![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
59 Cards in this Set
- Front
- Back
|
Thrust mobilization is a type of _________technique that uses high-velocity / low amplitude forces after the restricted segment is positioned up against the restrictive barrier (in all planes).
|
direct
|
|
|
what kind of thrust is used in HVLA
|
A quick short thrust, with a small-moderate amount of force is delivered by the operator in an effort to remove the joint through the restrictive barrier and restore normal motion.
|
|
|
when using HVLA how long should it take to see improvements?
|
Improved joint motion should result very quickly
|
|
|
Is HVLA active or passive?
|
Considered ‘passive’ because the physician provides the treating force and the patient remains passive.
|
|
|
Indications for HV/LA manipulation
|
Sub-acute and/or chronic articular somatic dysfunction
---Specific to joint mobilization |
|
|
Goal of Manipulation
|
To restore maximal pain-free movement to the musculoskeletal system in postural balance
|
|
|
Duration of benefit from effective manipulation depends on _________________
|
depends on the identification and correction of the origin of the dysfunction.
|
|
|
when examining a patient you think you can use HVLA on. what kind of barrier must you find when looking at restriction of motion?
|
firm, distinct barrier
|
|
|
before you begin HVLA what might you do to make it easier
|
Soft tissue preparation
----Reduce hypertonicity ----Allow for increased resiliency of tissues surrounding the dysfunctioned joint. ----Relaxation and reassurance to the patient ----When the muscles and soft tissues are relaxed, less force is needed to move the joint |
|
|
what are the Effects of Treatment when using HVLA?
|
----HV/LA techniques gap the joint (stuck drawer)
----The operator must know the anatomy ----An audible ‘pop’ may coincide with joint gapping ----Production of a ‘pop’ is not the therapeutic goal! |
|
|
Basic Principles of HV/LA
|
1) Accurate diagnosis
2) Choice of vectoring force 3) Engage the restrictive barriers ----In all planes being used or lock other joints not being targeted ----Not overloading the tissues ----Without causing patient guarding 4) Maintain localization throughout the thrust ----Balance and control 5) Specificity!!! 6) Apply a HVLA thrust ----Minimal force, short distance, rapid acceleration/short duration without hesitation (Speed is important!!! Strike fast….just don’t use a big hammer) |
|
|
Technique Enhancers for HVLA
|
1) Prepare tissues - soft tissue or muscle energy techniques
2) Localizing the restricted segment about the planes involved 3) Respiratory reflex 4) Redirection of attention 5)Mild traction 6) Double thrust technique 7) Adjust the treatment to fit the patient AND your skill level 8) Post-thrust pause 9) Attitude for success! 10) Close contact with patient |
|
|
Forms of thrust mobilization
|
1) Rotational - cervical, lumbar
2) Translatory - thoracic, cervical 3) Distraction - an added dimension to all areas |
|
|
What is the ‘popping’ sound in HVLA
|
The patient must be assured that the sound is harmless, as well as unnecessary
|
|
|
Indications for modification of thrust (HV/LA) techniques to accommodate different patients
|
--Pregnancy
--Children --Guarding --Pain |
|
|
Absolute Contraindications for HVLA
|
1) Vertigo or loss of consciousness with cervical extension and rotation:
-----indication of vertebral artery occlusion. 2) “Rubbery” quality of soft tissue restriction 3) Pathologic instability of the O/A joint, i.e. RA, Down’s Syndrome 4) Suspicion of a fracture / dislocation / spinal instability 5) Septic joint (osteomyelitis) 6) Vasculitis/bursitis/ history of CVA 7) Metastatic bone disease 8) Moderate to severe osteoporosis 9) Patient’s refusal |
|
|
Relative Contraindications for HVLA
|
1) Cancer
2) Extremes of Age 3) Toddlers 4) Geriatric patients 5) Mild – Moderate osteoporosis 6) Neurologic disease (cerebral palsy, Parkinson’s, 7) Acute Herniated disc / radiculopathy 8) Acute somatic dysfunction 9) Metabolic bone disease |
|
|
Guidelines for Safety when using HVLA
|
1) Make an accurate diagnosis!
2) Be aware of possible complications 3) Listen with you hands 4) Emphasize specificity…not force!! 4) Ask permission to treat 5) SD with joint restriction is an indication for thrust techniques…not pain! 6) SD often coexist with other diseases….so look at the whole patient! |
|
|
Articulatory pop:
|
The sound made when cavitation occurs in a joint. See also cavitation
|
|
|
Axoplasmic transport:
|
The antegrade movement of substances from the nerve cell along the axon toward the terminals, and the retrograde movement from the terminals toward the nerve cell.
|
|
|
Cavitation:
|
the formation of small vapor and gas bubbles within fluid caused by local reduction in pressure. This phenomenon is believed to produce
an audible “pop” in certain forms of OMT. |
|
|
Chapman reflex:
|
A system of reflex points that present as predictable anterior and posterior fascial tissue texture abnormalities (plaque-like changes or stringiness of the involved tissues) assumed to be reflections of visceral dysfunction or pathology. 2. Originally used by Frank Chapman, DO, and described by Charles Owens, DO.
|
|
|
Contracted muscle:
|
The physiologic response to a neuromuscular excitation. See also contractured muscle
|
|
|
Contractured muscle:
|
histological change substituting non-contractile tissue for muscle tissue, which prevents the muscle from reaching normal relaxed length. See also contracted muscle
|
|
|
Dermatome:
|
The area of skin supplied by cutaneous branches from a single spinal nerve. (Neighboring dermatomes may overlap.) 2. Cutis plate; the dorsolateral part of an embryonic somite.
|
|
|
Homeostasis:
|
Maintenance of static or constant conditions in the internal environment. 2. The level of well- being of an individual maintained by internal physiologic harmony that is the result of a relatively stable state or equilibrium among the interdependent body functions.
|
|
|
Homeostatic mechanism:
|
A system of control activated by negative feedback
|
|
|
Mechanoreceptor:
|
A receptor excited by mechanical pressures or distortions, such as those responding to touch and muscular contractions.
|
|
|
Neurotrophy:
|
The nutrition and maintenance of tissues as regulated by direct innervation
|
|
|
Posterior component:
|
A positional descriptor used to identify the side of reference when rotation of a vertebral segment has occurred. In a condition of right rotation, the right side is the posterior component. It usually refers to a prominent vertebral transverse process.
|
|
|
Region:
|
An anatomical division of the body defined either by natural, functional or arbitrary boundaries. 2. Body areas for the diagnosis and coding of somatic dysfunction as defined in the International Classification of Diseases (currently ICD-9 CM) using the codes:
|
|
|
Regional motor inputs:
|
Motion initiated by an osteopathic practitioner through body contact and vector input that produces a specific response at each segment in the mobile system
|
|
|
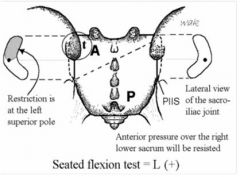
Anterior translated sacrum:
|

a sacral somatic dysfunction in which the entire sacrum has moved anteriorly (forward) between the ilia. Anterior motion is freer, and the posterior motion is restricted. (Fig. 42)
|
|
|
Backward torsions:
|
A backward sacral torsion is a physiologic rotation of the sacrum around an oblique axis such that the side of the sacral base contralateral to the named axis rotates posteriorly. L5 rotates in the direction opposite to the rotation of the sacral base. 2. Referred to as non-neutral sacral somatic dysfunctions (Archaic use). 3. A term by Fred Mitchell, Sr, DO, that describes the backward torsion as being non-physiologic in terms of the walking cycle.
|
|
|
Bilateral sacral extension
|

(sacral base posterior): . A sacral somatic dysfunction that involves rotation of the sacrum about a middle transverse axis such that the sacral base has moved posteriorly relative to the pelvic bones. Backward movement of the sacral base is freer, forward movement is restricted and both sulci are shallow. 2. The reverse of bilateral sacral flexion. (Fig 43)
|
|
|
Bilateral sacral flexion (sacral base anterior):
|
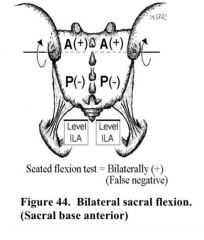
1. A sacral somatic dysfunction that involves rotation of the sacrum about a middle transverse axis such that the sacral base has moved anteriorly between the pelvic bones. Forward movement of the sacral base is freer, backward movement is restricted and both sulci are deep. 2. The reverse of bilateral sacral extension. (Fig 44)
|
|
|
Forward torsions:
|
Forward torsion is a physiologic rotation of the sacrum around an oblique axis such that the side of the sacral base contralateral to the named axis glides anteriorly and produces a deep sulcus. L5 rotates in the direction opposite to the rotation of the sacral base. 2. Referred to as neutral sacral somatic dysfunctions (Archaic use) 3. A group of somatic dysfunctions described by Fred Mitchell, Sr, DO, based on the motion cycle of walking.
|
|
|
Left on left (forward) sacral torsion:
|
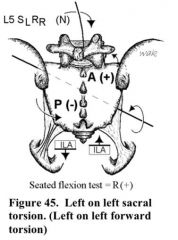
Refers to left rotation torsion around a left oblique axis
|
|
|
Left on right (backward) sacral torsion:
|

Refers to left rotation around a right oblique axis. Findings: The left superior sacral sulcus is posterior or shallow, and the right ILA is anterior or deep. There is a positive seated flexion test on the left. L5 is non- neutral SRRR. Left superior sacral sulcus will be restricted when springing. The lumbosacral spring test is positive, and the sphinx test is positive. (Fig. 46) See sacral torsion.
|
|
|
Posterior sacrum:
|
a positional term based on the Strachan model referring to a sacral somatic dysfunction in which the sacral base has rotated posterior and sidebent to the side opposite to the rotation. The dysfunction is named for the side on which the posterior rotation occurs. The tissue texture changes are found at the lower pole on the side of rotation. (Foundations). (The motion characteristics of L5 are not described.) (Fig. 47)
|
|
|
Right on left (backward) sacral:
|

Refers to right rotation on a left oblique axis. Findings: The right superior sacral sulcus is posterior or shallow, and the left ILA is anterior or deep. The seated flexion test is positive on the right. L5 is non-neutral SLRL. The right superior sacral sulcus is restricted when springing. The lumbosacral spring test is positive. The sphinx test is positive. (Fig. 49) See sacral torsion.
|
|
|
Posterior translated sacrum:
|

a sacral somatic dysfunction in which the entire sacrum has moved posteriorly (backward) between the ilia. Posterior motion is freer, and anterior motion is restricted. (Fig. 48)
|
|
|
Right on right (forward) torsion:
|
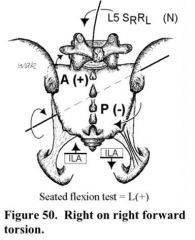
refers to a right rotation about a right oblique axis. (Fig. 50) See sacral torsion.
|
|
|
Rotated dysfunction of the sacrum:
|
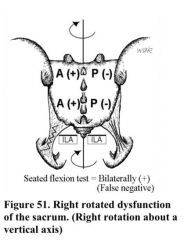
a sacral somatic dysfunction in which the sacrum has rotated about an axis approximating the longitudinal (y) axis. Motion is freer in the direction that rotation has occurred, and is restricted in the opposite direction. (Fig. 51)
|
|
|
Unilateral sacral extension:
|
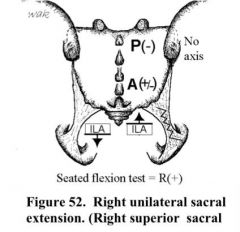
is a sacral somatic dysfunction described as a superior shear of one side of the sacrum resulting in a shallow (full) of, sacral sulcus and ipsilateral superior- anterior inferolateral angle of the sacrum. (Fig.52) See sacrum, somatic dysfunctions of, sacral shear.
|
|
|
Unilateral sacral flexion:
|
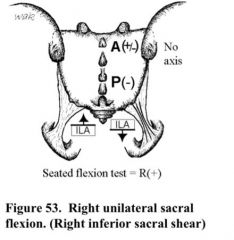
is a sacral somatic dysfunction described as a superior shear of one side of the sacrum resulting in a shallow (full) of, sacral sulcus and ipsilateral superior- anterior inferolateral angle of the sacrum. (Fig.52) See sacrum, somatic dysfunctions of, sacral shear.
|
|
|
Scan:
|
An intermediate detailed examination of specific body regions that have been identified by findings emerging from the initial examination
|
|
|
Somatogenic:
|
That which is produced by activity, reaction and change originating in the musculoskeletal system.
|
|
|
Somatosomatic reflex:
|
localized somatic stimuli producing patterns of reflex response in segmentally related somatic structures.
|
|
|
Somatovisceral reflex:
|
localized somatic stimulation producing patterns of reflex response in segmentally related visceral structures.
|
|
|
Spasm:
|
(compare with hypertonicity) a sudden, violent, involuntary contraction of a muscle or group of muscles, attended by pain and interference with function, producing involuntary movement and distortion (Dorland’ s).
|
|
|
Strain:
|
Stretching injuries of muscle tissue. 2. Distortion with deformation of tissue. See also ligamentous strain
|
|
|
Spinal facilitation:
|
1. The maintenance of a pool of neurons (e.g., premotor neurons, motor neurons or preganglionic sympathetic neurons in one or more segments of the spinal cord) in a state of partial or subthreshold excitation; in this state, less afferent stimulation is required to trigger the discharge of impulses. 2. A theory regarding the neurophysio- logical mechanisms underlying the neuronal activity associated with somatic dysfunction. 3. Facilitation may be due to sustained increase in afferent input, aberrant patterns of afferent input, or changes within the affected neurons themselves or their chemical environment. Once established, facilitation can be sustained by normal central nervous system (CNS) activity.
|
|
|
Trigger point (myofascial trigger point):
|
1. A small hypersensitive site that, when stimulated, consistently produces a reflex mechanism that gives rise to referred pain and/or other manifes- tations in a consistent reference zone that is consistent from person to person. 2. These points were most extensively and systematically documented by Janet Travell, MD, and David Simons, MD
|
|
|
Trophic:
|
Pertaining to nutrition, especially in the cellular environment (e.g., trophic function — a nutritional function).
|
|
|
Trophicity:
|
1. A nutritional function or relation. 2. The natural tendency to replenish the body stores that have been depleted
|
|
|
Trophotropic:
|
Concerned with or pertaining to the natural tendency for maintenance and/or restoration of nutritional stores.
|
|
|
Velocity
|
The instantaneous rate of motion
in a given direction. |
|
|
Visceral dysfunction:
|
Impaired or altered mobility or motility of the visceral system and related fascial, neurological, vascular, skeletal and lymphatic elements.
|

