![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
208 Cards in this Set
- Front
- Back
|
physiological changes preceding labor:
|
backache: low dull backache,pelvic muscle relaxation
weight loss: 1-3 lbs lightening: 14 days fetus dropped--> easier breathing, more pressure on bladder---> urinary frequency contractions: irregular uterine contractions bloody show: brownish blood tinged mucus--> mucus plug discharged---> from dilation and effacement energy burst: "nesting" GI changes: less N&V or indigestion rupture of membranes: spontaneous |
|
|
RUPTURE OF MEMBRANES
|
- usually happens 24 hours before labor
- prolonged---> infection - immediately check FHR--> decelerations - should be watery, clear, and pale to straw yellow color - odor SHOULD NOT BE FOUL - volume is between 500-1200ml - nitrazine paper---> blue |
|
|
what are the five P?
|
- passenger
-presentation -passageway -powers -postion |
|
|
passenger
|
fetus and placenta
- size of fetal head, fetal presentation, lie attitude, position |
|
|
what does presentation mean?
|
the part of the fetus that entering the pelvic inlet FIRST, It can be the head (occiput), chin (mentum), shoulder (scapula), or breech (sacrum or feet)
|
|
|
what does the lie mean?
|
2 types: transverse, or parellel (longitudinal)
the relationship of the maternal longitudinal axis spine to the fetal longitudinal axis (spine) - transverse: get long axis is horizontal and forms a right angle to maternal axis---> no vaginal birth, usually the shoulder is the presenting part---> cesarean - parellel or longitudinal: fetal long axis is parallel to maternal axis, either cephalic or breech presentation |
|
|
what does attitude mean?
|
relationship of fetal body parts to one another
fetal flexion: chin flexed to chest, extremities flexed into torso fetal etension: chin extended away from chest, extremities extended - fetopelvic or fetal position: the relationship of the presenting part of the fetus ( sacrum, mentum, or occiput) to its directional position as it relates to one of the four maternal pelvic quadrants - first letter: R, or L of maternal pelvis second letter: presenting part O, S, M or Sc (scapula) third letter: references A for anterior, P for posterior, or T for transverse - station: measurement of fetal descent in cm with station 0 being at the level of imaginary line at the level of the ischial spines, minus--> superior to ischial spine, plus--> inferior to the ischial spines |
|
|
what is passageway?
|
birth canal is composed of the bony pelvis, cervix, pelvic floor, vagina, introits (vaginal opening), the size and shape of the bony pelvis must be adequate to allow the fetus to pass
- cervix must be dilating and contractions |
|
|
what is powers?
|
uterine contractions cause effacement and dilation of the cervix and the descent of the fetus
- involuntary urge to push and voluntary bearing down in the second stage of labor helps in the expulsion of the fetus |
|
|
position
|
it is the position the woman is during labor, the client should engage in frequent position changes during labor to increase comfort, relieve fatigue, and promote circulation,
- gravity can aid in the fetal descent upright, sitting, kneeling, and squatting positions |
|
|
leopold manuevers
|
abdominal palpation of the number of fetuses, the fetal presenting part, lie, attitude, descent and probable location of where the fetus is and where the fetal heart tone be can auscultated
first maneuver: what part of the fetus is located in the fundus and uterus second manuever: determine the location of the fetal back third maneuver: presenting part fourth manuever: determine the location of the cephalic prominence |
|
|
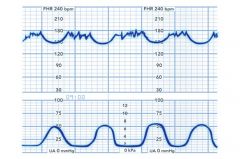
tocotransducer or external electronic monitoring
|
separate transducer apple to the maternal abdomen over the fundus that measures uterine activity
- uterine contraction patterns - must be repositioned with maternal movement to ensure good placement -15-20 mmhg when uterus is relaxed |
|
|
external fetal monitoring (EFM)
|
transducer applied to the abdomen of the client to asses FHR patterns during labor and birth
|
|
|
what are some labs we have to do preceding labor and birth?
|
group B streptococcus: obtained at 36-37 weeks, if positive give prophylactic antibiotics
- urinalysis: clean- catch urine to see: hydration status-->specific gravity nutrition status--> ketones proteinnuria--> gestational HTN UTI infection---> bacterial count blood test: HCT level, ABO typing and RH factor |
|
|
what can you do as a nurse before baby is born?
|
ROM---> check temp every 1-2
asses FHR ---> EFM or spiral electrode on fetal scalp uterine contraction--> place hand on fundus contraction frequency, duration, intensity |
|
|
when assessing for the uterine contractions you look at frequency, duration, and intensity what do those mean?
|
frequency: beginning of one contraction to the beginning of the next
- duration: the time between the beginning of a contraction to the end of that same contraction - intensity: strength of the contraction at its peak mild, moderate, or strong - resting tone: tone of the uterine muscle in between contractions |
|
|
what happens during a prolonged contraction duration
|
- greater than 90 seconds or too frequency more than 5 in 10 mi period---> reduces blood flow to the placenta
--> fetal hypoxia and decreased FHR |
|
|
what can you measure uterine contractions with?
|
a sterile, water filled intrauterine pressure catheter inside the uterus
- displays uterine contraction patterns on monitor - requires membrane to be ruptured and cervix to be dilated |
|
|
vaginal examination
|
performed digitally by the provider or qualified nurse to asses for:
-cervical dilation -descent of the fetus through the birth canal, fetal station in CM - fetal position, presenting part, and lie -membranes that are intact or ruptured |
|
|
what are the signs of a true labor
|
contractions:
- may begin irregular, but come regular in frequency - stronger, lasts long, and frequent - felt in the lower back-->radiates to abdomen - walking causes the intensity to increase Cervix -change in dilation, and effacement - moves anterior position - bloody show fetus--> presenting part engaged in pelvis |
|
|
false signs of a labor
|
contractions:
-painless, irregular frequency, and intermittent - decrease in frequency, duration, and intensity with walking or position changes - felt in lower back or abdomen above umbilicus - stops with sleep, oral hydration, or emptying of bladder cervix: - no changes in dilation or effacement - often remains in post positon - no bloody show fetus: not engaged in in pelvis |
|
|
what is engagement?
|
occurs when the presenting part is biparietal largest diameter of the fetal head passes the pelvic inlet at the level of the ischial spines reffered to station *0*
|
|
|
what is descent?
|
the progress of the presenting part preferably the occiput through the pelvis, measured by station during a vaginal examination---> neg--> superior to station 0
pos--> measured if inferior to station 0 |
|
|
what is flexion?
|
what the fetal head meets the resistance of the cerviz pelvic wall or pelvic floor, the head flexes, bring the chin close the client and chest, presenting a small diameter in cm if inferior to station 0
|
|
|
what is extension?
|
the fetal occiput passes under the sympysis pubbis and then the head is deflected(change position) anteriorly and born by extension of the chin away from the fetal chest
|
|
|
what is internal position
|
the fetal occiput ideally rotates to a lateral anterior position as it progress from the ischial spines to the lower pelvis in a crocks crew motion to pass through the pelvis
|
|
|
what is recitation and external rotation
|
after the head is born it rotates to the position it occupied as it entered the pelvic inlet with the fetal body and complete quarter turn to face transverse as the anterior shoulder passes under the symphysis
|
|
|
what is expulsion?
|
after birth of the head and shoulders and the trunk of the neonate is born by flexing toward the symphysis pubis
|
|
|
FIRST STAGE OF LABOR
|
duration: 12.5 hour
- ends with complete dilation--> 1cm/hr for primigravida, 1.5 cm for multigravida |
|
|
latent phase
|
primigravida 6 HR
- multigravida 4 hr - beings with cervix 0 --->ends 3cm - frequency 5- 30 min - duration 30-45 seconds -some dilation - patient is eager and talkative |
|
|
active phase
|
-primigravida 3 hr
- multigravida 2 hr -cervix 4 cm --> ends with 7 cm - more regular, moderate to strong contractions - regquency 3-5 min -duration 40-70 seconds - rapid dilation and effacement - fetal descent -feeings of helplessness, and anxiety |
|
|
transition phase
|
20 min to 40 min longs
- starts with 8 cm--> ends with 10 cm - strong contractions - frequency every 2-3 min -duration 45-90 seconds - tired, restlessness and irritable, feeling out of control, N&V, urge to push, rectal pressure, *needing to have a bowel movement*, increased bloody show, hardest part of labor |
|
|
second stage
|
primigravida
30 min to 2 hr - multigravida 5 to 30 min - full dilation, - contractions every 1-2 min - BIRTH PUSHING FETUS OUT |
|
|
third stage
|
5 to 30 min
- delivery of the neonate -delivery of the placenta - placenta separation and expulsion *shultz presentation---> shiny fetal emerges first *Duncan presentation---> dull maternal surface of placenta emerges first |
|
|
fourth stage
|
1-4 hr
- delivery placenta - maternal stabilization of vital signs - bring back to homeostatis - lochia scant to moderate rubra |
|
|
what do you need asses during the fourth stage of labor?
|
maternal vital signs
-fundus -lochia--> color-->amount-->clots -perinuem -urinary ouput ----> bladder distention -maternal/newborn baby friendly activities vital signs--> 15 min - apply ice packs to perineum - monitor newborn status--> resp rate, skin color, adequacy or peripheral circulation, type of resp, level of con, tone activity every 30 min |
|
|
nursing interventions during the fourth stage
|
assses matneral vital signs every 15 min for first hour
- asses for fundus and lochia every 15 min for the first hour - massage the uterine fundus or administer oxytocics to maintain uterine tone to prevent hemorrhage - asses clients perineum, to provide comfort measures - encourage voiding to prevent bladder distention -promote an opportunity for maternal/newborn bonding - if the client has vaginal bleeding or passage of clots---> let physician know - check uterus every 15 minutes for first hour, 30 min the second hour every 4 hours for the next 22 hours - every first 24 hours thereafter |
|
|
FIRST STAGE PAINNNNN
|
internal or visceral pain felt by back or leg pain--> dilation, effacement, and stretching of the cervix
- distention of the lower segment of the uterus |
|
|
SECOND STAGE PAINNN
|
pain is somatic and occurs with fetal descent and expulsion ---->>>
- pressure and distention of vagina and perineum burning, spitting, and tearing - pressure and pulling ton the pelvic structures (ligaments, fallopian tubes, ovaries, bladder, and peritoneum) - laceration of cervix, vagina, and perineum |
|
|
THIRD STAGE PAINNN
|
pain with the expulsion of the placenta is similar to the pain experienced during the first stage
- uterine contraction -pressure and pulling of pelvic structures |
|
|
FOURTH STAGE PAIN
|
pain is caused----> distention of stretching of vagina and perineum just like the second stage with splitting, burning, and tearing sensation
|
|
|
anxiety and pain can be from?
|
fear, fatigue, full bladder, interlace, previous experience with pain, fetal malposition, cephalopelvic disproportion, childbirth preparation, level of support during labor
|
|
|
usual pain manifestations
|
crying, moaning, screaming, gesturing, writhing, avoidance, withdrawal,inability to follow instructions
- increased blood pressure, tachycardia, and hyperventilation |
|
|
non pharmacological pain interventions
|
lamaze or patterned breathing
- aromatherpay -breathing tecniques -imagery -music -focal points -subdued lighting - back rub and massage - effluerage: light, gentle circular stroking of the abdomen with breathing -sacral counter pressure -heat/cold therapy, hydropterhapy, acupressure |
|
|
what maternal changes promote relaxation and pain relief?
|
-semi sitting
-squatting -kneeling -kneeling and rocking back and forth -supine position with the placement of a wedge under one of the clients hips to tilt the uterus and avoid supine hypotension syndrome |
|
|
before giving any analgesia and local regional analgesia what must you check for?
|
- the labor is well established by performing a vaginal exam
- evaluating uterine contraction pattern and doing a vaginal examination |
|
|
sedatives (barbiturates)
|
secobarital (seconal), pentobarital (nembutal), and phenoarbital (luminal)
- not usually used for birth but can early latent phase - used to relieve anxiety and induce sleep - adverse effects: neonate respiratory depression, unsteady ambulation, - not given for pain - drowsiness, - provide dim light, quiet atmosphere |
|
|
opioid analgesics
|
meperidine hydrochloride (Demerol), fentanyl (Sublimaze), butorphanol (Stadol), and nalbuphine (Nubain)
- nubain and stadol---> less resp distress - adverse effects: - neonate resp depression - reduces gastric emptying--> N&V - sedation - tachycardia - Hypotension -decreased FHR variability - drowsiness - ambulation |
|
|
nursing actions for opioid analgesics
|
MUST BE AT LEAST 4 CM DILATED
- ADMINISTER ANTIMETICS - monitor vital signs, uterine contractions, FHR - have narcan ready just in case - reglan and zofran, antianxiety and antimietic --->dry mouth---> ice chips |
|
|
epidural and spinal regional analgesia
|
fentanyl (sublimaze) and sufentanil (sufenta) they are short acting opioids that are administered as a motor block into epidural or intrathecal space without anesthesia, able to still feel contractions and bear down
adverse effects: decreased gastric emptying in nausea and vomitng - inhibition of bowel and bladder elimination - bradycardia or tachycardia, hypotension - resp depression - allergic reaction and pruiritus, elevated temp |
|
|
regional block
|
pudendal block, epidural block, spinal block, paracervical nerve block
- goes transevaginally into the pudendal nerve to the perineum, vulva, and rectal areas---> episiotomy - second stage of labor 10-20 min before labor - adverse effects: ligament hematoma--> check, maternal bearing down reflex ---> tell client to bear down |
|
|
epidural block
|
local anesthetic, burpivacine marcaine that is injected into epidural space at the level of the fourth or fifth vertebrae--> eliminates sensation from level of the umbilicus to the thighs, relieving uterine contractions, fetal descent, and pressure from the stretching perineum
- MUST BE AT LEAST 4 CM DILATED - adverse effects: maternal hypotension -fetal bradycardia - inabilility to feel the urge to void - loss of bearing down reflex |
|
|
nursing actions of a epidural block
|
administer IV bolus fluids to help offest maternal hypotension
- position---> to sitting or side lying modified sims --> hypotensive crisis - pushing efforts--> coach - asses FHR, oxygen suction - asses for orthostatic hypotension - check for bladder distention--> if it is catheterize - vital signs every 5-15 min - N& V signs and symptoms - urinary retention |
|
|
spinal block
|
local anesthetic that is injected into the subarachnoid space into the spinal fluid at the third fourth fifth lumbar interspace
- sensations elminated--> level of nipple to the feet - FOR CESAREAN BIRTHS - give second stage or before C section - adverse effects: - maternal hypotension - loss of bearing down reflex in the mother - headache - maternal bladder and uterine atony |
|
|
spinal block nursing actions
|
- asses vital signs every 10 min
- give Iv fluid administration, and initiate oxygen - client uterine contractions asses level of anesthesia - asses FHR, safety - recognize signs of impending birth--> sitting on one buttock, making grunting sounds, bulging of the perineum |
|
|
interventions for postpartum headache from a cerebrospinal fluid leak
|
- place the client in supine position
- promote bed rest in dark room - administer oral analgesics, caffiene, and fluids - autologous blood patch is beneficial and reliable relief measure |
|
|
general anesthesia
|
RARELY USED FOR VAGINAL AND CESAREAN BIRTHS
- monitor vital signs, FHR -client has nothing by mouth - IV infusion is in place -anitemboli stockings - maintain an open airway and cardiopulmonary function - hemmorhage |
|
|
leopold manuevers
|
to determine: number of fetuses
- presenting part, fetal lie, fetal attitude - degree of descent of the presenting part into the pelvis - PMI fetal heart tones are ausculated the loudest on woman's abdomen, best heard over the fetal back |
|
|
vertex presentation PMI
|
right or lower quadrant or below the maternal umbilicus
|
|
|
breech presentation
|
PMI: either right or left upper quadrant above the maternal umbilicus
|
|
|
nursing actions of leopold maneuvers
|
- ask client to empty the bladder
- place the client in supine position with a pillow under the head have knees flexed slightly - place wedge under right hip--> prevent supine hypotension syndrome |
|
|
how to do the actual leopold maneuvers
|
identify the fetal part
HEAD: round, firm, move freely BREECH: irregular and soft--> fetal lie and presenting part FETAL BACK: use palm of hand--> irregular--> hands, feet, and elbows --> presenting part TRUE PELVIS: thumb and fingers, determine if flexed or extended the head Outline of the head: use fingertips of both hands to palpate the head --> if cephalic is on the same side as the small parts head is felexed with vertex presentation --> if chepalic is same side as the back, head is extended with a face presentation--> fetal attitude |
|
|
when to ausculatate or continuous fetal monitoring
|
low risk
latent-->60 min active--> 30 min second stage--> 15 min high risk latent-->30 min active--> 15 min second stage--> 5 min |
|
|
reason as to why you would want to ausculatate the FHR
|
ROM, either SROM or AROM
- vaginal exam--> after - expulsion or enema - urinary cath - extensive uterine contractions |
|
|
normal FHR
|
110-160
PMI--> palpate the fundus you want to count the FHR for 30-60 seconds to determine the baseline rate - ausculatate the FHR during a contraction and for 30 seconds following completion of contraction |
|
|
tocotransducer
|
fetal monitoring that records ultrasound over the client abdomen to determine PMI
- advantage: noninvasive, membranes don't have to be ruptured, doesn't have to be dilated, FHR&contraction - disadvantage: contraction intensity not measurable, movement, reposition transducers, obesity--> not good recording |
|
|
why do we need electronic fetal heart monitoring
|
multiple gestations, oxytocin pitocin
- placenta previa - fetal bradycardia - diabetes, HTN, kidney disease - IGR - postdate, active labor - meconium stained amniotic fluid - abruption placenta - abnormal nonstress test or contraction stress test - abnormal uterine contractions - fetal distress |
|
|
whats considered normal fetal HEART RATE and monitoring
|
EXCLUDE: accelatrions, deccelartions, periods of marked variability within a 10 min window
- it should be 2 min of baseline segments in a 10 min window should be present |
|
|
what does fetal variability mean?
|
IRREGULAR*
-fluctuations in the heart frequency and amplitude - absent or undetectable variability (NONREASSURING) - minimal variability ( less than 5 min) - moderate viarability (6 to 25 min) -marked variability (greater than 25 min) |
|
|
category I
|
baseline fetal heart of 110-160 min
- baseline fetal heart rate variability: moderate - accerlatrions: present or absent - early decelerations: present or absent - variable or late decelerations: absent * continue auscultation and palpation continue EFM, continue supportive interventions |
|
|
category II
|
fetal heart rate tracings not categorized as I or II such as:
- tachycardia - bradycardia--> absent baseline variability baseline FHR variability - minimal baseline variabilility - absent baseline viability not accompanied by recurrent deceleration - marked baseline variability - episodic decelartions, prolonged fetal rate deceleration get than 2 but less than 10 - decel--> w/ moderate or minimal variability - absence of induced acceleration after fetal stimulation * increase frequency of auscultation, continue or initiate EFM, intrauterine resuscitation measures |
|
|
category III
|
sinusoidal pattern
- recurrent variable decelerations - recurrent late decorations - bradycardia |
|
|
nonreassuring FHR patterns
|
* associated with fetal hypoxia and:
fetal bradycardia fetal tachycardia absence of FHR variability late decelerations variable decelerations |
|
|
interventions for accelerations increase in FHR above baseline
|
reassuring, not interventions required
- can be from: health fetal/placental exchange - CNS - vaginal exam - fundal pressure - 15 beats above the baseline and last from 15 seconds to less than 2 mites |
|
|
fetal bradycardia FHR less than 110 for 10 min or more REASON
|
Uteroplacental insufficiency
› Umbilical cord prolapse › Maternal hypotension › Prolonged *umbilical cord compression* › Fetal congenital heart block › Anesthetic medications - fetal hypoxia--> if remains above 90 tolerated but below not tolerated - hypothermia of fetus - hypokalemia of fetus - chronic head compression |
|
|
what are the interventions for fetal bradycardia
|
› Discontinue oxytocin (Pitocin) if being administered. › Assist the client to a side-lying position.
› Administer oxygen by mask at 8 to 10 L/min. › Insert an IV catheter if one is not in place. › Administer a tocolytic medication as prescribed. › Notify the provider. *sudden obstretical emergency |
|
|
fetal tachycardia FHR greater than 160 min for 10 min or more
|
Maternal infection, chorioamnionitis › Fetal anemia
› Fetal heart failure › Fetal cardiac dysrhythmias › Maternal use of cocaine or methamphetamines › Maternal dehydration - early fetal hypoxemia--> meds--> terbutaline - illicit drugs * interventions give antibiotics, fluids for dehydration *antiprytitcs--> temp regulation if fever *notify DR and take vital signs |
|
|
what interventions are you gonna do for fetal bradycardia
|
Administer prescribed antipyretics for maternal fever, if present.
› Administer oxygen by mask at 8 to 10 L/min. › Administer IV fluid bolus. |
|
|
decrease or los of FHR variability REASON
|
› Medications that depress the CNS, such as narcotics, barbiturates, tranquilizers, or general anesthetics
› Fetal hypoxemia with resulting acidosis › Fetal sleep cycle › Congenital abnormalities - supine hypotension - cord compression - uterine tachystotle - drugs ( prescription, illicit, alcohol) |
|
|
decrease or loss of FHR variability interventions
|
Stimulate the fetal scalp.
› Assist provider with application of scalp electrode. › Place client in left-lateral position. - consider AROM - change postion - give IV bolus - discontinue oxytocin - deliver o2 at 10 L/min - conisder invavsive monitoring such as internal FSE |
|
early deceleration of FHR REASON
|
nadir--> lowest point of deceleration
Compression of the fetal head resulting from uterine contraction › Vaginal exam › Fundal pressure * no interventions required |
|
|
late decelerations of FHR REASON
|
› Uteroplacental insufficiency causing inadequate fetal oxygenation
› Maternal hypotension, abruptio placentae, uterine hyperstimulation with oxytocin (Pitocin) |
|
|
decelartions FHR interventions
|
› Place client in side-lying position.
› Insert an IV catheter if not in place, and increase rate of IV fluid administration. › Discontinue oxytocin (Pitocin) if being infused. › Administer oxygen by mask at 8 to 10 L/min. › Notify the provider. › Prepare for an assisted vaginal birth or cesarean birth. |
|
|
variable decelerations of FHR
|
› Umbilical cord compression
› Short cord › Prolapsed cord › Nuchal cord (around fetal neck) › Oligohydramnios |
|
|
varibale deceleration of FHR interventions
|
› Short cord
› Prolapsed cord › Nuchal cord (around fetal neck) › Oligohydramnios › Reposition client from side to side or into knee-chest. › Discontinue oxytocin (Pitocin) if being infused. › Administer oxygen by mask at 8 to 10 L/min. › Perform or assist with a vaginal examination. › Assist with an amnioinfusion if prescribed. |
|
|
main nursing actions of FHR monitoring
|
do leopold manuevers, auscultate a PMU using listening device
- provide education regarding the procedure and the clients partner during placement and adjustments of the fetal monitor equipment - identify proper placement of tocotransducer - if not contraindicated and patients wants to use the bathroom thane them but take of FHR monitoring or if contraindicated use bedpan |
|
|
continuous internal fetal monitoring
|
scalp electrode by attaching a small spiral electrode to the presenting part of the fetus to monitor the FHR
- IUPC : avg pressure is 50-85mm hg - early detection of FHR --> distress - allows greater maternal freedom of movement because tracing is not affected by fetal activity maternal position changes or obesity, check maternal temp every 1 to 2 hours - |
|
|
disadvantages of FHR monitoring
|
disadvantages: membranes must have ruptured to use internal monitoring
- cervix must be dilated at least 2 cm to 3 cm - presenting part must be descended to place electrode - contraindicated with vaginal bleeding - left position, if supine put pillow on right hip or wedge to tilt uterus |
|
|
culturuallyyyy competent compatibility of hispanic, african american, asian american, native american, european american
|
Hispanic – Prefer mother to be present rather than partner
African American – Prefer female family members for support Asian American –May prefer mother to be present; partner not an active participant; labor in silence; caesarean birth undesirable Native American – Prefer female nursing personnel; family involved in birth; use of herbs during labor; squatting position for birth European American – Birth is public concern; focus on technology; partner expected to be involved; provider seen as head of health care team |
|
|
what does the admission history and care of plan include for the initial care
|
☐ Obtain laboratory reports.
☐ Monitor baseline fetal heart tones and uterine contraction patterns for 20 to 30 min. ☐ Obtain maternal vital signs. ☐ Check the status of the amniotic membranes. - do fetal assesment - do vaginal examination-->not if vaginal bleeding or until placenta pre via is ruled out - labor progess and fetal lie, presentation, attitude, and fetal side in relationship to the mothers pelivis - contractions |
|
|
first stage of labor assessment
|
leopold manuevers
- vaginal examination: for ROM and labor - encourage the client to slow breaths during vag exam - monitor cervical dilation, and effacement - monitor station and fetal presentation - prepare for impending delivery |
|
|
assessment of ROM
|
- suspected---> FHR to ensure there is no distress from possible umbilical cord prolapse, which can occur with gush of amniotic fluid
- verify that is amniotic fluid--> paper turns blue ph 6.5 to 7.5 - ases for color and odor--> should be clear straw color and free of odor meconium--> abnormal color yellow or port wine a foul odor |
|
|
bladder palpation for what reason
|
bladder distention
- clients may feel the urge to void secondary to labor process or anesthesia - encourage them to void frequently |
|
|
blood pressure assessment ulse and respiration measurements
|
latent phase every 30 min
active phase: every 30 min transition phas: every 15 to 30 min |
|
|
how often do we do temperature assessment
|
everyy 4 hours, if ROM--> 1 or 2 hours
latent phase: 30-60 min active phase: every 15-30 min transition phase every 10-15 min |
|
|
how often to oyou have to monitor FHR
|
latent phase: 30-60 min
active phase: 15- 30 min transitional phase: 15-30 min |
|
|
nursing interventions during the first stage of labor
|
breathing, effluerage ( stroking fingers in circular rhythm with breathing )
- upright position, application --> hot, cold, - encourage voiding every 2 hours - FHR monitoring - freqeunt position changes - encourage voiding at least every 2 hors - encourage deep cleansing breaths before and after - relaxation - nonpharmological |
|
|
interventions for first stage of transition phase
|
- encourage void every 2 hours
- monitor and support the client and fetus - encourage a rapid pant blow breathing pattern - discourage pushing efforts until cervix is dilated - listen for "BOWEL MOVEMENT"--> sign of fetal descent - look for perineal bulging or crowning - encourage to the client to begin bearing down with contraction once cervix is fully dilated |
|
|
second stage assessments
|
blood pressure, pulse, resp, every 5to 30 min
- uterine contractions - pushing efforts - increase in bloody show - FHR every 15 min and immediately following birth |
|
|
assesment for perineal lacerations usually fetal head is expulsed
|
First degree – Laceration extends through the skin of the perineum and does not involve the muscles.
■ Second degree – Laceration extends through the skin and muscles into the perineum. ■ Third degree – Laceration extends through the skin, muscles, perineum, and anal sphincter muscle. ■ Fourth degree – Laceration extends through skin, muscles, anal sphincter, and the anterior rectal wall. |
|
|
what are the nursing interventions for second stage of birth
|
monitor the client fetus
- assist in positioning the client for effective pushing - assisnt in partner involvement with pushing efforts and encourage bearing down efforts during contractions/promote rest - provide comfort measures - cleanse the perineum - prepare for episiotomy - prepare care of neonate -chekc oxygen flow and tank on warmer - preheat the radiant warmer - lay out newborn stethoscope and bulb syringe - have resuscitation in working order check suction apparatus |
|
|
third stage assessment
|
vital signs every 15 min
-signs of placental separation: fundus is firm and contracting - swift gush of dark blood from introits - umbilical cord appears to lengthen as placenta descends - vaginal fullness on exam - lochia - urinary output - asses maternal vital signs 15 min for first our asses fundus and lochia every 15 min for first hour *MASSAGE FUNDUS AND ADMINISTER OXYTOCIS |
|
|
interventions for bleeding after birth
|
bleeding---> uterine atony, most common cause of hemorrhage---> massage the fundus---> it is not firm give pitocin vitamin b---> you cannot use to treat magnesium sulfate, to treat preclmapsia, seizures, preterm labor so what do yo use?---> metogin contraindications high BP---> hemobate contraindications asthma---? massage uterus , give pitocin, hypotensive, pt has asthma no hemobate, oxytocin
|
|
|
external cephalic version
|
ECV
try to manipulate a malpositioned fetus into a normal vertex presentation after 37 weeks of gestation contraindications: uterine anomalies, cesarean births, cephalopelvic disproportion, placenta previa, multifetal gestation, olgihydramnios |
|
|
what are the nursing actions for ECV
|
breeech fetus
- obtain informed consent - ultrasounds: location position, locate umbilical cord, asses placenta previa, determine amount of amniotic fluid, or anomalies - perform non stress test - ROGHAM - IV fluids & tocolyicts - bradycardia and variable decoration--> look out - hypotension - kleihaur betke test--> more than 15 ml--> admister rhogam |
|
|
what will you asses for during ECV
|
■ Monitor uterine activity, contraction frequency, duration, and intensity.
■ Monitor for rupture of membranes. ■ Monitor for bleeding until maternal condition is stable. ■ Monitor for a decrease in fetal activity. |
|
|
bishop score
|
◯ A Bishop score is used to determine maternal readiness for labor
- Cervical dilation ■ Cervical effacement ■ Cervical consistency (firm, medium, or soft) ■ Cervical position (posterior, midposition, or anterior) ■ Station of presenting part 39 weeks--> should be greater than 8 --> mulipara 10--> nulipara |
|
|
cervical ripening
|
- oxytocin (pitocin)--> induce labor
- low dose used for cervical priming - balloon catheter inserted into intracervical canal to dilate the cervix - membrane stripping and an amniotomy - hygroscopic dilators and sponges may be inserted to absorb fluid from surrounding tissues and then enlarge - laminaria tents--> seaweed - syntetic dilators contain mangesium sulfate lamicel - prostaglandin |
|
|
cervical ripening interventions
|
look for:
Urinary retention ■ Rupture of membranes ■ Uterine tenderness or pain ■ Contractions ■ Vaginal bleeding ■ Fetal distress Failure of the cervix to dilate and efface ◯ Failure of labor to progress - side lying position - hypertension, diarrhea, and vomiting. ■ The nurse should proceed with caution in clients who have glaucoma, asthma, and cardiovascular or renal disorders. |
|
|
what should you do if you doing the cervical ripening and there is fetal distress?
|
☐ Apply O2 via face mask at 10 L/min.
☐ Position the client on her left side. ☐ Increase rate of IV fluid administration. ☐ Notify the provider. |
|
|
induction of labor
|
administration of IV oxytocin (pitocin)
- nipple stimulation - elective induction 39 weeks--> bishop score 8--> mulipara greater than 10---> nulipara |
|
|
why do induction of labor ?
|
posterm pregnancy
- dystocia proloned labor due to inadeqaute uterine conractions - prolonged rupture of membranes predisposes the client and fetus to risk of infection |
|
|
complications of induction of labor
|
Rh-isoimmunization
■ Diabetes mellitus ■ Pulmonary disease ■ Gestational hypertension ◯ Fetal demise ◯ Chorioamnionitis |
|
|
nursing actions oxytocin to induce labor
|
informed consent
- cervical ripening agents - oxytocin--> after 6-12 hour administration of prostaglandin - monitor FHR and uterine activity after administration of cervical ripening agents - HP--> fetal distress - before oxytocin--> nurse confirms--> fetus is engaged in birth canal and at minimum of station 0 - oxytocin piggyback to the main line and administered via infusion pump - IUPC--> contraction - check vital signs--> oxytocin - monitor FHR - asses fluid intake and urinary output |
|
|
when to increase oxytocin
|
☐ Increase oxytocin as prescribed until desired contraction pattern is obtained and then maintain the dose if there is a:
Contraction frequency of 2 to 3 min. Contraction duration of 60 to 90 seconds. Contraction intensity of 40 to 90 mm Hg on IUPC. Uterine resting tone of 10 to 15 mm Hg. Cervical dilation of 1 cm/hr. Reassuring FHR between 110 to 160/min. |
|
|
when to discontinue oxytocin if uterine hyper stimulation occurs
|
Contraction frequency more often than every 2 min.
☐ Contraction duration longer than 90 seconds. ☐ Contraction intensity that results in pressures greater than 90 mm Hg as shown by IUPC. ☐ Uterine resting tone greater than 20 mm Hg between contractions. ☐ No relaxation of uterus between contraction |
|
|
complications of inducing labor
|
An abnormal baseline less than 110 or greater than 160/min
☐ Loss of variability ☐ Late or prolonged decelerations |
|
|
what do you do if your inducing labor and complications happen with are you interventions?
|
Notify the provider.
■ Position the client in a side-lying position to increase uteroplacental perfusion. ■ Keep the IV line open and increase the rate of IV fluid administration to 200 mL/hr unless contraindicated. ■ Administer O2 by a face mask at 8 to 10 L/min as prescribed. ■ Administer the tocolytic terbutaline (Brethine) 0.25 mg subcutaneously as prescribed to diminish uterine activity. ■ Monitor FHR and patterns in conjunction with uterine activity. ■ Document responses to interventions. ■ If unable to restore reassuring FHR, prepare for an emergency cesarean birth. |
|
|
augmentation of labor
|
◯ Augmentation of labor is the stimulation of hypotonic contractions once labor has spontaneously
begun, but progress is inadequate. -ertain providers favor active management of labor to establish effective labor with the aggressive use of oxytocin (Pitocin) or rupture of membranes. This ensures that the client delivers within 12 hr of admission to the labor unit so that the risk of cesarean birth will be decreased. |
|
|
amniotomy
|
An amniotomy is the artificial rupture of the amniotic membranes (AROM) by the provider using
an Amnihook or other sharp instrument. ◯ Labor typically begins within 12 hr after the membranes rupture. ◯ The client is at an increased risk for cord prolapse or infection. * ASSES FROM COLOR, ODOR, AND CONSISTENCY |
|
|
amnioinfusion
|
amnoinfusion --> 0.9% sodium chloride or lactated ringers solution--> instilled into amniotic cavity through a transcervical catheter--> reduces variable decelerations--> cord compression
|
|
|
AMNIOINFUSION potential diagnoses
|
■ Oligohydramnios (scant amount or absence of amniotic fluid) caused by any of the following:
☐ Uteroplacental insufficiency ☐ Premature rupture of membranes ☐ Postmaturity of the fetus FETAL CORD COMPRESSION ☐ Postmaturity of fetus (macrosomic, large body), which places the fetus at risk for variable deceleration from cord compression |
|
|
AMNIOINFUSION interventions
|
assist with amniotomy if membranes are not already ruptured---> membranes have to ruptured--> perform amnioinfussion
- warm fluid using a blood warmer prior to infusion - perform nursing measures to maintain comfort and dryness because the infused fluid will leak -monitor client to prevent over distention and increase uterine tone, which will intensify uterine contractions and cause non reassuring FHR - MONITor fluid output from vagina to prevent uterine over distention |
|
|
vacuum- assisted delivery what is it
|
cup like suction attached to the fetal head, traction applied during contractions to assist in the descent and birth of the head, after the vacuum cup is released and removed preceding delivery of the fetal body
|
|
|
what conditions will happen with vacuum assisted birth and risk
|
■ Vertex presentation
■ Absence of cephalopelvic disproportion ■ Ruptured membranes RISK Scalp lacerations ■ Subdural hematoma of the neonate ■ Cephalohematoma ■ Maternal lacerations to the cervix, vagina, or perineum ● Indications ◯ Maternal exhaustion and ineffective pushing efforts ◯ Fetal distress during second stage of labor |
|
|
for vaccumm assisted delivery what are the nursing actions that you do?
|
lithotomy position
- asses and record FHR - asses for bladder distention - prepare for forceps assisted birth if vacuum assisted is not successful observe for lacterations, cephalohematoms, subdural hemotaoms after delivery - check the neonate for kaput sucessdaneum |
|
|
for cep assisted birth
|
forceps assisted birth consists using an instrument with two curved spoon like blades to assist in the delivery of the fetal head
FOR: ◯ Client presentation ■ Fetal distress during labor ■ Abnormal presentation or a breech position requiring delivery of the head ■ Arrest of rotation |
|
|
what can you do as a nurse for forcep assisted delivery
|
lithotomy position
- bladder is empty, catherize if necessary - make sure fetus is engaged and membranes have ruptured -asses and record FHR before during and after forceps - compression of a cord between the head will cause a decrease in FHR check for injuries - urine retention hematoma |
|
|
what are the complications of a for cep assisted delivery
|
◯ Lacerations of the cervix
◯ Lacerations of the vagina and perineum ◯ Injury to the bladder ◯ Facial nerve palsy of the neonate ◯ Facial bruising on the neonate |
|
|
epsiotomy
|
An episiotomy is an incision made into the perineum to enlarge the vaginal opening to facilitate
delivery and minimize soft tissue damage. |
|
|
why do a episiotomy
|
Shorten the second stage of labor
◯ Facilitate forceps-assisted or vacuum-assisted delivery ◯ Prevent cerebral hemorrhage in a fragile preterm fetus ◯ Facilitate birth of a macrosomic (large) infant |
|
|
median episiotomy
|
extends from the vaginal outlet toward the rectum, and is the most
commonly used. ■ Easier to repair ■ Less blood loss ■ Associated with a higher incidence of third- and fourth-degree lacerations |
|
|
mediolateral episiotomy
|
A mediolateral episiotomy extends from the vaginal outlet posterolateral, either to the left or right
of the midline, and is used when posterior extension is likely. ■ Third-degree laceration may occur. ■ Blood loss is greater, and the repair is more difficult. ■ Local anesthetic is administered to the perineum prior to the incision. |
|
|
what can you do as nurse for episitomy
|
■ Encourage alternate labor positions to reduce pressure on the perineum and promote perineal stretching to reduce the necessity for an episiotomy.
|
|
|
cesarean birth
|
◯ A cesarean birth is the delivery of the fetus through a transabdominal incision of the uterus to
preserve the life or health of the client and fetus when there is evidence of complications. |
|
|
why do a c section
|
■ Malpresentation, particularly breech presentation
■ Cephalopelvic disproportion ■ Fetal distress ■ Placental abnormalities ☐ Placenta previa ☐ Abruptio placenta High-risk pregnancy ☐ Positive HIV status ☐ Hypertensive disorders such as preeclampsia and eclampsia ☐ Diabetes mellitus ☐ Active genital herpes lesions ■ Previous cesarean birth ■ Dystocia ■ Multiple gestations ■ Umbilical cord prolapse |
|
|
for cesearan birth what is the prepocedure
|
asses FHR
- ultrasounds - supine position wedge under hip--> vena cava - insert indwelling urinary catheter - antiemboli stockings and sequential compression device - IV cath, IV fluids - informed consent - RH FACTOR TEST |
|
|
transprocedure for c section
|
■ Assist in positioning the client on the operating table.
■ Continue to monitor FHR. ■ Continue to monitor vital signs, IV fluids, and urinary output. |
|
|
postprocedure c section nursing actions
|
monitor for bleeding --> incision site
- asses uterine fundus for firmness and tenderness - asses lochia for amount 0 a tender uterus and foul smelling locia--> endometritis - asses for pneumonia -thrombophlebitis, which include tenderness, pain, and heat on palpation - I and O - vital signs - antimietics 0 - Encourage the client to turn, cough, and deep breathe to prevent pulmonary complications. ■ Encourage splinting of the incision with pillows. ■ Encourage ambulation to prevent thrombus formation. ■ Assess the client for burning and pain on urination, which could be suggestive of a urinary tract infection. |
|
|
what are some complications for c section
|
■ Aspiration
■ Amniotic fluid pulmonary embolism ■ Wound infection ■ Wound dehiscence ■ Severe abdominal pain ■ Thrombophlebitis ■ Hemorrhage ■ Urinary tract infection ■ Injuries to the bladder or bowel ■ Anesthesia associated complications |
|
|
VAGINAL DELIVERY AFTER CESAREAN BIRTH
|
● A vaginal birth after cesarean birth is when the client delivers vaginally after having had a previous cesarean birth.
|
|
|
indications for VAGINAL DELIVERY AFTER CESAREAN BIRTH
|
Client presentation
■ Previous documented low-segment transverse incision ■ No current contraindications ☐ Large for gestational age newborn ☐ Malpresentation ☐ Cephalopelvic disproportion ☐ Previous classical vertical uterine incision |
|
|
what can you do as a nurse for VAGINAL DELIVERY AFTER CESAREAN BIRTH intra, post, pre
|
Preprocedure
■ Nursing actions ☐ Review medical records for evidence of a previous low-segment transverse cesarean incision. ■ Client education ☐ Explain the procedure to the client and her partner. Nursing actions ☐ Assess and record FHR during the labor. ☐ Assess and record contraction patterns for strength, duration, and frequency of contractions. ☐ Assess for evidence of uterine rupture. ☐ Promote relaxation and breathing techniques during labor. ☐ Provide analgesia as prescribed and requested. Postprocedure ■ Nursing actions ☐ Nursing interventions for a vaginal delivery after a cesarean birth are the same as for a vaginal delivery. |
|
|
what are the main goals of postpartum period?
|
*prevent postpartum hemorrhage
- assisting in recovery, identifying deviations, providing comfort measures, and pharmacological pain relief, provide education about newborn and self care, provide infant activities |
|
|
what are the physiological maternal changes during postpartum?
|
uterine involution
- lochia flow - cervical involuation - decrease in vaginal distention - alteration in overran function and menstruation - cardiovascular - uniary tract, breast GI |
|
|
greatest risk in postpartum
|
hemorrhage, shock, and infection
(shock: not enough blood in body-->hemorrhage) for hemorrhage--> give pitocin |
|
|
postpartum hormones estrogen, progesterone, placental enzyme insulinase
|
estrogen decreased--> breast engorgement, diaphoresis, diuresis, excess extracellular fluid accumulated, vaginal lubrication, local dryness,
progesterone decreased--> increase in muscle tone throughout body decreased placental enzyme insulin's--> reversal of diabtogenic effects of pregnancy |
|
|
lacatating and nonlacting whats the difference between these women
|
- lactating women---> prolacted still elevated--? suppress ovulation--> 6 months
-nonlactating women--> menses return 4-6 weeks, ovulation 27-75 days after birth |
|
|
rh nefaive mothers
|
give RH D immune globulin or rhogam within 72 hours to women and gave birth to infants who are rh positive to prevent sensitization in future pregnancies
|
|
|
wants the Kleihauer-Betke test
|
determines the amount of fetal blood in maternal circulation ---> if 15 ml or more of fetal blood--> mother receives increased dose of rhogam
|
|
|
postpartum assessment
|
☐ B – Breasts
☐ U – Uterus (fundal height, uterine placement, and consistency) ☐ B – Bowel and GI function ☐ B – Bladder function ☐ L – Lochia (color, odor, consistency, and amount [COCA]) ☐ E – Episiotomy (edema, ecchymosis, approximation) *☐ If the client is stable, vital signs will be monitored every 15 min x 4 for the first hour, every 30 min x 2 for the second hr, hourly x 2 for at least 2 hr, then every 4 to 8 hr depending on the prescriptions set forth by the provider. |
|
|
postpartum chills
|
Postpartum chill, which occurs in the first 2 hr puerperium, is an uncontrollable shaking chill immediately following birth. Postpartum chill is possibly related to a nervous system response, vasomotor changes, a shift in fluids, and/or the work of labor. This is a normal occurrence unless accompanied by an elevated temperature.
* give blankets and fluids |
|
|
assessing the fundal height and fundus after postpartum
|
At 12 hr postpartum, the fundus may be palpated at 1 cm above the umbilicus.
- should be firm -◯ Every 24 hr, the fundus should descend approximately 1 to 2 cm. It should be halfway between the symphysis pubis and the umbilicus by the sixth postpartum day. ◯ By day 10, the uterus should lie within the true pelvis and should not be palpable -Cup one hand just above the symphysis pubis to support the lower segment of the uterus, and with the other hand, palpate the client’s abdomen to locate the fundus -◯ Apply clean gloves, a lower perineal pad, and observe lochia flow as the fundus is palpated. ■ Determine whether the fundus is midline in the pelvis or displaced laterally (caused by a full bladder). - count fundal height with finger breadths |
|
|
intreventions for boggyy uterus other than massaging
|
helps with --> contractions--> prevents hemorrhage
oxytocin --> causes hypotension - encourage early breastfeeding to prevent hemorrhage too - encourage emptying of bladder every 2 to 3 hours to prevent possible uterine displacement and atony |
|
|
what are the three stages of lochia
|
Lochia rubra – bright red color, bloody consistency, fleshy odor, may contain small clots,
transient flow increases during breastfeeding and upon rising. Lasts 1 to 3 days after delivery. ■ Lochia serosa – pinkish brown color and serosanguineous consistency. Lasts from approximately day 4 to day 10 after delivery. ■ Lochia alba – yellowish, white creamy color, fleshy odor. Lasts from approximately day 11 up to and beyond 6 weeks postpartum. |
|
|
saturation of preineal pads
|
■ Scant (less than 2.5 cm, less than 1 inch)
■ Light (less than 10 cm less than 4 inches ) ■ Moderate (more than 10 cm less than 6 inches ) ■ Heavy (one pad saturated within 2 hr, or 1 hour(book)) ■ Excessive blood loss (one pad saturated in 15 min or less, or pooling of blood under buttocks) look for blood clots 10 g= 10 ml |
|
|
when assessing the breasts
|
colostrum during pregnancy--> 2-3 days immediately after birth (immunoglobllin G and A)
engorgement: lyphmatic circulation, milk production, and temporary vein congestion - redness and tenderness - cracked nipples--> mastitis * encourage early demand of breastfeeding--> hemorrhage - latching on: takes part of the areola not just the nipple |
|
|
what are the cardiovascular changes during postpartum period and assessment
|
blood loss-->200- 500 ml for vaginal
1000 ml--> cesarean birth - diphoresis and diuresis of excess fluid--> 2-3 days post delivery - hypovolemic shock--> does not usually occur because during pregnancy you have more blood volume--> elimination of placenta divert 500-750 ml of blood back into mothers circulation - WBC: 25000 - othrostatic hypotension--> 48 hours - elevation of pulse, stroke, volume and cardiac output--> 1 hr postpartum temp 100 F--> dehydration after labor - check for venous thrombosis--> redness, swelling, and warmth, human's sign--> early ambulation |
|
|
what are the gastrointestinal changes during postpartum and assessment
|
- increased appetite
- conspitation with bowel evacuation delayed until 2-3 days after birth - hemorrhouds - spontanoeous bowel movement should not occur for 2-3 days after delivery - vaginal birth--> risk for hemorrhoids--> stool softener, enemas |
|
|
Urinary System and Bladder Function
|
A distended bladder as a result of urinary retention can cause uterine atony and displacement to one side, usually to the right. The ability of the uterus to contract is also lessened.
-(client should be voiding every 2 to 3 hr). Excessive urine diuresis (1,500 to 3,000 mL/day) is normal within the first 2 to 3 days after delivery. - dysuria, color, amount, smell |
|
|
what are the signs of a distended bladder postpartum
|
■ Fundal height above the umbilicus or baseline level
■ Fundus displaced from the midline over to the side ■ Bladder bulges above the symphysis pubis ■ Excessive lochia ■ Tenderness over the bladder area ■ Frequent voiding of less than 150 mL of urine is indicative of urinary retention with overflow |
|
|
Nursing interventions for the urinary system and bladder function
|
Encourage the client to empty her bladder frequently (every 2 to 3 hr) to prevent possible
displacement of the uterus and atony. ◯ Measure the client’s first few voidings after delivery to assess for bladder emptying. ◯ Encourage the client to increase her oral fluid intake to replace fluids lost at delivery and to prevent or correct dehydration. ◯ Catheterize if necessary for bladder distention if the client is unable to void to ensure complete emptying of the bladder and allow uterine involution. |
|
|
Musculoskeletal System changes and assessment
|
the joints return to their pregnant state and completey destabilized
- feet will remain permanently increased sized - rectus abdominis muscles of abdomen and puboccoygeal musce tone are restored---> 2-6 weeks - asses for diatasis recti---> separation of the recuts muscle--> 2-4 cm--> resolves 6 weeks |
|
|
nursing intrventions for postartum muscuoskeletal changes
|
Teach the client postpartum strengthening exercises, advising her to start with simple exercises, and then gradually progressing to more strenuous ones.
◯ Instruct clients who have had a cesarean birth to postpone abdominal exercises until about 4 weeks after delivery, or follow recommendations of her health care provider. ◯ Advise the client on good body mechanics and proper posture. |
|
|
changes of the immune system and assessment of it
|
rubeella: titer of less than 1:8 administered a sub Q injection of rubella vaccines Measles, mumps and rublaa vaccine during postpartum period to protect subsequent fetus malformations
- client should not get pregnant 1 month following immunization - HEP B: Newborns born to infected mothers should receive the hepatitis B vaccine and the hepatitis B immune globulin within 12 hr of birth. - rogham 72 hours neg mom to positive baby test 3 months after to see if they received immunity to rubella and rhogam - varicella: administered before discharge, should not get pregnant 1 month following the immunization, second dose--> 4-8 weeks - tetanus- diptheria- acellular pretussis vacine--> given if not received yet |
|
|
asses the comfort is important what do you exactly asses for?
|
Assess pain related to episiotomy, lacerations, incisions, afterpains, and sore nipples.
◯ Assess location, type, and quality of the pain to guide nursing interventions and client education. ◯ Administer pain medications as prescribed. |
|
|
phases of maternal role attainment, taking in phase, dependent- independent, interdependent
|
Dependent: taking-in phase
☐ First 24 to 48 hr ☐ Focus is on meeting personal needs ☐ Rely on others for assistance ☐ Excited, talkative; need to review birth experience with others ■ Dependent-independent: taking-hold phase ☐ Begins on day 2 or 3; up to 10 days to several weeks ☐ Focus on baby care and improving care-giving competency ☐ Want to take charge but need acceptance from others ☐ Want to learn and practice ■ Interdependent: letting-go phase ☐ Focus on family as a unit ☐ Resumption of role (intimate partner, individual) |
|
|
behaviors that are considered maternal bonding
|
holds infant face to face
- maintaing eye contact - infants behvior--> views positive - name the infant - feed and diapering - touches the infant - smilks, talks to and sings to |
|
|
behaviors that are considered lack of mother infant bonding
|
apathy--> infant cries
- disgust when the infants voids, stools, or spits up - turns away from infant - does not seek proximity - does not talk about infant unique features - hands the infant roughly |
|
|
what are signs of mod swings or personal insecurity
|
Feelings of being “down.”
■ Feelings of inadequacy. ■ Feelings of anxiety related to ineffective breastfeeding. ■ Emotional lability with frequent crying. ■ Flat affect and being withdrawn. ■ Feeling unable to care for the infant. |
|
|
how can mother and infant bond?
|
place infant skin to skin
- promote quite and private environment - promote early breastfeedin - encourage parents to bond through cuddling, bathing, feeding, diapering, and inspection - provide frequent praise supper and reassurance - expressing feelings of anxieties, fears, and feelings |
|
|
how can fathers bond with the infant
|
skin to skin contact, eye contact with the infant
- father claims its his infant - father talks, sings, and reads to infant |
|
|
with father talk about the expectations reality and transition of mastery
|
expectations: preconvied ideas
- reality: discovers expectations may not be met, sad frustrated, and jealous transition mastery: father decides to become actively involved in the care of the infant |
|
|
father bond conissits of three phases:
|
◯ Making a commitment – The father takes the responsibility of parenting.
◯ Becoming connected – The father experiences feelings of attachment to the infant. ◯ Making room for the infant – The father modifies his life to include the care of the infant. |
|
|
how do siblings adapt to the there new sibling
|
asses for postive responses from sibling
- interest and concern for infant - increased independence - assses for signs of sibling rivalry and jealousy - asses for regression or aggression toward the infant *let the sbling see the infant, give gift from infant to the sibling - allow older siblings to give care for the infant |
|
|
self care discharge teachings
|
perineal care:
- wipe from front to back--> warm water after voiding after bowel movement - |
|
|
how to give breast care for lactating mothers
|
- wear a well fitting supportive bra for the duration of the lactation
- hand hygiene prior to breastfeeding to prevent infection - relieve breast engorgement--> feedings--> nurse on demand--> 8 to 12 times in a 24 hour periods - breast engorgement--> cool compress - feedings--> warm compress or take shower before breastfeeding - sore nipples--> apple small amount of breast milk for her nipple to allow it to air dry after breastfeeding - have client apply breast creams to soften niples - promote adeqate fluid intake to replace fluid lost from breastfeeding |
|
|
teachings for nonlacting mothers discharge teaching
|
wear a fill fitting, supportive bra for the first 72 hour
- suppression of lactation is necessary for clients who are not breastfeeding--> avoid stimulation or running warm water over breasts for prolonged periods - breast engorgement--> 3 or 5 postpartum day--> cold compress 15 min on and 45 min off, |
|
|
discharge teaching for activities
|
- no heaavy lifting for at least 3 weeks
- do not sit for long time--> DVT--> thrombophlebitis -limit stair climbing - 4-6 weeks--> cesarean birth--> strenuous exercise |
|
|
nutrition discharge teaching
|
- diet should be high in protein to aid in tissue repair
- consume 2000 to 3000 ml--> 2 to 3 L--> fluids - lactating--> 500 claories/day |
|
|
discharge teaching for sexual intercourse and exercises
|
- regain pelvic floor muscle--> kegel exercise
- sexual intercourse -episiotomy/laceration--> healed--> lochia white--> 2-4 weeks-->lubricants for 6 weeks |
|
|
first second third and fourth maneuver
|
first maneuver: what part of the fetus is located at the fundus of the uterus
second manuever: location of the fetal back third maneuver: determine presenting part fourth manuever: location of the cephalic prominence |
|
|
blood loss is how much during vaginal birth
|
500 ml
|
|
|
for bleeding and lacerations what are you gonna give as far as meds?
|
oxytocin--> uterine atony--> vassopressor and antiduriutic effects
mehtylergonvine ( methergine)---> prevent hemorrhage---> do not give if HTN carboprost ( hemabate) ---> uterine atony--> asthma misoprostol cytotec ---> hemorrhage--> not yet approved by FDA |
|
|
apgar score when to take it
|
obtained once at 1 minute and then 5 minutes again
if at 5 minutes less than 7 than you should take it every 5 minutes for 20 minutes |
|
|
what are the apgar scores based on? what are you assessing for?
|
resp: absent-->0-->slow irregular-->1 good cry-->2
HR: absent-->0 slow below 100-->1 above 100--> 2 muscle tone: flaccid-->0 some flexion of extremities--> 1 active motion--> 2 reflex activity: none-->0-->grimace-->1-->vigorous cry color: pale blue-->0-->body pink, blue extremities-->1--> completely pink 2 |
|
|
what antibiotic is given for those mothers infected with chlamydia infections?
|
etheromycin---> eye blindness
|
|
|
vitamin K
|
Im injection--> prevent hemorrhagic diseases
|
|
|
HEP B
|
recommended for all newborns
|
|
|
symptoms of resp alkalosis
|
hyperventilation---> tingling of fingers, circumoral numbness, light headiness, dizziness
* tell her to breathe in cupped hand or bag to reverse |
|
|
specific labor methods for pain
|
dick reed: education and environmental control and relaxation
lamaze: promotes prophylaxis with conditioning and breathing bradley: this is husband- coached childbirth and support by working with and managing the pain rather than being distracted from it |
|
|
fetal scalp electrode
|
FHR
contraindicated if chromamniotiseis, genital herpes, HIV, placenta previa, and vaginal bleeding |
|
|
IUPC monitor
|
frequency and duration of contractions as well as the intensity of contractions
-->duration, freqeuncy, strenght --> 30mmhg--> in early spontaneous labor to 70 in transition to 70-90--> second stage - baseline presssure---> 5-25mmhg postion patient -->left, right, supine, lateral |
|
|
when should FHR assessment frequency increase
|
cat II, and III
--> every 15 min---> active phase every 5 min--> while pushing |
|
|
intiating interauterine resuscitation measures
|
change maternal postion
give 10L o2 mask IV hydration notify physician, request bedside evalaution - consider amnioinfusion - asses uterine activity - consider tocolysis - prepare woman for delivery |
|
|
PNS, SNS, barorceptors, CNS, chemorecptors, hormonal regulation
|
PNS--> decreases FHR SA, AV nodes--> vagus stimulation--> increase HR
SNS--> stim--> increase FHR --> variability--> HYpoxemia barorceptors--> decrease FHR, fetal BP, cardiac output CNS--> variations, baseline variability, vasomotor reflexes chemoreceptors--> changes of o2 and CO2 and PH levels --> stimulate vagal-> increase HR BP hormonal regulation--> epinephrine, noreephinephrine, catecholmines, vasopressin renin- angiotensin--> vasoconstriction |
|
|
tocodynamometer
|
the relative frequency and duration of uterine contractions UC and relative resting tone which is the tone of the uterus between contractions can be measured by this method
* external uterine monitors cannot measure the pressure intensity--> must be palpated |
|
|
assessing the uterus
|
before: tell the woman to void--> distended bladder can result in displacement and atony
- lower head of bed and foot--> woman is supine - support symphysis pubis---> prevent inversion -locate the fundus with other hand using gentle downward pressure - determine the tone of the fundus: firm--> contracted, or soft( boggy) boggy--> massage fundus with palm of hand--> give oxytocin if it is boggy and you do not massage or give oxytocin--> retained placental tissue, birth trauma, uterine atony can lead to postpartum hemorrhage - determine between fundus and umbilical one finger breadth is 1 cm - determine where the uterus is: shift to side--> bladder, if uterus is deviated soft or elevated above umbilicus immediate action is to explain that they need to void--> unable to void--> cauterization |
|
|
expected fundus assesemtn
|
within 12 hours: fundus is located at the level of the umbilicus of 1 cm above the umbilicus and is firm and midline
24 hours later: fundus should be below umbilicus firm and midline by 14 days should not be palpable |
|
|
vagina is assessed using REEDA
|
redness, edema, ecchymosis, dishcarge, and approximation
give ice and encourage cold sitz baths, encourage woman to lie down her side, tighten muscles kegel exercises, use a peri bottle and rinse after elimination |
|
|
what are the CBC results
|
hemacrit
hemoglobin decreases by 1.0 to 1.5 g/dl hemacrit decreaes 3%-4% per 500 m of blood loss |
|
|
thrombosis
|
you can check human sign but not that accurate
asses the legs for calf tenderness, edema, and sensation of warmth, swelling of veins, hard cordlike vessel |
|
|
pulmonary edema risks
|
women who received oxytocin, tocolytics, IV fluids, multiple births, preeclampsia, infection,
|
|
|
temperature elevation
|
less than 100.4 F 24 hours post birth--->hydrate woman, promote relaxation, and rest, reassess in 1 hour after interventions
|
|
|
signs of bladder distention
|
voiding less than 150 ml, uterine atony, displacement of the uterus above the umbilicus to the right, increased lochia, and fullness in the suprapubic area
- the woman should be able to void 4-8 hours, if they can't void they need to be catheterized - straight cath should be done if there is no edema peppermint oil-->hat plus water---> relaxing effect--> urinary tell her to drink 8 glasses |
|
|
diaphoresis
|
*results from less estrogen
- profuse sweating happens at night, it happens because the body is getting rid of the accumulated fluid during pregnancy education: feeling of warmth, sweating, and chills are signs of fever which is a cardinal sign of infection |
|
|
diastsis recti
|
separation of rectus muscle, the separation becomes less apparent as the body returns to a pre- pregnant state
- when assessing the fundus nurse can feel for separation - muscle sorness: ice pack for 15 minutes, heat area, warm shower, analgesia |
|
|
discharge teaching:
|
ecessive lochia more pad in one hour
- return of bright red heavy bleeding after lochia has diminished - foul smelling lochia - pelvic or abdominal tenderness/pain - breasts tender warm, redounded, - freqeuncy, urgency, burning on urination: cystitis - blurry vision, severe headaches: preclampsia - leg pain venous thrombosis, chest pain: pulmonary edema - thoughts of harming infant or self: postpartum depression - lactating women should increase diet to 500 calories per day - smoking around infant: ear infections |

