antigen |
|
|
cell derived from B-cell lymphocytes that produces antibodies in response to the presence of antigen |
plasma cell |
|
|
protein molecule, an immunoglobulin, that is secreted by plasma cells and reacts with a specific antigen |
antibody |
|
|
What are the five classes of antibodies? |
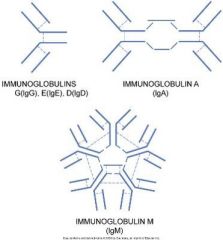
|
|
|
proteins that, when secreted by the plasma cells, serve as antibodies designed to respond to a specific antigen; remain attached to the surface of certain B cells and function as receptors |
immunoglobulins |
|
|
level of a specific antibody in the blood |
antibody titer |
|
|
IgA |
defense against proliferation of microorganisms in body fluids |
|
|
IgD |
activates the B-lyphocytes |
|
|
IgE |
hypersensitivity / allergic reactions |
|
|
IgG |
major antibody in blood serum and can pass the placental barrier |
|
|
IgM |
early immune response; activates complement |
|
|
combination of an antibody and antigen, producing a complex that can initiate a hypersensitivity reaction |
immune complex |
|
|
The formation of an immune complex usually renders the antigen _______. |
inactive |
|
|
organ consisting of lymphoid tissue located high in the chest, which is large in an infant and gradually shrinks in size in adulthood; site of T-cell lymphocyte maturation |
thymus |
|
|
lymphocyte that matures in the thymus and is mainly responsible for initiating cell-mediated immunity, as well as also modulating humoral immunity |
T-Cell Lymphocyte |
|
|
How can the T cell be distinguished from other lymphocytes? |
T-Cell Receptor |
|
|
What are the types of T-Cell lymphocytes? |

|
|
|
this T-cell lymphocyte increases the functioning of the B-cell, enhancing the antibody response |
T-helper cell
CD4 |
|
|
this T-cell lymphocyte turns off function of B cells |
T-suppressor cell
CD8 |
|
|
this T-cell lymphocyte is active in surveillance against virally infected cells and neo-plastic cells, directly attacking these cells |
T-cytotoxic cell
CD8 |
|
|
type of lymphocyte that is part of the initial innate immune response, which by unknown mechanisms is able to directly destroy cells recognized as foreign |
natural killer cells |
|
|
large tissue-bound mononuclear phagocyte derived from monocytes circulating the blood, which can become mobile when stimulated by inflammation and interact with lymphocytes in an immune response |
macrophage
*phagocytosis and assist B and T cells* |
|
|
What white blood cell is the messenger between the inflammatory response and the immune response? |
Macrophage |
|
|
a type of white blood cell that acts as an antigen-presenting cell in the skin and mucosa; antigen-presenting cell |
Dendritic Cell |
|
|
What type of white blood cell is the messenger between innate immunity and acquired immunity? |
dendritic cell |
|
|
specialized dendritic cell, found in the skin and mucosa, that is involved in the immune response |
Langerhans Cell |
|
|
proteins produced by various cell types for the purpose of intercellular communication; immunological ones are involved in the immune response |
cytokines |
|
|
a substance that alters the immune response by augmenting or reducing the ability of the immune system to produce antibodies or sensitized cells that recognize and react with the antigen that initiated their production |
immunomodulator |
|
|
cytokines produced by B-cell or T-cell lymphocytes in contact with antigens; mediators of the immune response |
lymphokines |
|
|
cytokines produced by monocytes or macrophages; mediators in an immune response |
monokines |
|
|
What are the two major divisions of the immune response? |

|
|
|
type of immunity in which both B-Cell lymphocytes and the antibodies they produce as plasma cells play the predominant role; protection against bacteria and viruses |
Humoral Immunity |
|
|
type of immunity in which the major role is played by T-cell lymphocytes; regulates both major immune responses |
Cell-mediated immunity |
|
|
What are the types of immunity that can occur? |
|
|
|
type of immunity that uses antibodies produced by another person to protect an individual against infectious disease |
passive immunity |
|
|
occurs when antibodies from a mother pass through the placenta to the developing fetus |
natural passive immunity |
|
|
immunity by injecting a person with antibodies against microorganism to which the person has not previously been exposed |
acquired passive immunity
*short lived* |
|
|
type of immunity based on antibodies developed in response to an antigen |
active immunity |
|
|
type of immunity that occurs naturally when a pathogenic microorganism causes disease |
natural active immunity |
|
|
type of immunity that occurs by artificial means through immunization |
acquired active immunity |
|
|
induction of active immunity; when the pathogenic microorganism used to induce active immunity is encountered after vaccination, a stronger, faster immune response is produced, which prevents disease development |
immunization |
|
|
a repeated exposure by way of vaccination is called a... |
booster |
|
|
vaccines that consist of heat or chemical treated microorganisms or toxins; less effective |
killed-type vaccines |
|
|
vaccines that consist of genetically altered microorganisms that have lost virulence but still undergo limited replication |
live-attenuated vaccines |
|
|
to reduce the severity of a disease or the virulence of a pathogenic agent, as is done in the development of certain vaccines |
attenuate |
|
|
the study of diseases caused by the malfunctioning of the immune system |
immunopathology |
|
|
What are the three immunopathologic conditions ? |
|
|
|
group of signs and symptoms that occur together to define the disease state |
syndrome |
|
|
hypersensitivity acquired through exposure to a particular allergen that elicits an exaggerated reaction on reexposure to the same allergen |
allergy |
|
|
altered state of reactivity in which the body reacts to a foreign agent, or allergen, with an exaggerated immune response |
hypersensitivity |
|
|
What are the four types of hypersensitivity reactions? |
Type I: Anaphylactic (IgE) *Immediate* Type II: Cytotoxic (IgG &IgM) *Blood Transfusion* Type III: Immune Complex *Tissue Destruction* Type IV: Cell-Mediated *Tissue Damage; Transplant Rejections*
|
|
|
antigen producing a hypersensitivity, or allergic, reaction |
allergen |
|
|
severe, immediate type of hypersensitivity or allergy in which an exaggerated immunologic reaction occurs on reexposure to a foreign protein or other substance after sensitization, resulting in hives, itching, swelling, vascular collapse, and shock |
anaphylaxis |
|
|
the type of hypersensitivity in which there is a latent period between the antigen introduction and the reaction; cellular reactions are mediated by T lymphocytes; it can be used to test for TB and is responsible for rejection of tissue grafts and transplanted organs |
delayed hypersensitivity or Type IV |
|
|
a delayed allergic response after exposure to some antibiotics or antiserum; it is caused by an antibody reaction to an antigen in the donor serum |
serum sickness |
|
|
mucosal inflammation due to a disease process |
mucositis |
|
|
disease characterized by tissue trauma caused by an immune response against tissue constitutes of one's own body |
autoimmune disease |
|
|
diseases in which the body's recognition mechanism breaks down and certain body cells are no longer tolerated; the immune system treats body cells as antigens
another name for autoimmune disease |
connective tissue disease |
|
|
reduced immune response resulting from hypoactivity or decreased numbers of lymphoid cells |
immunodeficiency
*can be congenital or acquired* |
|
|
painful oral ulcer with an unclear cause; occur in 20% of population; trauma is most common factor; may be associated with certain systemic diseases; more common in women; have a immunologic pathogenesis; occur in 3 forms |
Aphthous Ulcer |
|
|
What are the 3 forms of aphthous ulcers? |
|
|
|
the most commonly occurring type of aphthous ulcer; it appears as a discrete, round-to-oval ulcer that is up to 1cm in diameter and exhibits a yellowish-white fibrin surface surrounded by a halo of erythema; occur mostly in anterior |

minor aphthous ulcer |
|
|
larger than 1 cm in diameter and are deeper and last longer than minor; can be more painful, often occur in the posterior; less common |

Major Aphthous Ulcer (Sutton Disease) |
|
|
tiny aphthous ulcers 1 to 2 mm that resemble ulcers caused by the herpes simplex virus; generally occur in groups |

Herpetiform Aphthous Ulcer |
|
|
How is the diagnosis of aphthous ulcers made? |
Clinically, not laboratory test are specific for any form of aphthous ulcer. |
|
|
What systemic diseases are linked to aphthous ulcers? |
|
|
|
What is the treatment for aphthous ulcers? |
|
|

|
Urticaria (Hives) |
|
|
pruritus |
itching |
|
|
a lesion that appears as a diffuse swelling of tissue caused by increased permeability of deeper blood vessels; the skin covering the swelling appears normal; usually not accompanied by itching |

angioedema
*antihistamine and epinephrine* |
|
|
lesions that result from the direct contact of an allergen with the oral mucosa and skin, respectively; involves T-cell mediated immune response; Type IV hypersensitivity |

Contact Mucositis and Contact Dermatitis
*topical and systemic corticosteroids* |
|
|
lesions that appear in the same site each time a drug is introduces; type III hypersensitivity |
fixed drug eruption |
|
|
an acute, self-limited disease that affects the skin and mucous membranes; the cause is not clear; common in young adults; men; bull's-eye lesion |

Erythema Multiforme
*remove cause or topical or systemic corticosteroids or antiviral medication* |
|
|
severe form of erythema multiforme |

Stevens-Johnson Syndrome |
|
|
a benign, chronic disease affecting the skin and oral mucosa; unknown cause, slender white lines "Whickham Striae" 1% of population; middle aged women |

Lichen Planus (diagnosed through clinical and microscopic means)
*topical corticosteroids; good home care, oral examination, discontinue drug use; biopsy* |
|
|
most common form of lichen planus; oral lesions composed of Wickham striae along with slightly raised white plaquelike areas that do not rub off |
reticular lichen planus |
|
|
forms of lichen planus in which the epithelium separates from the connective tissue, resulting in erosions, bullae, or ulcers; less common |

Erosive and Bullous Lichen Planus |
|

Associated with lichen planus |
Desquamative gingivitis |
|
|
a chronic disease that classically comprises the triad of three features
more in men and could be genetic |

Reactive Arthritis or Reiter Syndrome
*aspirin, antibiotics, and physical therapy*
HLA-B27 marker |
|
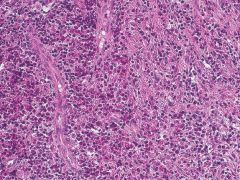
a group of rare disorders characterized by the presence of both Langerhans' cells and eosinophils |
Langerhans Cell Histiocytosis or Langerhans Cell Disease |
|
|
the acute disseminated form of Langerhans cell disease that usually affects children younger than 3 years of age; rapid; may respond to chemotherapy |
Letterer-Siwe Disease |
|
|
the chronic disseminated or multifocal form of Langerhans cell disease; occurs in children younger than 5 years of age; radiolucent areas in skull; diabetes; oral issues |
Hand-Schuller-Christian Disease |
|

|
Eosinophilic Granuloma of Bone
*surgical excision or radiation* |
|

an autoimmune disease that affects the salivary and lacrimal glands, resulting in a decrease in saliva and tears; xerostomia and parotid gland enlargement |
Sjogren Syndrome
Primary and Secondary (Alone and not alone Parotid gland enlargement in 50% of patients |
|
|
dry mouth and dry eyes |
sicca syndrome |
|
|
decreased salivary flow |
hyposalivation or xerostomia |
|
|
decreased lacrimal flow |
xerophthalmia |
|
|
damage to eyes |
keratoconjunctivitis sicca |
|

loss of filiform and fungiform papillae on dorsum of the tongue is associated with... |
Sjogren Syndrome
*biopsy of salivary glands* |
|
|
a disorder affecting the fingers and toes that goes with Sjogren syndrome |
Raynaud Syndrome |
|
|
an acute and chronic inflammatory autoimmune disease of unknown cause; affect women 8 times more frequently than men; more frequently in black women; periods of remission and exacerbation; autoantibodies to DNA are present; may be genetic |
Systemic Lupus Erythematosus |
|

|
Skin lesions occur n 85% of patients with Systemic Lupus Erythematosus Butterfly rash on bridge of nose |
|
|
a chronic, recurrent autoimmune disease consisting mainly of oral ulcer, genital ulcers, and ocular inflammation and skin lesions; no gender predilection; lifelong disorder with remissions and exacerbations |

Behcet Syndrome
*systemic and topical corticosteroids* |
|

a severe, progressive autoimmune disease that affects both the skin and mucous membranes; characterized by intraepitheial vesicle formation that results in the breakdown of the cellular adhesion between epithelial cells |
Pemphigus Vulgaris
no gender predeliction
Diagnosed by Biopsy
*high doses of corticosteroids and other immunosuppressive drugs* |
|
|
dissolution of the intercellular bridges of the prickle cell later of the epithelium |
acantholysis |
|
|
seen in some bullous diseases such as pemphigus vulgaris and bullous pemphigoid; the superficial epithelium separates easily from the basal layer on exertion of firm sliding manual pressure |
Nikolsky Sign |
|
|
detached rounded cells caused by a loss of attachment between epithelial cells |
Tzanck Cells |
|

a chronic autoimmune disease that affects the oral mucosa, conjunctiva, genital mucosa, and skin;not has severe as pemphigus vulgaris; cleavage of epithelial cells |
Mucous Membrane Pemphigoid
Diagnosed with Biopsy
*topical and systemic corticosteroids* |
|
|
an autoimmune disorder similar to mucous membrane pemphigoid; occurs in patients older than 60; oral lesions are less common; treated with systemic corticosteroids and nonsteroidal antiinflammatory drugs |
Bullous Pemphigoid |

