![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
27 Cards in this Set
- Front
- Back
|
Where is the nasotemporal division in the eye?
|
The fovea centralis
|
|
|
What is the 'classic' visual pathway/ what structures does it go through?
|
The image forming pathway:
1. Nasal or temporal visual field 2. Optic nerve 3. Optic chiasm (Nasal fields cross) 4. Optic tract 5. Lateral geniculate nucleus of thalamus (reorganised into function, location, eye - maps contralateral visual field) 6. Optic radiation (meyer's loop - temporal lobe - superior visual field) 7. V1 inferior retina - inf bank V1 superior retina - sup bank V1 central retina - caudal V1 peripheral retina - rostral V1 |
|
|
What structures does the non-image forming (unconscious) visual pathway go to?
|
Suprachiasmatic (Sch) - time-keeper (circadian)
Pretectum (Pre) - pupillary reflex (II,III) Superior Colliculus (SCol) - visual reflex (attention, avoidance) Pulvinar (Pul) - higher-order (attention, integration [see, touch, hear]) Secondary Visual Cortex (V2-V5) - orientation, colour, motion |
|
|
What problems with vision would occur with lesions to V1 and each of the secondary visual cortices (V2-5)?
|
V5 - motion detection: a life in photographs
V5a - face recognition: facial agnosia V4 - colour, colour edges: colour blind V2,V3 - orientation V1 - conscious vision, topography: blindsight (some residual vision) |
|
|
What is the pathway of the direct and consensual light reflex?
|
› Melanopsin ganglion cells of the retina project bilaterally via optic tract & Sup. brachium to pretectal nuclei.
› Pretectal nuclei projects crossed and uncrossed fibres to the Edinger- Westphal nucleus › Edinger-Westphal nucleus → preganglionic parasympathetic fibres › Exit midbrain with CN III and synapse with postganglionic parasympathetic neurons of the ciliary ganglion, › ciliary ganglion innervates the sphincter muscle of the iris. |
|
|
What is the cause of:
› normal consensual response when illumination of normal side › diminished pupillary constriction on direct illumination abnormal side |
Relative afferent pupillary defect (RAPD) - related to lesions within the anterior visual pathways (retina, optic nerve chiasm and optic tract)
|
|
|
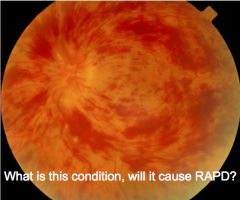
Central retinal vein occlusion, will cause RAPD
|
|

|
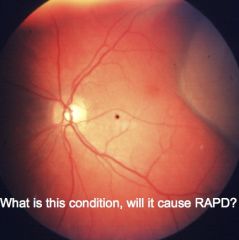
Papilloedema, will cause RAPD
|
|

|
Macular degeneration will not cause RAPD, because enough light signal will be coming through from spared retina to allow reflex
|
|
|
Retinal detachment, whether it causes RAPD depends on how much of the retina is detached
|
|
|
What artery supplies the optic nerve?
|
Posterior ciliary artery
|
|
|
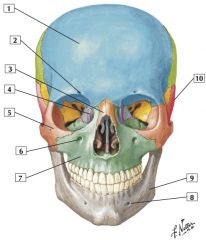
1. Frontal bone
2. Supra-orbital notch (foramen) 3. Nasal bone 4. Lacrimal bone 5. Zygomatic bone 6. Infra-orbital foramen 7. Maxilla 8. Mental foramen 9. Mandible 10. Temporal bone |
|
|
What is the pathway of the sympathetic (dilation) reflex of the eye?
|
• Arises from upper thoracic intermediolateral cell column of spinal cord (T1-T2) sending preganglionic fibres to sympathe0c trunk
• Synapse in Superior Cervical ganglion • Postganglionic fibres ascend along internal caro0d artery, and enter the orbit on Ophthalmic artery. • Pass thru’ the Ciliary ganglion (without synapse) or along Long and Short Ciliary nerves to eyeball • Innervate the Dilator muscle of the Pupil + Mullers muscle of the upper eyelid |
|
|
Which types of cells form myelin?
|
Oligodendrocytes
|
|
|
How many axons does one oligodendrocyte myelinate?
|
Up to 40
|
|
|
What investigations would you do for MS?
|
- MRI
- CSF - Optic nerve function |
|
|
What type of neuropathy does Thiamine deficiency cause?
|
Distal small fibre neuropathy (sensory > motor)
|
|
|
What type of neuropathy does Vitamin B12 deficiency cause?
|
Demyelination and axonal loss
May also cause degeneration of central axons |
|
|
What type of neuropathy does Charcot-Marie-Tooth Disease cause?
|
Dysmyelination, behaves as a length dependent neuropathy
|
|
|
What symptoms/ signs does Guillaine Barré Syndrome cause?
|
• Acute onset of ascending weakness
• May produce complete paralysis • Loss of reflexes (areflexia) • Peak weakness in days to weeks • Spontaneous improvement (limited by axonal loss) • Often follows an immune stimulus (respiratory or gastro-intestinal infection) |
|
|
How does diabetes cause neuropathy?
|
• Neurons are obligate glucose users
• High blood sugar = High neuronal sugar • This leads to: – Disrupted electron transfer in mitochondria – High reactive oxygen species levels – Peroxidation of proteins and lipids • The result is impaired metabolism and cell death • High glucose levels lead to: – Reactive Oxygen Species – Advanced Glycation End products • This leads to impaired production of nerve growth factors and a damaged axonal microenvironment • ROS and AGEs damage endoneurial endothelial cells in capillaries • AGEs lead to increased thickness and density of capilliary basement membrane material impairing oxygen transfer. |
|
|
What can delay onset and slow progression of diabetic neuropathy?
|
Good glucose control
|
|
|
What information is processed in the parvocellular and magnocellular layers of the LGN?
|
Parvocellular - chromatic vision (colour) and high acuity vision
Magnocellular - movement |
|
|
About 10% of the fibres in the optic nerve terminate in the superior colliculus. What is it's role?
|
The SC helps to orient the eyes to salient stimuli in the environment. It does this by integrating many sensory modalities.
|
|
|
Which part of the optic pathway is thought to be important in blindsight?
|
Retinal projections to the superior colliculus
|
|
|
Which part of the visual pathway is important in circadian rhythm?
|
Fibres from the optic nerve going to the suprachiasmatic nucleus of the hypothalamus
|
|
|
What pathway is involved in maintaining the visual field centred on the retina when the head is moving?
|
The vestibulo-ocular reflex - sensory afferents from semicircular canals --> vestibular nuclei -->
1. contralateral nucleus of relevant extraocular muscle via the medial longitudinal fasciculus (MLF) 2. ipsilateral oculomotor nucleus 3. inhibition to ipsilateral antagonist muscle |

