![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
21 Cards in this Set
- Front
- Back
|
What role does the cranium play in bacterial or viral encephalitis or meningitis?
|
Inflammation causes increased pressure and the cranium is very unforgiving --->herniation and death
|
|
|
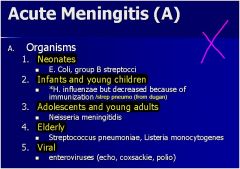
A young Marine recruit comes in from bootcamp complaining of a stiff neck, and headache. He has a fever and seems a little out of it.
You take a CSF sample from the lumbar cistern and feel a markedly increased pressure **. The CSF is markedly cloudy. When the labs come back , the patient has elevated PMNs, Glucose is <45 (↓), and proteins are >50 (↑). What are you dealing with? |
These labs indicate Bacterial Meningitis.
N. meningitidis is the likely culprit for his age group. |
|
|
have a look... just in case...
|
|
|
|
A 9 year old girl who recently started the 3rd grade presents complaining of a "heavy head", slight fever, and mild headache.
You perform a lumbar puncture and notice her pressure is slightly elevated. Labs show mostly lymphocytes*, normal glucose, and elevated proteins (>50). What are you thinking? |
Viral Meningitis
Normally self Limiting... |
|
|
You are seeing an AIDs patient who has been spending a month at home sick . He hasn't had too many visitors and spent a lot of time with his cat.
He is complaining of a constant headache that hasn't gone away for 3 weeks. He seems groggy and out of it. An MRI shows a ring-enhancing lesion on his brain. Biopsy reveals the lesion to be an abscess with necrosis and chronic inflammation. |
***Toxoplasmosis**
(seen in 30% of AIDs Patients) |
|
|
Fungal Meningitis is most common in _____ patients..
|
Immunocompromised
seen late in (elderly, AIDs, DM, Chronic Dz) |
|
|
Most common causes of Fungal Meningioencephalitis?
|
– Candida, Aspergillus, Mucor,
Criptococcus **Vasculitis = Aspergillus, Mucor **Parenchymal = Candida, Criptococcus |
|
|
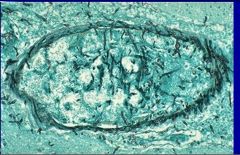
You are looking at a brain vessel biopsy of an AIDs patient and see branching hyphae invading a cerebral vessel.
|
**Aspergillus**
Aspergillus likes to invade vessels and produce hemorrhage and thrombosis. |
|
|
Aspergillus hyphae invading a cerebral vessel
|
|
|
Important and fatal sequela of suppurative CNS infection?
|
Increased intracranial pressure and progressive herniation can be fatal ---> Duret Hemorrhages
(Herniation of Cerebellar Tonsils through Foramen Magnum) |
|
|
You are looking at a post-mortum brain of a patient who died of an untreated bacterial encephalitis. You notice the cerebral ventricals are dilated and huge.
What is this? |
**Hydrocephalus**
CSF becomes too thick to reabsorb and obstructs ventricles ↓ ↑↑↑ Intracranial Pressure |
|
|
This is often present with seizure disorder, intracerebral or subarachnoid hemorrhage.
Most common site is middle cerebral artery (posterior branches) |
Arteriovenous Malformations
|
|
|
Micro for arteriovenous malformation?
|
tangled mesh of vascular channels
|
|
|
Most common cause of subarachnoid hemorrhage?
|
Most common cause is rupture of saccular (berry) aneurysm
|
|
|
What is the most common cause of intracranial aneurysm?
|
saccular (berry) aneurysm
|
|
|
- Rupture seen in 30's and 40’s; slightly more often in ladies
- 10 mm or greater have 50% risk of bleeding and this is increased with increase in intracranial pressure - Presents typically as “the worst headache I’ve ever had” **** - 25-50% die with first rupture; rebleeding is common -CSF is bloody**** |
Subarachnoid Hemorrhage
(ruptured berry aneurysm) |
|
|
What is the micro appearance of a saccular (berry) aneurysm?
|
No muscular wall or intima in aneurysm sac
**only hyalinized intima** |
|
|
Result from occlusion of deep penetrating arteries which supply basal ganglia, hemispheric white matter, brainstem.
**Gross & micro** • Cavitary lesions (lacunes-lake–like) 15 mm wide • Fat-laden macrophages with surrounding gliosis |
Lacunar Infarct
(plugging vessels, no bleeding) |
|
|
**Gross & micro**
• Cavitary lesions (lacunes - - - lake–like) 15 mm wide • Fat-laden macrophages with surrounding gliosis |
Lacunar Infarct
(plugging vessels, no bleeding) |
|
|
Most common causes of Hypertensive Cerebrovascular Disease?
|
Atherosclerosis, Diabetes
|
|
|
Hypertensive patient who has diffuse cerebral dysfunction including:
» Headaches » Confusion » Vomiting convulsion » Sometimes coma - Related to increased intracranial pressure ***Gross & micro**** Generalized edema • May have transtentorial and / or tonsillar herniation • Scattered petechiae in gray and white matter • Evidence of remote hemorrhage and foci of necrosis |
Hypertensive Encephalopathy
|

