![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
158 Cards in this Set
- Front
- Back
|
the result of an alteration in the environment that causes tissue damage or necrosis |
injury |
|
|
What are the body's 3 responses to injury? |
|
|
|
the pathological death of one or more cells or a portion of tissue or an organ that results from irreversible damage to cells |
necrosis |
|
|
a nonspecific response to injury and occurs in the same manner, regardless o the nature of the injury |
inflammation |
|
|
The inflammatory response may be _______ and limited to the area of injury. |
Local |
|
|
The inflammatory response may become _______ if the injury is extensive. |
systemic |
|
|
Inflammation of a specific tissue is denoted by the suffix .... |
itis |
|
|
If the injury is minimal and brief and is source is removed from the tissue, it is considered _______, and the duration is short, lasting only a few days. |
acute |
|
|
If injury to the tissue continues and the inflammatory response is longer lasting, it is referred to as _______ _______. This may last weeks, month, or even indefinitely. |
chronic inflammation |
|
|
Redness Heat Swelling Pain Loss of Normal Tissue Function |
Local Clinical Changes
Classic Cardinal Signs of Inflammation |
|
|
small blood vessels, including arterioles, capillaries, and venules |
microcirculation |
|
|
Fever Leukocytosis Elevated C-Reactive Protein Lymphadenopathy |
Systemic Signs of Inflammation |
|
|
the fluid component of blood in which blood cells are suspended |
plasma |
|
|
an excess of blood within blood vessels in a part of the body |
hyperemia |
|
|
What is the sequence of Microscopic Events? |
|
|
|
What two clinical signs of inflammation is hyperemia responsible for? |
erythema and heat |
|
|
redness of the skin or mucosa |
erythema |
|
|
the fluid component of blood that normally passes through the endothelial cell walls of the microcirculation and supplies oxygen and nutrients |
transudate |
|
|
a process during inflammation in which white blood cells tend to move to the periphery of the blood vessel at the site of injury |
margination |
|
|
the adherence of white blood cells to blood vessel walls during inflammation |
pavementing |
|
|
the passage of white blood cells through the walls of small blood vessels and into injured tissue |
emigration |
|
|
fluid filed with a high protein content that leaves the microcirculation during an inflammatory response; consist of serum that contains white blood cells, fibrin, and other protein molecules |
exudate |
|
|
excess plasma or exudate in the interstitial space that results in swelling |

edema |
|
|
a secretion having a water consistency; relating to serum |
serous exudate |
|
|
a secretion containing or forming pus |
purulent exudate |
|
|
a collection of purulent exudate that has accumulated in a cavity formed by the tissue |

Abscess
|
|
|
an abnormal passage that leads from an abscess to the body surface |

fistula |
|
|
directed movement of WBCs toward the site of injury |
chemotaxis |
|
|
the process by which WBCs ingest and then digest foreign substances
may include pathogenic organisms and tissue debris |
phyagocytosis |
|
|
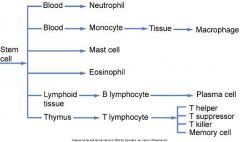
What two types of WBCs are initially involved in the inflammatory response? |
neutrophils (polymorphonuclear leukocytes) and monocytes (macrophages in tissue) |
|
|
What WBCs are seen in chronic inflammation and the immune response? |
lymphocytes and plasma cells |
|
|
When can eosinophils and mast cells be seen? |
in inflammation and the immune response |
|
|
Which WBCs are the most abundant during acute inflammation? |
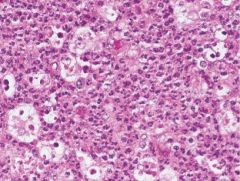
neutrophils |
|
|
Which WBCs are the most abundant during chronic inflammation? |
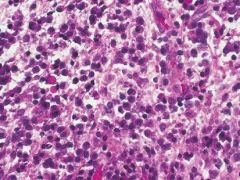
macrophages lymphocytes plasma cells |
|
|
What is the function of neutrophils? |
phagocytosis |
|
|
What WBC has a multilobed nucleus and granular cytoplasm that contains lysosomal enzymes? |
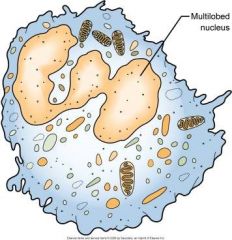
neutrophil |
|
|
What WBC constitutes 60% to 70% of WBC population? |
neutrophil |
|
|
Where are neutrophils derived from? |
bone marrow/stem cells |
|
|
an enzyme found in the granular cytoplasm of a neutrophil; destroy substances after the cell has engulfed them |
lysosomal enzyme |
|
|
Derivation of white blood cells from a stem cell in the bone marrow. |
|
|
What happens neutrophils after they complete phagocytosis? |
they die; this is important to know because after they die they release damaging cellular substances and can cause more tissue damage |
|
|
Which WBC has a single round nucleus and does not have granular cytoplasm? |

Macrophage |
|
|
Which WBC completes phagocytosis and plays a role in the immune system as its function. Constitutes 3% o 8% of WBC population and is derived from stem cells in bone marrow? |
Macrophages |
|
|
Never Let Monkeys Eat Bananas
(White Blood Cell Concentrations) |
Neutrophils (65%) Lymphocytes (25%) Monocytes (6%) Eosinophils (3%) Basophils (1%) |
|
|
What causes many of the events involved in the inflammatory response? |
biochemical mediators |
|
|
What are the three systems of plasma proteins circulating in the blood that may be activated during inflammation? |
(All are Interrelated) |
|
|
Which system is active in early phases of inflammation, activated by substances in plasma and injured tissue, induces pain, and causes dilation of blood vessels and permeability of local blood vessels? |
Kinin System |
|
|
What is the primary kinin? |
Bradykinin |
|
|
What is the primary function of the clotting system? |
to clot blood by producing a fibrinous meshwork at the site injury |
|
|
Which plasma protein system causes local vascular dilation and permeability by activating the kinin system? |
Clotting System |
|
|
the dissolution or destruction of a cell |
cytolysis |
|
|
Which system involves the production of a sequential cascade of plasma proteins and functions in inflammation and immunity? |
Complement System |
|
|
Which cells release histamine? |
Mast Cells |
|
|
What does histamine cause? |
an increase in vascular permeability and vasodilation |
|
|
The complement system can cause ________ and _______. |
cytolysis and opsonization |
|
|
the enhancement of phagocytosis by a process in which a pathogen is marked, with opsonins, for destruction by phagocytes |
opsonization |
|
|
What other biochemical mediators are released by the body during inflammation? Not from blood. |
Prostoglandins and Lysosmal Enzymes |
|
|
Cause increased vascular dilation and permeability, tissue pain and redness, and changes in connective tissue |
Prostaglandins |
|
|
Act as chemotactic factors and may cause damage to connective tissues and to the clot when released by WBCs |
lysosomal enzymes |
|
|
What biochemical mediators of inflammation are released by pathogenic microorganisms? |
Endotoxins and Lysosomal Enzymes |
|
|
Produced by cell walls of gram-negative bacteria and serves as a chemotactic factor; can activate complement, function as an antigen, and damage bone and tissue. |
endotoxin |
|
|
What are four major systemic manifestations of inflammation? |
|
|
|
an elevation of body temperature to greater than the normal level of 37 degrees C |
Fever |
|
|
Where is body temperature controlled? |
hypothalamus |
|
|
fever-producing substances produced by WBCs and pathogens |
pyrogens |
|
|
a temporary increase n the number of white blood cells circulating in blood |
leukocytosis |
|
|
What is the normal number of WBCs per mm of blood? |
4,000 to 10,000 |
|
|
During leukocytosis what is the range of WBCs increased to? |
10,000 to 30,000 |
|
|
An increase in lymphocytes indicates... |
a viral infection |
|
|
An increased in neutrophils indicates.... |
a bacterial infection |
|
|
An increase in eosinophils indicates.... |
an allergic reaction |
|
|
abnormal enlargement of lymph nodes |

lymphadenopathy |
|
|
Which cells are the main WBCs involved in he immune response? |
Lymphocytes |
|
|
an enlargement of a tissue or organ resulting from an increase in the size of its individual cells, but not in the number of cells |
hypertrophy
*like your head gets big when you win a trophy* |
|
|
an enlargement of a tissue or organ resulting from an increase in the number of normal cells; the result of increased cell division |

hyperplasia |
|
|
True or False? Changes in the lymphocyte population usually occur during acute inflammation. |
False; they occur during chronic inflammation |
|
|
the ring of lymphatic tissue formed by the two palatine tonsils, the pharyngeal tonsil, the lingual tonsil, and intervening lymphoid tissue |
Waldeyer's Ring |
|
|
a nonspecific protein, produced in the liver, that becomes elevated during episodes of acute iflammation or infection |
C-reactive protein |
|
|
Where is C-reactive protein produced? |
the liver |
|
|
What does C-reactive protein interact with? |
the complement system and the clotting mechanism |
|
|
What concentration of C-reactive protein is considered high? |
more than 10 mg/L |
|
|
this can be used to help assess rheumatoid arthritis, systemic lupus, monitor tissue healing, and detect infections |
C-reactive protein |
|
|
A chronically elevated level of C-Reactive protein is associated with an increased risk for _________ _______. |
cardiovascular disease |
|
|
C-reactive protein may also be a marker for... |
periodontal disease activity |
|
|
What WBCs are involved in chronic inflammation? |
macrophages lymphocytes plasma cells neutrophils monocytes fibroblasts |
|
|
a collection of macrophages usually surrounded by a rim of lymphocytes and plasma cells |
granuloma |
|
|
How do antiinflammatory drugs work? |
they inhibit the synthesis of prostaglandin |
|
|
the decrease in size and function of a cell, tissue, organ, or whole body |

atrophy |
|
|
the process by which injured tissue is replaced with tissue identical to that present before the injury |
regeneration |
|
|
the restoration of damaged or diseased tissues by cellular change and growth |
repair |
|
|
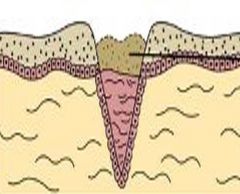
What are the three phases to the repair process during the 2 weeks? |
|
|
|
What microscopic events occur during the day of injury? |
|
|
|
What microscopic events occur during the day after the injury? |
|
|
|
the formation of fibrous tissue, as normally occurs in healing |
fibroplasia |
|
|
the formation and differentiation of blood vessels |
angiogenesis |
|
|
the initial connective tissue formed in healing |
granulation tissue |
|
|
the process of being covered with epithelium |
epithelialization |
|
|
What microscopic events occur two days after injury? |
|
|
|
What microscopic events occur seven days after injury? |
|
|
|
a fibroblast that has some of the characteristics of smooth muscle cells, such as the ability to contract |
myofibroblast |
|
|
What microscopic events occur two weeks after injury? |
Initial granulation tissue and its fibers have been remodeled. Matured, fibrous connective tissue is called scar tissue. |
|
|
What are the three types of repair that can occur? |
|
|
|
the healing of an injury in which little loss of tissue takes place |
healing by primary intention |
|
|
the healing of an injury in which tissue is lost; thus the edges of the injury cannot be joined during healing |
healing by secondary intention
*tooth extraction* |
|
|
excessive skin scarring that appears raised and extends beyond its original boundaries |
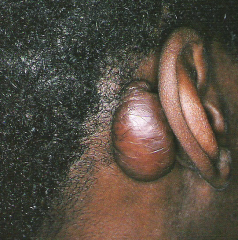
keloid |
|
|
delaying surgical tissue repair until infection is resolved |
healing by tertiary intention |
|
|
the pathogenic death of one or more cells, or a portion of tissue, or an organ that results from irreversible damage to cells |
necrosis |
|
|
bone-forming cells |
osteoblasts |
|
|
What are some traumatic injuries that can occur to the teeth? |
attrition abrasion abfraction erosion |
|
|
the wearing away of tooth structure during mastication
tooth-to-tooth wear
may be observed in primary and permanent dentition |

Attrition
*greater in men* |
|
|
the grinding of the teeth together for non-functional purposes |

Bruxism
|
|
|
the pathologic wearing away of tooth structure that results from a repetitive mechanical habit |

Abrasion
|
|
|
appears as a wedge-shaped defect at the cervical area of teeth, especially premolars; caused from microfracture of tooth structure in areas of concentration of stress |

Abfraction
*prevention may involve fabricating an acrylic splint* |
|
|
the loss of tooth structure resulting from chemical action without bacterial involvement |

Erosion
the area of erosion appears smooth and polished |
|
|
an eating disorder characterized by food binges followed by self-induced vomiting; results in erosion on the lingual aspect of teeth |

Bulimia
Fluoride Rinse and Toothpaste Rinse with water Avoid brushing immediately after purging
|
|
|
eating disorder which is characterized by intense fear of gaining weight and self-imposed starvation |
anorexia nervosa |
|

the extensive and rapid destruction of the teeth due to methamphetamine abuse |
Meth Mouth |
|

|
Aspirin Burn
Usually Heals in 7 to 21 Days Caused from misuse of Aspirin |
|

|
Phenol Burn
*product used in dentistry as a cavity-sterilizing and cauterizing agent; can also be found in over the counter drugs* |
|
|
usually seen in infants and young children who have bitten or chewed a live electric cord |
electric burn |
|
|
Hot Food Burn
|
|
|
Lesion Associated with Cocaine Use
Usually located at the midline of the hard palate. |
|

|
Traumatic ulceration caused by irritation of the gingiva by fingernails.
Self-Induced Lesion |
|

|
Chronic Tongue Chewing
Self-Induced Lesion |
|
|
a lesion that results from the accumulation of blood within tissue as a result of trauma; appears red to purple to bluish-gray mass; frequently seen on labial or buccal mucosa |

Hematoma |
|

|
Traumatic Ulcer
*usually heals in 7 to 14 days and may require a biopsy* |
|

|
Traumatic Granuloma |
|
|
a thickening of the keratin on the surface |
hyperkeratosis |
|

|
Frictional Keratosis |
|

A benign lesion typically associated with pipe and/or cigar smoking and may also occur with cigarette smoking |
Nicotinic Stomatitis |
|
Early lesion may have a granular or wrinkled appearance Long-standing lesions may be more opaquely white and have corrugated surface |
Tobacco Pouch Keratosis/Smokeless Tobacco Keratosis |
|
|
a lesion caused by injury to a perpipheral nerve |
Traumatic Neuroma
*Treatment is surgical excision* Can be painful and a biopsy is needed to diagnose. |
|
|
benign lesion; mucosal nodule; well-circumscribed lesion that is composed of nerve tissue partially surrounded by fibrous connective tissue; considered a reactive, hyperplastic lesion |
Palisaded Encapsulated Neuroma |
|

Normal physiologic pigmentation of the oral mucosa. |
Melanosis |
|

a degeneration of the tissue of the lips, caused by exposure to the sun |
Solar Cheilitis |
|
|
What are the three mucous retention lesions? |
mucocele ranula mucous cyst |
|

a lesion that forms when a salivary gland secretion spills into the adjacent connective tissue
not lined with epithelium |
Mucocele |
|
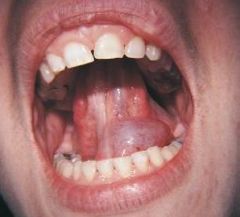
a larger mucocele-like lesion that forms unilaterally on the floor of the mouth |
Ranula
*surgery is needed* |
|

a salivary gland stone |
Sialolith
*milked or surgically removed* |
|

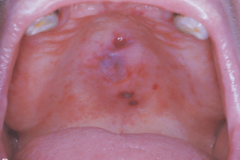
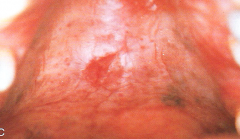
a benign condition of salivary glands characterized by moderately painful swelling and ulceration affects the tissue at the junction of the hard and soft palate loss of blood supply to salivary gland |
Necrotizing Sialometaplasia |
|
|
inflammation of salivary gland tissue |
sialadenitis |
|
|
Sialadenitis can be _____ or ______ and diagnosis may require ________ of a radiopaque dye into the gland. |
acute or chronic
injection |
|
|
consists of proliferating , exuberant granulation tissue and hyperplastic fibrous connective tissue ; these lesions result from over-zealous repair |
reactive connective tissue hyperplasia |
|

|
Pyogenic Granuloma/Pregnancy Tumor
*name is a misnomer* |
|

a lesion composted of well-vascularized connective tissue with multinucleated giant cells |
Peripheral Giant Cell Granuloma
*surgically removed* |
|

a broad-based, persistent exophytic lesion composed of dense, scarlike connective tissue containing few blood vessels |
Irritation Fibroma
*surgically removed* |
|

a common exophytic gingival lesion that can clinically resemble an irritation fibroma |
Peripheral Ossifying Fibroma |
|
|
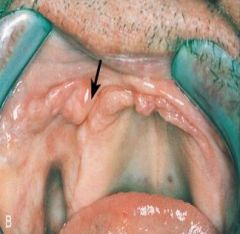
Denture-Induced Fibrous Hyperplasia (Epulis Fissuratum)
*surgical removal needed* |
|

|
Papillary Hyperplasia of the Palate
*surgery may be needed for removal* |
|

characterized by an increase in the size of the marginal an attached gingiva usually involving the interdental papillae |
Gingival Enlargement
*gingivoplasty orgingivectomy* or *meticulous home care* |
|

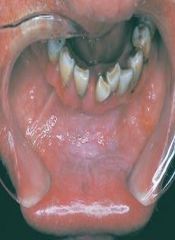
an excessive proliferation of chronically inflamed dental pulp tissue |
Chronic Hyperplastic Pulpitis
*extraction or endodontic treatment* |
|

composed of purulent exudate (pus), surrounded by connective tissue containing neutrophils an lymphocytes |
Acute Periapical Abscess
*painful for patient due to inflammation* *may need to have tooth extracted or drained* |
|
a localized mass of chronically inflamed granulation tissue that forms at the opening of the pulp canal, generally at the apex of a nonvital tooth root |
Dental Granuloma/Periapical Granuloma/Chronic Apical Periodontitis
*extraction or endodontic therapy* |
|
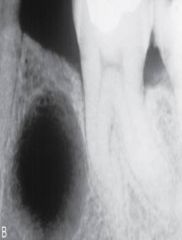
a true epithelium lined cavity
a result of proliferation of the rests of Malassez
usually asymptomatic |
Radicular Cyst
*extraction, curettage, endodontic treatment, or apicoectomy* |
|
form when the tooth is removed and all or part of a radicular cyst is left behind |
residual cyst
*surgical removal* |
|
|
when a cause cannot be identified |
idiopathic |
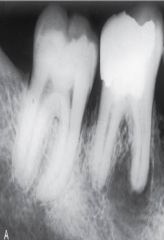
|

a change in bone near the apices of teeth that may be a reaction to low-grade infection
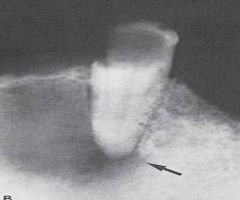
mandibular 1st molar most commonly assiciated |
Focal Sclerosing Osteomyelitis
*no treatment needed* |
|
|
a postoperative complication of tooth extraction |
Alveolar Osteitis / "Dry Socket"
*pain management, irrigation, and insertion of a medical dressing* |

