![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
295 Cards in this Set
- Front
- Back
|
|
|
|
|
|
|
A system of reflex points used by Frank Chapman, DO and described by Charles Owens, DO are called what?
|
Chapman's Points
|
|
|
Chapman's Points are Predictable anterior and posterior ____ _____ texture abnormalities assumed to be reflections of visceral disease*
|
fascial tissue
|
|
|
Chapman's Points are what type of reflex?
|
Viscero Somatic Reflex
|
|
|
what is a Gangliform congestion - increased sympathetic tone, in deep fascia or by periosteum, resulting in lymphatic edema and myofascial thickening?
|
Chapman's Points
|
|
|
a chapman point is a A painful nodule that has been described as:
|
Small, Smooth, Firm, Discreetly palpable
|
|
|
anterior chapman points are more for diagnostic or treatment?
|
anterior diagnostic. (don’t really treat the front)
|
|
|
between what anterior ribs would you find the esophagus reflex?
|
ANTERIOR - 2nd intercostal space at the Sternal Border
|
|
|
constipation, memory loss, coarse hair, dry skin, all of these are symptoms of a condition that could be noticed at which chapman point?
|
Thyroid! ANTERIOR - 2nd intercostal space at the Sternal Border. POSTERIOR- The space between the transverse processes of T2 and T3 midway between the spinous process and the tip of the transverse process.
|
|
|
between what posterior vertebrae would you find the thyroid reflex?
|
POSTERIOR- The space between the transverse processes of T2 and T3 midway between the spinous process and the tip of the transverse process.
|
|
|
if you cut someone off of steroids, what do you worry about?
|
adrenal insufficiency
|
|
|
where are the anterior adrenal reflex chapman points?
|
lateral aspect of rectus abdominis, at the level of the inferior margin of the costal margin.
|
|
|
where are the posterior adrenal reflex chapman points?
|
intertransverse spaces on both sides of T11 and T12, midway between spinous processes and transverse processes.
|
|
|
what do you do with posterior chapman points?
|
treated, by applying inhibitory pressure in a slow circular fashion for 10 to 30 seconds until any associated tissue texture change resolves. Treatment can vary from15 seconds to 2 minutes.
|
|
|
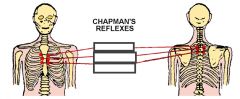
the following describes the chapman point for which viscera?: Anterior, Intercostal space between the 2nd and 3rd ribs close to the sternum. Posterior, midway between the spinous process and the tips of the transverse processes at T2
|
myocardial, bronchus, esophagus, and thyroid
|
|
|
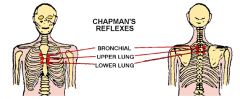
where are the chapman points for the upper lung?
|
Upper lung: Anterior, Intercostal space between the 3rd and 4th ribs close to the sternum. Posterior, midway between the spinous processes and the tips of the transverse processes of T3 and T4
|
|
|
where are the chapman points for the lower lung?
|
Lower lung: Anterior, Intercostal space between the 4th and 5th ribs close to the sternum. Posterior, midway between the spinous processes and the tips of the transverse processes of T4 and T5
|
|
|
chapman is at which intercostal space?: myocardial, bronchus, esophagus, and thyroid
|
2
|
|
|
chapman is at which intercostal space?: upper lung
|
3
|
|
|
chapman is at which intercostal space?: lower lung
|
4
|
|
|
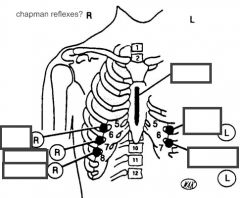
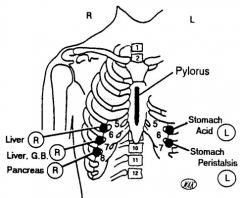
chapman is at which intercostal space?: liver
|
5th and 6th on the right
|
|
|
chapman is at which intercostal space?: stomach acid
|
5th left
|
|
|
chapman is at which intercostal space?: gall bladder
|
6th on the right
|
|
|
chapman is at which intercostal space?: stomach peristalsis
|
6th on the left
|
|
|
what chapman points are at the 7th intercostal space? (right and left)
|
right pancreas, left spleen
|
|
|
which chapman is at the 12th rib on the right?
|
apendix
|
|
|
chapman point for the appendix?
|
tip of the 12th rib on the right
|
|
|
what is the chapman point for the colon?
|
iliotibial band
|
|
|
iliotibial band is what chapman point?
|
colon
|
|
|
Distal portion of the ureters and the bladder receive parasympathetics from?
|
S2-S4
|
|
|
Lesser Splanchnics Synapse at what ganglion?
|
Superior mesenteric
|
|
|
sympathetic innervation to the small intestine, kidney, ureters, gonads, right colon?
|
T10-11
|
|
|
sympathetic innervation to the left colon, pelvic organs, bladder, distal ureters?
|
T12-L2
|
|
|
Sympathetic innervation to the head an neck?
|
T1-4
|
|
|
sympathetic innervation to the heart?
|
T1-6
|
|
|
Sympathetic innervation for the esophagus?
|
T2 - T8
|
|
|
Asthma reflex?
|
T2 left
|
|
|
VS: Bronchial mucosa
|
T2-3 lateralized
|
|
|
VS: Anterior infarct
|
T2-3 on L
|
|
|
Esophageal reflex?
|
T2
|
|
|
VS: Lung
|
T3-4 lateralized
|
|
|
VS: Inferior infarct
|
T3-5 on L
|
|
|
VS: Atria
|
T4-6
|
|
|
VS: Gallbladder
|
T6 on R
|
|
|
VS: Stomach
|
T5-8 on L
|
|
|
VS: Bile duct
|
T6 on R
|
|
|
VS: Pancreas
|
T7 on R
|
|
|
Duodenum Reflex?
|
T7-T8 right
|
|
|
VS: Small Intestine
|
T8-10
|
|
|
What are the 3 basic mechanisms for SOFT TISSUE?
|
"Tractional technique (longitudinal traction)
|
|
|
What is acheived through Soft Tissue?
|
Increase blood flow, remove metabolites, Increase GAGs, break Crosslinks
|
|
|
What is acheived through Articulatory Techniques?
|
Improve mobility by stretching tight muscles, induce fibroblasts to secrete GAGs and decrease joint adhesions, relieve pain.
|
|
|
How do Articulatory techniques act as a pain reliever?
|
Induce fast Group 1A (mylenated fibers) to inhibit (Group C) nociceptive fibers.
|
|
|
What is the goal of Muscle Energy Technique?
|
reset intrafusal/extrafusal fiber lenghts
|
|
|
Isometric ME?
|
EQUAL and OPPOSITE FORCE
|
|
|
Isotonic ME?
|
Physician has YIELDING COUNTERFORCE. Muscle maintains tone.
|
|
|
Isolytic ME?
|
Physician has STRONGER FORCE. Muscle forced to contract and elongate. This is most commonly used for the treatment of fibrotic or chronically shortened myofascial tissues.
|
|
|
What are the most common errors in MET?
|
"1. not monitoring motion of involved joint with palpating hand
|
|
|
Reciprocal Inhibition
|
"muscular contraction to produce a reflex
|
|
|
Crossed Extensor Reflex
|
This learned reflex applies to the relaxation of muscles with contraction on contralateral homologous muscles.
|
|
|
Monoarticular Muscles:
|
short restrictors, Type II segmental dysfunctions.
|
|
|
Polyarticular Muscles
|
long restrictors, maintaining Type I group dysfunctions.
|
|
|
Inferior scapula angle level?
|
T8 Transverse process, or T7 spinous process!!!
|
|
|
Pectus excavatum
|
"Caved in (think excavation),
|
|
|
Creep
|
Connective Tissue elongates but the deformation is constant
|
|
|
Ease
|
Direction of ease for connective tissue
|
|
|
Bind
|
Palpable restriction in motion, tightness in connective tissue
|
|
|
What are the types of fibers that inhibit nociceptive Group C fibers?
|
Group 1A (Fast) fibers
|
|
|
What is the role of joint manipulation on inhibitory monoamine interneurons?
|
Prevents transmission of nociceptive fibers
|
|
|
Monoarticular fibers are also known as?
|
short restrictor muscles in Type II somatic dysfunctions
|
|
|
Polyarticular fibers are also known as?
|
long restrictor muscles in Type I neutral somatic dysfunctions.
|
|
|
Where is MET derived from?
|
Ruddy's "resistive duction", but officially developed by Fred Mitchell.
|
|
|
Burns study in Muscle Energy?
|
Burns found cervical range of motion in all three planes was improved in response to MET in experimental vs. control groups.
|
|
|
What is tensegrity?
|
Trasmits loads through tension and compression. Dome shape skeleton.
|
|
|
What is the action of the piriformis?
|
"It ""CLOSE PACKS"" and stabilizes teh SI joint at the inferior pole of hte sacral axis.
|
|
|
What are the 8 steps of Muscle Energy?
|
"8 steps:
|
|
|
How would you find the L5 relative to the PSIS?
|
L5 Is 30 degree superior/medial to the most prominent aspect of the PSIS.
|
|
|
What is the relationship between GTO's and muscle energy?
|
post-isometric relaxation and inhibition of agonist muscles is due to GTO's. GTO's are very sensitive to minute changes in muscle and they have an inhibitory influence (type 1b fibers). They DO NOT function as safety valves and work in line with muscle spindles. They can't gauge threshold of contraction.
|
|
|
What is isometric contraction
|
Change in muscle tension without approximation of it’s origin and insertion. Equal force (pt and physician)
|
|
|
What is mechanism of action of the Isotonic contraction?
|
"1. Resets the intrafusal and extrafusal muscle fiber lengths during the post-contraction relaxation phase
|
|
|
What is isotonic contraction?
|
Approximation of muscle origin and insertion without change in muscle tension. Yielding physician force. Patient wins
|
|
|
What is isolytic contraction?
|
Contraction of a muscle against resistance while forcing the muscle to lengthen. Stronger physician force. used to stretch and break down fibrotic adhesions in affected soft tissue structures.
|
|
|
What is antagonistic contraction?
|
a techniques that uses isometric forces to reciprocally inhibit antagonistic muscles that are hypertonic
|
|
|
What is the H-reflex?
|
how much motor output is emanating from the anterior horn cells. Decreased H-reflex = relaxation.
|
|
|
How does the H-reflex relate to MET?
|
During relaxation of MET, alpha motor neurons are inhibited, so it allows us to reposition a joint. It also helps to inhibit nociceptive fibers activated by mechanoreceptors.
|
|
|
What is hysteresis
|
Energy loss in CT due to many load and unload cycles.
|
|
|
Do you perform Soft Tissue on one side only?
|
No, it is a bilateral technique so you'd perform on both sides
|
|
|
Which of the cervical articulatory techniques are regional/ segmental?
|
Flexion, Sidebending, Rotation are regional, but Extension (is only segmental), and Sidebedning can be segmental.
|
|
|
What are the dural attachments?
|
"1. OA
|
|
|
Why are C3-C7 considered pseudo Type II?
|
They have rotation and sidebending to the SAME SIDE, but they can be flexed, extended, or neutral.
|
|
|
Where is the C1 transverse process?
|
Between mastoid and mandible
|
|
|
Which is the first palpable spinous cervical process?
|
C2
|
|
|
Which ligament is especially important for rotation/
|
Transverse ligament (cruciate ligament)
|
|
|
What percentage of rotation is due to the AA joint?
|
50%
|
|
|
In the cervical region, why would you want to palpate the articular pillars instead of the transverse processes?
|
TP's are more sensitive
|
|
|
Where is the cricoid cartilage? (cervical level?)
|
C6
|
|
|
At what level is the hyoid bone?
|
C3
|
|
|
What cervical level is the thryoid cartilage?
|
C4-5
|
|
|
What is the fingerwidth rule?
|
each cervical vertebrae is about a finger width apart
|
|
|
What is the normal range of cervical flexion?
|
60 degrees
|
|
|
What is the normal range of cervical extension?
|
90 degrees
|
|
|
What is the normal range of cervical sidebending? Rotation?
|
45 degrees; 90 degrees
|
|
|
What is the Cobb angle used for?
|
It is usually used to monitor scoliosis progression. It only looks at one plane though.
|
|
|
What is the function of ligaments?
|
"They connect, stabilize and guide the bones forming the articulation.
|
|
|
What are the components of the intervertebral discs?
|
"1. Nucleus pulposus: 70-90% water. Also composed of collagen and proteoglycans. (proteoglycans attract water)
|
|
|
How do you decribe the motions of a spinal segment?
|
Description is always of a given segment relative to the segment below!
|
|
|
If a spinal segment is rotated right, how does the spinous process move?
|
Spinal process is moved to the left
|
|
|
What are the long restrictor muscles? involved in Type I Somatic Dysfunctions
|
"Erector spinalis
|
|
|
What are the short restrictor muscles involved in Type II somatic dysfunctions?
|
"Multifidus
|
|
|
In an extended position, which spinal ligament is taut?
|
Anterior longitudinal ligament
|
|
|
In a type I mechanic, where is the weight distributed on the vertebrae, how about Type II?
|
"Type I: vertebral body (since neutral)
|
|
|
What are the steps of palpation
|
"1. Detect
|
|
|
What are trophic changes?
|
"feel for bumpy areas, scaliness, unusually smooth or
|
|
|
What is a palpatory Red reflex?
|
"increased redness in areas that have been palpated (caused
|
|
|
What do alpha motor neurons innervate?
|
extrafusal fibers
|
|
|
What do gamma afferents innervate?
|
muscle spindles and intrafusal muscles
|
|
|
What are C fibers?
|
They have little myelin, can promote pain or inhibit pain. They can release neuropeptides. At low levels of sensitization ( inhibit pain). High levels (sensitized to pain).
|
|
|
What is tractional technique?
|
Soft tissue, structures are longitudinally separated.
|
|
|
What technique is particularly useful for treating transitional zones?
|
Articulatory
|
|
|
What are the joints of luschka
|
"Synovial joints in C3 to C7. Lateral aspect of body has superior projection (uncinate process), this process projects up and contacts a lip that projects down from the body above.
|
|
|
What parts of the heart do right sided autonomic fibers innervate?
|
Right heart and SA node
|
|
|
Left sided sympathetics innervate what part of the heart?
|
Left heart and AV node
|
|
|
Hypertonia of right sided sympathetics lead to what heart condition?
|
Supraventricular tachycardia
|
|
|
Hypertonia of left sided sympathetics lead to what?
|
Ectopic foci and v-fib
|
|
|
Left vagus innervates which part of the heart?
|
AV node
|
|
|
Hyperactivity of the left vagus nerve leads to which heart complication?
|
AV blocks
|
|
|
Appropriate action for a young male that comes in with recurrent urinary tract infections?
|
an imaging study
|
|
|
Inferior vagal ganglion sits where?
|
Body of C2
|
|
|
Greater splanchnics synapse @ what ganglion?
|
Celiac
|
|
|
Increased sympathetic tone has what affects on the lungs?
|
Increase bronchiole dilation, increase thickness of secretions, increase vasoconstriction of lung tissue, increase in goblet cells
|
|
|
Least splanchnics synapse at what ganglion?
|
Inferior mesenteric
|
|
|
Posterior Chapman's point for bladder?
|
intertransverse space between L1-2 and T12-L1
|
|
|
Posterior Chapman's point for adrenal glands?
|
intertransverse space on both sides of T11 and T12 midway between spinous processes and transverse processes
|
|
|
Superior vagal ganglion sits where?
|
Jugular Foramen
|
|
|
Anterior Chapman's point for adrenal glands?
|
One inch lateral and two inches superior to umbilicus
|
|
|
Kidney Anterior Chapman's point?
|
One inch lateral, one inch superior to the umbilicus
|
|
|
Parasympathetics fore left colon and rectum?
|
Pelvic splanchnics (S2-S4)
|
|
|
What type of axons are carried in the splanchnic nerves?
|
preganglionic sympathetic
|
|
|
Anterior Chapman's point for bladder?
|
umbilical area
|
|
|
Sympathetic effects on kidney afferent arterioles?
|
vasoconstriction
|
|
|
Dorsal wrist counterstrain points are treated in which position?
|
extension of the wrist
|
|
|
Ventral wrist counterstrain points are treated in which position?
|
flexion of the wrist
|
|
|
Which counterstrain tender points are treated with by flexing or extending the carpometacarpal joint and applying traction?
|
interossei tender points
|
|
|
Treatment for radial head/lateral epicondyle tender points?
|
Hold elbow in full extension, supinate and abduct arm. Hold for 90s
|
|
|
Treatment for coronoid counterstrain tender points?
|
fully flex elbow, forearm is pronated and abducted gently. Hold for 90s.
|
|
|
Treatment for olecranon counterstrain tender point?
|
elbow is hyper extended and forearm is abducted slightly and supinated
|
|
|
Location of anterior acromioclavicular tender point?
|
anterior surface of distal clavicle
|
|
|
Location of long head of biceps tender point?
|
over the tendon
|
|
|
Location of short head of biceps tender point?
|
inferolateral to the coracoid process
|
|
|
Location of posterior acromioclavicular tender point?
|
behind the lateral end of the clavicle
|
|
|
Location of supraspinatus tender point?
|
in the supraspinatus fossa
|
|
|
Location of subscapularis tender point?
|
on the anterior surface of the scapula in the axilla
|
|
|
Location of latissimus dorsi tender point?
|
deep in the axilla on the medial surface of the humerus
|
|
|
Treatment for anterior acromioclavicular tender point?
|
Patient supine. Arm is adducted across the chest 30 - 50 degrees and slightly internally rotated. Apply traction by pulling on wrist.
|
|
|
Treatment for long head of biceps tender point?
|
Patient supine. Arm is supinated and flexed 90 degrees at elbow and shoulder. Apply downward pressure @ elbow along the humerus.
|
|
|
Treatment for posterior acromioclavicular counterstrain tender point?
|
Patient prone. Adduct arm across back. Apply traction by pulling @ wrist. Hold for 90s.
|
|
|
Treatment for short head of biceps tender point is the same as what other tender point?
|
long head of biceps tender point.
|
|
|
Treatment for supraspinatus tender point?
|
Patient supine. Flex and abducted to 120 degrees. Externally rotate the humerus. Hold for 90s.
|
|
|
Treatment for subscapularis tender point?
|
patient supine. Hold patients arm posteriorly over side of table and toward feet. Internally rotate arm. NO TRACTION! Hold for 90s.
|
|
|
Treatment for latissimus dorsi tender point?
|
Patient supine. Hold patients arm posteriorly over side of table and toward feet. Internally rotate arm. ADD TRACTION. Hold for 90s.
|
|
|
Major motion of the occiput?
|
flexion/extension
|
|
|
Newborn cannot suckle properly and has problems swallowing. She is hiccupping, vomiting, and has what looks like torticollis. What somatic dysfunction can cause these symptoms in a newborn?
|
Occipital condylar compression
|
|
|
In a C3 RL SL dysfunction, what would you do with the neck to lock out vertebrae below C3 if performing a rotational HVLA correction
|
sidebend neck to the left
|
|
|
In a C3 RL SL dysfunction, where would the MCP joint of your correcting hand be placed if using a rotational HVLA correction?
|
Left MCP joint on the posterior aspect of C3
|
|
|
In a C4 RL SL dysfunction, what would you do with the neck to lock out vertebrae below C4 if performing a sidebending HVLA correction?
|
Rotate neck to left
|
|
|
If OA SLRR, which Transverse Process is closer to the mandible (left or right)?
|
Right, (meaning you feel the articular process more posterior on this side) though not as full (deep occ shelf)
|
|
|
If OA SLRR, which Transverse Process is closer to the mastoid (left or right)?
|
Left, (meaning you feel the articular process on this side more anterior than the other side) and therefore fullness (shallow occ shelf)
|
|
|
If OA SLRR, which articular pillar has the deeper occipital shelf, (left or right)?
|
Right
|
|
|
If OA SLRR, which articular pillar has the shallower occipital shelf, (left or right)?
|
Left
|
|
|
If OA SRRL, which Transverse Process is closer to the mandible (left or right)?
|
Left, (meaning you feel the articular process more posterior on this side) though not as full.
|
|
|
If OA SRRL, which Transverse Process is closer to the mastoid (left or right)?
|
Right, (meaning you feel the articular process on this side more anterior than the other side) and therefore fullness.
|
|
|
If OA SRRL, which articular pillar has the deeper occipital shelf, (left or right)?
|
Left
|
|
|
If OA SRRL, which articular pillar has the shallower occipital shelf, (left or right)?
|
Right
|
|
|
in cervical dysfunction, Articular fullness is on the side ____ Sidebending (tender).
|
Opposite. Ex . C4 FRLSL. Fullness on the right but articular pillar feels posterior on the left
|
|
|
mandible or mastoid is more posterior?
|
Mastoid
|
|
|
Arms receive their sympathetic innervation from which levels?
|
T2-T8
|
|
|
Legs receive their sympathetic innervation from which levels?
|
T11-L2
|
|
|
Atrial pain refers to what dermatomes?
|
T4-T6
|
|
|
Trigger point that serves an initiating role in supraventricular tachycardia?
|
Right pec major in the 5th intercostal space
|
|
|
Anterior bronchiole Chapman's point?
|
2nd intercostal space
|
|
|
Upper lung Chapman's point?
|
3rd intercostal space
|
|
|
Lower lung Chapman's point (anterior)?
|
4th intercostal space
|
|
|
Inferior wall MI; expect somatic dysfunction at which levels?
|
T3-T5 left and C2
|
|
|
Anterior wall MI; expect somatic dysfunction at which levels?
|
T2-T3 left
|
|
|
If there is atrial involvement during an MI expect somatic dysfunction at which levels?
|
T4-T6
|
|
|
Ventricular involvement during an MI would present with somatic dysfunction at which levels?
|
C8 - T3
|
|
|
Chapman Anterior T1 location?:
|
apex of sternal notch
|
|
|
Chapman Anterior T2 location?:
|
middle of the manubrium
|
|
|
Chapman Anterior T3-6 location?:
|
on the sternum at the same numbered costal level
|
|
|
Chapman Anterior T7 location?:
|
under the costalchondral margin, lateral, and inferior to the xiphoid process
|
|
|
Chapman Anterior T8 location?:
|
approximately 3 cm below the xiphoid process
|
|
|
Chapman Anterior T9 location?:
|
1-2 cm above the umbilicus, 2-3 cm lateral to the midline
|
|
|
Chapman Anterior T10 location?:
|
1-2 cm below the umbilicus, 2-3 cm lateral to the midline
|
|
|
Chapman Anterior T11 location?:
|
5-6 cm below the umbilicus, 2-3 cm lateral to the midline
|
|
|
Chapman Anterior T12 location?:
|
inner surface of the iliac crest at the midaxillary line
|
|
|
Anterior inguinal tender point = ?
|
Located on the lateral border of the pubic bone near the attachment of the inguinal ligament
|
|
|
T3 likes to SB to left side, right lateral pillar is prominent, what is diagnosis?
|
T3 SLRL Why? Have to SB and rotate to same side, fullness is found b/c facet joint on right side opens up and causes fullness
|
|
|
in the cervical spine, Preganglionic sympathetics travel from spinal nerves ___ to ___ and postganglionics travel to head, neck
|
T1-T4
|
|
|
The occipital condyles converge anteriorly at a ___ degree angle.
|
30 degree
|
|
|
The cruciform ligament forms a cross, and can be seen with the tectorial membrae removed. The horizontal portion gives integrity to the AA joint, if torn, sudden death is secondary to compression of the medulla or spinal cord. What is the name of this sub-ligament?
|
Transverse ligament (cruciate ligament)
|
|
|
posterior herniations are difficult in the typical cervicals due to broad _____ longitudinal ligament or tectorial membrane.
|
posterior
|
|
|
Pt prefers FB and dislikes BB, SB, or rotation to that side because these motions reduce size of what?
|
intervertebral foramen. Cervical Root pressure.
|
|
|
Pt prefers BB and slight sidebending to side of herniation keeps ___ ____ away from neural structures dislikes FB and sidebending.
|
nucleus pulposus , as in Cervical Disc Herniation
|
|
|
Neurovascular compression between anterior and middle scalenes or clavicle and first rib or pectoralis minor and upper ribs are also known as what?
|
Thoracic outlet syndrome
|
|
|
Suboccipital symptoms of tissue texture change and tension are usually associated with ___ ____ dysfunction.
|
upper thoracic
|
|
|
Acute neck problems usually involve ____ muscle (scalenes, SCM) while chronic problems usually involve ___ muscles (trapezius, levator)
|
prevertebral, postural
|
|
|
what motion causes articular pillars to close up?
|
back bending. SB and FB cause them to open up.
|
|
|
How do you do a Spurling Test and what does it look for?
|
The examiner extends the patient’s neck and rotates/SBs it to one side with axial compression (caudad)on the pt’s head. Positive sign: pain elicited down the ipsilateral arm from the neck (the side of the pt.’s symptoms). Indicates: cervical disc disease/nerve root irritation (Note: pain on ipsilateral side of neck could suggest facet pathology.)
|
|
|
How do you do a Underburg Test and what does it look for?
|
Supine, backward bend, rotate, WAIT 30 seconds. Positive with dizziness, nausea, lightheadedness. Test for vertebral artery insufficiency.
|
|
|
What is the rule of 3's?
|
Thoracic spinous processes are located at the level of the transverse process from T1-T3. From T4 to T6, they are halfway down to the next vert. The next 3 vertebrae, T7-T9, they are one vert below. And for T10-T12, they gradually go back to same level.
|
|
|
What is Yergason's Test?
|
Yergason’s Test-(Fig. A) Examiner externally rotates pt’s arm against resistance. +: Tendon will pop out of groove or pain, indicating unstable biceps tendon or subluxation
|
|
|
What is Speed's Test?
|
Speed’s Test-(Fig. B) Pt. elevates arm against resistance. +: Pain in bicipital groove, indicating tendon pathology, usually tendinitis.
|
|
|
Parallelogram effect: what is the movement of the wrist, ulnar head, and radial head when the carrying angle is altered?
|
When the carrying angle is increased, the ulna is abducted, and the radius glides distally, the radial head adducts a little bit, and the wrist is adducted. When the carrying angle is decreased, the wrist abducts, the radius glides proximally, the elbow moves slightly away from the body, and the ulnar head is adducted.
|
|
|
Supinate or pronate to make radial head move anteriorly?
|
Supinate (as when falling backwards)
|
|
|
Supinate or pronate to make radial head move posteriorly?
|
pronate (as when falling forwards)
|
|
|
Tell me about Halstead maneuver:
|
exaggerated military posture. Narrows costoclavicular space. scapula retracted and depressed with chest protruding.
|
|
|
Tell me about Wright’s maneuver.
|
shoulder external rotation, abduction beyond 90 degrees. Compresses below pectoralis minor insertion
|
|
|
Tell me about the Adson’s test: what do you do and what is a positive sign indicative of?
|
Neck extended, turned toward affected side. narrows interscalene space. Checks patency of ipsilateral artery passing between scalene triangle Positive with decreased or absent radial pulse on affected side
|
|
|
Where would you look for a heart issue that caused tachyarrhythmia of the SA?
|
Sympathetics. Right. T1-T6.
|
|
|
Where would you look for a heart issue that caused bradyarrhythmia of the SA?
|
Parasympathetics. Right. Vagus.
|
|
|
Where would you look for a heart issue that caused tachyarrhythmia of the AV?
|
Sympathetics. Left. T1-T6.
|
|
|
Where would you look for a heart issue that caused bradyarrhythmia of the AV?
|
Parasympathetics. Left. Vagus
|
|
|
SA node gets parasympathetic innervation from which nerve?
|
Right vagus, where hyperactivity predisposes to sinus bradyarrhythmias (slow)
|
|
|
AV node gets parasympathetic innervation from which nerve?
|
Left vagus, where hyperactivity predisposes to AV blocks
|
|
|
Esophagus sympathetic innervation, as well as head, neck, and arms?
|
T2-8
|
|
|
What organ is affected? Innervation: T5-T9. Viscerosomatic Reflex - T7 on Right or bilateral. Tend to exhibit non-neutral dysfunction. Anterior Chapman’s Reflex - Lateral to costal cartilage between 7th and 8th ribs on right. Posterior- Between transverse processes of T7-8 on the right.
|
Pancreas.
|
|
|
What organ is affected? T12 right with tenderness over tip of 12th rib right (anterior)
|
Appendix
|
|
|
What is articulation?
|
Taking a joint through full ROM
|
|
|
Lymphatic pump and MI, why should you do or not do this?
|
DO NOT DO IT!! It increases venous return (results in CHF, arrhythmias)
|
|
|
Reciprocal inhibition (indirect) is what type of technique?
|
ME, so is direct.
|
|
|
If biceps muscle in spasm, how would you perform Reciprocal inhibition (indirect)?
|
fully flex elbow, have pt contract triceps against resistance. Isometric force allows biceps muscle to relax & return to resting state
|
|
|
If biceps muscle in spasm, how would you perform Reciprocal inhibition (direct)?
|
fully extend elbow, have pt contract his triceps against resistance. Isometric force allows biceps muscle to relax and return to resting state
|
|
|
Crossed extensor reflex is used when?
|
Uses the crossed extensor reflex to achieve muscle relaxation. Used in extremities so severely injured/not accessable to direct manipulation. Example: contraction of right biceps produces relaxation of left biceps and contraction of left triceps
|
|
|
Cervical Manipulation contraindication, Absolute or Relative?: Fractures
|
Absolute
|
|
|
Cervical Manipulation contraindication, Absolute or Relative?: Odontoid instability
|
Absolute
|
|
|
Cervical Manipulation contraindication, Absolute or Relative?: Bone malignancies or osteomyelitis
|
Absolute
|
|
|
Cervical Manipulation contraindication, Absolute or Relative?: Acute myelopathy
|
Absolute
|
|
|
Cervical Manipulation contraindication, Absolute or Relative?: Cauda Equina Syndrome
|
Absolute
|
|
|
Cervical Manipulation contraindication, Absolute or Relative?: Ligamentous instability
|
Absolute
|
|
|
Cervical Manipulation contraindication, Absolute or Relative?: Acute arthropathies
|
Absolute
|
|
|
Cervical Manipulation contraindication, Absolute or Relative?: Bruits auscultated over carotid arteries
|
Relative
|
|
|
Cervical Manipulation contraindication, Absolute or Relative?: Lens implant
|
Relative
|
|
|
Cervical Manipulation contraindication, Absolute or Relative?: Known neurological disease
|
Relative
|
|
|
Cervical Manipulation contraindication, Absolute or Relative?: Hemophiliacs
|
Relative
|
|
|
Cervical Manipulation contraindication, Absolute or Relative?: Osteoporosis
|
Relative
|
|
|
Cervical Manipulation contraindication, Absolute or Relative?: Medicolegal situations
|
Relative
|
|
|
Cervical Manipulation contraindication, Absolute or Relative?: Acute strains
|
Relative
|
|
|
Cervical Manipulation contraindication, Absolute or Relative?: Rheumatoid arthritis
|
Relative
|
|
|
Area of tissue ___ times more tender than surrounding area
|
Four
|
|
|
Intrafusal fibers (muscle spindles) prevent muscles from being torn, and are innervated by what?
|
Type 1a, 2, and gamma neurons
|
|
|
which type of neuron would detect how fast it was stretching?
|
1a of the intrafusal fiber.
|
|
|
which type of neuron would detect how far it is stretched?
|
type 2 of the intrafusal fiber
|
|
|
which type of neuron is the regulator for the muscle tone of the extrafusal fiber?
|
"gamma neuron. by changing the sensitivity of the Type Ia & II fibers to stretch
|
|
|
posterior cervical C1 tender point location?
|
located low on occiput, approximately 2 cm lateral to muscle mass at back of neck
|
|
|
what is the first cervical vertebrae of the articular pillar?
|
c2
|
|
|
where are the posterior tenderpoints for C2-C7?
|
located on spinous process of vertebrae and laterally in paravertebral muscle masses (articular pillars)
|
|
|
Where is the anterior cervical tenderpoint for C1?
|
Posterior edge of the ascending mandible
|
|
|
Where is the anterior cervical tenderpoint for C2 and C3?
|
appears on the SCM
|
|
|
Where is the anterior cervical tenderpoint for C4-C6?
|
appears anterior to the SCM
|
|
|
Where is the anterior cervical tenderpoint for C7?
|
lateral attachment of SCM to clavicle
|
|
|
Where is the anterior cervical tenderpoint for C8?
|
medial tip of clavicle
|
|
|
Posterior C3 tender point treatment?
|
Flex & STRAw
|
|
|
All cervical posterior tender points (except inion & C3) are treated in which position?
|
Extend and SARA
|
|
|
Inion tender point treatment?
|
Flex
|
|
|
Anterior C7 tender point treatment?
|
Flex & STRAw
|
|
|
All anterior cervical tender points except C1 and C7 are treated in which position?
|
Flex & SARA
|
|
|
C1 anterior tender point treatment?
|
Rotate Away
|
|
|
For the counterstrain tenderpoints, anterior C2-C8, but not C7, what do you do?
|
Flex and SARA, (c1 rotate away, C7 flex and STRAW)
|
|
|
For the counterstrain tenderpoints, anterior C1, what do you do?
|
c1 rotate away, (C2-C8, flex and SARA, except C7 flex and STRAW)
|
|
|
For the counterstrain tenderpoints, anterior C7, what do you do?
|
C7 flex and STRAP. (c1 rotate away, the rest of C2-C8 Flex and SARA)
|
|
|
For the counterstrain tenderpoints, posterior C1, what do you do?
|
Inion flex. (C2-C7 extend and SARA, except C3 Flex and Straw).
|
|
|
For the counterstrain tenderpoints, posterior C2-C7, but not C3, what do you do?
|
C2-C7 extend and SARA, except C3 Flex and Straw, (C1 inion flex)
|
|
|
For the counterstrain tenderpoints, posterior C3, what do you do?
|
Flex and Straw. (The rest of C2-C7 extend and SARA, C1 inion flex)
|
|
|
What is FPR for C0 F Sr Rl?
|
Indirect technique. 1. Pt Supine, Physician at Head of table 2. Doc monitors the sulcus on the left (it will feel shallow) 3. Bring cervical spine to neutral position (no Lordosis) 4. ADD COMPRESSIVE FORCE and maintain 5. Flex until you feel motion at C0 6. Sidebend Right and Rotate Left until you feel motion at C0 7. Hold for 4-5 seconds 8. Slowly return to neutral, release compression and recheck
|
|
|
If you SB C2 on the left, which pillar is more prominent posteriorly? Laterally?
|
The left pillar. (sticking out). Which pillar is more prominent laterally? The right side, (its stretched out, convex, and therefore more prominent than the other side).
|
|
|
temporal bone has muscular ties to the cervical region, dysfunction in either area can affect other, benign cervical ____ is common. Caused by a cervical spasm causing temporal bone asymmetry and therefore vestibular asymmetry.
|
vertigo
|
|
|
Petrous portion of the skull carries which cranial nerves?
|
7 and 8.
|
|
|
patients with cervical root problems experience “shoulder” pain when in what position?
|
supine, extension of neck exacerbates symptoms
|
|
|
The “most important” or most clinically significant somatic dysfunction which should be addressed in all newborns is what? And what does it cause?
|
occipital condylar compression. Treatment includes suboccipital (OA) release is great in newborns. Affecting cranial nerves 9, 10, & 11; it can be the cause of poor suck, swallowing difficulties, emesis, hiccups, congenital torticollis, and perhaps pyloric stenosis.
|
|
|
Whats the sympathetic level for the spleen?
|
T5-T9
|
|
|
what degree ATR angle requires radiographic evaluation to determine Cobb Angle? (Usually correlates to 10 – 120 Cobb Angle) and follow-up screening in 6 months.
|
5 degrees
|
|
|
what degreee or greater ATR angle requires referral to a scoliosis specialist (Usually correlates to >200 Cobb Angle)
|
7 degrees
|
|
|
gait cycle is equal to how many strides and how many steps?
|
1 stride, 2 steps.
|
|
|
width of stride is approx how many inches?
|
2 to 4 inches
|
|
|
length of step is an average of how many inches?
|
15 inches. (a stride is therefore 30 inches.)
|
|
|
Foot angle is normally how many degrees?
|
20-25 degrees
|
|
|
gait cadence is normally how many steps pr minute?
|
90-120 steps per min
|
|
|
What is the difference between swing and stance phase?
|
swing phase is toe off to heel strike, accounts for 40% of gait cycle. The other 60% is stance phase and is heel strike to toe off.
|
|
|
A cane should normally be carried in the (same or opposite?) hand from your injured leg.
|
opposite
|
|
|
What is the FPR treatment for someone C2 Rr?
|
FPR is an indirect technique using compression. 3 steps. First, bring to neutral. Next, add compression. Last, bring them the way they like to go, in this case, rotate right for 3-5 seconds until it releases. Loading the joing causes tissues to relax.
|
|
|
What is the FPR treatment for someone C4 E Sr Rr?
|
Pt Supine, Physician at Head of table. Doc monitors the articular pillar (transverse process) at C4. Bring cervical spine to neutral position (no Lordosis). ADD COMPRESSIVE FORCE and maintain. Extend until you feel motion at C4. Sidebend and Rotate Right until you feel motion at C4. Hold for 4-5 seconds. Slowly return to neutral, release compression and recheck.
|
|
|
what is ART?
|
Low velocity/Moderate to high amplitude. A technique in which an articulation is taken through it’s full range of motion with specific attention directed at the dysfunctional barrier(s). The therapeutic goal is increased freedom of articular motion
|
|
|
what is springing?
|
Low to medium velocity/Moderate amplitude. A technique in which the restrictive barrier is engaged repeatedly to produce an increased freedom of motion. The therapeutic goal is increased freedom of articular motion
|
|
|
What is the Still technique?
|
first engage with a indirect force, (away from the restrictive barrier. (for instance, in a pronated forearm, further pronate AND push the radial head further posterior.) then reverse the movement and engage the restrictive barrier. In the previous example, now supinate the forearm and push the radial head anteriorly.
|

