![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
105 Cards in this Set
- Front
- Back
|
The most common causes of blindness in Australia are:
|
Aged-related Macular Degeneration (AMD)
Glaucoma Cataracts Diabetes Myopia |
|
|
Eye presentations to emergency departments and GP’s:
|
1. Visual loss
2. Red eye 3. Trauma 4. Foreign body 5. Chemical injury 6. Diplopia 7. Flashes and floaters |
|
|
Visual loss Hx
|
1. Timing
a. What were you doing? b. When did the problem start? c. Was the onset sudden or gradual? d. What has happened to vision since the problem began? e. Has this happened before? 2. Trauma/foreign body? 3. Unilateral or bilateral loss of vision? 4. Painful or painless eye(s)? 5. Red or white eye(s)? 6. Contact lens wear? Glasses (reading or distance or both)? 7. Prior eye surgery or laser? 8. Microvascular risk factors – DM? HT? Chol? Smoking? 9. Always ask about Giant Cell Arteritis – Headache? Jaw claudication? Stiffness in shoulders or hips (polymyalgia rheumatica)? Weight loss? Fevers/night sweats? |
|
|
Visual loss Examination
|
1. Visual acuity
2. Visual fields 3. Pupils 4. Red reflex (direct ophthalmoscope), try to view the fundus 5. Is the eye white or red? 6. Eye movements/ptosis 7. Slit lamp biomicroscope |
|
|
The ideal pupil-dilating agent for fundoscopy?
|
tropicamide 1%
|
|
|
Tropicamide pharmacology
|
antimuscarinic
|
|
|
Tropicamide actions
|
mydriasis
cycloplegia |
|
|
Tropicamide duration of effect
|
4–8 hours
|
|
|
Tropicamide onset of action
|
15-30 minutes
|
|
|
cycloplegic agents
|
usually antimuscarinics
atropine, cyclopentolate, homatropine, scopolamine, tropicamide |
|
|
Indications of cycloplegic drugs
|
- uveitis
- to paralyze the ciliary muscle in order to determine the true refractive error of the lens - with mydriatic effects for ophthalmic examination |
|
|
Define uveitis
|
inflammation of uvea (ciliary body, iris, choroid)
|
|
|
Classifications of uveitis
|
anterior
intermediate posterior panuveitis |
|
|
Anterior uveitis
|
anterior chamber & iris
(majority of cases) |
|
|
Intermediate uveitis
|
vitritis (inflammatory cells in the vitreous cavity)
|
|
|
Posterior uveitis
|
retina & choroid
|
|
|
Pan-uveitis
|
inflammation of all the layers of the uvea
|
|
|
commonly floaters are due to
|
degenerative changes of the vitreous humour
|
|
|
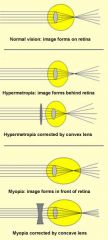
long sighted =
|
hyperopia
|
|
|
short sighted =
|
myopia
|
|
|
presbyopia
|
hardening of the lens associated with aging, resulting in loss of accomodation
bifocal lenses - top half concave for distance vision & bottom half convex for close-up vision |
|

|
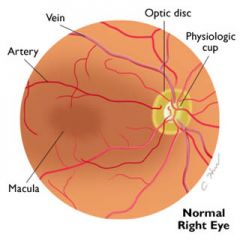
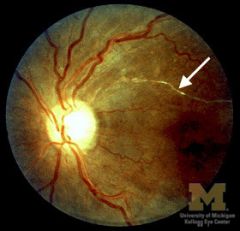
normal optic nerve
(central cup is small and the neuroretinal rim is thick) |
|

|
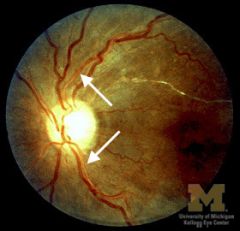
glaucomatous optic nerve is characterized by vertical elongation of the cup and a large notch inferiorly
|
|

|
Optic neuropathy in glaucoma may be characterized by significant loss of neuroretinal rim tissue
|
|

|
floaters
|
|
|
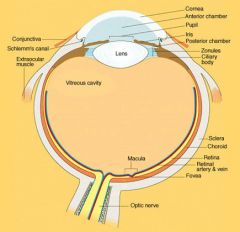
Describe the passage of aqueous humour
|
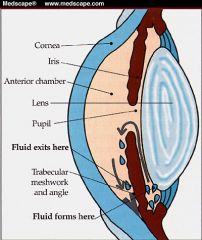
ciliary body → aqueous humor → pupil → anterior chamber → trabecular meshwork in angle of anterior chamber
|
|
|
Describe the image & lens relationship
|
|
|
|
|
|
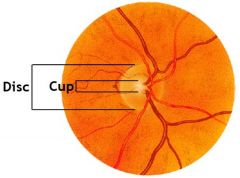
Normal disc/cup ratio?
|
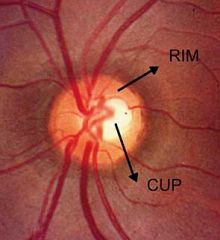
disc/cup ratio 0.3 or one third
|
|
|
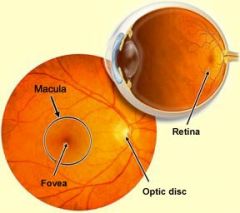
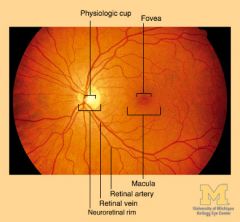
Define optic disc
|
AKA optic nerve head (physiological blind spot)
- where ganglion cell axons exit the eye to form the optic nerve - shaped like a doughnut with a pink neuroretinal rim and a central white depression called the physiologic cup |
|
|
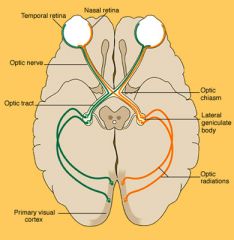
Parts of the optic nerve
|
Intraocular (the optic nerve head)
Intraorbital (between globe and optic canal) Intracanalicular (within the optic canal) Intracranial (between optic canal and chiasm) |
|
|
normal fundus
|
|
|
|
alternative to tropicamide in dilating for fundoscopic exam?
|
phenylephrine 2.5%
(modest dilation, delayed for 30 minutes) |
|
|
neuroretinal rim
|
carries the axons of the retinal ganglion cells
|
|
|
COLOUR of the neuroretinal rim?
|
normally orange-pink
If its axons die (inflammation, infarction, compression) the rim will turn white |
|
|
DISTINCT neuroretinal rim?
|
- Some fuzziness of the nasal margin is acceptable
- Otherwise swollen |
|
|
Causes of optic disc oedema?
|
↑ ICP
optic nerve inflammation & infarction |
|
|
Commonest cause of pathologic optic disc cupping
|
Glaucoma
|
|
|
Diameter of physiologic cup?
|
1/3
should not exceed 0.5 |
|
|
Where do the retinal arteries and veins emerge from?
|

retinal arteries and veins emerge from the nasal side of the optic disc
Vessels directed temporally have an arching course; those directed nasally have a radial course. |
|
|
Appearance of retinal arteries and veins?
|
Arteries are brighter red and narrower than veins
|
|
|
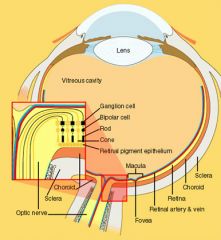
outer retina (rods and cones and retinal pigment epithelium)
is supplied by the |
choroidal circulation
|
|
|
Appearance of Fovea
|
2.5 mm-diameter area that looks slightly darker than the surrounding retina because of increased pigment
It is centered about 2 1/2 disc diameters temporal to the optic disc. The fovea lies in the center of the macular region. |
|
|
the fovea is made up of
|
cones exclusively
|
|
|
the fovea processes
|
high-contrast discriminative vision (visual acuity) & colour vision
|
|
|
List some macular disorders
|
AMD
diabetic macular oedema toxoplasmosis cherry-red spot |
|

|
optic disc cupping
thin neuroretinal rim large cup-to-disc ratio (0.8) |
|
|
|
|
|
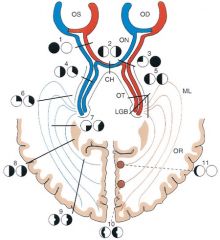
Pupillary light reflex
|

|
|
|
|
|
|
|
|
|
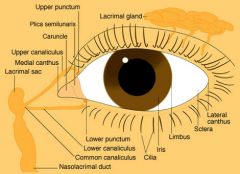
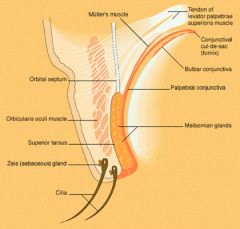
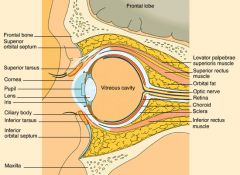
Saggital section eye in orbit
|
|
|
|
Chalazion
|
meibomian cyst
- chronic sterile lipogranulomatous inflammation involving the sebaceous glands of the eyelid |
|
|
a secondarily infected chalazion
|
internal hordeolum
|
|
|
Chalazion - presentation?
|
- gradually enlarging painless nodule
- any age |
|
|
What are the types of secretory product from an exocrine gland?
|
Serous (watery) - protein rich
Mucous (viscous) - CHO rich Sebaceous (oily) |
|
|
Hordeolum
|
an infection of the sebaceous gland of the eyelid
|
|
|
external hordeolum
|
=stye
acute staphylococcal abscess of a lash follicle & gland of Zeis |
|
|
Styes more commonly presents in
|
children
|
|
|
Treatment of Stye
|
topical antibiotics
warm compresses epilation of associated eyelash |
|
|
chalazion vs. hordeolum
|
chalazion is a painless lump away from the lid margin
vs. hordeolum is a painful red lump near the lid margin |
|
|
lamina cribrosa
|
layer of optic nerve head consisting of sheets of connective and elastic tissue, containing fenestrations which give passage to the nerve fibre bundles and retinal blood vessels.
- maintains IOP against a gradient between the intra-ocular and extra-ocular spaces - Being structurally weaker than the much thicker and denser sclera, the lamina cribrosa is more sensitive to changes in the intraocular pressure and tends to react to increased pressure through posterior displacement, thought to be one of the causes of nerve damage in glaucoma |
|
|
assessment of optic disc mnemonic
|
the 3 Cs
cup, colour, contour |
|
|
optic neuropathy causes mnemonic
|
NIGHT TICS
Neuritis Ischaemic Granulomatous Hereditory Traumatic Toxic Irradiation Compression |
|
|
ddx unclear contours of optic disc
|
- swollen in papilloedema due to ↑ ICP
- blurry with optic disc drusen |
|
|
Normal colour of optic disc
|
orange-pink donut with a pale centre
|
|
|
Ddx:
loss of orange-pink colour to optic disc to pale |
optic atrophy:
advanced glaucoma optic neuritis arteritic/non-arteritic ischaemic optic neuropathy compressive lesion |
|
|
Normal colour of optic disc cup
|
pale centre surrounded by an orange-pink rim
|
|
|
an increased cup to disc ratio may indicate
|
a decrease in the quantity of healthy neuro-retinal tissue and hence, glaucomatous change
|
|
|
Optic disc edema is commonly caused by
|
The 4 "I's":
increased intracranial pressure (papilledema) infarction inflammation infiltration (by cancer) Compression and toxins are other causes |
|

|
"sheathing" or perivenous lymphocytic infiltration = retinal vasculitis
sarcoidosis, Behçet's Disease, MS, idiopathic |
|

|
cotton wool spots
- caused by retinal nerve fiber layer microinfarcts - located around the optic disc and along the temporal vascular arcades |
|

|
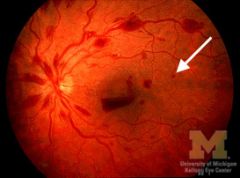
Roth Spot
- white-centered hemorrhage - cotton wool spot surrounded by hemorrhage - The cotton wool comes from ischemic bursting of axons; the small hemorrhage comes from ischemic bursting of a pre-capillary arteriole - not specific to bacterial endocarditis |
|

|
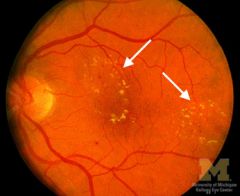
Retinal drusen
- tombstones of dead retinal pigment epithelial cells - commonest cause AMD |
|
|
Causes of cotton-wool spots
|
Any process that occludes small retinal arterioles
hypertension, diabetes, HIV, severe anemia or thrombocytopenia, hypercoagulable states, connective tissue disorders, viruses, lues, Behçet's |
|
|
greatest threat to vision in AMD
|
development of submacular neovascularization, which can cause bleeding in the retina
|
|

|

AV nicking
|
|

|
acute optic disc oedema
|
|

|
boat hemorrhage
|
|
|
dot hemorrhage
|
|

|

flame hemorrhage
|
|

|

cotton wool spots
|
|

|
retinal neovascularisation
|
|

|
chronic optic disc oedema
|
|

|
retinal hemorrhage types
|
|

|
retinal drusen
|
|

|
subtle optic disc oedema
|
|
|
hard exudates
|
|
|
silver wiring
|
|
|
copper wiring
|
|
|
yellow-white retina DDX
|

|
|
|
Sjögren's Syndrome assc ophthy cond'n
|
Keratitis sicca
|
|
|
Adult Rheumatoid Arthritis assc ophthy cond'n
|
Keratitis sicca, Scleritis
|
|
|
Relapsing Polychondritis assc ophthy cond'n
|
Scleritis, Orbital pseudotumor
|
|
|
Wegener's Granulomatosis assc ophthy cond'n
|
Scleritis, Sclerokeratitis, Orbital pseudotumor
|
|
|
Reiter's Syndrome assc ophthy cond'n
|
Uveitis, Conjunctivitis
|
|
|
Behçet's Disease assc ophthy cond'n
|
Uveitis, Retinal vascular occlusion
|
|
|
Juvenile Pauciarticular Arthritis assc ophthy cond'n
|
Uveitis
|
|
|
Sarcoidosis assc ophthy cond'n
|
Uveitis, Retinal vascular occlusion
|
|
|
Ankylosing Spondylitis assc ophthy cond'n
|
Uveitis
|
|
|
Lupus Erythematosus assc ophthy cond'n
|
Retinal vascular occlusion
|
|
|
Polyarteritis Nodosa assc ophthy cond'n
|
Retinal vascular occlusion
|
|
|
Scleroderma assc ophthy cond'n
|
Retinal vascular occlusion, Keratitis sicca
|
|
|
Primary CNS Angiitis assc ophthy cond'n
|
Retinal vascular occlusion
|
|
|
Giant Cell Arteritis assc ophthy cond'n
|
Ischemic optic neuropathy
|

