![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
21 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
1. Where is the primary cortex, somatosensory cortex, supplementary motor area and premotor cortex located.
|

The primary motor cortex (Brodmann’s area 4) is in the precentral gyrus, while the primary somatosensory cortex (Brodmann’s areas 3, 1, and 2) is in the postcentral gyrus (see
Lesions in these areas cause motor or sensory deficits, respectively, in the contralateral body. Several important areas of motor association cortex, including the supplementary motor area and premotor cortex, lie just anterior to the primary motor cortex. These regions are involved in higher-order motor planning and project to the primary motor cortex. Similarly, somatosensory association cortex in the parietal lobe receives inputs from primary somatosensory cortex and is important in higher-order sensory processing. Unlike lesions in the primary cortices, lesions in sensory or motor association cortex do not produce severe deficits in basic movement or sensation. Instead, lesions of the association cortex cause deficits in higher-order sensory analysis or motor planning, discussed later. |
|
|
|
What is the dorsal (posterior) horn responsible for?
what is the Intermediate zone responsible for? What is the ventral (anterior) horn responsible for? |

The central gray matter has a dorsal (posterior) horn that is involved mainly in sensory processing, an intermediate zone that contains interneurons and certain specialized nuclei (Table 6.2), and a ventral (anterior) horn that contains motor neurons. Motor neurons send their axons out of the spinal cord via the ventral nerve root filaments.
|
|
|
|
Explain how the spinal cord changes as you descend it.
In what two areas does it have enlargements? |

The spinal cord does not appear the same at all levels.
The white matter is thickest in the cervical levels, where most ascending fibers have already entered the cord and most descending fibers have not yet terminated on their targets, while the sacral cord is mostly gray matter. In addition, the spinal cord has two enlargements. The cervical enlargement and the lumbosacral enlargement give rise to the nerve plexuses for the arms and legs. The spinal cord has more gray matter at the cervical and lumbosacral levels than at the thoracic levels, particularly in the ventral horns, where lower motor neurons for the arms and legs reside. In the thoracic cord, a lateral horn is present that contains the intermediolateral cell column. |
|
|
|
Describe the spinal cord blood supply.
Where do most of the arteries terminate? What are the names of the arteries that reach the spinal cord. What is Great Radicular artery of Adamkiewicz located? |
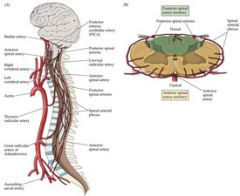
The blood supply to the spinal cord arises from branches of the vertebral arteries and spinal radicular arteries.
The vertebral arteries give rise to the anterior spinal artery that runs along the ventral surface of the spinal cord. In addition, two posterior spinal arteries arise from the vertebral or posterior inferior cerebellar arteries and supply the dorsal surface of the cord. The anterior and posterior spinal arteries are variable in prominence at different spinal levels and form a spinal arterial plexus that surrounds the spinal cord. Thirty-one segmental arterial branches enter the spinal canal along its length; most of the branches arise from the aorta and supply the meninges. Only six to ten of these reach the spinal cord as radicular arteries, arising at variable levels. There is usually a prominent radicular artery arising from the left side, anywhere from T5 to L3, but usually between T9 and T12. This is called the great radicular artery of Adamkiewicz, and it provides the major blood supply to the lumbar and sacral cord. |
|
|
|
What part of the spinal cord is the vulnerable zone in regards to blood supply?
When is this area at risk for ischemia? What is Batson's plexus? How is the structure of these veins different from other veins? As result of this change, what can spread more easily? |
The mid-thoracic region, at approximately T4 to T8, lies between the lumbar and vertebral arterial supplies and is a vulnerable zone of relatively decreased perfusion. This region is most susceptible to infarction during thoracic surgery or other conditions causing decreased aortic pressure. The anterior spinal artery supplies approximately the anterior two-thirds of the cord, including the anterior horns and anterior and lateral white matter columns.
The posterior spinal arteries supply the posterior columns and part of the posterior horns. Venous return from the spinal cord occurs initially via drainage into a plexus of veins located in the epidural space before reaching systemic circulation. These epidural veins, called Batson’s plexus do not contain valves, so elevated intra-abdominal pressure can cause reflux of blood carrying metastatic cells (such as prostate cancer) or pelvic infections into the epidural space. |
|
|
|
Explain the general organization of the motor systems in brain and spinal cord.
|
|
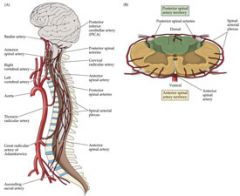
Only the most important loops are depicted, and sensory inputs have been omitted.
Recall that the cerebellum and basal ganglia participate in important feedback loops, in which they project back to the cerebral cortex via the thalamus, and do not themselves project to lower motor neurons. We will discuss the roles of the cerebellum and basal ganglia in motor control further in Chapter 15 and Chapter 16. Within the cerebral cortex itself, there are numerous important circuits for motor control. For example, circuits involving association cortex regions such as the supplementary motor area, premotor cortex, and parietal association cortex are crucial to the planning and formulation of motor activities. As we will discuss in Chapter 19, lesions of these regions of association cortex can lead to apraxia, a condition characterized by a deficit in higher-order motor planning and execution despite normal strength (neuroexam.com Video 15). Although not shown, sensory inputs clearly also play an essential role in motor control and participate in motor circuits and feedback loops that range from the level of the spinal cord to the cerebral cortex. |
|
|
Describe the two lateral motor systems?
Which parts does each pathway control? Where do the pathways cross over? |
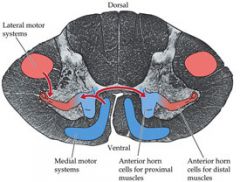
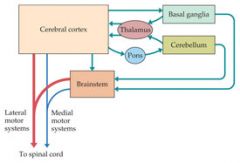
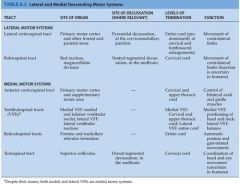
The two lateral motor systems are the lateral corticospinal tract and the rubrospinal tract.
These pathways control the movement of the extremities. The lateral corticospinal tract in particular is essential for rapid, dextrous movements at individual digits or joints. Both of these pathways cross over from their site of origin and descend in the contralateral lateral spinal cord to control the contralateral extremities. |
|
|
|
What are the four medial motor systems?
What do these pathways control? Where do each of them cross over? Will you see defects where there is a lesion of an unilateral medial motor system? Why or why not? |
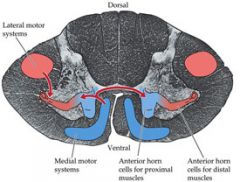
The four medial motor systems are the anterior corticospinal tract.
The vestibulospinal tracts, the reticulospinal tracts, and the tectospinal tract. These pathways control the proximal axial and girdle muscles involved in postural tone, balance, orienting movements of the head and neck, and automatic gait-related movements. The medial motor systems descend ipsilaterally or bilaterally. Some extend only to the upper few cervical segments. The medial motor systems tend to terminate on interneurons that project to both sides of the spinal cord, controlling movements that involve multiple bilateral spinal segments. Thus, unilateral lesions of the medial motor systems produce no obvious deficits. In contrast, lesions of the lateral corticospinal tract produce dramatic deficits. The rubrospinal tract in humans is small, and its clinical importance is uncertain, but it may participate in taking over functions after corticospinal injury. It may also play a role in flexor (decorticate) posturing of the upper extremities, which is typically seen with lesions above the level of the red nuclei, in which the rubrospinal tract is spared. |
|
|
|
|
|
|
|
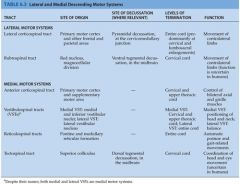
Name the two Lateral motor systems.
1. What is the site of origin of each one? 2. What is the site of decussation of each one? 3. Where do the each of the lateral motor systems terminate? 4. What movement does each of the lateral motor systems control? |
|
|
|
|
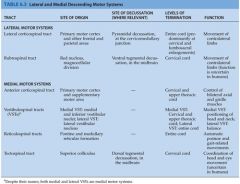
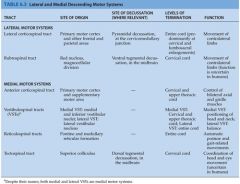
Name site of origina, site of decussation, level of termination, and function for each medial motor system.
1. Anterior Corticospinal Tract 2. Vestibulospinal Tract 3. Recticulospinal Tract 4. Tectospinal tract |
|
|
|
|
Which motor pathway is considered clinically the most important? Why?
Understand the course of the Lateral Corticospinal Tract. 1. Where do half of fibers originate from in the brain? Where do the other half originate from? 2. From what Cortical layer are the primary motor cortex coming from? Where do these neurons synapse? 3. What are Betz cells? What is the primary characteristic of these cells? 4. What area do these neurons enter first and where do they descend down to? |

The corticospinal tract—more specifically, the lateral corticospinal tract—is the most clinically important descending motor pathway in the nervous system.
This pathway controls movement of the extremities, and lesions along its course produce characteristic deficits that often enable precise clinical localization. Over half of the corticospinal tract fibers originate in the primary motor cortex (Brodmann’s area 4) of the precentral gyrus. The remainder arise from the premotor and supplementary motor areas (area 6) or from the parietal lobe (areas 3, 1, 2, 5, and 7). The primary motor cortex neurons contributing to the corticospinal tract are located mostly in cortical layer 5. Layer 5 pyramidal cell projections synapse directly onto motor neurons in the ventral horn of the spinal cord as well as onto spinal interneurons. About 3% of corticospinal neurons are giant pyramidal cells called Betz cells, which are the largest neurons in the human nervous system. Axons from the cerebral cortex enter the upper portions of the cerebral white matter, or corona radiata and descend toward the internal capsule. |
|
|
|
What does the cerebral white matter do?
How does internal capsule change as it descends? |
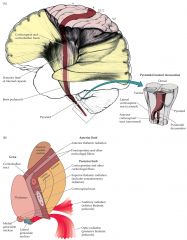
Axons from the cerebral cortex enter the upper portions of the cerebral white matter, or corona radiata, and descend toward the internal capsule.
In addition to the corticospinal tract, the cerebral white matter conveys bidirectional information between different cortical areas, and between cortex and deep structures such as the basal ganglia, thalamus, and brainstem. These white matter pathways form a fanlike structure as they enter the internal capsule, which condenses down to fewer and fewer fibers as connections to different subcortical structures are made. |
|
|
|
1. What are the 3 parts to the internal capsule?
2. How are the Thalamus and Caudate nucleus arranged in regards to the internal capsule. 3. What separates head of caudate from the globus pallidus and putamen. 4. What is genu? 5. In which part does the Corticospinal Tract lie? 6. To what part of the midbrain does the internal capsule continue until? 7. In what portion of the cerebral pundcles is the white matter located in? 8. What is contained in the middle one-third of the basis peduncil? |

The internal capsule is best appreciated in horizontal brain sections, in which the right and left internal capsules look like arrowheads or two letter Vs, with their points facing inward.
Note that the thalamus and caudate nucleus are always medial to the internal capsule, while the globus pallidus and putamen are always lateral to the internal capsule. There are three parts to the internal capsule: anterior limb, posterior limb, and genu. Note that the anterior limb of the internal capsule separates the head of the caudate from the globus pallidus and putamen, while the posterior limb separates the thalamus from the globus pallidus and putamen. The genu (“knee” in Latin) is at the transition between the anterior and posterior limbs, at the level of the foramen of Monro. The corticospinal tract lies in the posterior limb of the internal capsule. The somatotopic map is preserved in the internal capsule, so motor fibers for the face are most anterior, and those for the arm and leg are progressively more posterior. Fibers projecting from the cortex to the brainstem, including motor fibers for the face, are called corticobulbar instead of corticospinal because they project from the cortex to the brainstem, or “bulb.” Despite the somatotopic arrangement, the fibers of the internal capsule are compact enough that lesions at this level often produce weakness of the entire contralateral body (face, arm, and leg). However, occasionally capsular lesions can also produce more selective motor deficits. Additional details of the fibers carried by the internal capsule other than the corticobulbar and corticospinal tracts. The internal capsule continues into the midbrain cerebral peduncles, meaning, literally, “feet of the brain”. The white matter is located in the ventral portion of the cerebral peduncles and is called the basis pedunculi. The middle one-third of the basis pedunculi contains corticobulbar and corticospinal fibers with the face, arm, and leg axons arranged from medial to lateral, respectively. The other portions of the basis pedunculi contain primarily corticopontine fibers. |
|
|
|
1. Where do Corticospinal fibers go to after leaving the cerebral peduncles?
2. What are the medullary pyramids? 3. What do 85% of the fibers do in the pyramidal decussation? 4. Where do the fibers go after the medulla? 5. Where do the remaining 15% of fibers cross? |

The corticospinal tract fibers next descend through the ventral pons, where they form somewhat scattered fascicle.
These collect on the ventral surface of the medulla to form the medullary pyramids. For this reason the corticospinal tract is sometimes referred to as the pyramidal tract (this terminology, though widely used, is somewhat imprecise since the pyramids include reticulospinal and other brainstem pathways in addition to the corticospinal tract). The transition from medulla to spinal cord is called the cervicomedullary junction, which occurs at the level of the foramen magnum. At this point about 85% of the pyramidal tract fibers cross over in the pyramidal decussation to enter the lateral white matter columns of the spinal cord, forming the lateral corticospinal tract. A somatotopic representation is present in the lateral corticospinal tract, with fibers that control the upper extremity located medial to those that control the lower extremity. Finally, the axons of the lateral corticospinal tract enter the spinal cord central gray matter to synapse onto anterior horn cells. The remaining ~15% of corticospinal fibers continue into the spinal cord ipsilaterally, without crossing, and enter the anterior white matter columns to form the anterior corticospinal tract. |
|
|
|
What are two divisions of the ANS?
Where are the preganglionic neurons of the Sympathetics located at? Name the ganglion that supply the head and neck. |
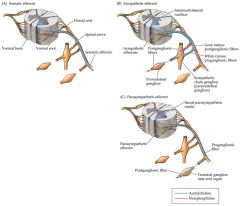
The autonomic nervous system has two main divisions. The sympathetic, or thoracolumbar, division arises from T1 to L2, or T1 to L3, spinal levels and is involved mainly in such “fight-or-flight” functions as increasing heart rate and blood pressure, bronchodilation, and increasing pupil size. The parasympathetic, or craniosacral, division, in contrast, arises from cranial nerve nuclei and from S2 through S4 and is involved in “rest and digest” functions, such as increasing gastric secretions and peristalsis, slowing the heart rate, and decreasing pupil size. The enteric nervous system, considered a third autonomic division, consists of a neural plexus, lying within the walls of the gut, which is involved in controlling peristalsis and
gastrointestinal secretions. Preganglionic neurons of the sympathetic division are located in the intermediolateral cell column in lamina VII of spinal cord levels T1 to L2 or T1 to L3. There are two sets of sympathetic ganglia. The paired paravertebral ganglia form a chain called the sympathetic trunk (or sympathetic chain) running all the way from cervical to sacral levels on each side of the spinal cord. The sympathetic trunk allows sympathetic efferents, which exit only at thoracolumbar levels, to reach other parts of the body as well. For example, sympathetics are provided to the head and neck by the upper thoracic spinal cord (T1–T3) intermediolateral cell column via three sympathetic chain ganglia named the superior, middle (often absent), and inferior (stellate) cervical ganglia. The other sympathetic ganglia are unpaired prevertebral ganglia, located in the celiac plexus surrounding the aorta and include the celiac ganglion, superior mesenteric ganglion, and inferior mesenteric ganglion. |
|
|
|
1. Typically which axons are longer in Symapthetic; the pre or post ganglioinic?
2. Describe the Parasympatetics. Which axons are longer? 3. What are the neurotransmitters used by each division of the ANS? |

Axons of preganglionic sympathetic neurons thus have a fairly short distance to travel, while axons of postganglionic neurons travel a long distance to reach effector organs.
In contrast, parasympathetic preganglionic fibers must travel a long distance to reach the terminal ganglia located within or near the effector organs. Parasympathetic preganglionic fibers arise from cranial nerve parasympathetic nucleiand from the sacral parasympathetic nuclei located in the lateral gray matter of S2, S3, and S4, in a location similar to that of the intermediolateral cell column. The sympathetic and parasympathetic systems also differ in terms of their neurotransmitters. Sympathetic postganglionic neurons release predominantly norepinephrine onto end organs. Parasympathetic postganglionic neurons release predominantly acetylcholine, activating muscarinic cholinergic receptors on end organs. Preganglionic neurons in both sympathetic and parasympathetic ganglia release acetylcholine, activating nicotinic cholinergic receptors. Noradrenergic (a1, a2, b1, b2, b3) and muscarinic cholinergic (M1, M2, M3) receptor subtypes mediate different actions of these transmitters on end organs (see the References section at the end of this chapter). In addition, various peptides and other substances (such as ATP and adenosine) are released at autonomic synapses. One notable exception to the norepinephrine/sympathetic, acetylcholine/parasympathetic rule for postganglionic neurotransmitters is the sweat glands, which are innervated by sympathetic postganglionic neurons that release acetylcholine. |
|
|
|
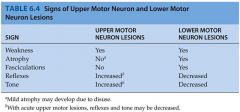
1. What are differences between upper motor neurons and lower motor neurons in regards to deficits?
|

The concept of upper motor neuron versus lower motor neuron lesions is very useful in clinical localization.
Upper motor neurons of the corticospinal tract project from the cerebral cortex to lower motor neurons located in the anterior horn of the spinal cord. Lower motor neurons, in turn, project via peripheral nerves to skeletal muscle. An identical concept of upper and lower motor neurons applies to the corticobulbar tract and cranial nerve motor nuclei. Signs of lower motor neuron lesions include muscle weakness, atrophy, fasciculations, decreased tone, and hyporeflexia. Fasciculations are abnormal muscle twitches caused by spontaneous activity in groups of muscle cells. An example of a benign fasciculation not associated with motor neuron damage is the eyelid twitching often experienced during periods of fatigue, caffeine excess, and eye strain (such as while reading too much neuroanatomy in one night). Signs of upper motor neuron lesions include muscle weakness and a combination of increased tone and hyperreflexia sometimes referred to as spasticity. Additional abnormal reflexes seen with upper motor neuron lesions, such as Babinski’s sign, Hoffmann’s sign, posturing. Note that with acute upper motor neuron lesions, flaccid paralysis with decreased tone and decreased reflexes may initially occur and gradually, over hours or even months, develop into spastic paresis. Spinal shock is an example of this process. |
|
|
|
Explain whether each sign will be present in an UMN or LMN or lesions.
1. Weakness 2. Atrophy 3. Fasciculations 4. Reflexes 5. Tone |
|
|
|
|
Under the commonly used terms to describe weakness.
|

|
|
|
|
Unilateral Face, Arm, and Leg Weakness or Paralysis.
a. Which areas can be ruled out. b. Which areas may have the lesion. c. Which side of the body will be affected? Contralateral or Ipsalateral d. Common causes of the lesion e. Associated Features |

LOCATIONS RULED OUT: Unlikely to be cortical because the lesion would have to involve the entire motor strip, in which case sensory involvement is hard to avoid. Unlikely to be muscle or peripheral nerve because in that case coincidental involvement of the face, arm and leg, all on one side of the body, would be required. Not the spinal cord or medulla because in that case the face would be spared.
LOCATIONS RULED IN: Corticospinal and corticobulbar tract fibers below the cortex and above the medulla: corona radiate, posterior limb of the internal capsule, basis pontis, or middle third of the cerebral peduncle. SIDE OF LESION: Contralateral to weakness (above the pyramidal decussation). COMMON CAUSES: Lacunar infarct of the internal capsule (lenticulostriate branches of the middle cerebral artery or anterior choroidal artery; or of the pons (median perforating branches of the basilar artery). Infarct of the cerebral peduncle is less common. Demyelination, tumor, or abscess in these locations or in the corona radiata can also cause pure motor hemiparesis. ASSOCIATED FEATURES: Upper motor neuron signs are usually present. Dysarthria is common, giving rise to the name dysarthria–pure motor hemiparesis. Ataxia of the affected side may also occasionally be seen because of involvement of the cerebellar pathways (corticopontine fibers), giving rise to the name ataxia-hemiparesis. |
|

