![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
121 Cards in this Set
- Front
- Back
|
Paget's disease of the vulva
|
-intraepithelial pre-invasive neoplasia
-20% have coexisting adenocarcenoma -long-standing pruritis -velvety red lesions that scar into white plaques Tx:wide local excision (high recurrence rate) -likely fatal if spreads to nodes |
|
|
Vulvar intraepithelial neoplasia
|
VIN
-associated with HPV, condyloma, smoking, obesity, htn -20% have coexistent invasive carcinoma -50% asymptomatic. others: vulvar pruritis or irritation -variable lesions Tx: wide local excision, f/u colposcopies q3months |
|
|
Vulvar cancer
|
-majority are SCC
-pruritis, pain, bleeding -may have a mass, anywhere, but commonly on labia majora -prognostic indicator: inguinal nodes Tx: wide excision, inguinal node dissection; may irradiate |
|
|
Vaginal intraepithelial neoplasia
|
-VAIN (I, II, III: carcinoma in situ)
-associated with CIN, HPV, condylomas -pts in mid to late 40s -pap smear, colposcopy Tx: local resection, laser vaporization. 5FU for multifocal lesions. follow with colposcopies |
|
|
Vaginal cancer
|
-usu SCC
-present with pruritis, post-menopausal bleeding -pap, colpo, biopsy Tx: Stage I and II local resection. Stage III and IV radiation only. |
|
|
Classification of cervical changes
|
CIN: cervical intraepithelial neoplasia (I, II, III)
CIS: carcinoma in situ LSIL / HSIL: low/high grade squamous intraepithelial lesion ASC: atypical squamous cells (US unknown significance, H can't rule out high grade) |
|
|
Tx of cervical dysplasia
|
CKC: cold knife cone, not usually used any more
LEEP: loop electrosurgical excision procedure Lletz: large loop excision of the transformation zone |
|
|
Endometrial cancer epidemiology
|
The most common and curable gyn cancer
Younger women: perimenopausal, chronic estrogen exposure, estrogen dependent. begins with endometrial hyperplasia. favorable prognosis Older women: estrogen independent. thin post-menopausal women Histologic grade is most important prognostic factor |
|
|
Endometrial cancer: presentation and tx
|
-presents with postmenopausal bleeding
-normal pelvic exam -Dx: endometrial biopsy. -workup: TSH, prolactin, FSH, Pap, pelvic US. Tx: sx staging, total abdominal hysterectomy, bilateral salpingo-oophorectomy for all stages. lymph node sampling (pelvic, para-aortic). high dose progestins |
|
|
DDx of Postmenopausal Bleeding
|
-endometrial atrophy
-exogenous estrogen/HRT -endometrial cancer -endometrial or cervical polyps -endometrial hyperplasia -miscellaneous |
|
|
most common genital tract cancers
|
1. Endometrial (most curable)
2. Cervical 3. Ovarian (25%, but 50% of deaths) |
|
|
ovarian cancers
|
-90% from epithelium
-krukenberg: mets to ovary -carcinomatous ileus: intraperitoneal spread causes intermittent bowel obstruction -presentation: usu asymp, may have vague lower abd pain, solid fixed mass -Dx: pelvic ultrasound |
|
|
ovarian epithelial tumors
|
-usu serous cystadenocarcinoma
-65% bilateral -56 to 60 yrs -frequent recurrene 75% are stage III/IV at dx Tx: Sx: TAHBSO (tot abd hysterect bilat salpingo-oophorectomy, carboplatin/paclitaxel |
|
|
ovarian germ cell tumors
|
-dysgerminoma (50%)
-immature teratoma (20%) -usu early stage at dx, generally curable. 95% are benign -rarely bilateral -serum markers, women under 20 present with unilateral rapidly enlarging adnexal mass Tx: unilateral salpingo-oophorectomy, chemo (BEP) |
|
|
meig's syndrome
|
ovarian tumor
ascites rt hydrothorax |
|
|
gonadal stromal cell tumors
|
-low grade, any age, do not recur
-granulosa-theca (70%) produce estrogen -sertoli-leydig (rare) produce testosterone -present with hormonal effects Tx: unilateral salpingo-oo, no chemo/rads |
|
|
fallopian tube cancer
|
-adenocarcinoma arising from the mucosa
-usu asymp -classic triad: profuse watery d/c, pelvic pain, pelvic mass (seen in only 15%) Tx: as ovarian ca: TAHBSO, omentectomy, chemo |
|
|
Complete molar pregnancy
|
-benign gestational trophoblastic dz
-fertilization of an enucleate ovum -heavy bleeding in early pregnancy -high B-hCG, hyperemesis gravidarum, preeclampsia prior to 22 wks -US "snowstorm", maybe bilat. theca lutein cysts Tx: D&E (suction evacuation), IV oxytocin. RhoGAM for Rh- moms -close f/u of B-hcg levels. persistent dz in 15-25% of pts. |
|
|
Incomplete molar pregnancy
|
-benign gestational trophoblastic dz
-normal ovum fertilized by 2 sperm -most common: 69XXY -placental abmormalities coexist with triploid fetus -pts usu present with vaginal bleeding from missed abortions -very high B-hCG levels -D&E, f/u B-hCG |
|
|
Malignant Gestational Trophoblastic Dz (GTD)
|
-persistent/invasive moles (75%)
-choriocarcinoma (25%) -PSTT (placental site trophoblastic tumor) (extremely rare) -50% occur months to yrs after molar pg -25% occur after normal pg -25% occur after miscarriage, ectopic pg, or abortion Dx: pelvic US, B-hCG levels. Look for signs of mets: CBC, coag and renal studies, liver and thyroid fx, abd/pelvic CT, CXR Tx: v. sensitive to single-agent chemo (methotrexate or actinomycin-D). multi-agent if poor prognosis. |
|
|
Choriocarcinoma
|
-malignant necrotizing tumor arising from trophoblastic tissue weeks to months after any type of gestation
-sheets of anaplastic cytotrophoblasts and syncytiotrophoblasts in the absence of chorionic villi -often mets hematogenously to nearly any tissue ("the great imitator") |
|
|
bloody nipple discharge
|
intraductal papilloma
invasive papillary cancer |
|
|
galactorrhea
|
pregnancy
pituitary adenoma acromegaly hypothyroidism stress medications |
|
|
serous nipple discharge
|
normal menses
OCPs fibrocystic change early pg |
|
|
yellow-tinged nipple discharge
|
fibrocystic change
galactocele |
|
|
green, sticky nipple discharge
|
duct ectasia
|
|
|
fibrocystic change of the breast
|
-painful breast masses
-often multiple, ususally bilateral -not associated with increased ca risk -usu 30-40 yrs, but can occur at any age |
|
|
fibroadenoma of the breast
|
-20-35 yrs
-most common benign breast tumor -round, rubbery, mobile, non-tender, usu solitary -follow if clinically stable, or FNA |
|
|
cystosarcoma phyllodes
|
-rare fibroadenoma of the breast
-rapidly growing, large, bulky, mobile mass (4-5 cm) -10% contain malignant cells -wide local excision |
|
|
intraductal papilloma
|
-benign solitary lesion
-epithelial lining of lactiferous ducts -bloody nipple discharge -r/o invasive papillary carcinoma -Tx: excision of involved ducts |
|
|
mammary duct ectasia (plasma cell mastitis)
|
-inflammation of ductal system, often bilateral
-infiltration of plasma cells -at or after menopause -green, sticky nipple discharge -breast pain, nipple retraction, or subareolar masses -Tx: local excision |
|
|
Non-invasive breast cancer
|
Ductal Carcinoma in Situ
-higher potential to invade than LCIS -mammogram: clustered microcalcifications -Tx: excision, occasionally astectomy Lobular Carcinoma in Situ -bilateral 50-90% -not palpable or visible by mammography -increased risk of subsequent invasive ca -Tx: local excision |
|
|
Invasive breast cancer
|
1) Infiltrating Ductal Carcinoma
-most common breast malignancy 2) Invasive Lobular Carcinoma -tends to be bilateral 3) Inflammatory Breast Carcinoma -extremely aggressive 4) Paget's dz of Nipple -often concomitant with DCIS or invasive carcinoma -eczematous changes: crusting, scaling, erosion, discharge |
|
|
Non-invasive breast cancer
|
Ductal Carcinoma in Situ
-higher potential to invade than LCIS -mammogram: clustered microcalcifications -Tx: excision, occasionally astectomy Lobular Carcinoma in Situ -bilateral 50-90% -not palpable or visible by mammography -increased risk of subsequent invasive ca -Tx: local excision |
|
|
Invasive breast cancer
|
1) Infiltrating Ductal Carcinoma
-most common breast malignancy 2) Invasive Lobular Carcinoma -tends to be bilateral 3) Inflammatory Breast Carcinoma -extremely aggressive 4) Paget's dz of Nipple -often concomitant with DCIS or invasive carcinoma -eczematous changes: crusting, scaling, erosion, discharge |
|
|
Dating Pregnancy
|
Nagele rule for EDC/EDD
-Subtract 3 months from date of LMP and add 7 days. US: +/- 1 week in 1st trimester +/- 2 weeks in 2nd trimester +/- 3 weeks in 3rd trimester |
|
|
Physiologic changes during pregnancy
|
-CO increases 30-50%
-SVR and BP decrease (progesterone decreases smooth muscle tone) -blood volume increases by 50% -prolonged gastric emptying and decreased GE sphincter tone -Kidneys increase in size, ureters dilate -hypercoagulable state although clotting and bleeding times do not change |
|
|
Hormone production during pg
|
-hyperestrogenic state (placenta produces estrogens) Estrogens increase TBG.
-placenta produces hCG which stimulates progesterone production by the corpus luteum -human placental lactogen (hPL or hCS) maintains nutrient supply. increases circulating FFAs, insulin antagonist |
|
|
Tests/screening at initial prenatal visit
|
CBC
blood type and screen RPR for syphilis rubella antibody screen hep B surface antigen pap/chlamydia/gonorrhea offer HIV testing UA/UCx PPD nuchal translucency |
|
|
maternal serum alpha fetoprotein
|
-MSAFP
-15-18 wks -elevation = incr risk of neural tube defects -decrease seen in some aneuploidies including down's |
|
|
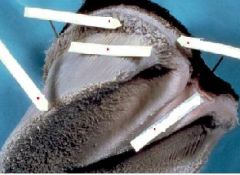
Incompetent cervix
|
Risk factors: sx, other cervical trauma, DES exposure, congenital cervical abnormality
Tx: tocolysis, emergent cerclage (suture placed vaginally around cervix) |
|
|
Trisomy Screening
|
1st Trimester:
-nuchal translucency -B-hCG, PAPP-A Second Trimester: Quad Screen -AFP (decreased) -hCG (elevated in t21, decreased in t18) -Estriol (decreased) -Inhibin-A |
|
|
spina bifida
|
US findings:
-"lemon" sign (concave frontal bones) -"banana" sign (flattened cerebellum) -ventriculomegaly -club feet -mom with MTHFR mutation doubles risk -AFP screening |
|
|
ROM
|
PROM:
-1 hour prior to onset of labor -10% of pregnancies -PPROM: preterm PROM (<37 wks) -pool, nitrazine, fern tests |
|
|
Cardinal movements of labor
|
engagement
descent flexion internal rotation (OT to OA) extension external rotation |
|
|
Stages of labor
|
1st stage: onset to 10 cm
-latent phase (to 3-4 cm) -active phase: at least 1-1.2 cm/hr -10-12 hrs for nulliparous (up to 20) 6-8 hrs for multiparous (up to 12) 2nd stage: 10 cm to delivery -prolonged if >2 hrs nulliparous (3 with epidural), >1 hr multiparous (2 with epidural) |
|
|
placental abnormalities
|
previa (complete, partial, marginal)
-painless vaginal bleeding -sentinel bleed ab 28 wks -vag exam contraindicated -dx: ultrasonography placental invasion -accreta: superficial -increta: invades myometrium -percreta: invades through myometrium to uterine serosa |
|
|
mgmt of placenta previa
|
-stabilize pt
-prepare for catastrophic hemorrhage -prepare for preterm delivery complications -prematurit -PROM -IUGR -malpresentation -vasa previa -congenital abnormalities |
|
|
placental abruption
|
-strong association with htn
-3rd trim bleeding with severe abd pain -small frequent or tetanic contractions -Couvelaire uterous at c-sx -ultrasonography to r/o p. previa -vaginal delivery is preferred |
|
|
velamentous cord insertion
|
blood vessels insert between amnion and chorion, away from the placenta
|
|
|
succenturiate placenta
|
accessory lobe: 1 lobe of placenta is implanted in a different portion of the uterine wall
|
|
|
Trisomy Screening
|
1st Trimester:
-nuchal translucency -B-hCG, PAPP-A Second Trimester: Quad Screen -AFP (decreased) -hCG (elevated in t21, decreased in t18) -Estriol (decreased) -Inhibin-A |
|
|
spina bifida
|
US findings:
-"lemon" sign (concave frontal bones) -"banana" sign (flattened cerebellum) -ventriculomegaly -club feet -mom with MTHFR mutation doubles risk -AFP screening |
|
|
ROM
|
PROM:
-1 hour prior to onset of labor -10% of pregnancies -PPROM: preterm PROM (<37 wks) -pool, nitrazine, fern tests |
|
|
Cardinal movements of labor
|
engagement
descent flexion internal rotation (OT to OA) extension external rotation |
|
|
Stages of labor
|
1st stage: onset to 10 cm
-latent phase (to 3-4 cm) -active phase: at least 1-1.2 cm/hr -10-12 hrs for nulliparous (up to 20) 6-8 hrs for multiparous (up to 12) 2nd stage: 10 cm to delivery -prolonged if >2 hrs nulliparous (3 with epidural), >1 hr multiparous (2 with epidural) |
|
|
Tocolysis
|
Attempts to prevent contractions/labor
-beta-mimetics: ritodrine, terbutaline -Mg sulfate: calcium antag and membrane stabilizer -CCBs -indomethacin (NSAID, prostaglandin inhibitor) -hydration (ADH may cross-react with oxytocin receptors) -if labor can be delayed for 48 hrs, betaethasone can enhance lung maturity |
|
|
When preterm labor should be allowed to progress
|
-chorioamnionitis
-nonreassuring fetal testing -placental abruption (also consider maternal disease, risks) |
|
|
Timing of IUGR
|
Insult before 20 weeks
-hyperplastic growth -symmetric growth restriction Insult after 20 weeks -hypertrophic growth -asymmetric growth restriction |
|
|
doppler study of umbilical artery in IUGR
|
-Normal flow higher during systole
-decreases 50-80% during diastole -Absent or reversed diastolic flow associated with high risk of fetal demise |
|
|
antenatal testing of SGA infant
|
NST: non-stress test
OCT: oxytocin challenge test BPP: biophysical profile |
|
|
UTI bugs in pregnancy
|
70% E. coli
Also: klebsiella, enterococcus, proteus, coag-neg staph, gbs. Rx: amox, nitrofurantoin or trim/sulfa. Pyridium for dysuria |
|
|
Pyelonephritis in pregnancy
|
complication of 1-2% of pregnancies
risks: septic shock, ARDS treat aggressively, often with IV amp/gent |
|
|
GBS in pregnancy
|
-UTIs, chorioamnionitis, endomyometritis
-neonatal sepsis -screening between wks 36 and 37 -pos screen: IV penicillin G or amp during labor. clinda for pcn allergies |
|
|
Chorioamnionitis
|
-w/ or w/o PROM/PPROM
-sequelae: endomyometritis, septic shock -fetal tachycardia -GS dx: amniotic fluid Cx. alt screening: IL6 levels in amniotic fluid Rx: IV abx |
|
|
DDx: fetal tachycardia
|
-chorioamnionitis
-B-agonist tocolytics -other meds administered to mom |
|
|
HSV in pregnancy/labor
|
-if outbreak, prophylaxis wks 36 to delivery
-if lesions: c-section -Infections in neonate: herpetic lesions skin and mouth, sepsis, pna, herpes encephalitis |
|
|
VZV in pregnancy
|
-vertical transmission: transplacental
-1st trimester: risk of abortion, poss teratogen -near term: postnatal infection (benign or fulminant) -VZIG may prevent transmission |
|
|
Parvovirus in pg
|
-fifth dz/slapped cheeks
-attacks fetal erythrcytes -1st trimester: abortion -2nd/3rd trimester: fetal hydrops -doppler US: peak systolic velocity of the MCA to ID fetal anemia/hemolysis |
|
|
CMV in pg
|
-in utero infections in 1% of newborns, 10% of which will result in clinical illness
-HSM, thrombocytopenia, jaundice, cerebral calcifications, chorioretinitis, interstitial pneumonitis -infected infants: mortality up to 30%, mental retardation, hearing loss, neuromuscular d/o |
|
|
Rubella in pg
|
-congenital rubella syndrome (CRS)
-deafness, cardiac abnormalities, cataracts, mental retardation -IgM titers (IgM doesn't cross placenta) - |
|
|
HIV in pg
|
-treatment reduces transmission from 25% to 1-2%
-c-section reduces transmission by 2/3 -triple therapy or HAART |
|
|
Hep B in pg
|
-HBsAg: sign of chronic dz
-if positive: HepB Ig at birth, 3 mo, 6 mo -Exposure in pg: HepB Ig to mom |
|
|
Syphilis in pg
|
-latent: may not transmit dz
-1* or 2* dz: more likely to transmit -early congenital syphilis: maculopapular rash, snuffles, HSM, hemolysis, LAD, jaundice -Rx: penicillin -late congenital syphilis: 8th CN deafness, saber shins, Hutchinson's teeth, saddle nose |
|
|
toxoplasmosis
|
-transplacental transmission
-Transmission most common if dz in 3rd trimester -if earlier transmission: more severe congenital infection: fevers, seizures, chorioretinitis, hydrocephaly, microcephaly, HSM, jaundice -Dx: IgM in neonate, IgG screening in mom -Rx: spiramycin |
|
|
Hyperemesis gravidarum
|
-hypochloremic alkalosis is common, give NS with 5% dextrose
-anti-emetics -frequent small meals -corticosteroids |
|
|
Seizure d/o in pg
|
-increase in seizure frequency in many pregnancies (estrogen, rapid hepatic metabolism, increased blood volume, stress)
-risk of fetal malf (w/ or w/o AED use) -cleft lip and palate, cardiac, NTDs, GDD -level II fetal survey at 19-20 wks -check AED levels monthly -phenytoin is DOC for L&D |
|
|
Cardiac meds and pregnancy
|
-ACE inhibitors, diuretics, coumadin associated with congenital anomalies, usually d/c'd
-newer anti-HTN and antiarrhythmics have little experience in pg and are commonly avoided -early epidural to diminish pain response -assisted vaginal delivery to diminish valsalva effects |
|
|
Cardiac conditions with poor prognosis in pg
|
-right to left shunts (PDA & VSD most common)
-pulm HTN -mortality rates 50% and higher -most dangerous: 2-4 wks postpartum |
|
|
Marfan's in pg
|
hyperdynamic state of pg leads to:
-increased risk of aortic dissection and/or rupture -increased risk of valvular complications -Tx: sedentary lifestyle, B-blockers |
|
|
peripartum cardiomyopathy (PPCM)
|
-classic s/s of dilated CM, heart failure
-EF 20-40% -usually induce if >34 weeks - > half pts return to baseline |
|
|
Chronic renal dz in pg
|
-increased risk of preeclampsia, preterm delivery, IUGR, worsening renal dz
-screen every trimester with 24 hr cr cl and protein -hard to dx preeclampsia if baseline proteinuria and HTN. take baseline uric acid |
|
|
Coagulation in pg
|
-PG is considered "hypercoagulable state"
-increased clotting factor production (except XI and XIII) -fibrinogen turnover time is decreased -endothelial damage -> collagen exposure -venous stasis due to decreased venous tone and compression of IVC by uterus -Tx: DVT, mild PE: heparin (coumadin contraindicated in pg) -Tx: massive PE: streptokinase |
|
|
Thyroid dz in pg
|
Graves dz:
-continue propylthiouracil or methimazole -maintain low TSI and TSH levels to reduce risk of fetal goiter Hashimoto thyroiditis -maintain low TSH levels with Synthroid |
|
|
SLE/ collagen vascular d/o in pg
|
-dz state in mother: 1/3 worsen, 1/3 improve, 1/3 unchanged
-continue aspirin, corticosteroids -d/c cyclophosphamide, mtx Fetal loss common, esp 2nd trimester -placental thrombosis -IUGR Lupus flare vs. preeclampsia -both mediated by Ab/Ag complexes -lupus flare: reduced C3, C4 Neonatal lupus -Anti-Ro (SSA), anti-La (SSB) |
|
|
Cocaine in pg
|
-abruptio placentae, IUGR, preterm L&D
-cerebral infarction, developmental delay |
|
|
Opiates in pg
|
-heroin, methadone
-no known teratogenic effects of narcotics -heroin withdrawal syndrome can cause miscarriage, preterm delivery, fetal death -enroll pt in methadone program |
|
|
Postpartum care
|
-perineal or c-section care
-pain control -6 wks pelvic rest -breast feeding: let down @ 24-72 hrs, breasts will be warm, firm, tender. progesterone only mini-pill, norplant or depo-provera. |
|
|
Postpartum hemorrage
|
- > 500 ml in vaginal delivery
- > 1000 ml in c-section -Causes: uterine atony, retained POCs, placenta accreta, cervical or vaginal lacerations -Sheehan syndrome: pituitary infarction, absence of lactation 2* to blood loss |
|
|
postpartum uterine atony
|
Higher risk:
-chorioamnionitis, mg sulfate exposure, multiple gestations, multiparous, macrosomia, uterine abnormalities/fibroids Tx: IV oxytocin, uterine massage Next steps: methergine (not in HTN), then prostin (PGF 2a, not in asthma) Refractory: D&C to r/o retained POCs |
|
|
Endomyometritis
|
-polymicrobial infection of uterine lining
-more likely after c-section, meconium, chorioamnionitis, PPROM Dx: fever, elevated WBCs, uterine tenderness 5-10 days postpartum. US of uterine contents Tx: triple abx. D&C if POCs on US |
|
|
Elective Abortion stats
|
-1/3 women under 20
-1/3 women 20-24 -1/3 women 25 and over -85% in 1st trimester -90% before 12 weeks -95% before 16 weeks -97% suction curettage -3% medical (mifepristone or mtx with prostaglandin analogue misoprostol) |
|
|
Risk factors for macrosomic infants
|
Diabetes
maternal obesity possterm previous LGA multiparity AMA Beckwith-Wiedemann syndrome |
|
|
Risks of macrosomia
|
To infant:
-childhood leukemia -wilms tumor -osteosarcoma -hypoglycemia -jaundice -lower Apgar scores To mother: -c section -perineal trauma -hemorrhage |
|
|
AFI
|
Amniotic fluid index
< 5 oligohydrammios > 20 or 25 polyhydramnios |
|
|
Erythroblastosis fetalis
|
Caused by serious anemia, often due to Rh-related hemolysis
-hyperdynamic state -heart failure -diffuse edema -ascites -pericardial effusion |
|
|
RhoGAM
|
-anti-D immunoglobulin (Rh IgG)
-give any time mom may be exposed to fetal blood (amniocentesis, miscarriage, vaginal bleeding, abruption, delivery) -Standard dose (0.3 mg) eradicates 15 mL of fetal RBCs -Kleihauer-Betke test for amount of fetal rbcs in maternal circulation |
|
|
Sensitized Rh-neg patient
|
-Rh Ab titer > 1:16 associated with fetal hydrops
-Recheck titer every 4 weeks -if > 1:16, serial amniocenteses, check by OD450 -can also check doppler flow of MCA |
|
|
Fetal Demise
|
< 20 wks: D&E
> 20 wks: induction -Test for cause (collagen vascular dz, hypercoagulable state, fetal karyotype, TORCH if > 4 weeks, release of thromboplastic substances can result in hypofibrinogenemia or DIC |
|
|
Conditions associated with postterm pg
|
Diminished levels of circulating estrogen
-anencephaly -fetal adrenal hypoplasia -absent fetal pituitary |
|
|
Complications of multiple gestation
|
-preterm labor
-placenta previa -cord prolapse -hemorrhage -cervical incompetence -gestational diabetes -preeclampsia |
|
|
Twin-to-twin transfusion syndrome
|
-Mo-Di twins: serial US every 2 weeks
-one small, anemic, hypovolemic twin -one large, polycythemic, hypervolemic twin with cardiomegaly, glomerulotubal hypertrophy, edema, ascites |
|
|
Preeclampsia
|
-nondependent edema, HTN, proteinuria
-classic: nulliparous, 3rd trim -generalized arteriolar constriction -general transudative edema leading to hypovolemia |
|
|
Fetal complications of preeclampsia
|
-prematurity
-decreased blood flow -uteroplacental insufficiency leading to abruption or fetal distress -IUGR |
|
|
Maternal complications of preeclampsia
|
Related to vasoconstriction:
-seizure and stroke -oliguria and renal failure -pulmonary edema -liver edema or subcapsular hematoma -thrombocytopenia, DIC |
|
|
HELLP syndrome
|
-subcategory of preeclampsia
-hemolysis, elevated liver enzymes, low platelets -poor maternal and fetal outcomes -epigastric pain, n/v -screen for acute fatty liver of pg |
|
|
Acute fatty liver of pg (AFLP)
|
> 50% have htn and proteinuria
Labs differentiate from HELLP: -elevated ammonia -glucose < 50 -reduced fibrinogen and ATIII levels Tx: supportive |
|
|
Preeclampsia treatment
|
-delivery is ultimate tx
-betamethasone to enhance lung maturity -if mild: may start mg sulfate for seizure prophylaxis -if severe: goal to prevent eclampsia, control maternal bp, deliver. mg sulfate and hydralazine |
|
|
Eclampsia
|
-grand mal seizure in pre-eclamptic patient
-Complications: cerebral hemorrhage, aspiration pna, hypoxic encephalopathy, thromboembolic events |
|
HTN management in pg
|

labetalol
nifedipine |
|
|
Risks to fetus in GDM
|
-macrosomia
-hypoglycemia -hypocalcemia -hyperbilirubinemia -polycythemia |
|
|
GDM
|
-usually related to size of placenta; occurs in 3rd trimester
-screen between 24 and 28 wks -Tx: diabetic diet, mild exercise, monitor sugars. insulin or oral hypoglycemic agent may be added -50% will have GDM in subsequent pg -25-30% will develop DM w/i 5 yrs |
|
|
Pregestational DM
|
-4x increased risk of preeclampsia
-2x increased risk of SAB -incr risk of infection, hydramnios, hemorrhage, c/s -5x increased risk of fetal death -2-3x increased rate of malf., including neural tube -delayed organ maturity |
|
|
Type 1 DM in pg
|
-very poor outcomes
-Screening: ECG, 24 hr urine for CrCl and protein, HgbA1C, TSH |
|
|
Fetal testing in pregestational DM
|
-testing begins at 32 weeks
-weekly NSTs until 36 wks, then add weekly BPPs -may elect to deliver btwn 37 and 39 wks if lungs mature |
|
|
Endometriosis
|
-Theories: lymphatic spread, retrograde menstruation, metaplastic transformation
-cyclic pelvic pain: 1-2 wks before menses until onset of flow -dysmenorrhea, dyspareunia, abnormal bleeding, infertility |
|
|
Endometriosis Tx
|
-"pseudopregnancy" NSAIDs, OCPs, medroxyprogesterone (Megace)
-"pseudomemopause" danazol/Danocrine (androgen) or Leupron, nafarelin/Synarel (GnRH agonist) -Rx may cause estrogen def. -Sx: ablation/excision or TAHBSO |
|
|
Adenomyosis
|
-extension of endometrium into myometrium
-basalis layer extends, so not responsive to cyclic changes -asymp or 2* dysmenorrhea or menorrhagia -Dx: endometrial biopsy and TSH to r/o other causes of irregular menses -Adenomyosis, endometriosis, and uterine fibroids frequently coexist |
|
|
DDx for uterine enlargement, menorrhagia and/or dysmenorrhea
|
-uterine fibroids
-polyps -menstrual d/o's -endometrial hyperplasia -endometrial ca -pregnancy -adnexal masses |
|
|
Order of events in puberty
|
-adrenarche (6-8 yrs, regen of zona reticularis of adrenal gland and production of androgens)
-gonadarche (8 yrs: GnRH stimulates ant pituitary to secrete LH and FSH) -thelarche -pubarche -peak height velocity -menarche |
|
|
Follicular phase
|
-withdrawal of est/progest from previous cycle
-gradual increase in FSH -FSH stimulates follicles -follicle produces estrogen -estrogen stim FSH and LH receptors |

