![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
110 Cards in this Set
- Front
- Back
|
What are some important aspects of the historical treatment of mandibular trauma?
|
- bandages and external appliances
- Barton bandage |
|
|
What are the most common causes of mandibular fracture?
|
1) Assault
2) Motor vehicle accident 3) Gunshot wound / fall |
|
|
What is the distribution of most common locations of mandibular fractures?
|
Body - 29%
Condyle - 26% Angle - 25% Symphyses - 17% Ramus - 4% Coronoid -1% |
|
|
Motor vehicle accidents most commonly result in fracture of mandible in which location?
|
Symphyseal
|
|
|
GUN SHOT WOUND most commonly result in fracture of mandible in which location?
|
Body of mandible
|
|
|
ASSAULT most commonly result in fracture of mandible in which location?
|
angle
|
|
|
Define DORLAND'S "GREENSTICK' FRACTURE:
|
one cortex intact, one broken/bent
|
|
|
Defin DORLAND'S "SIMPLE/CLOSED" FRACTURE:
|
does not procuce a wound open to the external environment, whether it be through skin, mucosa or periodontal membrane
|
|
|
Define DORLAND'S "COMPOUND/OPEN" FRACTURE:
|
involving an external wound, skin, mucosa or periodontal membrane
|
|
|
Define DORLAND'S "COMMINUTED" FRACTURE:
|
bone is splintered or crushed
|
|
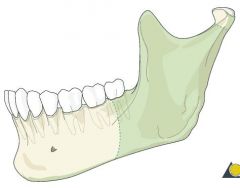
What type of angle fracture is this?
|
Vertically unfavourable
|
|
What type of angle fracture is this?
|
Vertically favourable
|
|
What classification of angle fracture is this?
|
Horizontally favourable
|
|
What classification of angle fracture is this?
|
Horizontally unfavourable
|
|
|
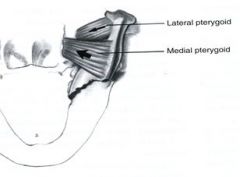
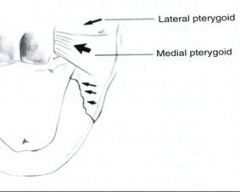
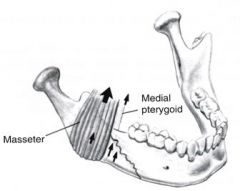
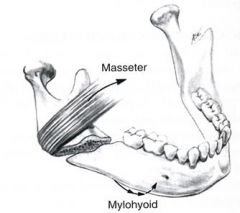
Lateral pterygoid muscle has what kind of tendency during fracture of the condylar head?
|
- anterior and medial displacement of the condylar head
|
|
|
What information is important during diagnosis of mandibular fracture?
|
- HEALTH HISTORY: pre-existing bone disease? Neoplasia? Arthritis?
- TMJ dysfunction history? legal and post-tx ramifications - HISTORY OF PREVIOUS TRAUMA? - Type and direction of force, type of object. |
|
|
What important clinical exam things should be thoroughly checked in cases of trauma / potential jaw fracture?
|
- CHANGE IN OCCLUSION: ask if bite feels different, open bites? OJ? Cross-bite?
- ANAESTHESIA, PARESTHESIA, or DYSTHESIA of lower lip? - ABNORMAL MANDIBULAR MOVEMENTS: trismus due to guarding of MOM. Deviation towards affected side in condylar fx. Impingmenent of coronoid by zyg. arch. - CHANGE IN FACIAL CONTOUR / MAND ARCH FORM - LACERATION, HEMATOMA, ECCHYMOSIS - LOOSE TEETH, CREPITATION ON PALPATION - DOLOR, TUMOUR, RUBOR, CALOR, LASSAE FUNCTION |
|
|
What are all the types of radiologic exam that can be attained?
|
- panoramic
- lateral oblique - pa skull - occlusal - periapical - reverse towne's - CT scan |
|
|
What are some of the primary principles of treatment of a patient with mandibular fracture?
|
1) DENTAL INJURIES should be evaluated and treated concurrently with treatment of fracture. Mand. canines should be maintained at all costs
2) REESTABLISHMENT OF OCCLUSION is the primary goal in treatment 3) MAND FRACTURES should always be treated first in multiple facial fracture cases 4) IMFIXATION varies with type, location, number, severity, pt age/health, and method for reduction and immobilization 5) PROPHYLACTIC abx for compound fractures 6) MONITOR NUTRIOTIONAL needs closely post-op |
|
|
What are the indications for CLOSED REDUCTION of mandibular fractures?
|
- nondisplaced favourable fractures
- grossly comminuted fractures - fractured exposed by significant loss of overlying soft tissue - edentulous mandibular fractures - mandibular fractures in children with developing dentitions - coronoid and condylar fractures |
|
|
What are some indications for OPEN REDUCTION of mandibular fractures?
|
- displaced unfavourable fracture through angle
- displaced unfavourable fracture of body or parasymphyseal region - multiple fractures of the facial bones - midface fractures and displaced bilateral condylar fractures - fractures of edentulous mandible with severe displacement of fracture fragments - edentulous maxilla opposing a mand. fracture - delay of treatment and interposition of soft tissue between noncontacting displaced fragments - malunion - special systemic conditions |
|
|
What are some ABSOLUTE INDICATIONS for open reduction of condylar fractures?
|
- displacement into middle cranial fossa
- inability to obtain adequate occlusion - lateral extracapsular dislocation - foreign bodies - mechanical obstruction impeding function of TM - open injury |
|
|
In planning open reduction and internal fixation in a patient with low subcondylar neck fracture, which of the following extraoral incisions provides the safest and most versatile exposure to the fracture site?
|
Retromandibular - less injury to the marginal mandibular, temporal, and zygomatic branches of the facial nerve. Allows access superiorly to the coronoid notch and inferiorly to the angle of the mandible.
|
|
|
Pre-auricular incision would be useful when needing to access what structure?
|
TMJ
|
|
This is the exposure that is given via the SUBMANDIBULAR INCISION:
|
SUBMANDIBULAR INCISION
|
|
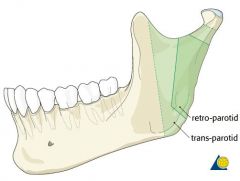
These are sites accessed via RETROMANDIBULAR INCISION:
|
RETROMANDIBULAR INCISION
|
|
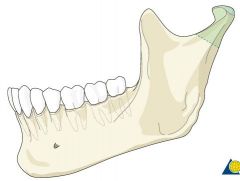
These are the sites accessed by PRE-AURICULAR INCISION:
|
preauricular
|
|
|
POST AURICULAR incision allows superior access to what?
|
- posterior TMJ
- good lateral joint exposure - fair anterior joint exposure - decreased risk of injury to facial nerve |
|
|
Pediatric mandibular fractures may result in what long term consequences?
|
Mandibular hypoplasia
|
|
|
On CT a subcondylar fracture of mandible the condyle is displaced medially and anteriorly. Which muscle would cause this?>
|
Lateral pterygoid
|
|
|
What are the three main buttresses that allow the face to absorb inferosuperior directed force?
|
- CANINE
- ZYGOMATIC - PTERYGOID |
|
|
The midface is well-equipped to withstand _____ impact, but poorly constructed to withstand ________ assault.
|
Well-equipped directly upward from below, poorly equiped for lateral / frontal assault
|
|
|
What are the general boundaries of a LE FORT I fracture?
|
- lateral border of piriform sinus
- across lateral max sinus wall - behind tuberosity - across pterygoid junction |
|
|
Where is hte force generally delivered in LE FORT I fracture?
|
above the level of the teeth
|
|
|
What are some of the symptoms/signs of LE FORT I fracture?
|
- maxillary mobility
- impacted or freely moveable - palatal ecchymosis - malocclusion - edema |
|
|
Where is the force generally delivered with LE FORT II fracture?
|
- level of nasal bones
|
|
|
What are the general borders of LE FORT II fracture?
|
- course along nasofrontal suture
- lacrimal bones - infraorbital rim |
|
|
What is another name for LE FORT II fracture?
|
pyramidal fracture
|
|
|
What are some signs / symptoms with LE FORT II?
|
- bilateral periorbital edema / ecchymosis
- paresthesia - malocclusion / open bite - step deformities - epistaxis |
|
|
Where is hte force direct with LE FORT III fracture?
|
- orbital level
|
|
|
What are some of the borders of a LE FORT III fracture?
|
- zygomaticotemporal and zygo-frontal sutures
- lateral orbital wall - inferior orbital fissure - nasofrontal suture - pterygomaxillary fissure |
|
|
What are some common signs / symptoms of Nasal-Orbital-Ethmoid Fractures?
|
- nasal fracture
- widened nasal bridge - epistaxis / rhinorhea - telecnathus - narrowed palpebral fissure |
|
|
What is more common, blow-out or blow in fractures of orbit?
|
BLOWOUT more common
|
|
|
What are some signs of BLOW-OUT fractures?
|
- increased orbital volume
- entrapment - enophthalmos - diplopia |
|
|
The best denture support has what characteristics?
|
- no evidence of intraoral or extraoral pathologic conditions
- proper inter-arch jaw relationship in AP, transverse and vertical dimensions - alveolar processes that are as large as possible nad proper configuration - no body or soft tissue protruberances or undercuts - adequate palatal vault form - proper posterior tuberosity notching - adequate attached keratinized mucosa in the primray denture-bearing/implant-bearing area - adequate vestibular depth - adequate strength where mandibular fractures may occur - protection of the neurovascular bundle - adequate bony support and attached soft tissue covering to facilitate implant placement when necessary |
|
|
What are the advantages of IMMEDIATE DENTURES:
|
- immediate psychological and esthetic benefit to pt
- splint the surgical site = less bleeding - improves tissue adaptation - vertical dimension more easily manipulated - aids in the forming of new speech patterns immediately with denture in place - may be less resorption |
|
|
What are the disadvantages of IMMEDIATE DENTURES?
|
- may not fit good immediately due to guesswork
- can have much bleeding under dneture if poor fit - need for possible frequent relining post op - occasional denture sores and delayed healing - |
|
|
Define ALVEOLECTOMY:
|
- removal of part of the alveolar ridge
|
|
|
Define ALVEOPLASTY:
|
- reshaping of alveolar ridge or process to accomodate a prosthesis
|
|
|
ALVEOPLASTY may include what things?
|
- eliminating the undercuts
- removing sharp protruberances - removal of exostoses or tori - recontouring bony max tuberosities |
|
|
What are the POST-OP instructions following alveoplasty?
|
- should not remove denture but should wear continuously. bite gauze bilaterally for hemostasis
- after 24hrs patient returns for post-op check, remove denture as tissues are swollen - dentist washes denture and has pt rinse mouth - underlying mucosa and alveolar ridges are inspected for any areas of excessive pressure - all areas of high-pressure are relieved - patient advised to contiunue to wear denture continuously except to clean and to rinse mouth with saline - pt is seen at 1 week for suture removal and 2 weeks for another check - 3 months for reline - NO SmoKEinG |
|
|
What are some MINOR PREPROSTHETIC SURGERIES?
|
HARD TISSUE PROCEDURES:
- alveloplasty - SOFT TISSUE PROCEDURES: - enlarged max tuberosities - soft tissue ridge - epulis fissuratum - inflammatory papillary hyperplasia - frenectomies |
|
|
What are some MAJOR PREPROSTHETIC SX?
|
RELATIVE HEIGHTENING
- vestibuloplasty +/- lowering of the floor of mouth - Casangion lip-flip technique: increase depth of vestibule to increase flange ABSOLUTE HEIGHTENING - bone grafting - visor osteotomy - max sandwich graft - tent-pole procedure |
|
|
Define BRONJ:
|
- exposure of bone in the maxilla or mandible persisting for more than 8 weeks in a patient who has taken or who is currently taking a bisphosphonate and who has no history of radiation therapy to the jaws
|
|
|
What is the most common Bisphosphonate prescribed?
|
FOSAMAX (Alendronate) - Oral - most commonly used to tx osteoporosis and osteopenia
- greater than 10 year half life in bone |
|
|
What is the 2nd most commonly prescribed bisphosphonate?
|
ACTONEL
|
|
|
What is the biologic action of bisphosphonates?
|
- inhibition of bone resorption, hence bone turnover and renewal
- reduction of serum calcium - due to inhibition and/or irreversible cell death of the osteoclast - repeated doses of bisphosphonates accumulate readily to the mineral crystals on every bone surface |
|
|
How are bisphosphonates removed from the body?
|
- only by osteoclast mediated bone resorption
|
|
|
Why are the jaws mainly affected in Bisphosphonate therapy?
|
- jaws have greater uptake of bisphosphonates and readily accumulate at high concentrations
- depend more on orthoclastic bone resorption-remodelling and renewal than any other bone in adult skeleton |
|
|
What are some "off-label" medical indications for BisPhos use?
|
- children w/ osteogenesis imperfecta
- fiborus dysplasia - juvenile osteoporosis - gaucher disease - steroid induced osteoporosis - attempts at reduction of periodontal bone loss in post-meno women |
|
|
Osteoclasts develop from what?
|
- bone marrow precursors
|
|
|
What is the HOWSHIP LACUNA?
|
- sealed area around osteoclast
- HCl is secreted here (pH 1) |
|
|
The primary cause of complications in implant dentistry is related to what?
|
Biomechanics
|
|
|
What are some biomechanical considerations in implant treatment planning that can decrease failure/complications?
|
- prosthesis design
- patient force factors - bone density in edentulous sites - key implant position and number - implant size - availalbe bone in the edentulous sites - implant design |
|
|
What are the different widths of implants available?
|
- 3.7mm
- 4.2mm - 5.2mm - 6.2mm |
|
|
How much space is required between implant and adjacent root?
|
1.5mm
|
|
|
How much space is required between TWO ADJACET IMPLANTS?
|
3.0 mm
|
|
|
A papilla is ALWAYS present if the distance between contact point and alveolar ridge is how long?
|
5mm or less
|
|
|
At 6mm between contact point and alveolar ridge what percentage will have interdental papilla?
|
- 56%
|
|
|
What are the 4 key implant positions?
|
- no cantilevers
- no three adjacent pontics - canine-molar rule - an arch is divided into five segments, when more than one segment of an arch is being replaced, a key implant position is at least one implant in each segment |
|
|
How much force would be produced if 25lb of force was placed on a 10mm cantilever pontic?
|
The abutment would experience 250lb force
|
|
|
Effort Arm / Resistance Arm = Mechanical Advantage
|
?
|
|
|
What are some conditions that require cantilever implants?
|
- edentulous mandible / maxilla that doesnt have sufficient bone in posterior regions
- |
|
|
How is the AP spread of five implants in the mandible measured?
|
From distal of the last two implants to the mid position of the most anterior implant
|
|
|
When five or more implants are positioned around an arch, the cantilever may extend as far as _____ the AP distance?
|
2.5 times
|
|
|
Metal flexure is related to the SQUARE/CUBE of the distance.
|
CUBE!
|
|
|
The span of pontics in ideal tx plan should be limited to what size?
|
2 premolars =~ 13-16mm
|
|
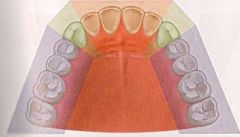
KNOW THE AREAS
|
KNOW THE AREAS
|
|
|
What are the general rules for implant placement planning?
|
- no cantilever
- no 3 adjacent pontics - canine position - at least 1 implant in each segment of the arch |
|
|
What is the advantage of SPLINTED IMPLANTS?
|
- increase functional surface area
- increase AP spread to resist lateral loads - decreased risk of screw loosening - decreased risk of marginal bone loss - decrease risk of implant component fracture |
|
|
What is the highest prosthetic complication with single-tooth implants?
|
Screw-loosening
|
|
|
Why is it that maxilla usually needs more implants?
|
less dense bone
|
|
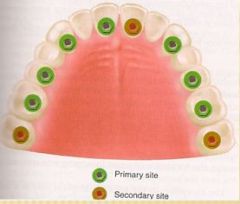
KNOW!
|
know
|
|
|
Implants are important in completely edentulous patients for what reasons?
|
- maintain bone volume
- maintain function - masticatory muscle activity - esthetics - psychological health |
|
|
What are the advantages of implant overdentures?
|
- minimum anterior bone loss
- improved stability / retention / support - improved occlusion - decrease in soft tissue abrasion - improved chewing efficiency and force - improved speech - reduced prosthesis size |
|
|
How much space is required for mandibular overdenture?
|
12mm of space between crestal bone and occlusal plane
|
|
|
What are some factors that can cause alveolar bone resorption?
|
- periodontal disease
- tooth eruption - ortho therapy - parafunction - trauma - vertical root fracture - apicoectomy - ill-fitting crown - subgingival tooth preparation - extractions |
|
|
Which plate is the first to remodel or resorb after exodontia?
|
FACIAL plate
|
|
|
What is the rate of loss of facial plate after tooth extraction?
|
- FIRST year 25%
- THREE yrs 40-60% |
|
|
What are the keys to successful bone grafting?
|
- absence of infection
- soft tissue closure - space maintenance - graft immobilization - RAP - host bone vascularization - growth factors - BMP - healing time - defect size / topgraphy - graft material |
|
|
What is the most common post-op complication from bone grafting?
|
- incision line opening
|
|
|
Define "space maintenance" in regards to bone grafting?
|
- the space must exist long enough for bone to fill the desired region
|
|
|
How long does an exo socket take to fill up with bone?
|
4-6 months
|
|
|
Bone graft healing time is related to waht factors?
|
- number of remaining walls of bone
- amount of autogenous bone in the graft - size of defect - systemic diseases - gen rule 4-6 months when graft volumes <5mm in dimension |
|
|
What are the four phases of Autogenous bone grafts?
|
PHASE 1: osteogenesis - bone regeneration. Surviving cells 4 weeks (osteoid)
PHASE 2: Osteoinduction. BMP release 2 wks to 6 mon, peak at 6 weeks PHASE 3: Osteoconduction. Inorganic matrix-space filler PHASE 4: Cortical plate, barrier membrane |
|
|
What are the borders of the oral cavity?
|
ANTERIOR: skin - vermillion junction of lips
POSTERIOR: tongue base / circumvallate papillae SUPERIOR: junction of hard / soft palate |
|
|
What are some signs and symptoms of ORAL CANCER?
|
- oral pain
- bleeding - dysarthria - odynophagia - dysphagia - trismus - halitosis - ear pain - loose teeth - numbness (lip, tooth, jaw) - neck mass - assess bony fixation |
|
|
What are the most common sites for oral cancer?
|
- Lips
- FOM - tongue - retromolar - buccal mucosa - hard palate - alveolar ridge |
|
|
What are some risk factors for Oral Cancer?
|
- smoking
- EtOH - chewing tobacco - reverse smoking - chronic irritation - immunocompromised - HPV 16 18 - sun (UV) exposure - genetic factors |
|
|
Which pre-cancerous lesions have the HIGHEST risk of developing into full cancer?
|
- erythroplasia / erythroplakia (50%)
- leuko (5%) - lichen planus (1%) |
|
|
What are some treatment options for Lichen Planus?
|
- avoidance of triggers
- improve oral hygeine - steroids (oral or topical) - cyclosporin 500mg qidx 4-8 weeks - cryotherapy - uv light - laser surgery |
|
|
What is the tumour grading system?
|
CIS: carcinoma in situ
G1: well-differentiated G2: moderately-well-diff G3: poorly diff G4: undifferentiated |
|
|
What is the most common oral cancer?
|
Squameous
|
|
|
What are our differential diagnoses for Squamous cell carcinoma?
|
- granular cell myoblastoma
- minor salivary gland neoplasm - sarcomas - Lymphomas - malignant melanoma - Hairy leukoplakia, kaposi, HIV |
|
|
What are the 5 histological subtypes of SCC?
|
- generic
- adenoid - spindle (aggressive / mets = 37%) - basaloid (high grade / 64% regional mets) - verrucous (low-grade, low risk regional spread) |
|
|
What is the TUMOR staging protocol?
|
TIS: carcinoma in situ
T1: tumour 2cm or less in greatest dimension T2: 2-4cm T3: >4cm T4: tumour invades adjacent structures (ie through cortical bone, FOM, facial skin, deep muscles) |
|
|
What is the LYMPH NODE staging protocol?
|
NX: cannot be assessed
N0: no regional lymph node mets N1: Met in single ipsilateral lymph node, >3cm N2a: Met in single, ipsi LN, 3-6cm N2b: Met in multi-ipsi LN, none>6cm N3: Met in LN >6cm in greatest dimension |
|
|
What are some ADVERSE FEATURES of oral cancer once biopsied?
|
- perineural invasion
- depth of invasion >4mm - lymphovascular invasion - positive resection margins (>5mm) - aggressive tumour subtype (ie spindle) - extracapsular spread |
|
|
CT or MRI is required for what tumour stage?
|
T2 or greater
|
|
|
What are some complications of radiotherapy?
|
- skin necrosis
- mucositis - dental caries - cataracts - xerostomia - transverse myelitis - myelopathy - osteoradionecrosis |

