![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
|
With the Biomechanics of the thoracic spine...
The orientation of the ______ allows the greatest motion in rotation Least amount of motion in the thoracic spine is in? why? |
facets
extension- minimal glide of the superior articular process on the inferior process by the spinal processes and anterior longitudinal ligaments |
|
|
Mid back pain causes?
Why are X-rays not always necessary? |
large velocity/force- but mostly degenerative changes which is why X-rays are not necessary
|
|
|
What do yo look for in lab evaluations?
|
If Hx of cancer or other problems that could cause viscero somatic pain
|
|
|
Viscerosomatic Reflex
What is it again? What does it cause? |
Disturbances in the viscera (organs) increases sympathetic outflow to somatic structures
- this causes increased muscle tones at certain points (chapman point changes) - Also referred pain |
|
|
Name the sympathetic outflow for the following...
a. All that originate from T1-4 b. T1-6 |
a. head/neck, thyroid
b. Mammary, Esophagus, Heart, Lung |
|
|
Name the sympathetic outflow for the following...
a. T5-9 b. T5R c. T7L d. T7R |
a. Stomach, Duodenum/liver
b. Gallbladder c. Spleen d. Pancreas |
|
|
Name the sympathetic outflow for the following...
a. Stomach, Duodenum/liver b. Gallbladder c. Spleen d. Pancreas |
a. T5-9
b. T5R c. T7L d. T7R |
|
|
Name the sympathetic outflow for the following...
a. head/neck, thyroid b. Mammary, Esophagus, Heart, Lung |
a. All that originate from T1-4
b. T1-6 |
|
|
What is a facilitated segment?
|
sustained CNS activity occurs less stimulation is required due to continued previous stimulation resulting in the somatic dysfunctions we find
|
|
|
What are causes (general categories) of mid back pain? (6)
|
1. Musculoskeletal
2. GI 3. GU 4. Pulmonary 5. Cardiac 6. Other- viruses, cancers, aneurysms |
|
|
What are the GI causes of mid back pain?
|
IBS, GERD, PUD, Gall Bladder
|
|
|
What might cause itchy burning type pain in someone with thoracic pain?
|
Herpes Zoster
|
|
|
Name the main musculoskeletal mimicking pathologies for mid back pain (5)
|
PPURK
Pancreatitis Pelvic Infections UTI's Reproductive tract dysfunction Kidney Stones |
|
|
If you were to summarize the order of the evaluation and work up of someone with back pain... what do we have? (Physical)
|
Start with...
1. Posture‐‐static 2. Seated- Para‐spinal evaluation (C, T, L spine), ribs, maybe check upper extremity 3. Supine- C spine assessment, ribs, Pelvic Rock, ASIS/PSIS, leg length, LE eval ‐ fibular head, foot, ankle 4. Prone, Sacrum, Further para‐spinal evaluation (T, L spine), ribs |
|
|
What are some red flags to mid back pain?
What is most common back pathology for someone 20-29? |
Any pain from someone
<10 yr old think scoliotic problems, CA, intervertebral diskitis (aggrevated by activities) 20-29 disk injury |
|
|
What is the most likely anatomical problems with the 60-69 yr old group?
|
Spinal stenosis, degenerative problems, and tumors
|
|
|
What are two markers for palpation in thoracic spine?
What attaches to the upper/lower parts of the 12th ribs? |
T3- spine of scapula
T7- inferior angle of scapula - diaphragm upper and quadratus lumborum attaches to the lower |
|
|
If you ranked lower back pain (LBP) what is it as far as how common reason for visit? (in US)
How long before it is considered chronic? |
5th most common in US
- 6 weeks |
|
|
What do you have rule out for lower back first?
If Hx of drug abuse what is possible likely cause of LBP? |
bowel or bladder changes
- Emergency because it may be Cauda Equina Syndrome - drug use think spinal infection |
|
|
When getting the history from the patient with lower back pain how do you classify if the pain is...
a. Acute LBP b. Acute radiculopathy c. Chronic radiculopathy |
1. Acute LBP ‐ pain that does not radiate past knee for less than 6 weeks
2. Acute Radiculopathy – LBP with radiation past the knee for less than 6 weeks 3. Chronic Radiculatopthy ‐ LBP with radiation past the knee for more than 6 weeks |
|
|
What strength tests are used for LBP?
|
Ankle dorsiflexion
Great toe dorsiflexion Plantar flexion Hip flexor |
|
|
What are the classic D/D of LBP?
|
1. Low back strain/sprain
2. Lumbar disc herniation 3. Lumbar spinal stenosis 4. DDD (degenerative disc disease) 5. Spondylolisthesis |
|
|
For the physical exam of a pt with LBP what are the processes?
|
1. Palpate for tenderness on spine
2. Posture/range of motion 3. Strength testing (heels, plantars, flexors) 4. Reflex testing (ankle, knee) 5. Sensory testing |
|
|
Strain vs sprain?
|
Strain- musclulature
Sprain- ligaments |
|
|
What are the diagnostic tests for LBP most likely due to lower back strain/sprain?
|
– Reliance on comprehensive physical exam
– Complete neurologic assessment – Straight leg raising tests • Higher sensitivity for levels L5, S1 – Plain radiographs rarely assist in diagnosis |
|
|
Treatment for lower back strain/sprain
a. acute phase *days-1-2weeks* b. subacute phase |
a. Soft tissue OMT, ROM,
• Pharmacologic‐‐NSAIDS, muscle relaxants, strongly consider spinal manipulation b. More aggressive OMT as needed, aerobic conditioning and strength training • Usually about 4 weeks to recovery |
|
|
Ligamentous support portion of the intervertebral disk
• Disk does not herniate into the spinal canal, but leakage from the nucleus pulposus can cause localized inflammation affecting nerve roots • May weaken with repeated small tears |
annulus fibrosis
|
|
|
What causes the problems with an annulus fibrosis?
|
Annulus fibrosus is the ligamentous portion in the disks
- leakage from the nucleus pulposus cause localized inflammation affecting nerve roots |
|
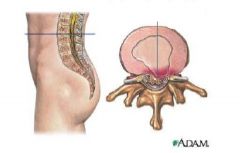
What is going on
|
annulus fibrosis
|
|
|
Acute phase treatment of Lumbar disk herniation...
|
• Soft tissue OMT
• NSAIDS • Muscle relaxants • Narcotic medications • Behavior modification • Oral steroids or epidural injections may benefit |
|
|
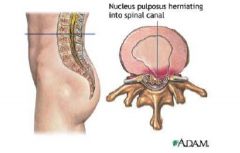
Compare an annulus fibrosis with an actual lumbar disk herniation...
|
Annulus fibrosis is when nucleus pulposis leaks out causing an inflammatory reaction
- disk herniation is when the nucleus pulposus extrudes through annulus fibrosis |
|
|
With lumbar disk herniation what symptoms do you want to keep eye out for that resemble Cauda equina syndrome?
|
• Urinary overflow incontinence
• Perianal numbness • Reduced anal sphincter tone • Bilateral involvement • Motor/Sensory Deficits |
|
|
Where do lumbar disk herniations usually occur?
Symptoms? |
L4-5 or L5-S1 on posterolateral portion which allows bulging or herniation into the lumbar canal
- usually abrupt with unilateral radicular (past knee and lower back) pain |
|
|
What is diagnostic image for disk herniation?
But what would cause you to order this test? |
MRI
- intolerable pain, or neurological changes |
|
|
How do DDD progress?
What does it lead to? |
Nucleus pulposus looses hydrophilic properties, disk height lessens, and ligaments become loose
– Twisting and bending can tear anulus fibrosus – Leads to chronic low back pain and osteoarthritis |
|
|
What symptoms does DDD present?
What makes it worse? better? What could long term pain cause other than structural probs? |
low back pain radiating to the butt
- made worse by bending, lifting, stooping, or twisting - relieved by lying down - could lead to depression |
|
|
In the physical exam of someone with DDD what would you findings most likely show?
|
– Lumbar and sacral tenderness
– Paravertebral muscle spasms – Motor and sensory function, reflexes are normal – Straight leg raising and ROM mildly restricted |
|
|
For DDD what are the diagnostic tests ordered?
|
Ap and lateral radiographs show...
a. • Anterior osteophytes b. Reduced disk height c. Occasional “vacuum sign” (nitrogen in disk space) |
|
|
What is the treatment for DDD?
|
– Chronic pain management
– Facet injections – OMT – NSAIDS/non‐narcotic pain meds – Antidepressants to modulate pain perception – Weight reduction – Exercise prescription – Smoking cessation |
|
|
Narrowing of one or more levels of the lumbar spinal canal and subsequent compression of the nerve roots. Few have symptoms, must be anatomically severe for symptoms to be present
|
lumbar spinal stenosis
|
|
|
Forward slippage of a lumbar vertebral body
Where does this slippage usually occur on spine? |
spondylolisthesis- usually L4 and L5
|
|
|
If a physical shows...
-Diminished lumbar lordosis and flattening of the gluteal region – Step‐off of spinous process with a significant one – Marked hamstring tension and very limited straight leg raising What is most likely diagnosis? |
thinking spondylolisthesis "You've got a spondy!"
|
|
|
What is the general treatment for spondylolisthesis?
|
– Flexion exercises, stretching exercises
– OMT as with spinal stenosis – Intermittent NSAID use as needed – May need to wear back brace or have surgery if the condition becomes severe |
|
|
What is the level usually find spondylolithesis?
Is it different for pediatric? |
L4-5
Peds- L5-S1 |
|

|

|
|
|
During a physical exam of someone with spondylolsthesis...
What should cause pain? What are diagnostic radiographs? |
Pain- flexion and extension
- AP and lateral are adequate, but may want MRI to see canal space changes and oblique view to to rule out spondylolysis |

