![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
107 Cards in this Set
- Front
- Back
|
Gypsum:Fixation casts to articulators
w/p=63cc/100g |
Quick Set Plaster
|
|
|
Gypsum: Diagnosis/Planning
w/p=45 to 55 cc/100g |
Plaster Study Models
|
|
|
Gypsum: Fabricate Appliances
w/p=30cc/100g |
Stone Casts
|
|
|
Gypsum: Crown Fabrication
w/p=22cc/100g |
Improved Stone Dies
|
|
|
If more water is used than recommended. Mixes have _______ setting time, are _________, poor _________ (too fluid), and ________ hard, so it ________more easily
|
LONGER
WEAKER STACKING LESS ABRADES |
|
|
Accelerators
|
2% KSO4
Slurry Water Longer Mix/Vibration |
|
|
Retarders
|
Blood
Salivia Alginate Less mixing/vibration |
|
|
6 to 8 minutes
|
initial set/loss of gloss
|
|
|
15 to 30minute
|
final set
|
|
|
30 to 60minutes
|
separate from impression
|
|
|
Mixing Principles
|
-Sift powder into water bowl with vibrator on high
-Mix without fluffling until homogeneous on Vibrator -Flex bowl vigourously and repeatedly while pressing bowl hard on vibrator on high setting |
|
|
sources of macroscopic porosity
|
-air trapped in btw powder particles
-air mixed in while homogenizing -air trapped while pouring the mix in the mold |
|
|
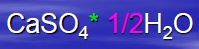
Gypsum Powder
|
|

|
Gypsum Cast
|
|
|
Gypsum Rxn
|
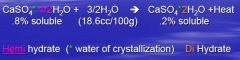
|
|
|
Forming Gypsum powder into Gypsum Cast is what type of chemical reaction?
|
Exothermic-releases heat
|
|
|
3 things that cause Alginate's poor dimensional stability
|
-water evaporation
-imbibition -syneresis |
|
|
explain Water evaporation in relating to poor dimensional stability
|
evaporation from gel causes 25+% shrinkage
|
|
|
explain imbibition in relating to poor dimensional stability
|
water absorption with water soaking
|
|
|
explain syneresis in relating to poor dimensional stability
|
shrinkage with continued reaction in humidor. AT 100% HUMIDITY
|
|
|
When do you pour your cast after taking the Alginate impression?
|
ASAP-as soon as possible
|
|
|
sets alginate too fast
|
hot water
|
|
|
slow set and flows too much
|
cold water-also problem for sensitive teeth.
|
|
|
a type whose physical condition is changed by a chemical action that is not reversible. It is an impression material that is elastic when set.
|
irreversible hydrocolloid
|
|
|
a type whose physical condition is changed by temperature. The material is made fluid by heat and becomes an elastic solid on cooling. Can change from a gel to solid set with the addition or removal of heat
|
reversible hydrocolloid
|
|
|
particles less than 0.5um
|
colloid
|
|
|
Steps in making successful alginate impressions
|
1. fluff powder and scoop parallel to container
2. level scoop, NO packing 3. 1 scoop/water ring 4. use room temperature water 5. wet powder slowly 6. spread in thin layers with flat spatula, to eliminate air bubbles by "strooping" back and forth til cmppth and creamy 7. load tray back to front, must be full 8. seat pt upright, wipe alginate on tray with wet glove finger 9. rotate corner of tray into mouth, center tray on midline of arch 10. pull lips over the tray before seating. seat posterior first. (3-5mm material tray btw teeth and soft tissue) 11. wit 2 minutes 12. break air lock 13. rinse in water for 30s 14. check impression for voids 15.spray with disinfectant and wrap in damp towl and placed in plastic bag 16. clean metal tray/ pour casts |
|
|
the condylar housing is on the upper member of the articulator and the condylar ball is on the lower articulator
|
arcon articulator
|
|
|
Same relationship found in the human skull
|
arcon articulator
|
|
|
the condylar housing is on the lower member of the articulator and the condylar ball is on the upper member of the articulator
|
non arcon articulator
|
|
|
opposite of what is found in the human skull
|
non arcon articulator
|
|
|
caliper-like instrument which is used to relate the maxillary cast to the condyle elements of the articulator just like the maxilla is related to the condyles and fossa of your patient
|
facebow
|
|
|
facebow utilizes an estimate of the location of the transverse horizontal or hinge axis
|
arbitary/ average value
|
|
|
facebow has adjustible caliper ends which are used to locate the transverse horizontal axis of the mandible
|
kinematic
|
|
|
precise enough for most diagnosis and treatment
|
arbitrary facebow and fixed conylar width articulator
|
|
|
mechanical instrument that represents the tempromandibular joints and jaws, to which maxillary and mandibular casts are attached to stimulate some or all mandibular movements
|
articulator
|
|
|
Masseter
|
Superficial head
O: Anterior 2/3 of lower border of the zygomatic arch I: On the angle and ramus of the mandible Deep head O: Medial surface ( posterior) of the zygomatic arch I : On ramus and part of the coroniod process Action: elevation (as in closing of the mouth) and protraction of mandible |
|
|
temporalis
|
O: Lateral surface of the skull;
temporal fossa and temporal fascia I: Coronoid process of mandible and border of ramus A:Elevation and retraction of mandible |
|
|
Occipitalis
|
Origin: Superior nuchal line of the occipital bone and mastoid process of the temporal bone
Insertion: Galea aponeurosis Actions: Moves the scalp back |
|
|
frontalis and occipitalis joined at _______ by fascial connective tissue sheath and aponeurosis (tendon) sheath
|
vertex
|
|
|
Sternocleidomastoid
|
Origin: Manubrium sterni and medial portion of the clavicle
Insertion:Mastoid process of the temporal bone, superior nuchal line Actions: Acting alone, tilts head to its own side and rotates it so the face is turned towards the opposite side. Acting together, flexes the neck, raises the sternum and assists in forced inspiration. |
|
|
digastric
|
Origin:
anterior belly - digastric fossa (mandible); posterior belly - mastoid process of temporal bone Insertion: Intermediate tendon (hyoid bone) Actions: Opens the jaw when the masseter and the temporalis are relaxed. |
|
|
Medial Pterygoid
|
Origin:
deep head: medial side of lateral pterygoid plate behind the upper teeth superficial head: pyramidal process of palatine bone and maxillary tuberosity Insertion: medial angle of the mandible Actions: elevates mandible, closes jaw, helps lateral pterygoids in moving the jaw from side to side |
|
|
Lateral Pterygoid Muscle
|
Origin: Great wing of sphenoid and pterygoid plate
Insertion: Condyloid process of the mandible Actions: depresses mandible, protrude mandible, side to side movement of mandible |
|
|
Occurs when there is contact
between the maxillary and mandibular posterior teeth on the same side of the arches as the direction in which the mandible has moved |
working interference
|
|
|
An occlusal contact between
maxillary and mandibular teeth on the side of the arches opposite the direction in which the mandible has moved in a lateral excursion |
nonworking interference
|
|
|
The proximity of the teeth to the
muscles and the oblique vector of the forces make contacts between opposing posterior teeth during protrusion |
protrusive interference
|
|
|
Pattern of Disclusion
A pattern of mutually-protected articulation in which the vertical and horizontal overlap of the canine teeth disengage the posterior teeth in excursive movements of the mandible |
anterior/canine guidance
|
|
|
Pattern of dis-occulsion
Multiple mandibular teeth contact the maxillary teeth during lateral movement on the working side Occlusal forces distributed over a group of teeth |
group function
|
|
|
It is characteristic where the
incisal edges of the maxillary incisors extend below the incisal edges of the mandibular incisors when the posterior teeth are fully interdigitated. |
overbite
|
|
|
vertical dimension
|
overbite
|
|
|
It is the characteristic where the incisal edges of the maxillary teeth
extend labially to the incisal edges of the mandibular incisors when the posterior teeth are inter digitated |
overjet
|
|
|
horizontal dimension
|
overjet
|
|
|
When the upper canine
occludes in the embrasure between the lower canine and the lower first premolar |
Class 1
|
|
|
The maxillary first
molar mesiobuccal cusp tip occludes in the lower first molar buccal developmental groove |
Class 1
|
|
|
When the upper canine occludes
anterior to the embrasure between the lower canine and the lower first premolar |
Class 2
|
|
|
When the maxillary first molar
mesiobuccal cusp tip occludes anterior to the buccal developmental groove on the mandibular first molar |
Class 2
|
|
|
When the upper canine
occludes posterior to the embrasure between lower canine and the first premolar |
Class 3
|
|
|
When the upper first molar mesial cusp
tip occludes distal to the buccal develop-mental groove of the lower first molar |
Class 3
|
|
|
diagnostic dilemma
|
PATIENTS WITH PRIMARY MYOFASCIAL PAIN PROBLEMS CAN DEVELOP SECONDARY TEMPOROMANDIBULAR JOINT PATHOLOGY
PATIENTS WITH PRIMARY TMJ PATHOLOGY CAN DEVELOP SECONDARY MYOFASCIAL PAIN PROBLEMS |
|
|
joint pain is
|
constant and localized
|
|
|
muscle pain is
|
intermittent and poorly localized
|
|
|
muscle pain increases when biting on the
|
painful side
|
|
|
joint pain increases when biting on the
|
opposite side
|
|
|
congenital anomalies of the TMJ are characterized by
|
agenesis of the condyle
|
|
|
IS A CHRONIC LIMITATION OF MOVEMENT DUE TO JOINT CONSOLIDATION
|
ankylosis
|
|
|
IS LIMITATION OF MOVEMENT DUE TO MUSCLE INFLAMMATION OR SPASM
|
trismus
|
|
|
Patients with disc displacement have a history of
|
prior clicking
|
|
|
Patients with disc adhesion have a sudden onset of
|
locking without a prior history of any TMJ problems
|
|
|
TREATMENT OF THE MPD PATIENT Phase I (2-4 Wks)
|
INITIAL EXPLANATION OF THE PROBLEM
HOME THERAPY MEDICATIONS FOR PAIN AND ANXIETY MEDICATION FOR SLEEP POSSIBLE USE OF A BITE APPLIANCE |
|
|
TREATMENT OF THE MPD PATIENT Phase II (4Wks)
|
RECONSIDER THE DIAGNOSIS
CHECK FOR COMPLIANCE CONTINUE HOME THERAPY AND MEDICATIONS CONSIDER USING A BITE APPLIANCE |
|
|
TREATMENT OF THE MPD PATIENT Phase III (4-6 Wks)
|
CONTINUE HOME THERAPY AND MEDICATIONS
RE-EVALUATE THE BITE APPLIANCE INITIATE PHYSICAL THERAPY |
|
|
TREATMENT OF THE MPD PATIENT Phase IV
|
RE-EVALUATE DIAGNOSIS AND COMPLIANCE
DETERMINE THE NEED FOR CONSULTATION PSYCHOLOGICAL COUNSELING REFERRAL TO A PAIN CENTER |
|
|
oral devices that have been fitted over the occlusal surfaces of teeth for the treatment of different masticatory disorders
|
oral orthotic
occlusal/bite splint occlusal/bite guard night guard deprogrammer |
|
|
modes of action
|
use of appliances will induce muscle relaxation, and usually makes it possible to record centric relation clinically by jaw manipulation to produce stable records
some beneficial effects of the occlusal splint may be psychologic and based on congnitive awareness, allows for optimal positioning of the condyles and discourages bruxism through elimination of the habitual dysfunctional patterns of the teeth |
|
|
How do they work?
|
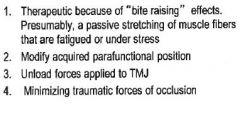
|
|
|
Stabilizing Occlusal Splints Indications
|
1. patients with tmj or muscle disorders such as bruxism
2. Diagnosis and treatment of trauma from occlusion 1 3. Establishment of the optimal condylar position in centric relation prior to definitive occlusal therapy 4. Stabilization of mobile teeth by mainting them in stable position 5. Holding maxillary teeth in the desired position following orthodontic therapy or loss of opposing teeth 6. temporary disocclision of teeth for orthodontic or other purpose 7. differential diagnosis in patients with signs and symptoms imitating TMJ or muscle 8. treatment of headaches caused by neurousclar tension |
|
|
Full Coverage: Advantages
|
1. worn continuously w/o tooth movement
2. good for bruxism, even if uncontrolled 3. can be worn on maxillary of mandibular teeth |
|
|
Full Coverage: Disadvantages
|
1. longer adjustment period
2. patients with jaw pain and manipulation during adjustment difficult 3. commercial lab fee |
|
|
occlusal scheme full coverage appliance
|
stabilizing splint with stops for all opposing teeth and controlled cuspid rise
|
|
|
Partial Coverage: Advantages
|
Good diagnostic device
Easy adjustment and more acceptable to patients with jaw pain Lack of bulk makes it easier to wear |
|
|
Partial Coverage: Disadvantages
|
Should not be worn for extended periods of time
Less acceptable by patient because palatal coverage is necessary |
|
|
Functional Activities: Force of contact
|
17,200 lb-sec/day
|
|
|
Functional Activities: Direction of Force to teeth
|
Vertical-tolerated
|
|
|
Functional Activities: Mandibular position
|
C.O.-stable
|
|
|
Functional Activities: Protective relfexes influence
|
present
|
|
|
Functional Activities: Pathology
|
unlikely
|
|
|
Para-Functional Activities: Force of Contact
|
57,600 lb-sec/day
|
|
|
Para-Functional Activities: Direction of force to teeth
|
horizontal-not tolerated
|
|
|
Para-Functional Activities: Mandibular position
|
Eccentric-unstable
|
|
|
Para-Functional Activities: Protective reflexes influence
|
absent
|
|
|
Para-Functional Activities: Pathology
|
highly likely
|
|
|
involuntary activity of the jaw musclature characterised by parafunctional activities such as jae clencing, tooth gnashing, and grinding
|
bruxism
|
|
|
Awake Bruxism
|
Unrelated to sleep bruxism
•Ususally occurs subconsciouly without cognitive awareness, however, it is under voluntary control •Protective reflexes intact •Often occurs during periods of concentration , exertion, stress, anxiety of grinding •May accompany other types of parafunctional oral habits such as cheek biting, tongue posturing, nail biting, lip biting, jaw bracing or posturing •20% are aware of at least occasional daytime clenching |
|
|
Sleep Bruxism
|
•(International Classifacation of Sleep Disorders)
ICSD -2 (2005) : Sleep bruxism was re-classified as a sleep-related movement disorder (relatively simple, usually stereotyped movements that disturb sleep and are less complex that other parasomnias) •An oral activity characterized by grinding or clenching of the teeth during sleep •Usually associated with microarousals • Often seen in lighter stages of sleep • Change in sympathetic-parasympathetic activity • Tonic muscle contractions = clenching • Phasic, repetitive muscle contractions = grinding •Not under voluntary control •Protective reflexes decreased |
|
|
Sleep Bruxism Etiology
|
The most accepted theory of SB is that it is a movement disorder involving a cascade of physiological events characterized by autonomic-cardiac activities as related to sleep arousal.
|
|
|
NREM Bruxism
|
Stage 1: Transitional lighter sleep
•Stage 2: Deeper sleep •Stage 3: Slow wave activity •Stage 4: Slow wave activity •Stages 3 and 4 are referred to as slow-wave sleep or delta sleep •Parasympathetic nervous system predominates. Hormonal changes to promote anabolism. Protein synthesis and tissue repair. Restorative period |
|
|
REM Bruxism
|
•“Dream” stage
•Sympathetic nervous system predominates •– Increased oxygen consumption •– Increased BP, pulse, respirations, CO •Increased chance of plaque rupture due to surges in pressure and changes in coronary artery tone |
|
|
Bruxism: Diagnosis Based on History
|
Self Awareness
•Report of witnessed sounds of tooth grinding or tapping •Jaw discomfort, fatigue or stiffness in the morning •Morning headache •Generalized sensitivity of the teeth to cold |
|
|
Bruxism: Diagnosis Based on Clinical Findings
|
•Tooth wear (100% of bruxers; 40% of nonbruxers)
•Masseter muscle hypertrophy •Mandibular angle hypertrophy on panoramic radiograph •Masticatory muscle tenderness to palpation •TMJ tenderness to palpation •Maxillary exostosis and mandibular tori •Other evidence of parafunctional jaw activity (tongue scalloping/buccal mucosal lesions) |
|
|
2 types of Sleep Bruxism
|
1.Idiopathic: without clear cause
2.Secondary Bruxism: Associated with an identifiable cause; may also occur while awake |
|
|
2 types of Secondary Bruxism
|
a)Drug induced (alcohol, caffeine, cigarettes, SSRI, cocaine, ecstacy)
b)Medical disorders (cerebral palsy, Parkinson’s disease, mental retardation, autism) |
|
|
Evidence of Bruxism
|
1. excessive tooth wear
2. fractured tooth structure or restoration 3. tooth sensitivity 4. tooth mobility 5. pulp necrosis 6. abfractions 7. alveolar exostosis and tori 8. periodontal bone loss 9. masticatory muscle hypertrophy 10. muscle pain and headache 11. traumatic ulcer 12. linea alba and tongue indentation |
|
|
Management of Bruxism
|
Identify the cause and work toward reducing factors
behavioral modifications occlusal appliances pharmacology |
|
|
Behavioral Modifications
|
1.Avoidance of known triggers (smoking, caffeine, SSRIs)
2.Stress management (hypnosis, biofeedback) 3.Sleep Hygiene education 4.Change sleep position |
|
|
Occlusal Splints-management
|
Comprehensive reviews by Dao et al and Kato et al conclude that splints are useful adjuncts in the management of sleep bruxism, but are NOT DEFINITIVE treatment
|
|
|
PHARMACOTHERAPY
|
The short term use of pharmacotherapy aimed at reducing sleep onset, increasing sleep continuity and total sleep time has been helpful in managing sleep disturbances, including bruxism.
1) muscle relaxants ( Methocarbamol; Robaxin) 2)Benzodiazepines ( Valium) 3)low dose of tricyclic antidepressants |

