![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
180 Cards in this Set
- Front
- Back
|
nursing process
|
Assessment
Analysis --Nursing diagnoses (NANDA) Planning --Expected outcomes (NOC) Implementation --Interventions (NIC) Evaluation |
|
|
prioritize planning
|
Level 1
--ABCs (includes acute changes in vital signs) Level 2 --Mental status changes --Acute pain --Acute urinary elimination problems --Untreated medical problems → immediate attention --Abnormal lab values --Risks of infection, safety, or security Level 3 --Lack of knowledge, activity, rest, family coping |
|
|
SBAR communication
|
Situation
Background Assessment Recommendation & Read back |
|
|
"Thinking Like a Nurse" by Tanner
|
Noticing
--A perceptual grasp of the situation at hand Interpreting --Developing a sufficient understanding of the situation to respond Responding --Deciding on a course of action deemed appropriate for the situation, which may include “no immediate action” Reflection --Attending to patients’ responses to the nursing action while in the process of acting --Reviewing the outcomes of the action, focusing on the appropriateness of all of the preceding aspects (i.e., what was noticed, how it was interpreted, and how the nurse responded) |
|
|
Bloom's Taxonomy
|
Analyzing: Breaking material into constituent parts, determining how the parts relate to one another & to an overall structure or purpose through differentiating, organizing, & attributing.
|
|
|
Healthy People 2020
(hearing & vision goals) |
↑ proportion of elementary, middle, & senior high schools that provide school health education
--To promote personal health & wellness related to preventing vision & hearing loss --Emphasize importance of health screenings and checkups ↑ vision rehabilitation ↑ proportion of Federally Qualified Health Centers (FQHCs) that provide comprehensive vision health services ↑ proportion of adults & older adults with hearing impairments who have ever used a hearing aid or assistive listening devices or who have cochlear implants ↑ proportion of adults & older adults who have had a hearing examination on schedule ↑ use of hearing protection devices ↑ proportion of persons with hearing loss & other sensory or communication disorders who have used Internet resources for health care information, guidance, or advice in the past 12 months |
|
|
age related changes
|
30% of those over age 65 have some level of visual impairment
Thickening of the lens with loss of elasticity Degenerative changes Choroid, retina, & optic nerve Decreased contrast sensitivity Delayed recovery from glare Presbyopia |
|
|
refractive errors
|
Emmetropia (Normal vision)
Myopia (Nearsightedness) --Eyeball is too long or cornea has too much curvature, so the light entering your eye is not focused correctly. --Distant objects do not come into focus → blurry, squinting Hyperopia (Farsightedness) --Eyeball is too short or the cornea has too little curvature, so light entering your eye is not focused correctly. --Distant objects usually seen clearly, but close ones do not come into proper focus --Eye strain → ocular fatigue from accommodative effort Astigmatism --Front surface of eye (cornea) is slightly irregular in shape → prevents light from focusing properly on back of eye (retina) --Blurred or distorted vision --Headache, ocular fatigue Presbyopia --Crystalline lens of eye loses flexibility → difficulty focusing on close objects --Natural part of aging process --Blurred near vision --Hold items at arm’s length --Eye fatigue & H/A with close work Aphakia --Absence of lens |
|
|
corrections & surgical interventions
(refractive errors) |
Non Surgical Corrections
--Corrective Lenses (Glasses, Contact Lenses) Keratorefractive Surgery --Laser or knife to correct curvature of cornea --Myopia most commonly corrected Lasik --Surgery laser removes internal layers of cornea Intraocular Lens Implantation --Surgical implantation of an intraocular lens (IOL) --Small plastic lens --Correction for aphakia (absence of the lens) at time of cataract extraction |
|
|
blindness
|
Central visual acuity of 20/200 or worse in corrected eye
Visual field no greater than 200 in widest diameter Elderly at increased risk for visual impairment Chronic disease increases risk for visual impairment (diabetes, hypertension) --Cataracts, glaucoma, diabetic retinopathy, macular degeneration --May cause confused or disoriented --Increased fall/injury risk Psychosocial Impact: --How does visual impairment affect quality of life? --Personal meaning of visual impairment --Disturbed sensory perception --Risk for injury --Self care deficits--reduces ability to remain independent Fear |
|
|
nursing care
(reduced vision) |
Maintain safety & assist in adaptation to environment
Assist in utilizing adaptive measures --Magnifier, large print, talking clock Health promotion --Sunglasses, handwashing, limit alcohol, no smoking, control BP/glucose/cholesterol, eat antioxidant rich foods Administer medications Initiate referrals --Social services, support groups, community resources Encourage all adults especially 40y/o or > to have annual eye exam & IOP measurement |
|
|
conjunctivitis
|
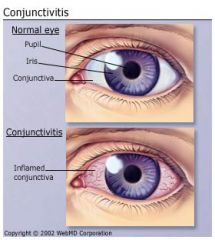
Inflammation or infection of conjunctiva
Usually viral, maybe bacterial, allergic --tearing, burning, itching, edema, discharge “Pink eye” Antibiotic drops or ointments Warm compresses Excellent hand washing Highly contagious (if infectious type/difficult to differentiate between infectious and allergic) |
|
|
glaucoma
|
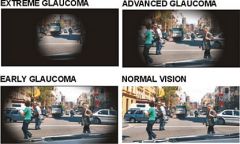
Group of disorders characterized by:
-↑ IOP (increased intraocular pressure) --Progressive or functional damage to eye --IOP regulated by formation & elimination of aqueous humor --Glaucoma is directly related to balance or imbalance of this fluid -Optic nerve atrophy from↑ pressure -Peripheral visual field loss -Leading cause of blindness in African Americans (1 in 10) -2nd leading cause of permanent blindness in US Aqueous humor leaves eye by 2 routes: 1. Trabecular meshwork to Schlemm’s canal 2. Anterior face of iris with absorption into blood vessels All current glaucoma therapies have mechanism of action affecting either production or outflow of aqueous humor |
|
|
assessment and diagnosis
(glaucoma) |
Assess↑ IOP:
Tonometry --Simple painless test, tilt head back & look at ceiling --Cornea anesthetized & tonometer placed on cornea with pressure applied --Pressure exerts force that moves an indicator --Normal pressure (10 – 21mmHg) Measure peripheral & central vision: --Central acuity may remain at 20/20 with severe peripheral loss |
|
|
primary open-angle glaucoma
|
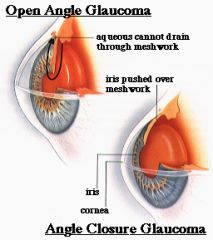
Primary Open Angle Glaucoma (90% of cases)
Outflow disturbance --Fluid normally regulated by constant formation & reabsorption of aqueous humor --↓ aqueous outflow & ↑ intraocular pressure ↑ IOP → slow optic to degeneration → slow, deteriorating vision loss Develops slowly and without symptoms --“Tunnel vision” --Mild eye discomfort --Impairment of peripheral vision before central vision --Bumping into things --↑ IOP > 21mmHg (Norm: 10-21mmHg) |
|
|
POAG care
|
Collaborative Care:
--Keep IOP low to prevent optic nerve damage Open Angle Glaucoma Initial treatment: Drugs ↓ aqueous humor production --β adrenergic blockers – Betoptic, Timoptic --Alpha adrenergic – Alphagan --Cholinergic agents – Pilocarpine --Carbonic anhydrase inhibitors – Diamox,Trusopt ↓ IOP by ↑ aqueous humor outflow: Prostaglandin agonist - Xalatan Secondary: Surgical Interventions → ↓ IOP Argon laser trabeculectomy --ALT- filtering procedure → gradual ↓ pressure Cyclocryotherapy --Freezes parts of ciliary body → ↓ production aqueous humor |
|
|
primary angle-closure glaucoma
|
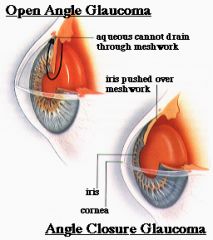
Acute Closed Angle Glaucoma:
Sudden build up of IOP --Complete blockage of filtering angle Emergency situation if untreated → blindness Signs & Symptoms: --Halos &/or rainbows --Pain in & around eye → ↑ IOP --Nausea & vomiting can occur --Ocular redness --Blurred or cloudy vision --↑ IOP > 21mmHg |
|
|
PACG care
|
Collaborative Care:
--Keep IOP low to prevent optic nerve damage Angle Closure Glaucoma: Ocular emergency → requires immediate attention Medications → ↓ IOP --Miotics - Pilocarpine --Hyperosmotic agent - Opthalgan Surgical Interventions --Allow aqueous humor to flow thru newly created opening into normal outflow channels ----Laser peripheral iridotomy ----Surgical iridotomy |
|
|
nursing diagnoses for patients with visual problems
|
Disturbed sensory perception: Visual
Risk for injury Social isolation Self care deficit Fear Anxiety |
|
|
preoperative care
eye surgery |
Prevent injury
↓ Anxiety --Support --Antianxiety agents Assess support systems Complete shampoo or scrub around eyes Administer pre-anesthetic medications --Mydratic eye drops → dilates pupil, e.g., cyclogyl --Cycloplegic eye drops → paralysis --Topical anesthesia Baseline assessment |
|
|
postoperative care
(eye surgery) |
Maintain eye patch or eye shield in place to prevent injury
↑ HOB 30-450 or unaffected side to ↓ IOP Maintain safety Give antibiotics Corticosteroid drops - ↓ inflammatory response Give analgesics as ordered --Use opioids with caution to prevent post-op vomiting or constipation √ Surgical complications --Sudden sharp eye pain, hemorrhage, or corneal edema Avoid activities that ↑ IOP --Sneezing, vomiting, straining |
|
|
hearing loss
|
One of most common physical handicaps in US
May be: --Conductive --Sensorineural --Combination of both Assessment most important |
|
|
conductive hearing loss
|
Conductive loss:
Cerumen Foreign body Perforated tympanic membrane Edema Infection Tumors Otosclerosis |
|
|
sensorineural hearing loss
|

Sensorineural loss:
Prolonged exposure to noise Presbycusis (Age related) Ototoxic substances Menieres Disease Acoustic neuroma Diabetes mellitus Labyrinthitis Infection Myxedema |
|
|
combination hearing loss
|

Combination:
Mixed conductive & sensorineural hearing loss |
|
|
nursing diagnoses for hearing problems
|
Disturbed sensory perception: Auditory
Risk for injury Social isolation Fear Anxiety |
|
|
communicating with hearing impaired
|
Nonverbal:
--Draw attention with hand movements --Avoid covering mouth, chewing, eating, smoking, distracting environment while talking --Use touch --Move closer to better ear --Good lighting Verbal: --Speak normally & slowly…avoid shouting! --Don’t over exaggerate facial expressions or over enunciate --Use simple sentences --Rephrase words --Write name or difficult words --Speak in normal voice directly into better ear |
|
|
hearing loss management
|
Early detection
Assistive devices: Hearing aids -Assist in gradual adjustment of device -Teach proper hearing aid care! --Keep dry --Clean ear mold with mild soap & H2O --Clean debris from hole --Turn off & remove battery when not in use --Check & replace battery frequently --Keep extra batteries available --Store in safe place --Avoid dropping --Avoid temperature extremes --Adjust volume --Avoid oil based products Other devices --Telephone amplifiers --Flashing lights --Animal assistant --Audio amplifiers Medication Surgery |
|
|
Meniere's disease
|
Disorder of inner ear
Cause unknown --Excessive accumulation of endolymphatic fluid in membranous labyrinth Assessment --Sudden severe attacks of whirling vertigo --Roaring or tinnitus, fluctuating hearing loss (20’-24hr) --Pallor, sweating, nausea, vomiting, H/A → exhaustion Can be triggered by: --↑ Na+ intake, stress, allergies, menstrual fluid retention Diagnosis --Hearing testing → audiometric exam --Electronystagmograph (ENG) --X-ray & CT scan → abnormalities in ear structure |
|
|
interventions
(Meniere's disease) |
Low Na+ diet & diuretics
Avoid alcohol, caffeine, nicotine Bedrest to control vertigo Medication treatment: --Atropine (anticholinergic), diazepam (Valium) → n/v --Vestibular suppressants: Meclizine (antivert) Tell brain not to pay attention to abnormal impulses coming from brain Surgical Intervention --Endolymphatic decompression ↓ pressure in labyrinth & creates shunt for fluid drainage --Vestibular neurectomy Balance nerve is cut as it leaves inner ear --Labyrinthectomy Destruction of the membranous labyrinth (inner ear) --Cochlear implant → sensorineural hearing |
|
|
nursing care
(Meniere's disease) |
--Priorities: Maintain safety & minimize vertigo
--Restrict Na+, fluid, nicotine, alcohol --Take medications --Allergy follow up --Learn signs of impending attack --Quiet, darkened room during acute attack --Avoid sudden movements, move head slowly --Medic Alert bracelet |
|
|
Healthy People 2020
(skin goals) |
↑ proportion of:
--persons who participate in behaviors that ↓ their exposure to harmful UV irradiation & avoid sunburn --adolescents in grades 9 -12 who follow protective measures that may ↓ risk of skin cancer --adults aged 18 years & older who follow protective measures that may ↓ risk of skin cancer --elementary, middle, & senior high schools that provide school health education to promote personal health & wellness in sun safety ↓ occupational skin diseases or disorders among full-time workers ↑ % adults 60 years & > who are vaccinated against zoster (shingles) |
|
|
health promotion
(skin) |
Environmental Hazards
Sun Exposure → degenerative changes resulting in premature aging --Loss of elasticity --Wrinkling --Drying of skin --Sun Practices: UVA, UVB - sunscreen 15 SPF or > Cultural & Ethnic Considerations --Sunny climates ↑ incidence of skin cancer --Skin assessment Hygiene Exercise → ↑circulation Rest & Sleep Nutrition → well balanced diet --Vitamins A, B complex, C, & K --Protein --Unsaturated fatty acids |
|
|
drugs that may cause photosensitivity
|
Anticancer - Methrotrexate
Antidepressants - Elavil, Anafranil, Sinequan Antiarrhythmics - Quinidine, Cordarone Antihistamines - Benadryl Antimicrobals - Tetracycline, Zithromax Antifungals - Nizoral Antipsychotics - Thorazine, Haldol Diuretics - Lasix, Hydrodiuril Hypoglycemics - Orinase, Glucotrol NSAIDS - Voltaren, Feldene |
|
|
malignant skin neoplasms
|
Persistent lesion that does not heal, should be have a biopsy
Self examination Risk factors --Fair skin --Chronic UV light (sun) exposure --Family hx of skin cancer --Exposure to tar & systemic arsenical chemicals Living near the equator Outdoor work & frequent recreational activities Dark skinned persons are less susceptible |
|
|
basal cell carcinoma
(non-melanoma skin cancer) |

--Most common & least deadly
--Sun exposed skin --Slow growing & invades local tissue --Metastasis rare --Middle to older adults --Slow enlarging papule with pearly appearance, slight erythema, & translucent border --Excisional surgery |
|
|
squamous cell carcinoma
(non-melanoma skin cancer) |

--Previously damaged skin
--Potentially metastatic & can cause death --Firm reddish rough thick nodules with indistinct borders with scaling & ulceration, opaque & bleeding --Surgical excision |
|
|
malignant melanoma
|
Tumors arising in cells producing melanin
Can metastasize to brain & heart Most deadly skin cancer causing 40,000 deaths/year Risk factors --Cause is unknown --Skin sensitivity, UV radiation --Genetic --Hormonal --Immunologic factors --Recreational lifestyle --Spontaneous gene mutation – 70% of cases |
|
|
clinical manifestations
(melanoma) |

1/3 exist occur in existing nevi or moles
In women, melanoma occurs in lower legs In men, melanoma occurs on trunk, head & neck Melanin causes tumors to most often be brown or black ABCDE assessment --Asymmetry – one side does not match the other --Borders – irregular, ragged, or blurred edges --Color- lack of uniformity in pigmentation --Diameter – > 6mm or the size of a pencil eraser --Elevation |
|
|
collaborative care
(melanoma) |
Initial treatment of Malignant Melanoma is surgery
Spread to the lymph nodes or other sites requires chemo/biological/radiation therapy Gene therapy – being examined Prognostic Factor is the tumor thickness Spread to regional lymph nodes → 50% chance of 5-year survival Phototherapy- use of UV ray --Protection of eyes Radiation Therapy --Malignant cutaneous lesions --Painless with minimal damage to surrounding tissues --Multiple visits --Can cause permanent hair loss Laser Treatment --Cut, coagulated & vaporize tissue Drug Therapy --Antibiotics – topically or systemically --Corticosteriods – anti-inflammatory properties --Antihistamines – for urticaria or pruritis --Topical fluorouracil – 5FU – topical cytotoxic agent used especially for pre-malignant skin disease |
|
|
diagnostic & surgical therapy
(melanoma) |
Skin Scraping
--Scalpel to obtain sample surface cells Electrodesiccation --Tissue destroyed by burning Curettage Instrument --Circular cutting edge – the tissue is scooped away Punch Biopsy --Tissue samples for histological study for small lesions --Small lesions Cryosurgery --Subfreezing temperatures to perform surgery --Liquid nitrogen – causes death and destruction of treated skin --Inexpensive, rapid, leaves little scaring Excision – controlled removal of a cutaneous injury |
|
|
nursing diagnoses
(melanoma) |
Impaired Skin Integrity
Risk for Infection Disturbed Body Image Ineffective Health Maintenance Deficient Knowledge Anxiety Fear |
|
|
health promotion
(melanoma) |
Avoid or reduce sun exposure
Use sunscreen Wear protective clothing Avoid tanning beds Early detection |
|
|
nursing assessment
(melanoma) |
Persons at risk
Sunbathing habits Changes in moles Use magnifying glasses Examine the entire skin surface Examine the diameter of moles --Melanomas are usually larger then 6mm |
|
|
nursing interventions
(melanoma) |
Increase self awareness
--F/U skin exams --Full length mirrors --Learn location of moles & birth marks --Teach sun screening --Protective clothing --No artificial tanning Reduce anxiety Patient education |
|
|
bacterial skin infections
|
Staphylococcus aureus & group A β-hemolytic streptococci
--Major types of bacteria responsible for 10 & 20 skin infections Predisposing factors: --Moisture --Obesity --Skin disease --Systemic corticosteroids --Antibiotics --Chronic diseases such as DM |
|
|
cellulitis
(bacterial skin infections) |

Generalized inflammation of SQ tissues from an infectious process
Often following a break in the skin, e.g., trauma S. Aureus & Streptococci most common Rapidly spread thru lymph system Hot tender erythematous & edematous area with diffuse borders Malaise, chills & fever Treatment: --Moist heat, immobilization, elevation, & systemic antibiotics |
|
|
nursing interventions
(cellulitis) |
Assessment
--Hx of skin trauma --Observe borders, development of abscess formation --Watch for signs of antibiotic sensitivity Nursing Interventions --Administer antibiotics --Elevation of extremity --Warm soaks/moist heat --Reduce pain, bed cradles --IV fluids --Possible surgical interventions Pharmacology --Zithromax, Augmentin, Keflex or Dicloxicillin --Antibiotic therapy may change based on cultures Outcomes: Skin --Normal color --Normal temperature --Non tender --Non swelling --Intact --Active ROM --No pain |
|
|
herpes simplex 1 (HSV-1)
(viral skin infections) |

Oral infections (orolabial)
Transmission is by direct contact with active lesions, saliva --Inoculation of virus onto the skin or mucosal surfaces produces infection Virus remains on nerve root ganglion, exacerbated by stress, trauma, sunlight Symptoms occur about 3-7 days after contact Painful, fever & malaise --Cool compresses Local soothing agents --Abreva Antivirals --Zovarix, Famvir, Valtrex |
|
|
herpes simplex 2 (HSV-2)
(viral skin infections) |

Generally genital infections
Increasing number of genital herpes cases are attributable to HSV-1 Clinical manifestations and treatment same as herpes 1 |
|
|
herpes varicella virus
(viral skin infections) |

The primary infection which causes chicken pox and later herpes zoster (shingles) in adults
Immunization |
|
|
herpes zoster
(viral skin infections) |

Activation of the Varicella (Chicken Pox) Zoster virus
--May persist in dormant stage in dorsal nerve root ganglia & can emerge later → immunosupression or spontaneous Frequent occurrence in immunosuppressed patients. Contagious to anyone who has not had varicella or with immunosuppression. Painful linear patches along dermatome of grouped vesicles on erythematous base. Burning pain & neuralgia preceding outbreak. Neuralgia may continue post-outbreak Usually unilateral on trunk |
|
|
treatment & complications
(herpes zoster) |
Treatment:
Acylovir (Zovirax), Famcyclovir (Famvir), Valacyclovir (Valtrex) --Interferes with viral replication Moist compresses White petrolatum to lesions Pain management --Tylenol, NSAIDs & narcotics (if needed) Systemic corticosteroids (controversial) Complications: Chronic Pain syndrome “Postherpetic neuralgia” --Constant aching burning pain --Hyperesthesia of affected skin ----Treatment: tricyclic antidepressants, gabapentin (Neurontin) ----Topicals: Zostrix TID to healed areas Ophthalmic Complications --Trigeminal nerve damage Nerve Damage --Facial & auditory nerves ----Vertigo & facial weakness |
|
|
nursing diagnoses
(herpes zoster) |
Infection
Impaired Skin Integrity Situational Low Self-Esteem Disturbed Body Image Ineffective Health Maintenance Social Isolation |
|
|
health promotion
(herpes zoster) |
Handwashing
Good personal hygiene Not sharing personal items Older adults > 60y/o who had chickenpox --Zostavax vaccine |
|
|
assessment
(herpes zoster) |
Hx lesions in similar location
Presence of burning, tingling, or pain Recent stressors Recent contact with an infected person Cultures: wound & sometimes blood Note: Use contact precautions during examination |
|
|
nursing interventions
(herpes zoster) |
Priorities:
Patient & family education to prevent infection spread --Other areas --Other people Meticulous skin care Drug therapy Isolation procedures PRN |
|
|
Healthy People 2020
(respiratory goals) |
↑ proportion of adults who are vaccinated annually against seasonal influenza
↑ # of public health laboratories monitoring influenza-virus resistance to antiviral agents ↓ # new invasive pneumococcal infections among adults aged 65 years & older ↑ % of adults who are vaccinated against pneumococcal disease ↓ TB case rate for foreign-born persons living in the United States ↑ proportion of adults with TB who have been tested for HIV ↓ TB ↑ treatment completion rate of all TB patients who are eligible to complete therapy ↑ treatment completion rate of contacts to sputum smear-positive cases |
|
|
respiratory problems in adults & older adults
|
Upper Respiratory
--Influenza --Head and neck cancer Lower Respiratory --Atelectasis --Pneumonia --Tuberculosis --Hemothorax & pneumothorax |
|
|
influenza (the flu)
|
Highly contagious acute viral respiratory infection
High morbidity and mortality rates --Persons > 60 years old with underlying heart or lung disease (higher death rates) --Can be prevented with vaccination Risk factors: -- > 50y/o --Chronic disease – cardiac or pulmonary --LTC residents --Immunocompromised adults --Hospitalizations with in the last year Mandatory identification of high risk or susceptible patients is now required in the acute care setting --Droplet transmission |
|
|
clinical manifestations
(influenza) |
Abrupt onset of systemic symptoms:
--Cough, fever, myalgia, sore throat Milder symptoms: --Similar to common colds (may also occur) Usually subsides within 7 days, depending on the age and underlying health problems of the individual Dyspnea and diffuse crackles --Signs of pulmonary complication Pneumonia: --Common complication --Development of bacterial pneumonia --Development of cough & purulent sputum |
|
|
collaborative management
(influenza) |
Identification of patients who are at risk
Reduce Risks --Transmission/Acquiring Vaccination: --70-90% effective in adults, should be given in the fall (mid-October) before exposure --Health care workers and persons who are high risks should receive vaccinations Goals: --Relief of symptom and prevention of secondary infection --Patient Teaching Symptomatic Management --Rest, increase fluids if able Drug Therapy (if indicated) --Rimantadine (Flumadine) --Amantadine (Symmetrel) --Zanamivir (Relenza) --Oseltamivir (Tamiflu) |
|
|
head & neck cancer
|
Etiology:
--Result of a squamous cell carcinoma, arising from mucosal surfaces Affected areas: --Paranasal sinuses, oral cavity, nasopharynx, oropharynx, & larynx US Epidemiology (2011): --53, 810 new cases of oral & pharyngeal cancer --13,000 deaths --Males more often than females --75% related to alcohol and/or tobacco --HPV-related cancer increasing Usually squamous cell carcinoma and slow growing Usually begins with mucous that is chronically irritated, becoming tougher and thicker Usually leukoplakia and erythroplakia lesions |
|
|
assessment
(head & neck cancer) |
--Lumps in mouth, throat, neck
--Difficulty swallowing --Color changes in mouth or tongue --Oral lesion or sore that does not heal in 2 weeks --Persistent, unilateral ear pain --Persistent/unexplained oral bleeding --Numbness of mouth, lips, or face --Change in fit of dentures --Burning sensation when drinking citrus or hot liquids --Hoarseness or change in voice quality --Persistent/recurrent sore throat --Shortness of breath --Anorexia and weight loss |
|
|
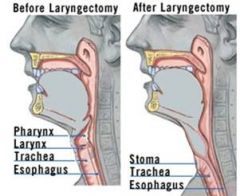
interventions
(head & neck cancer) |
Radiation therapy
Chemotherapy Cordectomy Laryngectomy |
|
|
throat after laryngectomy
|
|
|
|
postoperative care
(laryngectomy) |
First priorities are airway maintenance and ventilation!
Wound, flap, reconstructive tissue care Hemorrhage Wound breakdown Pain management Nutrition Speech and language rehabilitation |
|
|
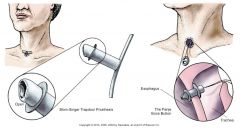
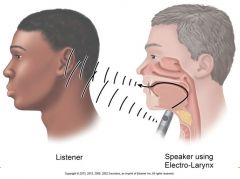
communication after laryngectomy
|
|
|
|
communication after laryngectomy
|
|
|
|
community-based care
(laryngectomy) |
Home care management
Teaching for self management: --Stoma care --Communication --Smoking cessation Psychosocial preparation Health care resources |
|
|
clinical manifestations
(head & neck cancer) |
Signs & sx vary with tumor location
Warning signs --Painless growth in mouth --Ulcer that does not heal or change in fit of dentures --Hoarseness or change in voice quaity --Persistent unilateral sore throat or otalgia --Pain, dysphagia, decreased mobility of tongue, airway obstruction, cranial nerve neuropathies --Change in fit of dentures --Oral cavity cavity (leukoplakia or erythroplakia) warrants biopsy ----Leukoplakia, erythroplakia, or gray, dark brown or black spots Lump in the neck or hoarseness for 3-4 weeks require medical intervention |
|
|
nutritional therapy
(head & neck cancer) |
Parenteral fluids during the first 24-48 hours postoperatively
Tube/enteral feedings: --NGT, Gastrostomy tube (PEG) --Observe for tolerance of tube feedings Swallowing evaluation &anticipate for swallowing problems (thick vs. thin liquids) --Progress from thick to thin & from bland diet to soft, regular --Speech language pathologist Aspiration precautions: If tolerating oral as well as tube feeds --Supraglottic swallowing exercise --High back rest Monitor caloric intake Administer antiemetic medications |
|
|
lower respiratory problems
|
Atelectasis
Pneumonia Tuberculosis Hemothorax/pneumothorax |
|
|
atelectasis
|

The collapse of alveoli or a lobule or larger lung unit
Etiology: Airway obstruction of bronchus --Impedes passage of air to and from the alveoli ----Air is trapped & absorbed into the blood stream ----External communication is blocked, replacement of air from outside is impossible --Results from exudates and secretions (common cause) --Usually seen postoperatively Common in cardiac, thoracic and upper abdominal surgeries Complications: --Acute: Pneumonia --Chronic: Pulmonary fibrosis |
|
|
collaborative management
(atelectasis) |
Assessment
--Identification of high risk patients --Subjective and objective data Plan: Goal is absence of atelectasis --Lungs that have collapsed because of an obstruction should be re-expanded as rapidly as possible to avoid the complications of pneumonia or lung abscess Interventions: Mobilization/ambulation of postoperative patients --Turned frequently Deep breathing and coughing exercises --Postural drainage/chest physiotherapy --Nebulizer treatments Suctioning to stimulate coughing Mechanical aids for lung inflation: Incentive spirometry, positive airway pressure system, IPPB, etc Evaluation |
|
|
pneumonia
|
An excess of fluid in lungs resulting from an inflammatory process
Triggered by many infectious organisms & inhalation of irritating agents Caused by bacteria, viruses, mycoplasmas, fungi, rickettsiae, protozoa, & helminths (worms) Infectious pneumonias categorized as: --Community-acquired pneumonia (CAP) --Hospital-acquired pneumonia (HAP) ----More likely to be resistant to some antibiotics than CAP ----20% - 50% mortality rate |
|
|
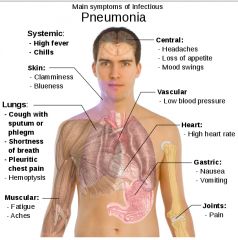
clinical manifestations
(aspiration pneumonia) |
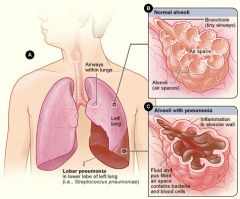
Symptoms are similar to other types of pneumonia:
Fever, chills, productive cough, Pleuritic chest pain Confusion, hypoxia Diminished breath sounds Crackles, sonorous & sibilant wheezing Altered respiratory pattern (Tachypnea) Abnormal chest radiograph --Normal initially in time shows consolidationPatients with sign & sx of respiratory failure may require mechanical ventilation |
|
|
ventilator-associated pneumonia (VAP)
|
Incidence increasing, especially with ET tubes in place for mechanical ventilation
“Ventilator bundles” reduce incidence --Hand hygiene --Oral care --Head of bed elevation |
|
|
lab assessment
(pneumonia) |
Gram stain, culture and sensitivity of sputum
CBC ABGs Serum BUN Electrolytes Creatinine |
|
|
imaging & diagnostic
(pneumonia) |
Chest x-ray
Pulse oximetry Transtracheal aspiration Bronchoscopy |
|
|
community-based care
|
Home care management
Teaching for self-management Health care resources |
|
|
pulmonary tuberculosis
|
Highly communicable; caused by Mycobacterium tuberculosis
Transmitted via aerosolization Secondary TB Incidence increase related to onset of HIV |
|
|
clinical manifestations & assessments
(TB) |
Clinical Manifestations:
--Progressive fatigue --Lethargy --Nausea --Anorexia --Weight loss --Irregular menses --Low-grade fever, night sweats --Cough, mucopurulent sputum, blood streaks Assessment --History --Physical assessment --Clinical manifestations |
|
|
diagnostic assessment
(TB) |
Manifestation of signs/symptoms:
--NAAT (results in 2 hr) --Sputum smear for acid-fast bacillus --Sputum culture of M. tuberculosis --Tuberculin (Mantoux) test—PPD given intradermally in forearm --Induration of 10 mm or greater diameter = positive for exposure --Positive reaction does not mean that active disease is present, but does indicate exposure to TB or dormant disease. |
|
|
PPD skin test
|

|
|
|
interventions
(TB) |
Combination drug therapy with strict adherence:
--Isoniazid --Rifampin --Pyrazinamide --Ethambutol Negative sputum culture = no longer infectious |
|
|
community-based care
(TB) |
Home care management
Teaching for self-management Health care resources |
|
|
hemothorax & pneumothorax
|
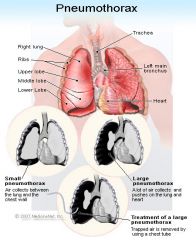
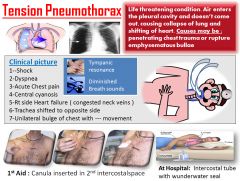
Pneumothorax
--Presence of air or gas in pleural space that causes lung collapse Tension pneumothorax --Occurs when air enters pleural space during inspiration thru 1 way valve caused by blunt chest trauma & can’t exit upon expiration --↑ pressure compresses blood vessels & ↓ venous return → ↓CO → death can occur quickly if untreated Hemothorax --Accumulation of blood in pleural space |
|
|
tension pneumothorax
|
|
|
|
diagnostics
(hemothorax & pneumothorax) |
Common Risks
--Blunt chest trauma --Penetrating chest wounds --Closed/occluded chest tube Diagnostics --ABG – specimen placed in heparinized syringe on ice --CXR --Thoracentesis – may be used to confirm hemothorax |
|
|
assessment
(hemothorax & pneumothorax) |
Pleuritic pain
Respiratory distress --↑ RR, ↑ HR, hypoxia, cyanosis, dyspnea, use of accessory muscles Tracheal deviation to unaffected side (tension pneumo) ↓ or absent BS (affected side) Asymmetrical chest wall movement Anxiety Percussion --Hyperresonance (pneumothorax) --Dullness (hemothorax) Subcutaneous emphysema |
|
|
interventions
(hemothorax & pneumothorax) |
Assess & monitor respiratory status
--BS, document ventilator settings q1h, ABGs, V/S, O2 sat, positioning Monitor chest tube drainage Give meds as ordered --Anxiolytics – lorazepam (Ativan) or midazolam (Versed) --Analgesics – morphine or fentanyl Provide emotional support |
|
|
chest tube placement
|
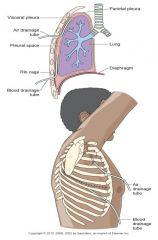
|
|
|
chest tube chambers
|
Chamber 1: collects the fluid draining from the patient
Chamber 2: water seal that prevents air from entering the patient’s pleural space Chamber 3: suction control of the system |
|
|
chest tube drainage system
|
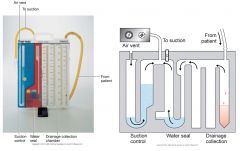
|
|
|
systematic review of chest drains conclusions
|
Lack of research on most aspects of nursing care of chest tubes
--Dressings --Optimal positioning of tubing & drainage unit --Frequency for changing drainage collection units --Clamping tubes --Pt position & optimal breathing patterns during removal Need for rigorous research |
|
|
clinical guidelines for care
(chest tubes) |
Management of Chest Tube Drainage Systems
Patient --Ensure that the dressing on the chest around the tube is tight and intact. Depending on agency policy and the surgeon's preference, reinforce or change loose dressings. --Assess for difficulty breathing. --Assess breathing effectiveness by pulse oximetry. --Listen to breath sounds for each lung. --Check alignment of trachea. --Check tube insertion site for condition of the skin. Palpate area for puffiness or crackling that may indicate subcutaneous emphysema. --Observe site for signs of infection (redness, purulent drainage) or excessive bleeding. --Check to see if tube “eyelets” are visible. --Assess for pain and its location and intensity, and administer drugs for pain as prescribed. --Assist patient to deep breathe, cough, perform maximal sustained inhalations, and use incentive spirometry. --Reposition the patient who reports a “burning” pain in the chest. Drainage System --Do not “strip” the chest tube. --Keep drainage system lower than the level of the patient's chest. --Keep the chest tube as straight as possible, avoiding kinks and dependent loops. --Ensure the chest tube is securely taped to the connector and that the connector is taped to the tubing going into the collection chamber. --Assess bubbling in the water seal chamber; should be gentle bubbling on patient's exhalation, forceful cough, position changes. --Assess for “tidaling.” --Check water level in the water seal chamber, and keep at the level recommended by the manufacturer. --Check water level in suction control chamber, and keep at the level prescribed by the surgeon (unless dry suction system is used). --Clamp the chest tube only for brief periods to change the drainage system or when checking for air leaks. --Check and document amount, color, and characteristics of fluid in the collection chamber, as often as needed according to the patient's condition and agency policy. --Empty collection chamber or change the system before the drainage makes contact with the bottom of the tube. --When sample of drainage is needed for culture or other laboratory test, obtain it from the chest tube; after cleansing chest tube, use a 20-gauge (or smaller) needle and draw up specimen into a syringe. Immediately Notify Physician or Rapid Response Team for: --Tracheal deviation --Sudden onset or increased intensity of dyspnea --Oxygen saturation less than 90% --Drainage greater than 70 mL/hr --Visible eyelets on chest tube --Chest tube falls out of the patient's chest (first, cover the area with dry, sterile gauze) --Chest tube disconnects from the drainage system (first, put end of tube in a container of sterile water and keep below the level of the patient's chest) --Drainage in tube stops (in the first 24 hours) (Ignatavicius 2013, p. 637) Ignatavicius, Workman. (2013). Medical-Surgical Nursing: Patient-Centered Collaborative Care, 7th Edition. W.B. Saunders Company. Retrieved from <vbk:978-1-4377-2801-9#outline(40.13.1.7.1.3.1.1.1.2)>. |
|
|
notify MD or Rapid Response Team immediately if...
(chest tubes) |
Tracheal deviation
Sudden onset or ↑SOB O2 sat < 90% Drainage > 70 mL/hr CT falls out of chest --1st cover dry sterile dsg & tape 3 sides CT disconnects from drainage system --1st put end of tube in sterile H2O & keep below level of chest Drainage in tube stops within 1st 24 hours |
|
|
Healthy People 2020
(cardiovascular goals) |
↑ overall CV health in US
↓ CV deaths --From 129:100,000 to 100:100,000 ↑ BP screening & ↓ # people with HTN ↑ cholesterol screening & ↓ # people with high cholesterol ↑ aspirin use with no hx CVD --Women 55-79 y/o --Men 45-79 y/o ↑ awareness of s & sx heart attack & importance of early emergency care Follow guidelines --BMI --Low saturated fat/cholesterol diet --Na+ intake --Physical activity --Moderate alcohol consumption --Take prescribed medications ↑ # eligible pts with MI or strokes who receive timely artery-opening therapy as specified by current guidelines --Fibrinolytics w/in 30 min hospital arrival for MI --PCI w/in 90 min for MI --Acute reperfusion w/in 3hrs sx onset for strokes |
|
|
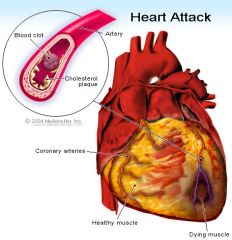
coronary heart disease (CHD)
or coronary artery disease (CAD) |
Coronary heart disease (CHD) is a leading cause of death worldwide
About 50% of men & 64% of women who died suddenly of CHD had no previous sx of this disease (Rosamond et al., 2008) 30% of patients who have an MI die within 5 years (AHA, 2010) |
|
|
women
(CAD) |
Heart disease is the No. 1 killer of women, and is more deadly than all forms of cancer combined.
Heart disease causes 1 in 3 women’s deaths each year, killing approximately one woman every minute. An estimated 43 million women in the U.S. are affected by heart disease. Ninety percent of women have one or more risk factors for developing heart disease. Since 1984, more women than men have died each year from heart disease. The symptoms of heart disease can be different in women and men, and are often misunderstood. |
|
|
cultural awareness
(CAD) |
African Americans have highest prevalence of HTN in world
American Indians have highest percentage of smokers High cholesterol is > common among African Americans & Hispanics |
|
|
clinical manifestations
(CAD) |
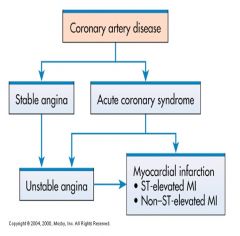
Angina Pectoris
--Stable angina* – results if lack of oxygen supply is temporary & reversible Acute Coronary Syndrome (ACS) --Develops when the oxygen supply is prolonged & not immediately reversible --Unstable angina* --Myocardial Infarction* ----Non-ST segment elevation MI (NSTEMI) ----ST segment elevation (STEMI) Sudden Cardiac Death |
|
|
myocardial infarction (MI)
(CAD) |
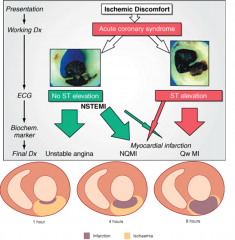
Divided by ACC/AHA
--Non-ST MI (NSTEMI) --ST elevation MI (STEMI) |
|
|
types of MI
(CAD) |
Transmural MI
--Involves entire thickness of myocardium Subendocardial MI --Damage has not penetrated thru entire thickness Described by area (wall) of occurrence --Anterior, Inferior, Lateral, Septal, etc --Anterior wall MI’s have the highest mortality rate |
|
|
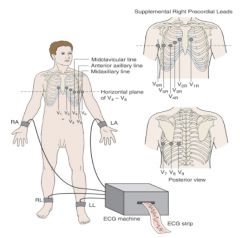
lab assessment
(MI) |
--Troponin T and troponin I
--Creatine kinase-MB (CK-MB) --Myoglobin --Imaging assessment --12-lead electrocardiograms --Cardiac catheterization |
|
|
ECG lead placement
|
|
|
|
assessment
(acute MI) |
Pain
--Chest pain not relieved: hallmark of MI --Diabetics --Women --Older Adults Nausea & vomiting Fever CV symptoms Sympathetic Nervous System Stimulation |
|
|
pain management
(acute MI) |
--Nitroglycerin
--Morphine sulfate --Oxygen --Position of comfort; semi-Fowler’s position --Quiet and calm environment |
|
|
ineffective tissue perfusion
(cardiopulmonary) |
Interventions:
Drug therapy (aspirin, thrombolytic agents) Restoration of perfusion to injured area limits amount of extension, improves left ventricular function Complete sustained reperfusion of coronary arteries in first few hours after MI has decreased mortality |
|
|
thrombolytic therapy
(MI) |
Fibrinolytics dissolve thrombi in coronary arteries, restore myocardial blood flow
--Tissue plasminogen activator --Reteplase --Tenecteplase |
|
|
other drug therapies
(MI) |
Glycoprotein (GP) IIB/IIIa inhibitors
Once-a-day beta blockers ACE inhibitors or angiotensin receptor blockers Calcium channel blockers Ranolazine (Ranexa) |
|
|
reperfusion therapy
(MI) |
Myocardial tissue can become increasingly ischemic and necrotic
Thrombolytic therapy using fibrinolytics dissolves thrombi in the coronary arteries and restores myocardial blood flow |
|
|
medical management
(MI) |
Pain relief and decreased myocardial oxygen requirements through preload and afterload reduction
Drug therapy Intra-aortic balloon pump Immediate reperfusion |
|
|
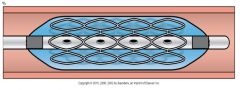
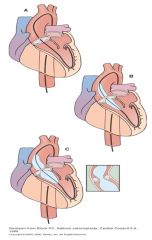
percutaneous transluminal coronary angioplasty
(MI) |
Clopidogrel before procedure
IV heparin after procedure IV or intracoronary nitroglycerin or diltiazem Possible IV GP IIb/IIIa inhibitors Long-term therapy, antiplatelet therapy, beta blocker, ACE inhibitor, or ARB |
|
|
percutaneous transluminal coronary angioplasty
(MI) |

|
|
|
coronary stent
(MI) |
|
|
|
nursing interventions
(post CC/PCI) |
Frequent/continuous monitoring of V/S, ECG, SpO2 , coagulation profile, e.g., activated clotting time (ACT), PT/PTT
Check puncture site, distal pulses, skin color/temp, capillary refill, urine output, etc Watch for complications: --Bleeding, hematoma, pseudoaneurysm, retroperitoneal bleed, compartment syndrome, reocclusion, dysrhythmias |
|
|
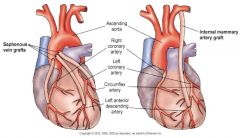
coronary artery bypass graft
(MI) |
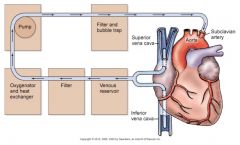
|
|
|
coronary artery bypass graft
(MI) |
|
|
|
coronary artery bypass graft
(MI) |
Preoperative care
Postoperative care --Manage F&E balance --Complications—hypotension, hypothermia, hypertension, bleeding, cardiac tamponade, change in level of consciousness |
|
|
nursing interventions
(pre-op coronary artery bypass graft) |
Interventions:
NPO Reinforce teaching Complete pre-op checklist --Type & cross match blood products --Labs (check for abnormal values), ECG, CXR, Echo, cath report, old medical record, etc --Consent: Surgical, Anesthesia, Blood --Skin prep: clip versus shave, betadine shower --Medication “on call “ to OR Pain relief/comfort measures, therapeutic environment Anxiolytic meds, integrative cardiac medicine, sleep meds Pre-op considerations: emergent vs. elective, choice of grafts (e.g. radial: non-dominant hand, job a factor) |
|
|
immediate post-op period
cardiac surgery patient |
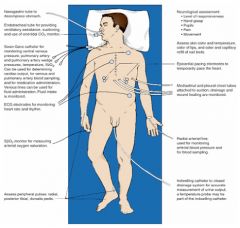
|
|
|
common complications
(cardiac surgery) |
--Bleeding (early or delayed)
--Electrolyte imbalance --Arrhythmias --Atelectasis, pneumothorax --Low cardiac output syndrome --Hypertension/Hypotension --Renal failure --Infections (e.g., graft sites, sternal wound) --Stroke, cognitive impairment “pump head” --Metabolic –related, e.g., hyperglycemia --Respiratory failure, e.g., diaphragmatic paralysis |
|
|
collaborative problems
(post-acute MI) |
Dysrhythmias (AKA arrhythmias)
--Most common complication Heart Failure (HF) Cardiogenic Shock |
|
|
priority problems
(acute MI) |
--Acute pain
--Ineffective tissue perfusion: Cardiopulmonary --Decreased cardiac output --Anxiety --Activity intolerance --Ineffective therapeutic regimen management --Ineffective coping Common Collaborative Problem --Depression |
|
|
planning
(acute MI) |
Overall goal:
Oxygen supply will meet demand --Relief of pain --No progression of MI --Immediate & appropriate treatment --Cope effectively with associated anxiety --Cooperation of rehabilitation plan --Modify or alter risk factors |
|
|
nursing interventions
(acute MI) |
Administration of oxygen, positioning
Continuous ECG monitoring Frequent vital signs Pain relief (e.g. morphine), rest & comfort Anxiety Emotional & behavioral reactions --Communicate with family --Provide support Nursing measures to prevent complications &/or progression of MI |
|
|
nursing interventions: discharge
(acute MI) |
Discharge Teaching & Home Care
Patient teaching --Factors that precipitate angina --Avoid exposure to extremes of weather Rehabilitation --Cardiac rehab, physical exercise Resumption of sexual activity --Emotional readiness --Physical training |
|
|
valvular heart disease
|
Mitral stenosis
Mitral regurgitation (insufficiency) Mitral valve prolapse Aortic stenosis Aortic regurgitation (insufficiency) |
|
|
aortic valve (AV) dysfunction
|
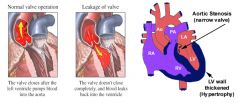
|
|
|
main causes of valvular heart disease
|
Rheumatic Heart Disease
Endocarditis Marfan’s syndrome Congenital Age-related valve calcification (Aortic Stenosis) ACS/MI |
|
|
assessment
(valvular heart disease) |
Sudden illness or slowly developing symptoms over many years
Ask about attacks of rheumatic fever, infective endocarditis; ask about possibility of IV drug abuse Chest x-ray, ECG, stress test |
|
|
clinical manifestations
(valvular heart disease) |
Vary with type of valvular disease
Can be asymptomatic Common: --Heart Failure symptoms (dyspnea, orthopnea, PND) --Angina --Murmur --Syncope |
|
|
nonsurgical management
(valvular heart disease) |
Rest
Drug therapy --Diuretics --Beta blockers --Digoxin --Oxygen --Nitrates --Vasodilators --Anticoagulants |
|
|
surgical management
(valvular heart disease) |
Reparative procedures
Balloon valvuloplasty Direct or open commissurotomy Mitral valve annuloplasty Replacement procedures |
|
|
heart valves
|
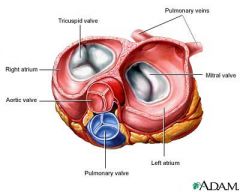
|
|
|
percutaneous transluminal balloon valvuloplasty
|
Perform in the Invasive Cardiac Lab
Femoral artery approach Pre & post-op management similar to PCI patients |
|
|
ineffective endocarditis
|
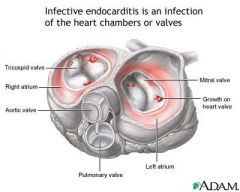
Microbial infection involving the endocardium
Those at high risk: --IV drug abusers --Valve replacement recipients --People who have had systemic infections --People with structural cardiac defects Possible ports of entry --Oral cavity --Skin rash --Lesion/abscess --Infection --Surgery or invasive procedure |
|
|
manifestations
(ineffective endocarditis) |
--Murmur
--Heart failure --Arterial embolization --Splenic infarction --Neurologic changes --Petechiae --Splinter hemorrhages |
|
|
diagnostic assessment
(ineffective endocarditis) |
Positive blood cultures
New regurgitant murmur Evidence of endocardial involvement by echocardiography |
|
|
nonsurgical management
(ineffective endocarditis) |
Antimicrobials
Activities balanced with adequate rest |
|
|
surgical management
(ineffective endocarditis) |
Removal of infected valve
Repair or removal of congenital shunts Repair of injured valves and chordae tendineae Draining of abscesses in heart or elsewhere |
|
|
guidelines for antibiotic prophylaxis
(ineffective endocarditis) |
People with the following conditions are considered to be at the highest risk of developing infective endocarditis. Preventive antibiotics are generally recommended for people with the following conditions before certain procedures:
--A prosthetic heart valve --Valve repair with prosthetic material --A prior history of infective endocarditis --Many congenital (from birth) heart abnormalities, such as single ventricle states, transposition of the great arteries, and tetralogy of Fallot, even if the abnormality has been repaired. Patent foramen ovale, the most common congenital heart defect, does not require prophylaxis AHA, 2007 |
|
|
dysrhythmias
|
AKA Arrhythmias
Abnormal cardiac rhythms --May include rate, rhythm or both Prompt assessment of abnormal cardiac rhythm and patient’s response is critical |
|
|
cardiac conduction system
|
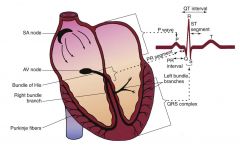
Sinoatrial node
--Electrical impulses 60-100 beats/min --P wave on ECG Atrioventricular junction --PR segment on ECG --Contraction known as “atrial kick” Bundle of His --Right bundle branch system --Left bundle branch system |
|
|
electrocardiographic waveforms
|
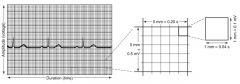
Electrocardiographic waveforms are measured in amplitude (voltage) and duration (time).
|
|
|
electrocardiographic waveforms
|
Each segment between the dark lines (above the monitor strip) represents 3 seconds when the monitor is set at a speed of 25 mm/sec. To estimate the ventricular rate, count the QRS complexes in a 6-second strip and then multiply that number by 10 to estimate the rate for 1 minute. In this example, there are 9 QRS complexes in 6 seconds. Therefore the heart rate can be estimated to be 90 beats/min.
|
|
|
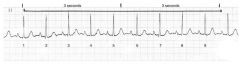
normal ECG
|

|
|
|
ECG rhythm analysis
|
1) Determine heart rate
2) Determine heart rhythm 3) Analyze P waves 4) Measure PR interval 5) Measure QRS duration 6) Interpret rhythm |
|
|
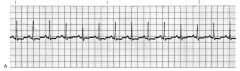
normal sinus rhythm
|
Rate: 60-100 beats/min
Rhythm: regular P waves: Present, consistent configuration, one P wave before each QRS complex PR interval : 0.12-0.20 second and constant QRS duration: 0.04-0.10 second and constant |
|
|
sinus dysrhythmias
|
Variant of NSR
Results from changes in intrathoracic pressure during breathing |
|
|
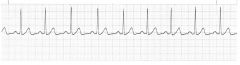
sinus bradycardia
|
|
|
|
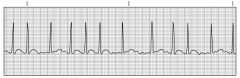
sinus tachycardia
|
|
|
|
supraventricular tachycardia
|
Rapid stimulation of atrial tissue occurs at rate of 100-280 beat/min with mean of 170 beats/min (adults)
Paroxysmal supraventricular tachycardia rhythm is intermittent, terminated suddenly with or without intervention |
|
|
atrial fibrillation
|
Associated with atrial fibrosis and loss of muscle mass
Common in heart disease such as hypertension, heart failure, coronary artery disease Cardiac output can decrease by as much as 20% to 30% Total depolarization of atrial activity without effective atrial contraction Chronic or intermittent Usually occurs with underlying heart disease, such as RHD, CHF, cardiomyopathy, pericarditis, thyrotoxicosis, alcohol intoxication, valvular disease, caffeine use, electrolyte disturbance, cardiac surgery Patient-centered collaborative care --Risk for PE, VTE --Antidysrhythmic drugs --Cardioversion --Percutaneous radiofrequency catheter ablation --Bi-ventricular pacing --Maze procedure |
|
|
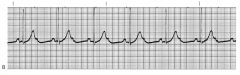
ventricular dysrhythmias
|

More life-threatening than atrial dysrhythmias
Left ventricle pumps oxygenated blood through the body to perfuse vital organs and other tissues (Ventricular dysrhythmias. A, Normal sinus rhythm with unifocal premature ventricular complexes (PVCs). B, Normal sinus rhythm with multifocal PVCs (one negative and the other positive)) |
|
|
premature ventricular complexes
|
Result of increased irritability of ventricular cells—early ventricular complexes followed by a pause
|
|
|
ventricular tachycardia
|
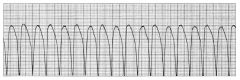
Also called V tach—repetitive firing of irritable ventricular ectopic focus, usually at 140-180 beats/min
|
|
|
ventricular fibrillation
|
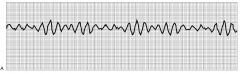
Also called V fib—result of electrical chaos in ventricles
|
|
|
ventricular asystole
|
Also called ventricular standstill—complete absence of any ventricular rhythm
|
|
|
nonsurgical management
(dysrhythmias) |
Antidysrhythmic agents
Drugs used during cardiac arrest Vagal maneuvers—carotid sinus massage, vagal reflex |
|
|
pacemakers
|
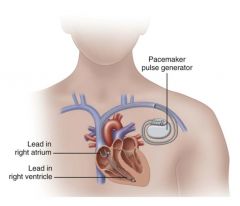
Temporary pacing—invasive and noninvasive
Permanent pacemakers (PPM) Indications: --Chronic AF with slow ventricular response --Fibrosis or sclerotic changes of cardiac conduction system --Sick sinus syndrome --SA node dysfunction --Tachyarrhythmias --Third degree AV-Block |
|
|
cardioversion
|
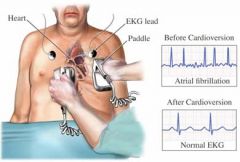
Synchronized countershock
Used in emergencies for unstable ventricular/supraventricular tachydysrhythmias Used electively for stable tachydysrhythmias resistant to medical therapies Rapid AF, SVT, stable ventricular dysrhythmias (w/ BP & pulse) Synchronized countershock during QRS complex Non-emergency If elective & dysrhythmia > 48 hrs, may give anticoagulant few wks & hold Digoxin 48hrs before Nursing Responsibilities: --Informed consent --Conscious IV sedation & analgesic --V/S, ECG monitoring --Respiratory support --A-B-C-D of life support |
|
|
defribillation
|
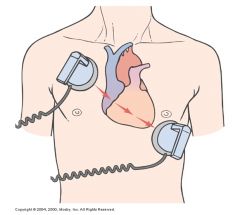
Asynchronous countershock that depolarizes critical mass of myocardium simultaneously to stop re-entry circuit and allow sinus node to regain control of heart
Most effective method of terminating VF Ideally performed within 15 to 20 seconds of onset of arrhythmia Passage of direct current electrical shock through heart to depolarize cells Intent to all SA node to resume role New defibrillators come with “defib pads” rather than paddles |
|
|
ICD
|
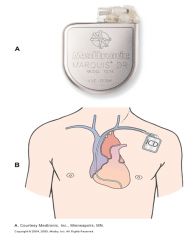
Treatment for life-threatening ventricular arrhythmias
Lead system placed via subclavian vein to endocardium Pulse generator is implanted over pectoral muscle |
|
|
shock
|
Syndrome characterized by ↓ &/or impaired tissue perfusion
--Inadequate delivery O2 & nutrients to support vital organs Cause & initial presentation of various types of shock may differ --Same physiological responses of cells to hypoperfusion Treatment strategies differ for each type of shock |
|
|
nursing priorities
(shock) |
Shock prevention
Early & rapid intervention Ongoing systematic assessment Close collaboration with health care team --Anticipate orders Prevent complications --ARDS, DIC, ARF, Multiple organ dysfunction syndrome Nutritional support Promote rest, comfort & ↓ anxiety Support family members |
|
|
classifications of shock
|
Low flow shock
--Hypovolemic shock --Cardiogenic shock Distributive shock --Anaphylactic shock --Septic shock --Neurogenic shock |
|
|
hypovolemic shock
|
Loss of intravascular fluid volume
--Hemorrhage, GI loss, fistula, drainage or diuresis Blood volume insufficient to meet metabolic demands of tissues Signs & Sx --Confusion --↑ HR --↓ CO --↑ RR & depth --↓ B/P --Cool skin --↓ Body temperature --CBC - ↓ Hgb & HCT |
|
|
cardiogenic shock
|
Cardiac failure → ↓ tissue perfusion
Heart is damaged & unable to supply sufficient blood to body Examples: --Myocardial infarction --Pulmonary hypertension --Heart failure --Valve disorders --Abnormal heart rhythms Signs & Sx --Impaired cerebral perfusion → Anxiety & delirium --↑ HR --↓ BP --↑ RR --Pulmonary congestion --Crackles --Cyanosis, pallor, cool clammy skin & ↓ capillary refill --↓ Renal blood flow → Na+ & H20 retention with ↓ U/O |
|
|
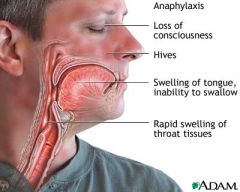
anaphylatic shock
|
Caused by a severe systemic response to an allergen resulting in:
--Massive vasodilation --↓ Perfusion --↓ Venous return --↓ Cardiac output Acute life threatening rx --Drug, chemical, vaccine, food, insect venom --Can lead to respiratory distress Signs & Sx --Syncope --Swelling of lips & tongue --Angioedema --Wheezing & stridor --↓ BP, ↑ HR --Chest pain --Flushing --Pruritis --Urticaria --Nausea/vomiting |
|
|
anaphylactic shock
|

|
|
|
anaphylactic shock
|
|
|
|
septic shock
|
Overwhelming infection leads to:
--↓ BP --↓ Blood flow Vital organs may not function properly or may fail Occurs in people with underlying disease Gram negative & positive bacteria Mortality rates 45% - 60% |
|
|
neurogenic shock
|
Vasodilation as result of loss of balance between parasympathetic & sympathetic stimulation
Mimics hypovolemia although blood volume is adequate Common Causes: --Spinal cord injury (SCI) --Spinal anesthesia, medications --Nervous system damage Signs & Sx --↓ SVR --↓ BP --Bradycardia --Syncope/fainting --Dry, warm skin |
|
|
stages of shock
|
Initial
--May not be clinically apparent --Lactic acid build up begins Compensatory --Attempt homeostasis --Tissue Hypoxia --Goal to fix underlying problems—prevent progression Progressive --Begins when all compensatory mechanism fail --Hallmarks of decreased cellular perfusion & altered capillary permeability --Multisystem organ involvement Refractory --Recovery is unlikely |
|
|
diagnostics
(shock) |
ABG
Urine output < 30mL/hr BUN to assess for ↓ renal perfusion Blood glucose Electrolyte levels Blood cultures WBC & ESR may ↑ in the presence of infection |
|
|
pharmacological interventions
(shock) |
Cardiogenic shock
--Sympathomimetics --Vasopressors --Vasodilators --Diuretics Hypovolemic Shock --No pharmacotherapy unless severe… need fluid replacement --Fresh whole blood, PRBCs --Colloids --Crystalloids:Lactated Ringers solution & 0.9% NS, 3% ---NaCl Anaphylactic Shock --Epinephrine --Bronchodilators --Antihistamines --Hydrocortisone --Vasopressors Septic Shock --Antibiotic therpy --Fluid administration --Vasopressor drugs Neurogenic Shock --Heparin or LMWH --Osmotic diuretics, glucose, LR, steroids |
|
|
nursing diagnoses & interventions
(shock) |
Ineffective peripheral, cerebral & renal tissue perfusion re: ↓ circulating blood volume
--Neuro status --Monitor B/P at frequent intervals for hypotension ----Readings > 20mmHg below normal range → indicate hypotension → dizziness, orthostatis ----BP must be > 80/60 for adequate coronary & renal perfusion --√ Peripheral pulse perfusion ----Report coolness & pallor of extremities, delayed capillary refill Ineffective peripheral, cerebral & renal tissue perfusion re: ↓ circulating blood volume --√ ↓ Cardiac perfusion --√ Urine output < 30mL with adequate intake --Electrolytes – ↓ Na+, ↑ K+, √ s/sx --Administer fluids – to ↑ volume ----Hypovolemic shock – amt lost is replaced ----Cardiogenic shock – fluids limited to prevent overload ----Septic Shock – LR, plasma & blood Impaired gas exchange re: altered oxygen supply --Ensure a patent airway --Monitor respirations --Monitor pulse oximetry --Monitor mental status Impaired gas exchange re: altered oxygen supply --Encourage patient to breath slowly & deeply to promote oxygenation --Administer O2 --Monitor ABG ----Be alert to hypoxemia → ↓O2 sat & ↓PaCO2 ----Acidosis may be present |

