![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
117 Cards in this Set
- Front
- Back
|
What are common features of all types of locomotion? |
It's rhythmic with alternating movements. |
|
|
What are the four types of animal models used to study locomotion? |
1. Intact: no cuts/preps, everything is intact. 2. Reduction: spinal cord is cut, so that muscles controlling hind limbs are intact but the brain stem, cerebellum, and cortex are missing 3. Decerebrate: Brainstem is cut either above or below midbrain. If cut below, the cerebral cortex is not intact while the midbrain, pons, medulla, and spinal segments are. Deafferentation: Cut is at the dorsal roots so motor neuron activity/muscle activity is intact, but there is no sensory information. 4. Immobilization: Neuromuscular junction is cut. Sensory information and motor neuron DISCHARGE is intact but there is a loss of muscle ACTIVITY, including reflexes. |
|
|
What are the two types of human evidence used in the study of locomotion? |
1. Developmental studies 2. Clinical populations |
|
|
What is the central pattern generator? Where are they? |
A neuronal network that generates a rhythmic pattern of motor activity in absence of rhythmic activity from sensory receptors. They are found in L6 in invertebrates/lower vertebrates. ie. in the spinal cord. |
|
|
Explain Brown's Half-Center theory of CPGs. |
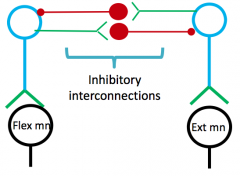
Claims that flexors and extensors are controlled by two groups of CPGs, and that each limb has its own set. There are mutual inhibitory connections between the half centres so that when the flexor is activated, the extensor will be inhibited. The inhibited half center will be activated when excitability of the active one falls below a critical value. |
|
|
Are CPGs independent? |
They are capable of producing movement on their own, but they actually don't usually. We have to adapt rhythmic movements when we approach obstacles, which is when the sensory system helps them out. Therefore, CPGs do receive input from afferent pathways (ie. somatosensory from skin/muscle, visual, vestibular) and descending commands. |
|
|
What are the types of sensory information that provide input to CPGs? |
Muscle: ie. cat and treadmill experiment - stance becomes shorter as treadmill speeds up even without descending commands from the brain. During peak extension, flexors had a burst of activity in the muscle spindles (swing phase). Also prolonged activity in extensors during stance with inhibition of flexors via GTOs being on, which isn't the usual action for them (phase dependent reflex reversal). Skin: again with cats - touching the paw during STANCE phase give extensor activity with flexors inhibited; touching the paw during SWING phase elicits flexor activity with extensors inhibited. |
|
|
What is the MLR? |
Area in the midbrain that controls initiation and speed of locomotion. Stimulating this area initiates stepping, and the intensity of that stimulation directly affects walking speed. THIS DOES NOT AFFECT LIMB COORDINATION. |
|
|
Where does the MLR project to? |
Medial reticular formation, which then projects to the spinal cord. |
|
|
True or false: ataxia is a medical diagnosis. |
False. Ataxia is a symptom of something else. |
|
|
Name the types of ataxia. |
Sensory ataxia: occurs when you have a disruption of propioceptive input (don't know where your limbs are in space). - Can have these disruptions at a central level (ie. at level of CNS; ascending paths, thalamus/parietal cortex) or peripheral paths (afferent peripheral roots, dorsal nerve roots) Cerebellar ataxia: occurs via direct damage to the cerebellum or pathways leading in or out of it, or structures related to it. |
|
|
What are the features of sensory ataxia? |
Wide, stomping gait with heavy heel strike. The patient relies heavily on visual feedback (marked disability with eyes closed or in the dark) Can detect this via balance testing with eyes open and closed |
|
|
Lesions to midline structures of the cerebellum lead to ____________. |
Lesions to midline structures of the cerebellum lead to bilateral symptoms, such as truncal ataxia (ie. of the trunk), titubations (head and upper trunk tremors), and gait abnormalities. |
|
|
Lateral lesions to the cerebellum lead to ____________. |
Lateral lesions to the cerebellum lead to ipsilateral limb symptoms during skilled motor activity. |
|
|
Define dysmetria. |
Dysmetria is the inability to judge distance or range, resulting in either over or undershooting errors. |
|
|
Define dysdiadochokinesis. |
Dysdiadochokinesis is difficulty with movement reversal, ie. the inability to perform rapid alternating movements. The agonist cannot begin second phase while the antagonist muscle involved can't cease its activity. |
|
|
Define interaction torques. |
Interaction torques are turning moments brought on by one torque. In other words, one torque is influencing other turning torques (ie. if you swing your shoulder forward, you hips will turn to keep your body from lurching forward). |
|
|
What is the decomposition of movement in relation to cerebellar lesions? |
Decomposition of movement is a manifestation of cerebellar disease in which movements cannot be carried out smoothly, but are instead broken up into components. |
|
|
Define the rebound phenomenon. |
The rebound phenomenon describes the loss of the "check" reflex which functions to halt forceful, active movements (ie. braking). It illustrates the dysfunction fo the antagonist-agonist relationship. |
|
|
What are the two types of tremors? |
Resting Action (postural, intention) |
|
|
True or false: hypotonia usually clears up within a few weeks following an acute cerebellar lesion. |
True. |
|
|
What are the cognitive impacts of a cerebellar lesion? |
Poor executive functioning (ie. decreased verbal fluency, working memory) Impaired spatial cognition (ie. poor visuo-spatial memory) Linguistic difficulties |
|
|
What are the impacts on eye movement following a cerebellar lesion? |
- Ocular dysmetria (over or undershooting of eyes when attempting to focus gaze) - Nystagmus - Fixation of vision accuracy is decreased |
|
|
How do clients with ataxia generally present? |
Wide BOS, slow/uneven steps Slower movements Increased reliance on vision Restricted action Increased postural sway Locked joints Brace segments Using hands during STS |
|
|
How does COP movement change with damage to the lateral lobe of the cerebellum? |
Very slight, actually! Not much different from normal. |
|
|
How does COP movements change with lesions to the medial lobe of the cerebellum? |
Low frequency with high amplitude. |
|
|
Which lobe of the cerebellum would have to be damaged if the patient presents with a postural tremor? |
The anterior lobe. |
|
|
Which lobe of the cerebellum would have to be damaged if the patient presents with increased intersegmental movements? |
The anterior lobe. |
|
|
What are the three motor performance tests for ataxia? |
Tapping test: takes number of finger taps in 10 secs. Tests motor dexterity. Spiral test: measures deviations from a template NHPT: measures fine motor dexterity |
|
|
What are some compensatory approaches to managing ataxia? |
Decompositioning of multi-joint movements to single joints Using visual/verbal cues to take bigger steps Using assistive tech Using aids (ie. seating aids to help posture) |
|
|
What are some remediation approaches to managing ataxia? |
Physiotherapy has positive effects on gait, trunk control (NOT limbs), and decreases activity limitations. Cycling programs are good to increase coordination/locomotion/balance. This is especially true in cerebellar vs. sensory ataxia. Adding OT might improve global functional status and diminish depression. |
|
|
True or false: people with neurological conditions often have CVD comorbidities from deconditioning. |
True - 75% of people with stroke have heart disease, people with MS have a higher chance of heart failure, post-TBI patients have a greater chance of mortality from circulatory conditions. |
|
|
True or false: there is strong evidence for increased mental ad aerobic capacity for patients with TBI following aerobic exercise. |
False - evidence in this area is pretty weak. |
|
|
True or false: there is strong evidence for increased aerobic capacity and walking endurance/speed for patients with MS and stroke with aerobic exercise. |
True! |
|
|
What is a submaximal exercise test? |
A submaximal exercise test is designed for testing in the neurological population. |
|
|
What are the advantages and limitations of submaximal exercise testing? |
Pros: accessible for PTs (feasible, more options); feasible for participant (ie. exercises are planned for intensity, not exhaustion); and it's an objectively graded exercise test (ie. good for aerobic prescription) Limitations: you're only hitting the submax training zone, relies on ACCURATE USE of Rated Perceived Exertion scale, and ECGs are recommended for those with cardiac disease. |
|
|
What blood pressure levels indicate that you should stop exercising and alert the physician immediately? |
SBP >180; DBP>110 |
|
|
What blood pressure levels indicate that it's OK to exercise? |
SBP <140; DBP <90 |
|
|
What are some indications to stop the submaximal aerobic test? |
If patient requests to stop, if HR drops/fails to rise, drop in DBP, excessive rise in BP, sign of poor perfusion, angina, failure of equipment, severe SOB, HR exceeds outer limits, RPE reaches 5/10, cadence cannot be maintained |
|
|
How does one determine the HR outer limit during an aerobic exercise test? |
60-70% of age predicted HR (use 60 if lower intensity is warranted), or 45% of HRR (difference between resting/max HR) |
|
|
What RPE range do we usually want the patient to reach during a submaximal aerobic exercise test? |
3-4/10
|
|
|
What is PROPEL? |
A 6 week program upon transition to outpatient rehab, including fitness class plus a 1 hour group discussion which identifies barriers, setting goals, and promoting self management after discharge. This program resulted in greater exercise outcome expectations, fewer perceived barriers, and greater participation in PA. |
|
|
What is AIDS? |
HIV infection + CD4 count less than 200 cells/mm^3 |
|
|
What is toxoplasmosis? |
An infection caused by a protozoan that causes mass lesions. Signs and symptoms include intellectual slowing and seizures. Px is good. |
|
|
What is PML? |
Patches of demyelination caused by JC virus. Broad symptoms, like cerebellar signs, dementia, blindness, etc. Px is poor. |
|
|
What is a primary CNS lymphoma? |
Cancer of the lymphatic system. Symptoms include lethargy and headaches. Px is poor. Palliative radiation is possible. |
|
|
What is vacuolar myelopathy? |
Most common spinal cord disease seen in HIV. Presents as hyperreflexia in the lower extremity, ataxia, and progresses to loss of sphincter function. Px is fair to poor. Progresses with periods of stability. |
|
|
What do spinal cord infections stemming from HIV present as? |
As ipsilateral symptoms to paraplegia. These symptoms can be reversed. |
|
|
What is distal symmetrical polyneuropathy? |
Axonal degeneration. Shooting pain distal to knees, hypersensitive, reflexes in ankle absent, but it's rare to have weakness or affected thighs/hands. |
|
|
What is inflammatory demyelinating polyneuropathy? |
Presents as progressive ascending quadraparesis, generalized areflexia, resp/swallowing muscles affected. However, sensory loss is minor. These symptoms can reverse but relapses are possible. |
|
|
What is mononeuropathy multiplex? |
Affects the nerve roots/trunks and cranial nerves. Signs and symptoms are scattered, can be sensory or motor. |
|
|
What is CMV radiculopathy? |
Infection involving lumbar/sacral roots, cauda equina. Shown as flaccid paralysis of LE, sphincter dysfunction, ascending sensory loss, sciatica. Px is a steady progression to death. |
|
|
What are the dimensions of episodic disability in the context of HIV? |
Uncertainty Challenges to social inclusion Difficulty with day to day activities Symptoms/impairments |
|
|
What are the contextual factors that interact with the dimensions of disability in HIV? |
Extrinsic (stigma, social support) Intrinsic (living strategies, personal attributes) |
|
|
What are triggers that can start an episode of disability in someone with HIV? |
Receiving the diagnosis Starting or changing meds Illness Suffering a loss of others |
|
|
What are the general advantages of using water as part of PT treatment? |
It has multisystematic applications and it makes things easier on the therapist. It's also good to practice skill performances in different context to facilitate motor learning (ie, in water!) Tactile info is also enhanced in water. = |
|
|
What are the three main properties of water? |
Intrinsic a) Viscosity: ease at which water will flow, influenced by temp (not density). Thermal a) Conductivity: ie. loss of heat is faster in water vs. air. Thermoregulation differs between core and peripheral body temperatures. Warm water reduces spasticity and, improves collagen distensibility, and induces relaxation. Mechanical a) Hydrostatic pressure: decreases sympathetic input, which reduces fight/flight response. The force exerted on the body can also aid in edema reduction. b) Buoyant force: want to align COB with COG c) Total drag force: |
|
|
What are the short term mechanical adaptations to being immersed in water? |
Venous compression to increase central blood vol Increased in stroke vol HR decreases due to more efficient pumping Increased renal output Increased endocrine system Increased blood flow to muscles Increased resp work |
|
|
True or false: aquatic PT training has equal effects to that of dry land PT training. |
True |
|
|
What are the exercise applications to turbulence of water? |
It tests balance and allows eccentric muscle action (stopping is harder) |
|
|
What are the exercise applications to buoyancy of water? |
Resistive and assists with movements. |
|
|
What are some of the contraindications of training in water? |
Open wounds Incontinence Acute vomiting, diarrhoea Medical instability Chlorine allergy SOB or angia at rest Cardiac failure etc |
|
|
What are some precautions to training in water? |
Tubing Preg Skin conditions Heart/resp conditions Hypermobile joints Fear of water Decreased sensation |
|
|
What are some of the disadvantages to using pools to train? |
Expensive upkeep Not very accessible in terms of time and money Effort and time to change clothing |
|
|
Who benefits from aquatic training? |
All conditions! As long as the goals are acceptable. This includes patients from the ICU, acute care, rehab, chronic, community... |
|
|
What are some goals suitable for aquatic therapy interventions? |
Reducing spasticity Reducing pain Reducing edema Mobilizations Joint off loading and traction Gait retraining Balance retraining |
|
|
Stimuli are elicited from _______, _______, and ______ in aquatic therapeutic environments |
Stimuli are elicited from the environment, the patient, and the therapist in aquatic therapeutic environments |
|
|
What are advantages for the therapist to use aquatic physio? |
Positional advantages Access to 3D patters and consistent resistance Therapist can move against or with movement |
|
|
What are advantages for the patient to use aquatic physio? |
They can maintain stance with little support Fall prevention Manages comorbidities |
|
|
What is the Halliwick Concept? |
Emphasizes students to have physical freedom in the water (no aids) When COB and COG are not equal, the body rotates to achieve balance Ten Point Program? |
|
|
What is the BRRM? |
Resistance aquatic therapy based on PNF. The client is fully supported by equipment and resists movements concentrically, eccentrically, and statically, directed by the therapist. Goal is to achieve stable equilibrium |
|
|
What are the principles of BRRM? |
1. Biomechanics:: temp increase = fluid tissue 2. Fluid mechanics: no fixed points due to buoyancy; turbulence = resistance; skin drag = propio 3. Neurophysiology: pushing pt facilitates stabilizing while pull and propio stimulation facilitates movement |
|
|
What is WATSU? |
Based on the benefits of touch from therapist or water - letting movement happen passively in a supported position |
|
|
What is AQUA-T RELAX? |
Aquatic therapy in a cradle position - using breath and perception of muscle tension to influence ANS |
|
|
True or false: the level of disability in a person with ALS changes over the course of several years. |
False. The course of disability progresses over a period of months. |
|
|
True or false: the prevalence of ALS is 50x greater in the Pacific Rim. |
True. |
|
|
True or false: certain occupations, such as soccer players or military workers, pose a greater risk of ALS development. |
True! |
|
|
True or false: ALS is more common in nonwhite males. |
False - ALS is more common in whites, males. |
|
|
What are the established risk factors of ALS? |
Age: risk peaks between 50-75, or juvenile if genetic Family history: 5-10% of patients have a family history of ALS. Environmental factors are inconclusive. |
|
|
What are the possible causes of the pathogenesis of ALS? |
Oxidative stress (ie. ROS damage), mitochondrial dysfunction (abnormal energy production, Ca homeostasis), increased glutamate in CSF, protein aggragation, impaired axonal transport, dysregulated endosomal trafficking, autoimmune/inflammatory processes, persistent viral infection |
|
|
True or false: ALS is classified as a motor disorder. |
False - it's a multisystem disorder, Sensory/spinocerebellar paths, substantia nigra, and hippocampus is affected in some patients. HOWEVER, motor neurons are affected earliest and most severely because they have large cell sizes and axons. ALS negatively impacts axonal transport and mitochondrial function, as well as Ca homeostasis - it all adds up. |
|
|
What are the first symptoms seen typically in ALS? |
Onset is usually asymmetrical, with the first signs being UMN or LMN in ONE LIMB that spreads to other areas. Initial weakness is also seen in isolated, distal muscles. Sensory exam is usually normal. Oculomotor, bowel, bladder functions are preserved - more resistant. |
|
|
Describe the bulbar-onset pattern of patients with ALS. |
The patient will present with dysarthria/dysphagia. LMN signs will include bulbar palsy (weakness of face, tongue, and palate). UMN signs include pseudobulbar palsy (jaw jerk, pathological laughing/crying, tongue spasms). This pattern is more commonly seen in women |
|
|
Describe the limb-onset pattern of patients with ALS. |
Can be presented as cervical or lumbar onset. Lumbar onset: LMN signs in the legs like foot drop, but the UMN signs often follow. Degeneration of anterior horn. Cervical onset: bilateral OR unilateral UE symptoms that include proximal or distal weakness, UMN OR LMN signs. |
|
|
Describe the respiratory-onset pattern of patients with ALS. |
The patient will present with dyspnea, respiratory muscle weakness, nocturnal hyperventilation, thick mucous secretions, pneumonia Can also experience dysphagia and dysarthria |
|
|
How does one diagnose ALS? |
There is no specific diagnostic test for it. The diagnosis is reached after ruling out other pathologies and when progression of the disease is observed. Definite diagnosis of ALS involved: Evidence of LMN and UMN degeneration, progression of symptoms to other regions, absence of both neuroimaging and pathological/electrophysiological evidence of other disorders that might explain symptoms |
|
|
True or false: multidisciplinary care prolongs survival in patients with ALS. |
False. Evidence for this is conflicting. However, this does not mean that MDC is ineffective. |
|
|
Describe the medical management of ALS. |
Disease modifying: riluzole (inhibits glutamate release), neurotrophins (saves dying motor neurons?), olexisome 64 (protective compound that targets mitochondria) Symptom control: benzos/morphine to manage chronic dyspnea, SSRIs to combat depressio, pathological laughing/crying responds to drugs well, opioids for pain, mucolytic drugs for secretions, Baclofen for spasms |
|
|
Describe PT involvement for patients with ALS. |
May be beneficial in the early stages with a focus on compensatory strategies. The rapid decline of this disease requires a unique PT approach to follow, called Rehab in Reverse (ie. transfer assistance seen in reverse from independent to using a lift; going from AROM to PROM). Otherwise, education (ie. pressure relief, environment mods, expectations), chest PT, ROM/strengthening (in EARLY stages, results in higher functional scale scores), preventing contractures and pain reduction are within the scope here. Long term goals reflect end of life concerns and care needs. |
|
|
What are some of the challenges PTs face when treating patients with ALS? |
Difficult conversations Patients may be looking for a CURE Family members PTs may feel like they have no impact Fulfilling needs in a short period of time Not getting patient's hopes up High drop out rates |
|
|
Where do preganglionic sympathetic neurons originate? |
Gray matter of lateral horns in T1-L2. |
|
|
Where do preganglionic parasympathetic neurons originate? |
Gray matter of lateral horns S2-S4. |
|
|
What kind of sensory stimuli does the ANS respond to? |
Visceral afferent (ie. ones attached to sensory receptors entering the dorsal horn OR cranial nerves carrying sensory info) or somatosensory stimuli like pain. |
|
|
Name the three visceral afferent pathways. |
1. Enters spinal cord and participates in reflex activity 2. Enters spinal cord and projects afferent info to the medulla 3. Projects directly to the medulla (if the afferent info is carried by a cranial nerve) |
|
|
True or false: the parasympathetic system does not participate in peripheral vascular control. |
True; here, there is just a decrease in sympathetic activity |
|
|
The parasympathetic system controls the cardiovascular system through the __________ nerve. |
The parasympathetic system controls the cardiovascular system through the vagus nerve. |
|
|
How is the CV system affected in a SCI with respect to the sympathetic and parasympathetic systems? |
- Loss of sympathetic preganglion neurons - The parasympathetic system remains intact because it controls the CV system via the vagus nerve and this nerve is safe in the skull - This results in decreased activity of the sympathetic system, so you get low BP, loss of BP adaptability, and loss of reflex control. |
|
|
How is the large blood supply in the abdomen controlled by the sympathetic system? |
At the level of T6 this supply is controlled. The descending sympathetic preganglia synapse with a splanchnic nerve at T6 and control the blood vessels supplying the organs in the abdomen. |
|
|
Define orthostatic hypotension. |
A decrease in SYSTOLIC BP by >20mmHg or a decrease in DIASTOLIC BP by >10mmHg after assuming an upright position from supine. Common in SCI patients. |
|
|
What is the clinical significance of orthostatic hypotension? |
It affects the patient's ability to participate in rehab and the likelihood of patients experiencing OH is greater if they have HIGHER SCI lesions. |
|
|
What are the differences in SBP and DBP in individuals with SCI vs. healthy individuals? |
Patients with SCI have lower SBP and DBP that progressively decreases after assuming an upright position -- with increased HR. |
|
|
How do therapists help address the issue of OH? |
Tilt table |
|
|
Define autonomic dysreflexia. |
Medical emergency resulting from uncontrolled sympathetic input - huge increase in BP triggered by stimuli below the lesion level. Increase in BP by at least 20% with symptoms like sweating, chills, goose flesh, headaches, or flushing, hypertension, bradycardia, vasoconstriction below lesion and vasodilation above lesion. |
|
|
Explain the mechanism of AD. |
A stimuli below the lesion, like distended bowel, is detected by mechanoreceptors and enters the SC, but cannot travel past the lesion. It goes to a postganglia instead and is detected as a noxious stimuli. This triggers a big sympathetic response. Vasoconstriction is detected by baroreceptors and this info is sent to the brain which interprets this as a crisis. HR slows down but the level below the lesion still goes unchecked. This can lead to coma, death, etc. |
|
|
Define autism. |
A neurodevelopmental disorder with an impairment in social interaction and repetitive behaviours. Onset is in early childhood and develops over the lifespan. |
|
|
What are the two core characteristics of autism according to the DSM? |
- Preference for sameness - Impairment with social interaction |
|
|
What are some of the motor impairments associated with ASD? |
Hypotonia Motor apraxia Toe walking Gross motor delay Postural instability Poor balance, coordination Visumotor/object manip impaired Decreased participation in rec activities |
|
|
What are some strategies a PT can use on a patient with ASD? |
Early intervention Core control General strength, endurance, balance Ball skills for object manipulation Gait training Stretching Postural alignment Remember to respect sensory concerns and to adapt the assessment. Make the treatment play-based and have ROUTINES. Communicate CLEARLY. Read child's cues and tune into their interests. |
|
|
ICF-CY ShortList of Activity and Participation Domains |
- Lifting and carrying heavy objects - Fine hand use - Transportation - Walking - Moving around |
|
|
What are the possible deficits associated with spina bifida (6)? |
Motor Sensory Bowel/Bladder Hydrocephalus GM function Ortho deformities |
|
|
With respect to spina bifida, what is the functional level of a thoracic level patient? |
Full time sitter as an adult (ie. wheelchair) - may do some walking with a walker or RGO when young. For upright mobility they use a stander. |
|
|
With respect to spina bifida, what is the functional level of an upper lumbar level patient at L3? |
Can do walking at home, may do some ambulation out in the community but orthosis usually required for walking (AFOs, HKAFO, KAFO) |
|
|
With respect to spina bifida, what is the functional level of an lower lumbar level patient at L4? |
70-80% are community ambulators, using wheelchairs for LONG distances or equipment like AFO, KAFO, canes |
|
|
With respect to spina bifida, what is the functional level of an upper lumbar level patient at L5? |
Full time ambulators, may use rigid or hinged AFOs. |
|
|
With respect to spina bifida, what is the functional level of a sacral level patient? |
Community ambulator as an adult. May have foot deformities. May have AFOs. No physical impairments but they may have impaired bowel/bladder. |
|
|
Assessment of spina bifida (6)? |
Spinal and primitive reflexes Tone Passive range of motion Mappingof motor and sensory deficits Skeletal abnormalities Hydrocephalus For infants you might include visual tracking |
|
|
Treatment for spina bifida (5)? |
Parenteducation Support sensorimotor development Monitor skin Address PT orthopaedic needs, Arrange communityrehabilitation support |

