![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
18 Cards in this Set
- Front
- Back
|
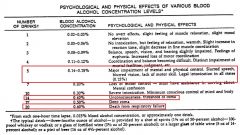
Given the blood levels of ethanol of .15%, .4%, and .6%, describe the manifestations of intoxication
|
|
|
|
Describe the mechanisms by which ethanol produces its effects. (sedative/ataxia/blackout)
|
An action on the GABA receptor – increases GABA – mediated inhibition. This action may mediate sedative and ataxia effects.
May also inhibit NMDA receptors causing blackouts |
|
|
Describe the primary effects of ethanol on CNS
how do you get hypothermia ? |
Alcohol causes a dose-related depression of all areas of the CNS. Depression of hypothalamus results in hypothermia
Acute intoxication can be lethal due to depression of medullary respiratory and CV centers Stimulation observed after one or two drinks is a result of depression of inhibitory control mechanism of the reticular activating system. Chronic use can lead to irreversible neurological damage. |
|
|
Describe the primary effects of ethanol on respiratory and CV system
|
Respiratory system:
At about 0.40% - depression of respiratory center results in death Cardiovascular system: Moderate amount – peripheral vasodilation causing slight ↓ BP and heat loss. Regular moderate consumption decreases risk of heart disease (↑ HDL, ↓ platelet aggregation). High dose – myocardial depression Chronic change – alcoholic cardiomyopathy |
|
|
Describe the primary effects of ethanol on the GI (stomach, intestine, and pancreas)
|
Stomach – at low doses, alcohol stimulates salivary and gastric acid secretion. High concentrations of alcohol (>20%) may inhibit gastric acid secretion and peptic activity.
Intestine – chronic ingestion will lead to ↓ absorption of folic acid, thiamine, niacin, other vitamins, constipation, or diarrhea. Pancreas – chronic ingestion may lead to pancreatitis |
|
|
Describe the primary effects of ethanol on the liver
|
Chronic ingestion → induction of hepatic microsomal enzyme system and other enzyme systems.
Chronic excessive use fatty → infiltration, hepatitis, and hepatic cirrhosis. Biochemical changes |
|
|
what important endocrine effect does ethanol have?
** |
decreases ADH release
|
|
|
leading cause of teratogenesis
|
booze
|
|
|
Describe the metabolism and elimination kinetics of ethanol
what enzyme does this? |
90-98% of ethanol ingested is completely oxidized in the body. The rest is excreted via the urine and expired air.
At BAC > 0.01% the metabolism of ethanol follows zero-order kinetics alcohol dehydrogenase |
|
|
how does drinking cause hypoglycemia
|
NAD is used to metabolize etoh and you dont have any left for gluconeogenesis
|
|
|
Wernicke-Korsakoff Syndrome
|
memory loss and psychosis due to vitamin loss and booze
|
|
|
moa of Disulfuram? use?
|
Inhibition of aldehyde dehydrogenase leads to increase blood levels of acetaldehyde following ingestion of alcohol
causes a person to get really sick and deter them from drinking can also be used against cocaine |
|
|
Naltrexone, an opiod antagonist has what other use?
|
Opioid antagonist which blocks the rewarding effects of alcohol. Limitation is possibility of liver damage at high dose
|
|
|
what kind of drug is acamprostate?
|
An anti-craving drug approved by FDA August, 2004. Used to maintain abstinence in former drinkers.
|
|
|
Describe the potential drug interactions between ethanol and CNS depressants, oral hypoglycemics, anticoagulants, salicylates, acetaminophen, anticonvulsants, and antimicrobial agents
|
CNS depressants: potentiate effect
hypoglycemia: Alcohol causes potentiation of hypoglycemic effect. May also see disulfiram-like effect, particularly with chlorpropamide and tolbutamide anticoagulants: Half-life of warfarin decreased by chronic use of alcohol; however, anticoagulant effect may be enhanced in the presence of liver disease. Occasional moderate doses of ethanol unlikely to interfere with warfarin therapy in patients with normal liver function salicylates: Increase risk of gastric hemorrhage (aspirin) acetaminophen: potentiate breakdown to toxic metabolite-->liver damage anticonvulsants: Half-life decreased with chronic ingestion of large doses of alcohol due to induction of microsomal enzymes. Alcohol withdrawal associates with seizures antimicrobial agents: disulfram like rxns |
|
|
2 metabolites of methanol? things they cause
|
formic acid (metabolic acidosis-death)
formaldehyde (damage retinal cells-->blindness) |
|
|
tx for methanol?
|
Hemodialysis, support respiration
NaHCO3 administration to correct for metabolic acidosis Delay methanol metabolism with ethanol or Fomepizol (Antizol) - an inhibitor of alcohol dehydrogenase which decreases metabolism of methanol to toxic metabolites |
|
|
Oxidation to glycoaldehyde and oxalate may cause serious metabolic acidosis (anion gap) and renal damage (oxalate crystals)....
|
Ethylene Glycol
Solvent, antifreeze. Sweet taste attracts children and animals |

