![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
164 Cards in this Set
- Front
- Back
|
A 35 yo female with chronic back pain has tenderness at the superior aspect of both posterior superior iliac spines that reproduces her pain. Which chronic back pain syndrome does she most likely have?
|
iliolumbar ligament syndrome
**bilateral UPL5 tender points** |
|
|
A 28 year old male with chronic back pain has reproduction of his pain with the ASIS compression test. What does he most likely have?
|
Sacroiliitis
**ASIS compression worsens, diffuse SI tenderness** |
|
|
A 42 yo female with chronic back pain has tendrness medial to both ASIS's that reproduce her back pain. Hip extension is NOT restricted. Which chronic back pain syndrome does she most likely have?
|
Pelvic Pain
**anterior pelvic tender points** |
|
|
A 16 year old male patient exhibits sacrococcygeal tenderness. A structural exam reveals coccyx flexion. What low back pain syndrome does this patient have?
|
Coccydynia
**sacrococcygeal tenderness, coccyx flexion** |
|
|
Head and Neck
Sympathetic: Parasympathetic: |
Sympathetic: T1-4
Parasympathetic: Vagus |
|
|
Cardiovascular
Sympathetic: Parasympathetic: |
Sympathetic: T1-5
Parasympathetic: Vagus |
|
|
Respiratory
Sympathetic: Parasympathetic: |
Sympathetic: T2-7
Parasympathetic: Vagus |
|
|
Stomach, liver, gallbladder
Sympathetic: Parasympathetic: |
Sympathetic: T5-9
Parasympathetic: Vagus |
|
|
Small Intestine
Sympathetic: Parasympathetic: |
Sympathetic: T9-11
Parasympathetic: Vagus |
|
|
Ovary, Testicle
Sympathetic: Parasympathetic: |
Sympathetic: T9-T10
Parasympathetic: S2-4 |
|
|
Kidney, Ureter, Bladder
Sympathetic: Parasympathetic: |
Sympathetic: T10-L1
Parasympathetic: S2-4 |
|
|
Large Intestine
Sympathetic: Parasympathetic: |
Sympathetic: T8-L2
Parasympathetic: Vagus & S2-4 |
|
|
Uterus
Sympathetic: Parasympathetic: |
Sympathetic: T10-L1
Parasympathetic: S2-4 |
|
|
Prostate
Sympathetic: Parasympathetic: |
Sympathetic: L1-2
Parasympathetic: S2-4 |
|
|
Patient presents with pelvic pain. R ASIS is inferior. R PSIS is superior
|
R Anterior Innominate
|
|
|
Patient presents with pelvic pain. L ASIS is superior. L PSIS is inferior
|
L Posterior Innominate
|
|
|
Patient presents with pelvic pain. R ASIS is superior. R PSIS is superior
|
R Superior Innominate Shear
|
|
|
Patient presents with pelvic pain. L ASIS is inferior. L PSIS is inferior
|
L Inferior Innominate Shear
|
|
|
Patient presents with pelvic pain. R ASIS is medial. R PSIS is lateral
|
R Innominate Inflare
|
|
|
Patient presents with pelvic pain. L ASIS is lateral. L PSIS is medial
|
Innominate Outflare
|
|
|
Patient has a left short leg, what
direction is the pelvic side shift? Lumbar concavity is likely toward what direction? |
Pelvic side-shift and rotation
toward side of long leg. (Right Leg) In the lumbar spine the convexity points towards the short leg and the concavity towards the long leg. (Concavity toward R leg) |
|
|
In Short Leg syndrome:
What side does the pelvis shift to? |
Pelvic side-shift and rotation
toward side of long leg. |
|
|
In Short Leg syndrome:
Concavity of L-spine = ? Convexity of L-spine = ? |
convexity points towards the short leg
the concavity towards the long leg. |
|
|
What ligament is often first to react to Short Leg?
|
Iliolumbar lig. on side of
convexity (short leg) is often the 1st to react • Referred pain: – Ipsilateral groin and hip |
|
|
Sciatic nerve may pierce through this muscle and cause sciatica type symptoms
|
Piriformis m.
(Externally rotates femur) |
|
|
Posititve Standing flexion test and ASIS compression test both indicate what?
|
Side of Restriction
|
|
|
Associated Clinical Findings:
-Ipsilateral tight hamstrings, tight iliolumbar ligament. May be accompanied by symptoms of sciatica (piriformis dysfunction) |
Associated with Anterior Innominate
|
|
|
Clinical Associations:
Usually Caused by trauma. Pt may complain of pelvic pain. |
Superior Iliac Shear
|
|
|
Clinical Associations:
Can be caused by tripping (imagine beingtackled by foot). It is fairly rare- Walking often reduces dysfunction |
Inferior Innominate Shear
|
|
|
_______ means that the probability and magnitude of harm or discomfort anticipated in the research are not greater in and of themselves than those ordinarily encountered in daily life
|
Minimal Risk
|
|
|
Study designed to obtain data that will occur in the FUTURE
|
Prospective Study
|
|
|
- Study has a COMPARISON GROUP, which does not receive the intervention
- Control Group |
Placebo Controlled
|
|
|
- Subject Group(s) assignment is determined with a random process
|
• Randomized Human Clinical Trial
|
|
|
subjects, drug givers & data
gatherers not aware of who is in the treatment or control group. |
Double Blind Study
|
|
|
Name some conditions for which a psychosomatic etiology is common (3)
|
**Chronic Pain Syndromes**
- Chronic Migraine, Fibromyalgia, Neck Pain **ANS- Related Disorders** - IBS, Interstitial Cystitis, Orthostatic Tachy **Neurologic Syndromes** - Insomnia, Tinnitus, Fatigue, Parathesia |
|
|
Develop osteopathic manipulative treatment for psychosomatically correlated conditions
|
Fuck this...The only real time he mentioned anything was in a table...
- Thoracic OMT - cranial balancing - relaxation breathing |
|
|
Cardiac related tissue
texture changes & somatic dysfunction typically involve: |
upper thoracic region
OA, AA C2 and C6 |
|
|
Chapman’s points for heart:
|
• Medial second
intercostal spaces • Transverse process T2 |
|
|
Restriction in thorax, spine, diaphragms has significant ramifications in patients with CHF.
|
***KNOW THIS ***
|
|
|
OMT Goals for pt's with cardiovascular disease?
|
- ↓ cardiac load of the heart
- ↑ O2 supply to myocardium - ↓ local myofascial tension -Alleviate restriction in thoracic cage, thoracic inlet, abdominal and pelvic diaphragm (optimizes circulatory return to the heart) -Minimizes any facilitated segments to normalize sympathetic tone |
|
|
Explain how respiratory muscles effect CV performance
|
**Inspiration**
-Creates pressure gradient to draw blood, lymph into chest and air into lungs Squeezes viscera and moves fluid toward the chest **Expiration** Rib cage recoils, diaphragm relaxes, ↓ thoracic diameter Compresses lungs--> forces air out Fluid is drawn from periphery (veins and lymph channels) |
|
|
• Simultaneous appearance of:
– Carpal tunnel syndrome – Thoracic outlet syndrome • Compression of a nerve at one point renders it more susceptible to damage at another site. • Altered function is greater than the sum of the impairment caused by individual lesions. (1+1=3) **EXAM** |
DOUBLE CRUSH SYNDROME
|
|
|
OMT - Three Phase Treatment for Carpal Tunnel
|
Phase 1 - release of transverse carpal ligament
Phase 2 - Opponens roll Phase 3 - wrist extension to pull flexor tendons into carpal tunnel |
|
|
Classical symptoms include:
– Intermittent tingling with nocturnal arm/hand pain in thumb, index, and middle fingers – Thenar atrophy (muscle wasting) with loss of thumb dexterity – Proximal arm/shoulder pain – Frequently bilateral with greater severity in the dominant hand |
Carpal Tunnel Syndrome
|
|
|
What forms the Carpal Tunnel?
|
STOP + Flexor Retinaculum
Scaphoid Trapezium hook Of hamate Pisiform |
|
|
Less compression on the median nerve at the carpal tunnel is required to produce symptoms when a proximal lesion is present.
|
DOUBLE CRUSH SYNDROME
|
|
|
Altered structure of the carpal tunnel leads to altered function of the _____ nerve.
|
MEDIAN NERVE
|
|
|
Describe home stretching excercises for carpal tunnel patients
|
Wrist and digits are simultaneously hyperextended.
• Thumb is hyperextended, hyperabducted and laterally rotated. |
|
|
What hospital tests can confirm carpal tunnel syndrome?
|
-EMG/ NCS
-US |
|
|
Carpal Tunnel causes:
MEDIAN TRAP |
M- Myxoedema
E- Edema Premenstrually D- Diabetes I- Idiopathic A- Acromegaly N- Neoplasm T- Trauma R- Rheumatoid Arthritis A- Amyloidosis P- Pregnancy |
|
|
Headache with numbness or tingling
of scalp – Pain and paresthesias limited to one side of the head. • May be brief, sharp lancinating pain in distribution of nerve, usually lasting several seconds • May also be continuous aching or hyperesthesia in distribution of relevant nerve. • “Hurts to brush hair” |
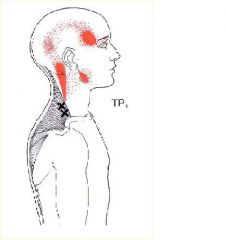
Occipital Neuralgia
**EXAM** |
|
|
Patient says it hurts to brush hair. Tinel's Sign Worsen's headache. Problem and where do you focus tx?
|
Occipital Neuralgia
Focus Tx on: -OA -AA Sub-occipital triangle |
|
|
You should Avoid direct action OMT of upper cervical in patients with what disorders?
|
- rheumatologic disorders
(especially RA) - Down’s syndrome. **Weakened Cruciate and Odontoid ligaments** |
|
|
This is a Connective tissue bridge between posterior
atlanto-occipital membrane (dura) and rectus capitis posterior minor (atlas to occiput). |
Myodural Bridge
Tx with suboccipital release |
|
|
When to order tests for head pain?
|
• Focal or sudden onset of
neurological symptoms or signs. • Progressive headaches • Symptoms of increasing intracranial pressure. |
|
|
Young adult who thinks he has
“the flu”: • headache, hoarseness, vomiting and difficulty swallowing. Physical exam • Afebrile, Oropharyngeal exam normal, • Cranial merve exam yields decreased gag reflex. Order MRI • Cerebellum portion of brain protruding into spinal canal |
Arnold Chiari Malformation
|
|
|
Order MRI
• Cerebellum portion of brain protruding into spinal canal |
Arnold Chiari Malformation
|
|
|
Red Flags for headaches?
**EXAM** |
Sudden, Severe Headaches
• Neck Stiffness and fever • Association with head injury • “First or worst” headache in one’s life • Visual Changes • Headaches accompanied by neurological or personality changes • Recurrent localized headaches • Recurrent high intensity or frequency • Change in nature or frequency of headaches |
|
|
• Overweight, young women with headache, nausea, and vomiting
– Symptoms may be caused by elevated CSF pressure! Problem? Clinical Exam you NEED TO DO... |
Pseudotumor Cerebri
**Fundoscopic exam** look for papilledema, evidence of subarachnoid hemmorhage, optic neuritis |
|
|
-Primary motion is
flexion and extension – 50 % of cervical flexion and extension occurs here – When sidebending is introduced, rotation will occur in OPPOSITE direction (SLRR) |
OA (C0-1)
|
|
|
Primary motion is rotation
• 50 % of cervical rotation occurs at this cervical segment |
AA (C1-2)
|
|
|
How should you tx an OA Flexed somatic dysfunction?
|
Treat OA flexion S/D in neutral,
not extension -decrease risk of vertebral artery compromise |
|
|
Explain active motion testing to diagnose OA somatic dysfunction
|
-Flex then SB and R
–Extend then SB and R |
|
|
• Usually bilateral
• tightening or vice-like gripping • “A band of pain from my forehead to the base of my skull.” • Radiation into trapezius muscle and posterior neck • Intensity is rated as mild to moderate • Usually lasts greater than 30 minutes • Not provoked by low level activity • Migraine symptoms are usually absent |
Tension Headaches
|
|
|
Episodic- usually 1-2
times/month • Unilateral • Prodrome is common • Aura (classic) • Lasts 4-72 hours • Pulsating, Throbbing (50%), Dull, ache type (50%) • More common in females • Often relieved by sleep. |
This is a migraine headache
|
|
|
This type of headache may be accompanied with:
• Nausea* • Vomiting* • Photophobia* • Phonophobia* • Unable to perform usual daily tasks* |
Migraine
|
|
|
_____ is considered the main cause of migraine headaches.
|
**Vascular Tone**
trigger ↓ release of serotonin and NE ↓ Vascular DILATION ↓ Stimulates TRIGEMINAL SYSTEM ↓ Stimulates spinal cord ↓ tightness of mm. in back of head and neck |
|
|
What should be done for EVERY headache patient?
|
Do the cranial nerve exam for every headache patient and do it well.
|
|
|
Median nerve origination: ?
|
from C6, C7, and C8 and T1 nerve roots
i. C6 and C7 supply sensory info to the hand ii. C8 and T1 supply median motor fibers that innervate distal median muscles of forearm and hand **Median nerve controls FLEXORS!!!** |
|
|
Congestion can cause temporalis tension. What nerve facilitates this?
|
Trigeminal Nerve!!
**V3** |
|
|
Increased cervical lordosis can cause _________
|
**Mouth Breathing**
-Decreased air filtering -Hypoventilation -Nasopharyngeal Stasis |
|
|
A patient with frequent upper respiratory infections presents with a congestion headache. Upper cervical OMT will stimulate what nerve to produce watery mucous and help alleviate congestion?
|
Upper cervical treatment stimulates the vagus nerve producing watery mucous
|
|
|
A patient with frequent upper respiratory infections presents with a congestion headache. What are some common upper cervical somatic dysfunctions that can be treated to help this patient?
|
Sub-occipital Tension
OA restriction AA restriction Treating these areas may stimulate the VAGUS nerve and make WATERY MUCOUS |
|
|
Congestion can affect what levels of the thoracic spine?
|
T1-4
Upper thoracic treatment can reduce facilitation to thin nasal secretions |
|
|
Name 2 treatments that can promote lymphatic drainage from the head
|
Submandibular Effleurage
Thoracic Pump |
|
|
Trigeminal stimulation triggers _____
mucous |
watery mucous
|
|
|
What are they key areas to check for somatic dysfunction in a patient with congestion headache?
|
T1-5
thoracic inlet upper cervical temporalis |
|
|
Chapman's points for respiratory system?
|
T3-4 transverse processes
3rd and 4th intercostal spaces |
|
|
Restriction in what 2 areas may lead to shortness of breath?
|
Structural factors
– Rib restriction – Diaphragm tension |
|
|
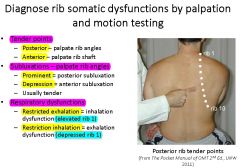
Know this rib Dx stuff
|
|
|
|
Should you perform thoracic pump on a COPD patient?
|
No, it's contraindicated...
Thoracic pump rebound can worsen aspiration and COPD Also, avoid it in patients with: -pulmonary embolism -CHF -unstable arrythmia |
|
|
An 88 yo female is admitted to the hospital with cough and shortness of breath for one week. Decreased breath sounds, and crackles are heard in the lower right lobe. CXR shows right lower lobe consolidation. Which is the most appropriate OMT protocol during her hospitalization?
A) Thoracic soft tissue and rib raising 2x a day B) Thoracic Pump 4x a day C) Thoracic & rib counterstrain, MF release, ME and articulatory daily D) Compression of the 4th ventricle E) Thoracic and rib thrust every other day? |
A) Thoracic soft tissue and rib raising 2x a day
|
|
|
An 88 yo female is admitted to the hospital with cough and shortness of breath for one week. Decreased breath sounds, and crackles are heard in the lower right lobe. CXR shows right lower lobe consolidation. Which structural exam findings would be present with ACUTE somatic dysfunction?
A) blanching B) coolness C) dryness D) edema E) ropiness |
D) Edema
(ropiness, dryness, coolness and blanching are found in CHRONIC somatic dysfxn) |
|
|
An 88 yo female is admitted to the hospital with cough and shortness of breath for one week. Decreased breath sounds, and crackles are heard in the lower right lobe. CXR shows right lower lobe consolidation. Which manipulative treatment would normalize sympathetic tone to her lungs?
A) rib raising B) sacral rocking C) subocciptal inhibition D) superior mesenteric ganglion inhibition E) thoracolumbar inhibition |
A) rib raising
|
|
|
An 88 yo female is admitted to the hospital with cough and shortness of breath for one week. Decreased breath sounds, and crackles are heard in the lower right lobe. CXR shows right lower lobe consolidation. At which vertebral levels would you expect to find somatic dysfunction?
A) C1-2 B) T4-5 C) T10-11 D) L1-2 E) L5-S1 |
B) T4-5
|
|
|
A 55 yo female has had nasal congestion and facial pain for two weeks. Which somatic dysfunction would be most related to difficulty breathing through her nose?
A) increased cervical lordosis B) T2 ESR left C) Suboccipital tension D) thoracic inlet restriction E) first rib restriction |
A) increased cervical lordosis
|
|
|
A 55 yo female has had nasal congestion and facial pain for two weeks. Which of the following general manipulative treatments is recommended as part of her tx?
A) venous sinous drainage B) upper extremity effleurage C) rib raising D) thoracic pump E) diaphragm myofacial release |
D) thoracic pump
|
|
|
A 55 yo female has had nasal congestion and facial pain for two weeks. Which of the following structural exam components is most pertinent for her evaluation?
A) thoracic outlet/diaphragm rotation B) typical rib motion testing C) upper thoracic palpation D) posterior axillary fold tenderness E) tempomandibular motion |
C) upper thoracic palpation
|
|
|
Excessive sympathetic activity would be expected to lead to which of the following?
A) vasodilation and thick nasal secretions B) vasodilation and thin nasal secretions C) vasospasm and thick nasal secretions D) vasospasm and thin nasal secretions E) rhinorrhea and vasomotor instability |
C) vasospasm and thick nasal secretions
|
|
|
What does a positive spring test indicate?
|
sacral extensions or backward torsions
|
|
|
Increased sacral base asymmetry in backwards bending test indicates what?
|
sacral extensions
or backward torsions |
|
|
How does the sacrum move during respiration?
|
– Inhale-spine elongates →sacral base posterior (EXTENSION)
– Exhale- spine recoils →sacral base anterior (FLEXION) |
|
|
What is the movement in the sacrum like during a right heel strike?
|
– Left rotation on left axis
– Lumbar spine sidebends to the left |
|
|
What is the movement in the sacrum like during a left heel strike?
|
– R rotation on R axis
– Lumbar spine sidebends to the R |
|
|
If L5 is sidebent to one side, a
sacral oblique axis is typically engaged on the ____ side **EXAM** |
SAME side
|
|
|
If L5 is rotated, sacrum rotates
the _______direction on oblique axis (torsion). **EXAM** |
OPPOSITE direction
|
|
|
make sure to do Krib's powerpoint questions for the Sacrum
|
do it...
|
|
|
- an acute or chronic painful condition of muscles and their related structures characterized by the presence of myofascial TRIGGER POINTS
• A more general meaning includes a REGIONAL muscle pain syndrome of any soft tissue origin that is associated with muscle tenderness |
Myofascial Pain Syndrome
|
|
|
A _____ is usually an exquisitely tender nodule in the taunt band of skeletal muscle
|
Trigger Point
**The presence of a local twitch response confirms the presence of a trigger point** |
|
|
The presence of a _____ confirms the presence of a trigger point
|
local twitch response
|
|
|
Know that trigger points can be mapped from person to person because they are the same from person to person
|
he might ask that...
|
|
|
- a transient contraction of those muscle fibers in the taunt band that are associated with the trigger point
- It can be elicited by a “snapping palpation” perpendicular to the muscle fibers |
local twitch response
|
|
|
What's the difference between active and latent trigger points?
|
Active trigger points - produce a clinical complaint (usually pain) which the patient recognizes when the trigger point is digitally compressed (it reproduces their symptoms)
• Latent trigger points - can produce other effects characteristic of a trigger point including increased muscle tension and muscle shortening (but do not produce spontaneous pain) **active TP=spontaneous pain at any time **Latent TP= produce pain only when probed |
|
|
What are some of the differences between trigger points and counterstrain tender points?
|
**Trigger Points**
- Regional!!! - Treated by STRETCHING the muscle **Counterstrain Tender Points** - ***Locally*** tender - Do not typically refer the pain beyond the area being compressed - Treated by SHORTENING the muscle |
|
|
This trigger point can activate one or more satellite points.
Inactivation of this point can also inactivate satellite trigger points |
Key trigger point
**Target the key trigger point w/ treatment** |
|
|
No matter what modality you
use to treat trigger points, an essential component in the treatment is _________ |
HOME STRETCHES
|
|
|
What is the hypothetical physiologic cause of trigger points?
|
There is an abnormal ↑ in production and release of ACh from motor nerve terminals this depolarizes the membrane and causes Ca to leak out.
- this creates a sustained shortening (contracting) of the sarcomere |
|
|
What are some of the differences between Myofascial Pain Syndrome and Fibromyalgia?
|
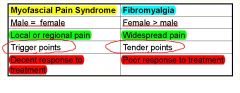
|
|
|
The Histochemical environment surrounding trigger points are strongly _____ and full of noxious chemicals
|
ACIDIC
|
|
|
What are some factors that perpetuate myofascial pain syndrome?
(reactivate trigger points) |
The only two he made a big deal about were:
HYPOTHYROIDISM ALLERGIC RHINITIS |
|
|
OMT for trigger points?
|
ME
MFR **THESE STRETCH THE MUSCLE*** |
|
|
Spray and stretch uses a vapocoolant
spray followed by a stretch to deactivate a trigger point.. What is the essential part of this treatment? |
THE STRETCH
|
|
|
What's the difference in results between injection and dry needling (accupuncture) for trigger points?
|
Dry needling (acupuncture) is just as effective as injection; there may be more soreness afterwards
|
|
|
What are the least and most myotoxic agents for trigger point injection?
|
- Procaine and lidocaine are the least myotoxic
- Bupivacaine (Marcaine) is the most myotoxic |
|
|
Muscle most often found to have trigger points?
|
Trapezius
|
|
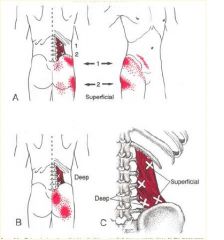
• Easily mistaken for lumbar
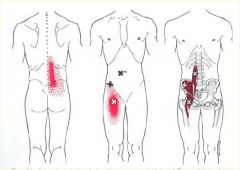
radicular pain (coughing or sneezing may increase the pain) or piriformis syndrome • 2 superficial and 2 deep trigger points • Activation: 1) simultaneous bending over and reaching to one side to pull or lift 2) trauma • Perpetuation: short leg, small hemipelvis, short upper arms, a soft bed with a hammock like sag, leaning forward with poor elbow support over a desk, and weak abdominal muscles |
Quadratus Lumborum
"Joker of Low Back Pain" |
|
|
OMT for trigger point directed to the quadratus lumborum muscle
|
Muscle energy to the 11-12th ribs
|
|
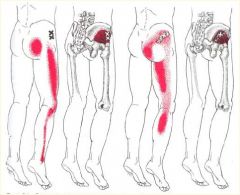
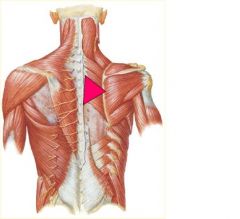
What's this Trigger Point?
|
***Gluteus Minimus***
- Pain is often attributed “ Pseudo-sciatica”to “sciatica” • The more anterior the trigger point, the more lateral the referral zone • Activation: acute or repetitive overload (walking too far or too fast), SI joint dysfunctions, nerve root irritation • Perpetuation: prolonged immobility (esp. driving a car), SI joint dysfunctions, sitting on a wallet placed in a back • Corrective exercises: have pt roll over a tennis ball in the area of the trigger point; sleeping on side with thighs flexed and pillow between knees |
|
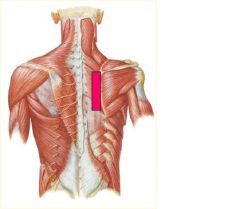
Trigger Point?
|
***Iliopsoas m.***
- It serves many important functions but Travell considered it as relatively inaccessible • Symptoms are aggravated by weight bearing activities and relieved by recumbency • Activation: prolonged sitting with the hips flexed • Perpetuation: short leg, small hemipelvis, repetitive vigorous contractions (situps) • Correction of somatic dysfunctions of the thoracic, lumbar, or sacral areas and avoid prolonged sitting |
|
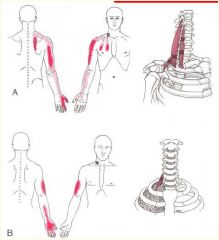
Trigger Point
|
**Scalene Muscles***
- Common source of back, shoulder, and arm pain • Often confused with cervical radiculopathy • Symptoms include myofascial pain or secondary sensory and motor disturbance due to neurovascular entrapment • Activation: pulling, lifting, tugging with the arms or overuse of these muscles in respiration • Perpetuation: tilted shoulder girdle axis • Corrective exercises: neck stretches or coordinated respiration (piston breathing) |
|
|
OMT for Scalene trigger points?
|
OMT should directly address
the scalene muscles • Cervical kneading – p. 203 • Cervical stretching – p. 204 • Scalene ligamentous articular strain –p. 205 • Scalene stretch – p. 206 • Cervical long restrictor muscle energy – p. 216 • Cervical sidebending or rotational ME/HVLA |
|
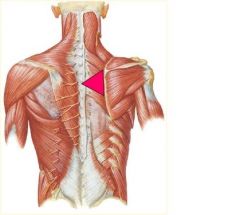
Trigger Point?
|
**Trapezius m.**
- Muscle most often found to have trigger points • Frequently overlooked source of temporal and cervicogenic headache • Activation: commonly results from the stress of sustained elevation of the shoulders and trauma • Corrective exercises: trapezius tension release exercises • OMT would be very similar to those for the scalenes |
|
|
History of WIDESPREAD PAIN - pain is considered widespread when all of the following are present:
- Pain in the right and left side of the body*** - Pain above and below the waist*** - In addition, AXIAL SKELETAL PAIN (cervical spine, anterior chest, thoracic spine, or low back) must be present. **THIS IS ON THE EXAM** |
Criteria for Fibromyalgia Dx
(American College of Rheumatology) |
|
|
What is the cornerstone of fibromyalgia treatment?
|
****Exercise is the cornerstone of Treatment****
|
|
|
American College of Rheumatology requires Pain on digital palpation of 11-18 of the following tender points for Dx of Fibromyalgia:
|
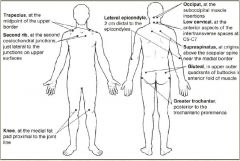
|
|
|
FEMALE patient presents with:
- Pain lasts much longer into the day (compared to RA) - Bialteral Tender Points - Fatigue--> may be debilitating - Depression-->d/t chronic pain |
Fibromyalgia
|
|
|
Treatment recommendations for fibromyalgia?
|
First recommendations = exercise and NO ASPIRIN (b/c it is not inflammatory process)
|
|
|
60% of delta wave time is interrupted by alpha type sleep in _____ patients
|
Fibromyalgia
**Poor sleep predicts pain the next day** |
|
|
What must you always rule out before making a diagnosis of fibromyalgia?
|
**OCCULT MALIGNANCY**
|
|
|
OMT for Fibromyalgia?
|
• Patients respond best to gentle indirect OMT
• MFR → Treat Transverse Diaphragm restrictions first THEN Longitudinal Fascial Restrictions |
|
|
Burning pain in the upper or lower extremities associated with:
– Swelling – Decreased range of motion – Vasomotor instability – Trophic skin changes – Patchy bone demineralization |
**Reflex Sympathetic Dystrophy**
|
|
|
- Continuing pain, allodynia or hyperalgesia; pain is disproportionate to the inciting event
- Abnormal sweating in the affected region (sweat a lot) |
**Reflex Sympathetic Dystrophy**
|
|
|
What's the big deal about stage III RSD?
|
Stage III is IRREVERSIBLE!
|
|
|
What is the best tx for RSD?
|
PREVENTION!!
Aggressively treat somatic dysfxn |
|
|
What's so special about neural blockade in a pt. with RSD?
|
**Neural blockade - diagnostic and therapeutic**
(Stellate ganglion block or Epidural block) |
|
|
Garlitz, Lecture 14...
Know slides 17-22 |
THIS WILL BE ON THE EXAM
|
|
|
Where does nerve C5 exit the cervical spine?
|
between C4 & C5
Cervical nerve roots exit above the vertebral body that bears its name |
|
|
How can a pateint's posture cause neck pain?
|
Forward Head Carriage puts a lot of stress on the cervical spine
|
|
|
Should you diagnose a cervical radiculopathy with a CT or MRI?
|
**Never should the diagnosis be made merely upon CT or MRI interpretation**
Use your H&P!!! |
|
|
When should surgery be done to treat dengenerative cervical discs?
|
Surgery if:
– Intractable pain – Progressive neurological impairments |
|
|
Thoracic outlet syndrome consists of pain and parathesia in the upper extremity due to compression of the _________
|
brachial plexus
|
|
|
Which portion of the brachial plexus does Thoracic Outlet Syndrome affect?
|
Usually involves lower brachial plexus.
– C8-T1, Ulnar nerve distribution |
|
|
What type of tumor should be ruled out when diagnosing thoracic outlet syndrome?
*** |
Pancoast Tumor
|
|
|
What test has been noted to be highly sensitive for thoracic outlet syndrome?
|
elevated arm stress test
|
|
|
What creates optimum success of double crush syndrome treatment?
****** |
Treatment must be directed at both lesions for optimum results
|
|
|
When observing gait, normal least motion should be around what spinal level?
|
L3
this is going to be the ONLY fucking card from the Gait Lecture... Have fun with that.. |
|
|
The sicker the patient, the less time spent treating the patient, but the treatment is more _______
|
frequent
|
|
|
- One thing + another = disease
- i.e. Pneumonia is caused by an infection - We are taught to think this way (everything is separate) |
Cause and Effect
|
|
|
- Different factors all contribute to the outcome of disease
- Need to change our train of thought to this perspective - i.e. Pneumonia results from a susceptibility to an infection • What is the susceptibility |
Holistic Logic
|
|
|
- Pediatric patients respond slowly/quickly
- Geriatric patients respond more slowly/quickly (to OMT) |
- Pediatric patients respond quickly
- Geriatric patients respond more slowly |
|
|
If a patient is receiving their first ever OPP treatment, what should you warn them about?
******** |
Soreness!
-They may be sore for 24-48 hours! -This pain is DIFFERENT than the pain caused by their somatic dysfunction. (more of like pain after you work out) |
|
|
Should you see patients with chronic problems more often or less often for OMT?
|
More often = weekly/ 10 days
|
|
|
Pediactric patients respond best to ____ treatment (type of OMT tx)
|
direct technique
|
|
|
You should use ______ techniques for sicker or older or patients with acute injuries..
|
indirect techniques
|
|
|
***Stiles***
If the area of greatest resistance is in the upper nuchal ligament or if there is a horizontal noncontracting (rubbery) band of tightness over C1 and C2 a _____ restriction is suspected |
dural restriction
|
|
|
**STILES**
If the area of greatest resistance is in the upper cervical area or there is a horizontal, contracting band of tightness over C1 and C2 an ______ or ______ dysfunction is suspected |
OA or AA
|
|
|
**Stiles**
If a thoracic segment dysfunction is present, the restriction will be localized around 1 or 2 segments and will have a hard end-feel which will decrease as the clinician palpates ___________ |
Toward the rib
|
|
|
**Stiles**
If the key somatic dysfunction is in the upper extremity, the restriction will present as a unilateral, diffuse, vertical band of tightness ________ |
Medial to Scapula
|
|
|
**STILES**
If the key somatic dysfunction is in the ribs, the restriction worsens as you palpate ___________ |
laterally
|
|
|
**Stiles**
If the area of greatest resistance is below T12 do _____ and _____ |
Do a standing and seated flexion test
|
|
|
What's the difference between cervicogenic headaches and tension headaches?
|
Cervicogenic:
- UNILATERAL - Triggers: Neck Movement. Digital pressure over C1-3 facets Tension Headaches: - BILATERAL - Triggers: Stress, jaw clenching, TMJ Syndrome |
|
|
Define mind body medicine
**EXAM* |
An approach of medicine factoring in the relationship of psychological and physical dimensions of the person in health and illness
|
|
|
Who developed the psychosocial model:
-Physical/psychological/social component of any illness *COMEAUX* |
Engle
|
|
|
• Who developed empirical biomedical science?
*COMEAUX* |
Hopkins/Flexner
|

