![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
29 Cards in this Set
- Front
- Back
|
What structural feature is most important for the physical aspects of the BBB?
|
The continuous tight junctions between endothelial cells form the morphological correlate of the BBB.
The endothelial cells in systemic tissues have discontinuous tight junctions. |
|
|
Why is L-Dopa used for treatment of Parkinson Disease instead of Dopamine?
|
Dopamine cannot cross the BBB, L-Dopa has a transporter (and is converted to dopamine in brain parenchyma)
|
|
|
At what temperature does cardiac fibrillation occur?
A. 40-44 B. 34-36 C C. 30-34 C D. 27-29 C |
• Normal range: 36-38 C
• Fever or exercise: 38-40 C • Heat stroke: 40-44 • Mild hypothermia: 34-36 C • Severe hypothermia: 30-34 C • Cardiac fibrillation: 27-29 C |
|
|
The classic triad of bacterial meningitis consists of
|
Fever
Headache Neck stiffness |
|
|
How is acute meningitis diagnosed?
|
CSF examination of blood culture
|
|
|
What are the 3 common bacterial pathogens of acute meningitis?
|
Streptococcus pneumoniae, Haemophilus influenzae type b (Hib), and Neisseria meningitidis
|
|
|
What would you expect to find in the CSF of a patient with acute bacterial meningitis?
|
- Numerous neutrophils
- Low glucose - High protein |
|
|
What are the 4 common pathogens of acute viral meningitis?
|
– Echo
- Coxsackie - Mumps - Measles |
|
|
What would you expect to find in the CSF of a patient with acute viral meningitis?
|
- Lymphocytes
- Normal glucose - protein ± raised |
|
|
What organisms commonly cause chronic meningitis?
|
– Tuberculosis
– Cryptococcus |
|
|
What type of encephalitis is carried and spread by fruit bats in Australia?
|
Lyssavirus
|
|
|
What is the empirical therapy for bacterial meningitis?
|
– ceftriaxone/(cefotaxime) (3rd generation cefalosporin)
+ penicillin/(ampicillin) (beta lactam) (not required 3 months - 15 years. ie. Listeria rare unless neonate, immune suppressed, pregnancy, alcoholism, >60yo) – increasingly, vancomycin if ? pen-R pneumo Penicillin or cephalosporin ceased once organism identified and susceptibility available. |
|
|
What treatment can be added to antibiotics to reduce inflammatory damage in bacterial meningitis?
|
Corticosteroids (dexamthasone) given prior to or simultaneously with antibiotics decreases damage from host inflammation response, esp in children
|
|
|
What is the treatment of TB?
|
4 drugs for 9-12 months
• Isoniazid • Rifampicin • Pyrazinamide • Ethambutol (+/- Fluoroquinolones + Corticosteroids) |
|
|
The most common cause of aseptic meningitis is...
|
Enteroviruses (80%)
|
|
|
What would you expect to find in the CSF of a patient with aseptic (enterovirus) meningitis?
|
A moderate white blood cell count (50 - 500 cells) and the absence of bacterial pathogens
Enteroviruses may be isolated from CSF by cell culture in 50-60% of cases. Molecular diagnostic assays, such as the polymerase chain reaction, can identify the presence of enteroviruses in the CSF in >90% of cases |
|
|
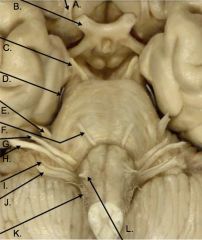
A. Olfactory
B. Optic C. Oculomotor D. Trochlear E. Trigeminal F. Abducens G. Facial H. Vestibulocochlear I. Glossopharyngeal J. Vagus K. Accessory L. Hypoglossal |
|
|
Lesion to WHICH nerve or nucleus results in ipsilateral ophthalmoplegia (paralysis or weakness of one or more of the muscles that control eye movement): It also results in
(i) mydriasis: loss of parasympathetic generating diluted pupil. (ii) accommodation of lens is lost; causes blurred vision for near objects (iii) eye turns down and out (unopposed actions of superior oblique [down,in] and lateral rectus (abduct]) (iv) ptosis (eyelid droop) (loss of LPS); usually more marked than Horner Syndrome |
CN III - Ocularmotor
|
|
|
What are two unusual features of the trochlear nerve?
|
(i) it is the only crossed cranial nerve;
(ii) it is the only one that exits dorsally from the brainstem. |
|
|
With a lesion to WHICH nerve, the eye displays:
(i) extortion (outward rotation), albeit slight, of superior aspect of eye, (ii) weak depression of eye, particularly when eye adducted. Diplopia, particularly noticeable when the patient is walking down stairs. |
Trochlear nerve (CN IV)
|
|
|
A lesion to WHICH nerve causes:
opened jaw deviates to ipsilateral side due to unopposed lateral pterygoid of contralateral side; some wasting in masseter muscle (major muscle of mastication). |
V3 Mandibular
|
|
|
A lesion to WHICH nucleus or nerve results in:
(i) Bell’s palsy (paralysis of ipsilateral facial muscles) (ii) loss of lacrimation (dry eye), some loss of taste, salivation impaired. (iii) hyperacusis: sound is abnormally loud (loss of stapedius which acts to dampen excessive vibrations of the tympanic membrane) |
Facial nerve (VII)
|
|
|
Damage to WHICH nerve can produce deafness, loss of balance as well as dizziness, nausea and nystagmus?
|
Vestibulocochlear (VIII)
|
|
|
WHICH lesions result in a loss of the gag reflex and dysphagia, loss of taste and can result in reflex bradycardia and syncope? Neuralgia can also result in pain affecting oropharynx and/or tonsils.
|
Glossopharyngeal nerve (IX)
|
|
|
A lesion to WHICH nerve commonly results in
i) Palate weakness (dyspalatia): sagging of faucial arch and uvula deviation to contralateral side of lesion ii) Pharyngeal weakness (dysphagia): if bilateral a marked dysphagia ensues iii) Laryngeal weakness (dysphonia): may cause hoarseness and vocal weakness |
Vagus nerve (X)
|
|
|
Damage to WHICH nerve can result in weakness of head rotation away from the damaged side and causes drooping of the shoulder?
|
Accessory nerve (XI)
|
|
|
A lesion to WHICH nerve results in atrophy of ipsilateral muscles of tongue: When protruded, the tongue deviates to side of lesion due to unopposed actions of the intact genioglossus muscle of the other side
|
Hypoglossal (XII)
|
|
|
What is the characteristic triad associated with raised intracranial pressure?
|
Headache, vomiting and papilloedema
|
|
|
What should never be done in the presence of papilloedema or focal neurological signs until you have ruled out focal mass lesion?
|
Lumbar puncture
|

