![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
118 Cards in this Set
- Front
- Back
|
Macrominerals (Major)
|
3.45% of body weight
-Calcium (Ca+) -Phosphorous (P-) -Sodium (Na+) -Chlorine (Cl-) -Magnesium (Mg+) -Potassium (K+) -Sulfur (S-) |
|
|
Trace minerals (micro)
|
0.55% of body weight
-Copper (Cu) -Cobalt (Co) -Fluorine (F) -Iodine (I) -Iron (Fe) -Manganese (Mn) -Molybdenum (Mo) -Selenium (Se) -Zinc (Zn) |
|
|
Classified as Essential Minerals (Micro)
|
-Ni
-Si -Vanadium -Chromium -Tin |
|
|
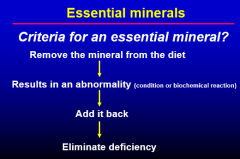
Essential Minerals
|
|
|
|
Possibly Essential Minerals
|
Under investigation:
-Arsenic -Barium -Bromine -Cadmium -Strontium |
|
|
Nonessential Minerals
|
-Aluminum
-Antimony -Lead** -Mercury** Found in bone, can accumulate **Very TOXIC when occur in high amounts |
|
|
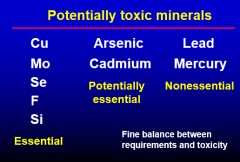
Potentially Toxic Minerals
|
|
|
|
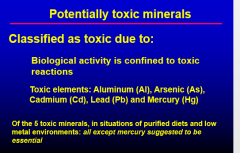
Classified as Toxic Due to:
|
|
|
|
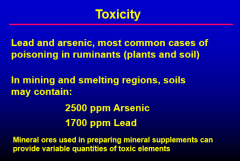
Toxicity
|
|
|
|
General Functions of Essential Minerals
|
1. Constituent of skeletal structure
Ca, P, Mg 2. Maintain osmotic pressure Na+, K+, Mg+ |
|
|
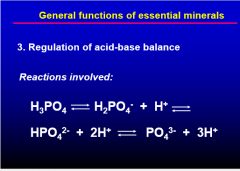
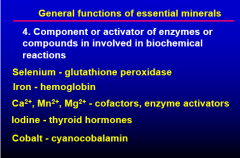
General Functions of Essential Minerals
|
|
|
|
General Functions of Essential Minerals (slide 2)
|
|
|
|
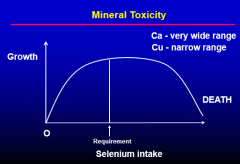
Mineral Toxicity Graph
|
|
|
|
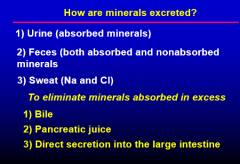
How are Minerals Excreted?
|
|
|
|
Factors Affecting Mineral Requirements
|
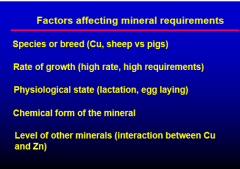
|
|
|
Calcium Sources
|
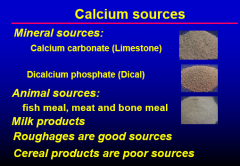
|
|
|
Functions of Calcium
|
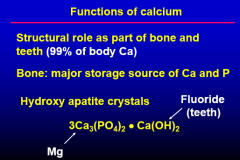
|
|
|
Other Functions of Calcium
|
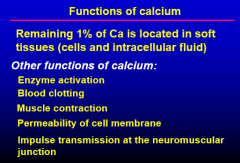
|
|
|
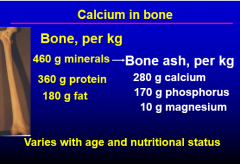
Calcium in Bone
|
|
|
|
Calcium Deficiency
|
-P and Mg can produce deficiency symptoms as well
-Same deficiency symptoms as vitamin D -Including reduced growth -Ricketts -Osteomalacia -Osteoporosis |
|
|
Ricketts (Calcium Deficiency
|
-Young animals
-Misshapen bones, enlarged joints, lameness and stiffness |
|
|
Osteomalacia (Calcium Deficiency)
|
-Mature animals
-Softening of bone due to decalcification |
|
|
Osteoporosis (Calcium Deficiency)
|
-decalcification of bone w/a reduction in bone mass
-20 million Americans, 80% women -Bone mass decreases after menopause |
|
|
Calcium Deficiency Results From
|
-Absence of vitamin D (helps movement of Ca)
-Low Ca intake -Low P intake -Abnormal Ca:P ratio -High fat diet, Ca soap formation -High requirement during pregnancy & lactation |
|
|
Calcium Deficiency in Dairy Cows
|
-Milk Fever:
-$10 million loss per year -high producers 12-72 hours post calving -blood Ca drops to 4-5 mg% -cow typically lose control of hind legs -give calcium gluconate I.V. |
|
|
Calcium: phosphorous ratio in diet formulation
|
-Ideal is 2:1 to 1:1
-Bone: have a ratio of 1.67:1, Ca to P in hydroxyl apatite -Why not 10:1? -high Ca & low P, formation of insoluble CaPO4 in the lumen -if high P and low Ca, also have reduced absorption |
|
|
Sources of Phosphorous
|
-Animals sources: meat & bone & fish meal
-Low in roughages but high in concentrates -Commercial sources: -dicalcium phosphate (Dical) -monocalcium phosphate (Monocal) -defluorinated rock phosphate (F removed) |
|
|
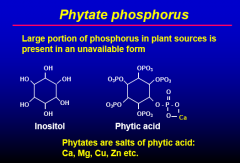
Phytate Phosphorous in Plant Source
|
|
|
|
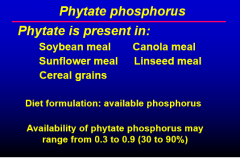
Phytate Phosphorous Present In
|
|
|
|
Phytase
|
-Commercial phytase is available
-Intrinsic phytase activity -is high in wheat products |
|
|
Phosphorus for Ruminants
|
-use of total phosphorus is adequate
-bacterial and fungal phytases |
|
|
Functions of Phosphorus
|
-Similar functions as calcium
-Part of hydroxyl apatite -Acid-base balance (HPO4-) -Carbohydrate metabolism (phosphorylated intermediates) |
|
|
Phosphorous (P-) Function
|
-80% in bone
-20% in soft tissues -Teeth -PO4- bonds -high energy bonds, ATP, ADP -Phospholipids (lecithin/phosphatidyl choline) -DNA, RNA, ATP, ADP |
|
|
Phosphorus Deficiency
|
-Especially a concern in tropical & subtropical areas - soils are deficient in P
-Symptoms are similar to Ca & vitamin D deficiency -Ricketts and Osteomalacia -Condition known as: -'pica' which is also referred to as: depraved appetite -animals will eat almost anything they see: soil, fences, ect. |
|
|
Phosphorous Toxicity
|
-Urinary Calculi - water belly (steers) or kidney stones
-1/3 of the P in grains is digested & utilized -2/3 of the P is in the form of Phytate -Microbes can break down & make Phytate P available -Phytase |
|
|
Functions of Magnesium
|
-Structural component of bone (60-70% of Mg)
-Bone ash: 0.5-0.7% Mg -Enzyme activation, is complexed w/ATP, ADP, & AMP, enzyme activator in carbohydrate & lipid metabolism, binds messenger RNA to ribosomes -Arginase = metalloenzyme, Mg is a functional part -a urea cycle enzyme |
|
|
Symptoms of Magnesium Deficiency
|
-Vasodilation (reduces bl. pressure)
-Hyperirritability, convulsions -Tetany, I.e. grass tetany or grass staggers (also known as hypomagnesemia) -Typical symptoms: -nervousness -tremors -twitching of facial muscles -staggering gait & convulsions |
|
|
Prevention of Grass Tetany
|
-Magnesium enema: give 60g MgCl2 in 200 ml of water
-Feed 1:1:1, MgO:TM. Salt:Grain -Start 2 weeks before turning cattle on pasture |
|
|
Magnesium Supplementation
|
-Magnesium carbonate, MgCO3
-Magnesium oxide MgO -Magnesium sulfate (Epsom salts) - MgSO4 |
|
|
Functions of Sodium
|
-osmotic balance
-acid base balance -absoption of carbohydrates & AA (Na+ pump) -Transmission of nerve impulses -body content is ~0.2% |
|
|
Sources of Sodium
|
-Plant & plant products are poor sources (0.01 tp 0.06%)
-animal products are good sources (meat meals, meat & bone meal, 0.1 to 0.8%) -especially those of marine origin: fish meals |
|
|
Sodium (sodium chloride, salt)
|
-usual practice is to supplement rations (diet)
-0.3 to 0.5% of the ration (diet) -or free choice salt blocks -salt, salt+iodine, salt+all trace minerals |
|
|
Sodium Deficiency
|
-during lactation (Na+ & Cl- secreted in milk)
-rapidly growing animals (fed cereal or forage based diets) causes reduced growth -under tropical conditions (Na+ loss in sweat) -decreased osmotic pressue --> dehydration --> weakness -poor growth --> reduced carbohydrate & AA absorption |
|
|
Sodium deficiency - Pica
|
-'salt craving'
-licking of wood, soil, or sweat of other animals -loss of appetite, decreased growth, unthrifty appearance, reduced milk production, weight loss |
|
|
Sodium & Nutritional Wisdom
|
-sodium is the only nutrient for which most animals show nutritional wisdom
-nutritional wisdom is when an animal detects a nutrient deficiency & seeks out a source of that nutrient -very toxic |
|
|
Chlorine
|
-closely associated w/Na+
|
|
|
Functions of Chlorine
|
-regulation of osmotic pressure
-HCl, gastric juice - protein digestion -electrolyte -Cl required for amylase activity |
|
|
Chlorine Deficiency
|
-deficiency only on purified or concentrated diets
-reduced growth, reduced milk production, depraved appetite, emaciation -Chlorine deficiency (hypochloremic): may lead to an abnormal increase in alkali (bicarbonate) or alkalosis |
|
|
Potassium
|
-After Ca & P, potassium is next most abundant mineral
-represents 0.3% of body dry matter (2/3 in skin & muscle) |
|
|
Functions of Potassium
|
-osmotic balance
-acid-base balance (cation/anion balance) -transmission of nerve impulses -activator of cofactor in enzyme systems: -adenosine triphosphatase -carbonic anhydrase -salivary amylase |
|
|
Sources of Potassium
|
-content in plants generally high (alfalfa > 2.0%)
-excess K can be problem for dairy cows fed alfalfa -grains (0.3-0.8%) -vegetable proteins (1.0-2.5%) -animal products (0.3-2.0%) |
|
|
Potassium Deficiency
|
-is rare, has to be induced
-reduced appetite -decreased growth, weakness, tetany -degeneration of vital organs, nervous disorders, diarrhea |
|
|
Sulfur (S-)
|
-not essential for normal production function
-organic metabolites are essential -S- containing AA -Glycoproteins -small quantities of inorganic sulfur in the body (as sulfates) -almost all sulfur is contained in methionine & cysteine (both protein bound) |
|
|
Sulfate forms occur in
|
Chondroitin sulfate
-cartilage -bone -tendons -blood vessels -HEPARIN |
|
|
Sulfur & Ruminant animals
|
-some inorganic sulfate is present in forages
-rumen microbes: incorporate sulfate into S-containing AA (only few species) -sulfur requirement of rumen microbes -insufficient S -reduced microflora -reduction in digestibility -optimum level in ruminant diets: 0.6-0.24% -not problem in diets w/adequate protein level -rumen bypass methionine (protected) |
|
|
Sulfur Deficiency in Ruminant animals
|
-reduced weight gain, appetite
-decreased wool growth (sheep) -dullness, weakness, emaciation -dairy cattle: decreased intake, decreased DM digestibility & milk production |
|
|
Inorganic Sulfur
|
Monogastric animals:
-2 wk old pigs -fed purified diets containing 0.8% methionine -tolerated 1/2 met replaced w/inorganic sulfate -no effect on weight gain, feed/gain ratio, collagen content of tendons |
|
|
Micro-Trace minerals
|
-takes long time to induce deficiencies & toxicity
-geographical deficiency problems |
|
|
Fluorine
|
-1920's - use of phosphorus supplements containing excessive F increased toxicosis in animals
-1942 - correlation between F concentration in drinking water & community prevalence of dental carries -most plants - limited ability to absorb F from soil -forages contain 2-20 ppm F (DM basis) -Cereals & byproducts 1-3 ppm F -Major source for humans is water -source for animals is mineral supplements & food ingredients (esp. bone, meat & bone meal) |
|
|
Flourine - Bones & Teeth
|
-0.02% to 0.05% of the apatite molecule
-soft tissues & fluids rarely contain more than 2-4 ppm) -causes crystals to become: -larger -harder -more resistant to acid |
|
|
Fluorine Toxicity
|
Chronic fluorosis in grazing livestock
1. continuous consumption of high-F supplements 2. drinking water high in F (3-15 ppm or >) 3. grazing F-contaminated forages close to industrial plants -eg. phosphate ore processors, aluminum, steel, copper smelters, brick & ceramic product factories, coal fired electricity generating plants |
|
|
Levels of Fluorine Toxicity
|
-1 ppm - reduction in dental carries
(1 ppm added to water in some locations) -2 ppm - mottled enamel -8ppm - osteosclerosis - abnormal hardening -110 - reduced growth, inhibition of enolase in glycolysis -2 ppm F is upper limit for the F concentration in water for livestock & poultry -2 ppm can cause mottling (dental fluorosis), serious toxicity problems observed when F>5 ppm |
|
|
Preventing Fluorine Toxicity
|
-Know sources of supplemental phosphate
-Sources of water that could potentially cause problems -wells on ranches w/toxicity problems: water: 4 to 12 ppm F |
|
|
Copper (1)
|
-Formation of hemoglobin
-Ceruloplasmin (feridoxase, contains Cu) Conversion between ferric (Fe3+) & ferrous (Fe2+) forms, permits binding to iron transport protein transferrin or incorporation into hemoglobin or myoglobin -Oxidation - reduction reactions Cu2+ cytochrome oxidase in oxidative phosphorylation |
|
|
Copper (2)
|
-Component of enzymes w/oxidase functions (e.g. tyrosinase, amine oxidase, ascorbic acid oxidase)
-Formation of melanin - skin, hair, pigments -Activation of amylase -Integrity of myelin sheath -cross-linking of connective tissue (collagen) -component of lysyl oxidase (adds an OH group to lysine & permits cross-linking) |
|
|
Copper Homeostasis
|
-controlled by rate of absorption
-regulated by intestinal mucosa -protein: metallothionein (Cu & Zn) -absorption by active transport & diffusion -90% of Cu, transported by ceruloplasmin (metalloprotein) |
|
|
Copper Absorption
|
Absorption can be decrease by:
-dietary phytates -high levels of Ca, Fe, Zn, and Mo -Excretion into bile, fecal excretion Absorption: -Adult monogastrics: 5-10% -Young animals: 15-30% -Ruminant animals: 1-3% |
|
|
Copper (3)
|
-CuSO4 - used as a growth promotant in young swine
-Sheep - very susceptible to copper toxicity -Accumulates in the liver, necrosis of cells, jaundice |
|
|
Copper Toxicity in Sheep
|
-Copper levels as low as 10 ppm has caused toxicity when molybdenum is low (<3ppm)
-Toxicity often occurs when trace mineral supplements designed for cattle are fed to sheep |
|
|
Cattle Breed & Copper Toxicity
|
-Holsteins can tolerate 100 ppm copper without problems
-Jerseys are susceptible to copper toxicity at >50ppm |
|
|
Copper Deficiency
|
-Poor growth
-Depigmentation of hair -Scouring as a secondary symptom Wool: Depigmentation decrease: -growth -tensile strength -crimp (disulfide bridges) -stringy or steely wool -Anemia -Nervous lesions: inability to coordinate bodily movements |
|
|
Molybdenum Functions
|
Metalloenzymes:
-purine breakdown -xanthine oxidase Hypoxanthine & Xanthine --> uric acid -Aldehyde oxidase -reduction of cytochrome C -electron transfer chain |
|
|
Molybdenum Deficiency
|
-Not reported under practical conditions
-No characteristic symptoms -Requirements for rats & young chickens are less than 0.2 ppm |
|
|
Cobalt
|
-Constituent of Vitamin B12
-Same deficiency symptoms as Vitamin B12, deficiency symptoms are due to a deficiency of Vitamin B12 |
|
|
Sources of Cobalt
|
-Most feedstuffs contain adequate levels of Co
-Soil deficiency is primarily in Florida & East Coast states |
|
|
Toxicity of Cobalt in Ruminant animals
|
-Wide safety margin between toxicity & requirement
-Unlikely under practical conditions -Poorly retained in the body vs. copper, excess is excreted |
|
|
Iron
|
-60-70% in hemoglobin & myoglobin
-oxidation - reduction reactions, electron transfer system -cytochromes & flavoproteins |
|
|
Sources of Iron
|
-Green leafy materials, most legumes, seed coats
-Feeds of animal origin: -meat & bone meal, meat meal, blood meal -Milk is a poor source, for animals under intensive conditions |
|
|
Iron Deficiency
|
-Decreased numbers of RBCs
-Sows: unless kept outdoors, no access to soil or pasture -Milk is deficient in iron -Injections of iron dextran |
|
|
Iron Deficiency - Baby Pig Anemia
|
-most common iron deficiency
-Signs: -pale skin -transparent ears |
|
|
Iron Deficiency - Signs
|
-Unthrifty appearance, listlessness
-Heavy breathing, enlarged heart -Diarrhea (secondary symptom) |
|
|
Selenium in Soil
|
-Soil concentration is between 0.1 and 2 ppm, average = 0.3 ppm
-high seleniferous soils: 2 to 10 ppm Se, potentially toxic to livestock -low seleniferous soils: supplement Se |
|
|
Functions of Selenium
|
-Scavenges free radicals
-Vitamin E absorption & retention -Recent discovery: involved in the synthesis of thyroid hormones |
|
|
Selenium Deficiency Symptoms
|
-Ruminants: white muscle dz
-vitamin E & selenium Monogastric animals: edema (membrane degradation) -Suppressed immune system -Impaired reproduction |
|
|
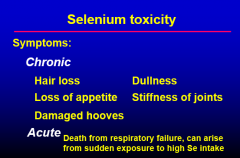
Selenium Toxicity Symptoms
|
|
|
|
Selenium Regulated by FDA
|
-FDA allows only 0.1 ppm of added selenium
-Maximum Tolerable Concentration is 2.0 ppm |
|
|
Iodine
|
-Thyroid gland: contains 50% of body I
-Triodothyronine (T3) -Thyroxine (T4) -Regulated basal metabolism |
|
|
Iodine Deficiency
|
-Goiter, enlarged thyroid gland
-hairless at birth |
|
|
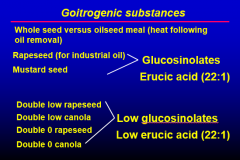
Goitrogenic Substances
|
-Enlarged thyroid gland
-Interfere w/synthesis of T3 & T4 -Crops which are members of the Brassica family |
|
|
Goitrogenic Substances (2)
|
|
|
|
Iodine Supplementation
|
-granular iodized salt
-iodized salt blocks |
|
|
Manganese Functions
|
-enzyme activation (as Mn2+)
pyruvate carboxylase & cholesterol synthesis -phosphate transferases (CHO metabolism) -decarboxylases -enzymes involved in synthesis of mucopolysaccharides & glycoprotein |
|
|
Deficiency of Manganese (1)
|
-may be promoted by high dietary levels of Ca & P
-reduced growth -low manganese diets for cows & goats cause depressed or delayed estrous & conception & increased abortion -skeletal abnormalities: "perosis" (slipped tendon) in young chickens, related to cartilage formation |
|
|
Deficiency of Manganese (2)
|
-Perosis (poultry)
-Poor bone development -Altered glucose metabolism |
|
|
Zinc
|
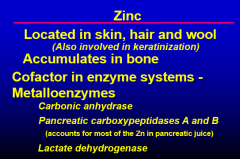
|
|
|
Zinc (2)
|
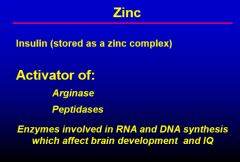
|
|
|
Zinc Homeostasis
|
-controlled by rate of absorption
-regulated by intestinal mucosa -protein: metallothionein (Cu & Zn) |
|
|
Zinc Absorption
|
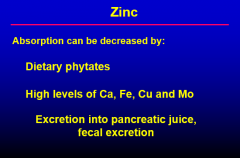
|
|
|
Zinc Deficiency Symptoms
|
-decreased growth, appetite
-aggravated by high levels of Ca in the diet -skin lesions: -reddening of skin, eruptions, scabs (Parakeratosis) -Reduced feathering -Reduced immune function |
|
|
Potentially Toxic Minerals
|
- Aluminum
- Arsenic - Cadmium - Lead |
|
|
Aluminum
|
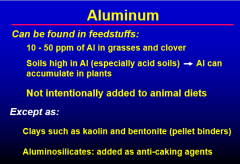
|
|
|
Metabolism of Aluminum
|
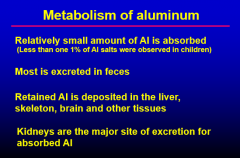
|
|
|
Aluminum Toxicity
|
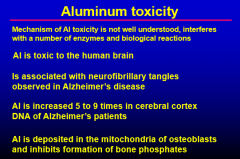
|
|
|
Aluminum Toxicity in Animals (1)
|
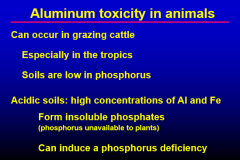
|
|
|
Aluminum Toxicity in Animals (2)
|
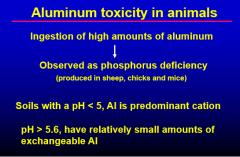
|
|
|
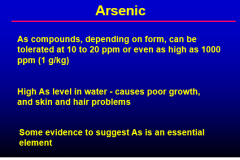
Arsenic (1)
|
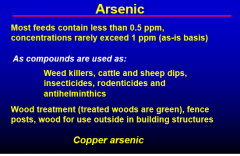
|
|
|
Arsenic (2)
|
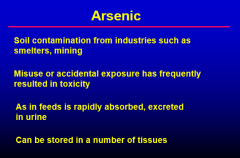
|
|
|
Clinical Signs of Arsenic Toxicity
|
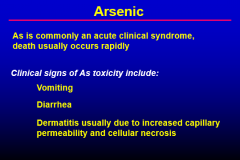
|
|
|
Arsenic (3)
|
|
|
|
Arsenic: Chronic toxicosis in cattle
|
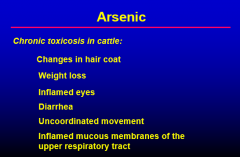
|
|
|
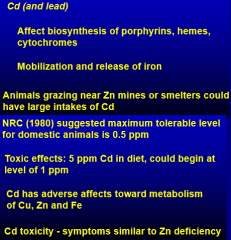
Cadmium
|
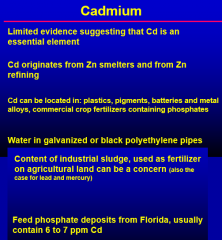
|
|
|
Aspects of Cadmium Metabolism
|
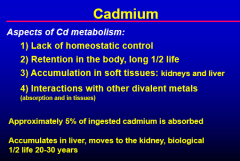
|
|
|
Cadmium Toxicosis
|
|
|
|
Cadmium Toxicosis Symptoms
|
-decreased feed intake
-reduced growth -infertility -liver & kidney damage -scaly skin -anemia -enlarge joints |
|
|
Sources of Lead in the Environment
|
-environmental lead can occur in plants, soil & water , hazard to grazing livestock
-soils, rocks, vehicle exhaust, pipes, paints, soldered Cu piping, batteries -lead smelting & mining areas can contaminate pastures |
|
|
Lead Metabolism
|
-gastrointestinal absorption, also skin & respiratory
-about 40% of absorbed lead is deposited in the skeleton relatively immobile -accumulates in liver & kidney -excreted in bile & urine |
|
|
Metabolic effects of Lead
|
-lead inhibits enzymes dependent on the presence of free sulfhydryl groups
-interferes w/heme synthesis -acute toxicity is the main issue -impaired cardiac performance, neuronal degeneration |
|
|
Treatment of Lead Toxicity
|
-treatment w/chelating agents to increase urinary excretion of lead & bile
-e.g. thiamin-EDTA -caution: loss of essential metals is also enhanced (Zn, Cu, etc.) |

