![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
98 Cards in this Set
- Front
- Back
|
ENDOMETRIUM
|
The endometrium is the mucous membrane that lines the inside of the uterus (womb). The endometrium changes throughout the menstrual cycle. It becomes thick and rich with blood vessels to prepare for pregnancy. If the woman does not get pregnant, part of the endometrium is shed, causing menstrual bleeding.
|
|
|
3 Layers of the UTERUS:
|
1. endometrium
2. Myometrium 3. Perimetrium |
|
|
The muscular outer layer of the uterus
|
Myometrium
|
|
|
Fertilization:
|
-72 h after Ovulation
-AKA: conception and impregnation) is the union of an ovum and a spermatozoon. - occurs in the outer third of a fallopian tube, the ampullar portion |
|
|
Fimbriae
|
fine, hairlike structures that line the openings of the fallopian tubes. A combination of peristaltic action of the tube and movements of the tube cilia help propel the ovum along the length of the tube.
|
|
|
IMPLANTATION:
|
- 6 -8- 10 days after fertilization
|
|
|
1. Zygote
2. Embryo 3. Fetus |
1. From fertilization to implantation
2. From implantation to 5-8 weeks 3. From 5-8 weeks until term |
|
|
What are the 3 factors that determine FERTILIZATION?
|
1. equal maturation of both sperm and ovum,
2. the ability of the sperm to reach the ovum, 3. the ability of the sperm to penetrate the zona pellucida and cell membrane and achieve fertilization |
|
|
Developing embryo or fetus and placental structures throughout pregnancy
|
Conceptus
|
|
|
Age of Viability
|
The earliest age at which fetuses could survive if they were born at that time, generally accepted as 24 weeks, or fetuses weighing more than 400 g
|
|
|
**Where does Fertilization occur?
|
outer third of the fallopian tube
|
|
|
It's where the Union of sperm and egg takes places and it's the beginning of Pregnancy?
|
-Fertilization
|
|
|
How does sperm travel the fallopian tube?
|
-their Flagella (tails) and
-uterine contractions |
|
|
Normally,only 1 spermatozoon is able to penetrate the cell membrane of the ovum. Once it penetrates the cell, the cell membrane changes composition to become impervious to other spermatozoa. What is an exception to this formation?
|
hydatidiform mole, in which multiple sperm enter an ovum; this leads to abnormal zygote formation
|
|
|
a complication of pregnancy in which the placenta grows in the lowest part of the womb (uterus) and covers all or part of the opening to the cervix
|
Placenta Previa
|
|
|
At what point is the Endometrium called DECIDUA?
|
Implantation: contact b/w the growing structure and the uterine endometrium
|
|
|
Occurs approx. 8 to 10 days after fertilization?
|
Implantation
|
|
|
a fertilized egg has implanted outside the uterus
|
Ectopic pregnancy
-most common site fallopian tubes -baby can not survive -caused by a condition that blocks or slows the movement of a fertilized egg through the fallopian tube to the uterus. This may be caused by a physical blockage in the tube. |
|
|
What "estogen" (hormone) causes the uterine endometrium to continue to grow in thickness and vascularity, instead of sloughing off as in a usual menstrual cycle.
|
HCG (human chorionic gonadotropin), secreted by the trophoblast cells p 193.
|
|
|
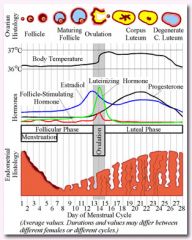
This phase follows ovulation and lasts from about day 15 to day 28. After the follicle ruptures as it releases the egg, it closes and forms a corpus luteum.
|
|
|
|
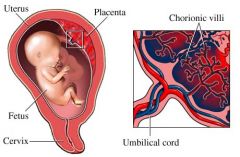
As early as the 11th or 12th day, miniature villi that resemble probing fingers, reach out from the single layer of cells into the uterine endometrium to begin formation of the placenta. At term, almost 200 such villi will have formed
|
chorionic villi
|
|
|
Fetal side of the placenta,
where the gases will exchange b/w the mother and the fetus? |
-Chorionic villi
|
|
|
sprout from the chorion in order to give a maximum area of contact with the maternal blood.
Embryonic blood is carried to the villi by the branches of the umbilical arteries, and after circulating through the capillaries of the villi, is returned to the embryo by the umbilical veins. Thus, the villi are part of the border between maternal and fetal blood during pregnancy |
|
|
|
What is the purpose of HCG?
|
act as a fail-safe measure to ensure that the corpus luteum of the ovary continues to produce progesterone and estrogen. This is important b/c, if the corpus luteum should fail and the level of progesterone fall, the endometrial lining will slough and the pregnancy will be lost.
|
|
|
What is the purpose of the Chorionic Membrane?
|
purpose is to form the sac that contains the amniotic fluid
-outermost fetal membrane |
|
|
A second membrane lining the chorionic membrane, ______ _____, or Amnion, forms beneath the chorion.
|
Amniotic membrane
|
|
|
"hormone of mothers"
|
-Progesterone: necessary to maintain the endometrial lining of the uterus during pregnancy, as a result of the continuation of the Corpus Luteum.
|
|
|
"Hormone of Women"
|
estrogen:contributes to the mammary gland development in prep. for lactation and stimulates uterine growth to accommodate the developing fetus
|
|
|
At what week does oxygen and other nutrients, such as glucose, amino acids, fatty acids, minerals, vitamins, and water, osmose from the maternal blood through the cell layers of the chorionic villi into the villi capillaries
|
by the 3rd week
|
|
|
What is able to cross into fetal circulation from the mother?
|
it is important that a woman take no nonessential drugs (including alcohol and nicotine)
|
|
|
What is a potential complication of twins?
|
nutrients vessels may fuse in utero, causing one twin to receive more blood than the other (twin-to-twin transfusion)
|
|
|
Fertilizied egg has implanted outside the uterus?
|
Ectopic pregnancy
|
|
|
When is Uterine perfusion, and thus placental circulation most efficient?
|
when the woman lies on her left side. This position lifts the uterus away from the inferior vena cava, preventing blood from being trapped in the woman's lower extremities
|
|
|
What happens to the placental circulation if the woman lies on her back and the weight of the uterus compresses the vena cava?
|
placental circulation can be so sharply reduced that supine hypotension (very low maternal blood pressure and poor uterine circulation) occurs
|
|
|
what is the weight of the placenta at term?
|
400 to 600 g (1 lb)
|
|
|
Placenta weighs less than normal (400 to 600 g), what does this suggest?
|
suggests that circulation to the fetus may have been inadequate
|
|
|
Placenta weighs > 400 to 600 g, what does this indicate about the circulation?
|
circulation to the fetus was threatened
|
|
|
The fetus of a woman with diabetes may also develop a larger-than-usual placenta, Why?
|
b/c of excess fluid collected between cells.
|
|
|
first placental hormone produced,can be found in maternal blood and urine as early as the first missed menstrual period (shortly after implantation has occurred
|
hCG
|
|
|
Test used as proof that placental tissue is no longer present after birth
|
hCG test
|
|
|
purpose of hCG?
|
act as a fail-safe measure to ensure that the corpus luteum of the ovary continues to produce progesterone and estrogen
|
|
|
Corpus Luteum:
|
(yellow body) it's going to die, unless you are pregnant and then it will continue to grow & secrete hormones, hCG and progesterone to maintain pregnancy
|
|
|
How can you tell if the mother has lost the baby without doing an ultrasound?
|
-progesterone levels and hCG levels will be low
|
|
|
What is the 2nd hormone produced that contributes to the woman's mammary gland development in preparation for lactation and stimulates uterine growth to accommodate the developing fetus?
|
Estrogen
|
|
|
What hormone reduces the contractility of the uterus during pregnancy, preventing premature labor?
|
Progesterone
|
|
|
Human Placental Lactogen (growth-promoting and lactogenic (milk-producing) properties:
|
promotes mammary gland (breast) growth in preparation for lactation in the mother
|
|
|
Place where gases & blood will exchange b/w the mother & embryo?
|
Chorionic Villi- Fetal side of placenta
-embedded in the endometrium |
|
|
outermost fetal membrane. Its purpose is to form the sac that contains the amniotic fluid
|
Chorionic membrane
-no nerve supply |
|
|
second membrane lining the chorionic membrane
|
amniotic membrane or amnion, forms beneath the chorion
-no nerve supply |
|
|
constantly being newly formed and reabsorbed
- never becomes stagnant -aid in fetal growth: muscular development b/c it allows the fetus to move) -maintains temp |
Amniotic fluid
-shock absorber-pressure -umbilical cord compression preventor |
|
|
most important purpose of amniotic fluid?
|
shield the fetus against pressure or a blow to the mother's abdomen
|
|
|
excessive amniotic fluid, (more than 2000 mL in total, or pockets of fluid larger than 8 cm on ultrasound?
|
hydramnios
-fetus is unable to swallow the amniotic fluid -occur in women with diabetes |
|
|
A disturbance of kidney function may cause _______, or a reduction in the amount of amniotic fluid (less than 300 mL in total, or no pocket on ultrasound larger than 1 cm)
|
oligohydramnios
|
|
|
pH of Amniotic fluid?
|
7.2
urine pH : 5.0-5.5 |
|
|
umbilical cord
|
provides a circulatory pathway that connects the embryo to the chorionic villi of the placenta
|
|
|
gives the cord body and prevents pressure on the vein and arteries that pass through it.
|
Wharton's Jelly: if there is a compression of the blood vessels then you will cutoff the blood, nutrients and O2
|
|
|
An umbilical cord contains:
|
only one vein (carrying blood from the placental villi to the fetus) but two arteries (carrying blood from the fetus back to the placental villi
|
|
|
The number of veins and arteries in the cord is always assessed and recorded at birth, why?
|
1% to 5% of infants are born with a cord that contains only a single vein and artery
-From 15% to 20% of these infants are found to have accompanying chromosomal disorders or congenital anomalies, particularly of the kidney and heart |
|
|
percutaneous umbilical blood sampling [PUBS]
|
Blood can be withdrawn from the umbilical vein or transfused into the vein during intrauterine life for fetal assessment or treatment
|
|
|
can be determined by ultrasound examination during pregnancy?
|
adequacy of blood flow (blood velocity) through the cord
-both systolic and diastolic cord pressure, |
|
|
nuchal cord?
|
loose loop of cord is found around the fetal neck at birth
|
|
|
contributes to hemostasis and helps prevent hemorrhage of the newborn through the cord.
|
-constriction of the smooth muscle
(walls of the umbilical cord arteries are lined with smooth muscle) |
|
|
Name Germ Layer: Central nervous system (brain and spinal cord)
Peripheral nervous system Skin, hair, and nails Sebaceous glands Sense organs |
Ectoderm
|
|
|
Mesoderm
|
Supporting structures of the body (connective tissue, bones, cartilage, muscle, ligaments, and tendons)
-Dentin of teeth - Upper portion of the urinary system (kidneys and ureters) -Reproductive system -Heart, Circulatory system -Blood cells -Lymph vessels |
|
|
Lining of pericardial, pleura, and peritoneal cavities
-Lining of the gastrointestinal tract, respiratory tract, tonsils, parathyroid, thyroid, thymus glands - Lower urinary system (bladder and urethra) |
Entoderm
|
|
|
Why is it important to know which structure arise from each germ layer?
|
b/c co existing congenital defects found in newborns arise from the same layer
-will arise to the development of organs and systems |
|
|
What virus is capable of infecting all three germ layers, or causing congenital anomalies in a myriad of body systems.
|
Rubella
|
|
|
one of the first systems to become functional in intrauterine life
|
cardiovascular system
|
|
|
heartbeat may be heard with a Doppler instrument as early as?
|
10th to 12th week of pregnancy
|
|
|
The heart rate of a fetus is affected by?
|
oxygen level, activity, and circulating blood volume, just as in adult life
|
|
|
During what time is the growing structure most vulnerable to invasion by teratogens?
|
time of organogenesis: organ formation
(at 8 weeks' gestation (the end of the embryonic period) |
|
|
When does fetal blood begin to exchange nutrients with the maternal circulation across the chorionic villi?
|
As early as the third week of intrauterine life
|
|
|
Why does fetal circulation differs from extrauterine circulation ?
|
b/c the fetus derives O2 and excretes CO2 not from gas exchange in the lung but from gas exchange in the placenta.
|
|
|
Blood arriving at the fetus from the placenta is highly oxygenated. This blood enters the fetus through the ?
|
umbilical vein (called a vein even though it carries oxygenated blood, because the direction of the blood is toward the fetal heart).
|
|
|
Blood flows from the umbilical vein to the _____ ______, an accessory vessel that directs oxygenated blood directly to the fetal liver.
|
ductus venosus
|
|
|
opening in the atrial septum?
|
Foramen ovale (connects the RA & LA)
|
|
|
Ductus Arteriosus:
|
connects pulmonary artery & the aorta
|
|
|
Name The 3 Fetal shunts (will redirect the flow of blood)?
|
a. ductus venosus
b. foramen ovale c. ductus arteriosus |
|
|
What is the fetal heart rate during pregnancy?
|
120-160 beats per minute
|
|
|
The rapid fetal heart rate during pregnancy is necessary
why? |
necessary to supply oxygen to cells, because the red blood cells are never fully saturated
|
|
|
1.newborn's hgb level?
2.newborn's hct level? |
1. 17.1 g/100 mL
2. 53% |
|
|
The bulk of fetal hgb has matured to adult hgb composition, at what age?
|
6 mths ( when clinical sx of sickle cell anemia are apparent
|
|
|
produces Amniotic fluid?
|
Amniotic membrane
|
|
|
produces Amniotic fluid?
|
Amniotic membrane
|
|
|
What shunt connects the pulmonary artery and the aorta?
|
ductus arteriosus
|
|
|
Why are there 3 shunts?
|
1. lungs of baby are Not functioning inside the womb
2. blood has to circulate through the baby from head to toe |
|
|
B/c there is no need for the bulk of blood to pass through the lungs, it is shunted, as it enters the RA, into the LA through an opening in the atrial septum, called the ?.
|
foramen ovale
|
|
|
blood flow from the descending aorta is transported by the ______ _____ (called arteries, even though they are now transporting deoxygenated blood, because they are carrying blood away from the fetal heart) back through the umbilical cord to the placental villi, where new oxygen exchange takes place.
|
umbilical arteries
|
|
|
How to calculate EDB?
|
, count backward 3 calendar months from the 1st day of a woman's LMP and add 7 days.
|
|
|
EDB
|
a pregnancy ending 2 weeks before or 2 weeks after the calculated EDB is considered well within the normal limit (38-42 weeks)
|
|
|
What is measured w/ a Nonstress Test?
|
Response of fetal heart rate in relation to fetal movements
|
|
|
What is the Normal findings w/ Nonstress Test?
|
-Two or more accelerations of fetal heart rate of 15 beats/min lasting 15 sec or longer following fetal movements in a 20-min period
|
|
|
What is the safety consideration w/ Nonstress test?
|
Woman should not lie supine to prevent supine hypotension syndrome
|
|
|
What is measured w/ Contraction Stress Test?
|
Response of fetal heart rate in relation to uterine contractions produced by nipple stimulation
|
|
|
Normal Finding w/ Contraction stress test?
|
no late decelerations w/ contraction
|
|
|
Safety consideration w/ contraction test?
|
In addition to preventing supine hypotension syndrome, observe woman for 30 min afterward to see that contractions are quiet and preterm labor does not begin
|
|
|
What are the risk for Amniocentesis?
|
hemorrhage from penetration of the placenta, infection of the amniotic fluid, and puncture of the fetus. If it leads to irritation of the uterus, it can initiate premature labor
|
|
|
Preparation for Amniocentesis
|
-empty bladder
-sterile technique (aseptic) -schedule b/w 14 to 16 week |

