![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
63 Cards in this Set
- Front
- Back
|
Describe the physiology of cerebral blood flow
|
-Brain makes up only 2% of body weight
-Brain uses 15-20% of cardiac output -Brain consumes 15% of oxygen at rest -Anterior circulation receives 70%, posterior circulation receives 30% -Gray matter requires more oxygen/blood than the white matter |
|
|
What does blood flow depend on?
|
-Blood flow is a fraction of perfusion pressure
-Resistance of vascular bed can be modified by: -Arterial pressure -pCO2, pH, and oxygen -intracranial pressure -blood viscosity -neurotransmitters Blood flow is relatively constant and governed by autoregulatory mechanisms |
|
|
Over what range of blood pressures is cerebral blood flow fairly constant?
|
40mmHg - 150mmHg
|
|
|
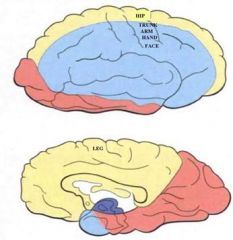
Yellow - Anterior cerebral artery
Blue - Middle cerebral artery Red - Posterior cerebral artery |
|
|
What supplies from to the striatum?
|
Lenticulostriate arteries from the MCA. The tip of the caudate is from the ACA.
|
|
|
What supplies the globus pallidus?
|
Ant. choroidal arteries from ICA
|
|
|
What supplies the thalamus and hippocampus?
|
PCA
|
|
|
Describe the epidemiology of stroke
|
-Almost 750,000 new or recurrent strokes per year in the US
-Third leading cause of death in US, second worldwide -Almost 4 million Americans are living with neurologic deficits due to stroke -Prevent is key -1-2% of ischemic stroke patients nationally are treated with Tissue Plasminogen Activator |
|
|
Define stroke
|
Rapidly developing clinical signs of focal (at times global) disturbance of cerebral function, lasting more than 24 hours or leading to death with no apparent cause other than that of vascular origin
|
|
|
Define transient ischemic attack
|
Similar to a stroke, but the symptoms resolve within 24 hours
|
|
|
What is important about TIAs
|
You have a 25% total risk for having a stroke in the next 90 days
|
|
|
What are the distribution of types of strokes in the US?
|
-Ischemic stroke (infarction): 85%
-Hemorrhagic stroke: 15% -Intracranial 67% -Subarachnoid hemorrhage 33% |
|
|
What was the number one cause of stroke in Japan?
|
Salt intake leads to hypertension which leads to hemorrhagic stroke
|
|
|
What are the non-modifiable risk factors for stroke?
|
-Age
-Gender -Ethnicity -Hereditary |
|
|
What are the modifiable risk factors for stroke?
|
-Hypertension
-Diabetes -Cardiac disease (atrial fibrillation) -Hypercholesterolemia -Cigarette smoking -Alcohol abuse -Physical inactivity |
|
|
What occurs when the proximal portion of the MCA is blocked
|
There will be extensive necrosis and infarction, likely sparing the globus pallidus
|
|
|
What sequence of events occurs in the first day after cerebral infaction?
|
>1 hour: -Microvacuoles form within neurons (swollen mitochondria)
-Perineuronal vacuolation (swollen astrocyte processes) These are intracellular/intrastructural changes that can not be seen with light microscopy 4-12 hours: -Neuronal cytoplasmic eosinophilia (pink neurons) -Disappearance of Nissl bodies -Pyknotic nuclei -Leakage of BBB Brain runs out of oxygen and the ATP levels drop. Intracellular pH drops and the lysosomal enzymes are released and disturb proteins essential for cell survival 15-24 hours: Neurophil infiltration begins |
|
|
What sequence of events occurs after the first day after cerebral infarction?
|
2-3 days: Macrophages (foam cells) appear. They clean up dead tissue
~5 days:Neurophilic infiltration ceases ~1 week: Proliferation of astrocytes around core infarct |
|
|
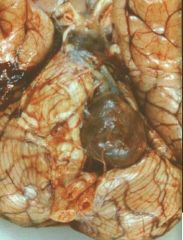
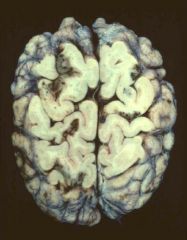
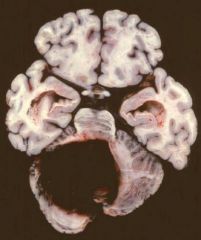
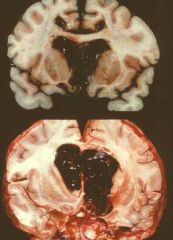
This is MCA territory ischemic infarction. The tissue is dead and discolorized. The consequence of this huge MCA territory is edema and you get midline shift with cingulate herniation and uncal herniation. There is also a duret hemorrhage.
|
|

|
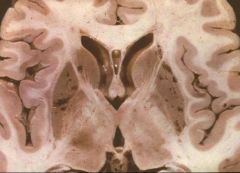
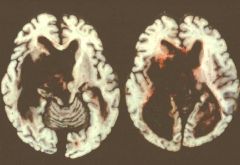
MCA infarction. Once the tissue is cleaned up you are left with a huge cavitation filed with glial mesencymal scars
|
|

|
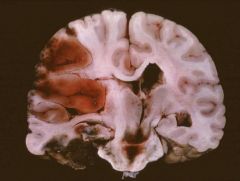
MCA infarction. This is what you see if you cut the brain coronally. The tissue defect is very significant.
|
|

|
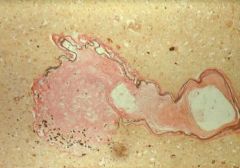
Atherosclerosis
In the basillar artery and MCA you can see lots of plaques. |
|
|
Atherosclerosis
An occluded vessel |
|
|
Atherosclerosis
There is a thickened intima that is blended into an atherloma composed of cholesterol and cholesterol esters as indicated by the needle shaped clefts. |
|

|
Athlerosclerotic vessels can be dilated, stiff, and tortuous. The surface of athleroma is rough and is very thrombogenic. It is not uncommon to see thrombosis built up on top of an artheroma. The lumen of the internal carotid is almost completely occluded.
|
|
|
Focal dilation of an atherosclerotic vessel called a fusiform aneurysm
The aneurysm that is a secondary dilatation of vascular lumen associated with atherleosclerosis is fusiform. |
|

|
Atherosclerosis
The lumen of the vessel is filled with thrombi and the medulla is squeeze to the other side. There is secondary hemorrhage |
|
|
Smaller meningeal vessels will show plaques when the atherosclerosis is very severe
|
|
|
What is arteriolar sclerosis associated with?
|
-Aging
-Sustained systemic hypertension -Diabetes mellitus |
|
|
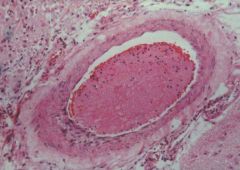
This is an extreme example of arteriolar sclerosis. The lumen is now tiny surrounded by brain parenchema. Sustained systemic hypertension or diabetes damaged the endothelial or smooth muscle cells. Plasma protein over time leaked out through the damaged vascular wall accelerating further the degeneration of smooth muscle cells or endothelial cells and you end up with all of this homogeneous eosinophilic called hyalinization or fibrinoid necrosis of the vascular wall. The parenchyma surrounding the vessel is gliotic meaning it is suffering from chronic ischemia.
|
|
|
Arteriole sclerosis
This shows better the internal elastic lamina. This is the lumen. Here the sclerotic change made a microaneurysm. The important matter is that this part of the vessel doesn’t have elastic lamina and is prone to further hemorrhage. |
|
|
Arteriolar sclerosis
This is the damaged wall. The black dots are evidence of hemorrhage or leakage of blood. |
|
|
-Holes involving the striatum are small infactions caused by blockage of lenticulostriate arteries
|
|
|
What are lacune?
|
-Lacune are small infarcts less than 1.5cm in the greatest dimension
-They can be solitary or confluent -Once confluence and involving extensive areas of the brain patients may present with dementia as opposed to focal neurological deficits |
|
|
What are the causes of cerebral embolism?
|
Large or small emboli:
-Atrial fibrilation -Myocardial infarction -Bacterial endocarditis -Rheymatic endocarditis -Nonbacterial endocarditis -Cardiac surgery -Arterial thrombosis Small emboli -Ulcerated atheroma -Trauma (fat emboli) |
|
|
This is a cardiac thrombi sent as emboli in the brain. The surrounding tissue is full of macrophages cleaning up dead tissue.
|
|
|
This is a fractured atheroma. We can tell it is because there are lots of cholesterol clefts.
The surrounding tissue is infarcted and filled with macrophages to clean up the dead tissue. |
|
|
The emboli can be multiple. Once emboli become very confluent the status can be called embolitic shower. Emboli tend to happen between the cortex and white matter where the diameter becomes drastically narrower. Embolitic events tend to involve white matter-gray matter junction.
|
|

|
Air embolism
These are bubbles in the vessels. Bad surgery can cause this as can going up in altitude too quickly. |
|
|
What primary cranial and./or cerebral inflammations are non-infectious vasculitdes?
|
-Takayasu's arteritis
-Griant cell or termporal arteritis -Primary angiitis of the CNS (granulomatous angiitis) |
|
|
What manifestations of systemic disease cause non-infectioyus vasculitides?
|
-Systemic lupus erythematosus
-Polyarteritis nodosa -Wegener's granulomatosis -Churg-Strauss syndrome -Behcet's syndrome -Malignancy related |
|
|
Describe drug induced vasculitis
|
There is drug induced vasculitis by both ilicit and non-ilicit drugs. Heroine and cocaine can cause vasculitis. Interferon can also cause vascultis as well.
|
|
|
What are the major causes of non-traumatic intracerebral hemorrhage?
|
-Hypertension 50%
-Cerebral amyloid angiopathy 12% -Anticoagulants 10% -Tumors 8% -Illicit and licit drugs 6% - |
|
|
What are the frequent sites of involvement for hypertensive hemorrhage?
|
1. Cerebral white matter
2. Basal ganglia/putamen/globus pallidus 3. Brain stem and cerebellar white matter |
|

|
This is a huge hemotoma associated with hypertensive hemorrhage involving whit e matter. Parts of the basal ganglia is involved. Part of the basal ganglia is involved and part of the intracorte x is necrotic.
|
|

|
This is the cavitary lesion that forms after a hemorrhage heals
|
|
|
This is massively involving cerebral white matter. Hematoma burst into the ventricular system. Once hemorrhage involves the ventricular system the patient is not likely to survive more than several hours.
|
|
|
This is a hemotaoma in the middle of the pons.
|
|
|
This is a hemotaoma in the middle of the pons.
|
|
|
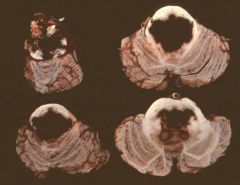
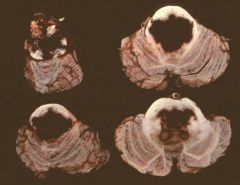
Cerebellar white mater hemorrhage
|
|
|
Describe subarachnoidal hemorrhages
|
-Also called saccral aneurysm
-Approx. 5% of all strokes -10-11/100,000 annual incidence -Non-traumatic conditions -Rupture of aneurysm (berry) 80% -Arteriovenous malformations 5-10% -Unidentified cause 10-15% |
|
|
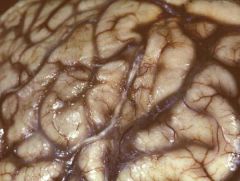
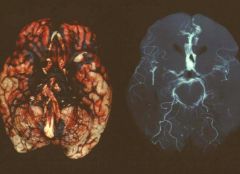
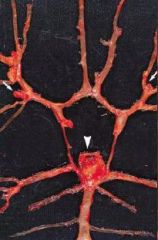
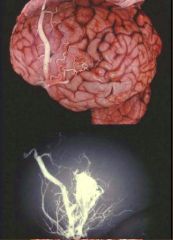
This is the result of a rupture of a berry aneurysm. The branching portion of the ACA. This is the result of rupture of this berry aneuysm,
|
|
|
Describe saccular (berry) aneurysms
|
Frequency at autopsy: 1-6%
Age at autopsy: 30-70yo Sex ratio: F:M=3:2 Associated hypertension: 50% Familial: Rare Location: Ant. circ >80%, Post circ <20% Multiple: 20% Ruptured aneurysm: Size>0.5cm Mortality: 60% . Patients surviving a rupture of their first aneurysm are predispossed to more aneuysms. There is a severe complication of aneurysms called vasospasm. This involves the parental artery of the aneurysm. This vasospam can aggrevate the brain much further. |
|
|
Where do aneurysms tend to form?
|
Branching sites of arteries in the anterior circulation
|
|
|
Aneurysm at the top of the basillar artery
|
|

|
Aneursym
|
|
|
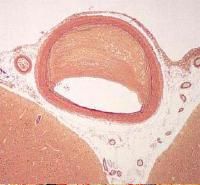
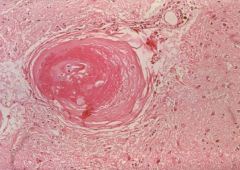
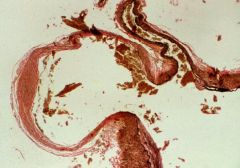
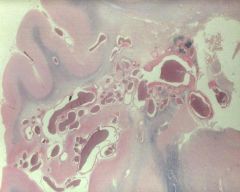
This is a histological prep of an aneurysm. This aneurysm has a thin collagenous wall only and it can be easily ruptured.
|
|
|
Aneurysm rupture can cause subarachnoidal hemorrhage. Sometimes if the pressure of blood shoots up into the brain parenchyma you make see intraparenchyma hemorrhage.
|
|
|
What can arteriovenous malformations cause?
|
This can cause intraparenchymal hemorrhage or subarachnoid hemorrhage
|
|
|
Describe arteriovenous malformations
|
Clincal onset: 10-40yo
Sex ratio: M:F=2:1 Location: Usually supratentorial Clinical presentation: Headache, seizures, focal neurologic deficit, hemorrhage Angiography: Evidence of arterivenous shunt and abnormal blood vessels Mortality after hemorrhage: 20% |
|
|
Arteriovenous malformation
This shows 100s-1000s of vascular channels |
|

|
This is the coronal slice of the arteriovenous malformation. This lesion spans from the ventricular surface to the meningeal surface. There are numerous vessels.
|
|
|
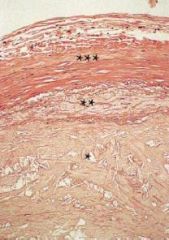
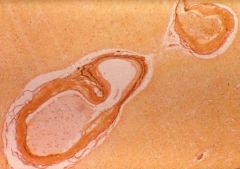
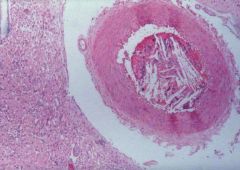
Histological presentation of an arteriovenous malformation. Some vascular channel walls are very thrick. In arterole venous malformation, unlike normal circulation, the blood tends to shut from A to V side. The vascular channel receiving high pressue blood tend to defend themselves by thickening their wall. You can see an irregularly thickened vascular wall in AVM.
|

