![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
54 Cards in this Set
- Front
- Back
|
What are the regions of the hypothalamus?
|
- Anterior = Parasympathetic area
- Medial - Posterior = Sympathetic area - Lateral = Drinking center thirst |
|
|
What are the consequences of lesions to the anterior hypothalamus?
|
Parasympathetic area:
- Hyperthermia - Insomnia - Diabetes insipidus (not enough ADH --> loss of water --> hypernatremia) - Emaciation |
|
|
What are the consequences of lesions to the medial hypothalamus?
|
- Hyperdipsia (excessive thirst)
- Diabetes insipidus (not enough ADH --> loss of water --> hypernatremia) - SIADH (too much ADH --> water retention --> hyponatremia) - Obesity - Rage - Amnesia - Dwarfism |
|
|
What are the consequences of lesions to the posterior hypothalamus?
|
Sympathetic area:
- Hypothermia - Poikilothermia (body temp. fluctuates by 2*) - Hypersomnia / coma - Narcolepsy - Apathy - Ipsilateral Horner Syndrome |
|
|
What are the consequences of lesions to the lateral hypothalamus?
|
Drinking Center
- Adipsia (lack of thirst) - Emaciation - Apathy |
|
|
Which divisions of the hypothalamus are involved in excessive or lack of thirst? Result of lesions to these areas?
|
- Excessive - medial hypothalamus
- Lack - lateral hypothalamus |
|
|
Which divisions of the hypothalamus are involved in weight? Result of lesions to these areas?
|
- Emaciation - lateral hypothalamus
- Obesity - medial hypothalamus |
|
|
Which divisions of the hypothalamus are involved in temperature? Result of lesions to these areas?
|
- Hyperthermia - anterior (PNS)
- Hypothermia, poikilothermia - posterior (SNS) |
|
|
Which divisions of the hypothalamus are associated with diabetes insipidus (not enough ADH --> loss of water --> hypernatremia) when lesioned?
|
- Anterior Hypothalamus (PNS)
- Medial Hypothalamus |
|
|
What are the significant nuclei of the anterior region of the hypothalamus?
|
- Suprachiasmatic Nucleus
- Anterior Nucleus |
|
|
What is the function of the Suprachiasmatic Nucleus? What will a lesion cause? Location?
|
- Regulates Circadian Rhythm - stimulated by light hitting retina
- Lesions cause insomnia - Anterior Hypothalamus (PNS) |
|
|
What can cause a loss of neurons in the Suprachiasmatic Nucleus?
|
- Alzheimer's disease
- People who work at night (inadequate stimulation of this nucleus) |
|
|
Which part of the brain is responsible for regulating the circadian rhythm?
|
Suprachiasmatic Nucleus (anterior region of hypothalamus)
|
|
|
A lesion to what part of the brain causes insomnia?
|
Suprachiasmatic Nucleus (anterior region of hypothalamus)
|
|
|
What is the function of the Anterior Nucleus? What will a lesion cause? Location?
|
- Dissipates heat
- Lesion causes hyperthermia - Anterior region of hypothalamus |
|
|
What stimulates the Anterior nucleus? How does it mediate its effect? Treatment?
|
- Stimulated by endogenous pyrogens (secreted by immune system during infxn), including IL-1 and PGE2
- Pyrogens travel to hypothalamus and induce a fever - PGE2 synthesis can be blocked by aspirin |
|
|
Which part of the brain is responsible for dissipating heat?
|
Anterior Nucleus (anterior region of hypothalamus)
|
|
|
A lesion to what part of the brain causes hyperthermia?
|
Anterior Nucleus (anterior region of hypothalamus)
|
|
|
What is the function of the Medial Hypothalamus? What will a lesion cause?
|
- Regulates feeding behavior (stops overeating)
- Lesion causes obesity due to overeating (eat more than normal and less active; react more emotionally to food) - Lesions frequently caused by craniopharyngioma, pituitary adenoma, and Prader-Willie syndrome |
|
|
What is a craniopharyngioma and what are the symptoms? What can it cause?
|
- Hypothalamic tumor (primarily in children)
- Tumor expands and increases intracranial pressure --> headaches, bitemporal hemianopsia, endocrine disturbances due to compression of pituitary stalk/gland - Can cause lesions to medial hypothalamus (or surgery to remove can) - Leads to overeating --> obesity - |
|
|
What is a pituitary adenoma? What can it cause?
|
- Pituitary tumor
- Can cause lesions to medial hypothalamus - Leads to overeating --> obesity |
|
|
What happens in Prader-Willie syndrome? Cause?
|

- Chromosomal deletion of 15q11-13
- Inherited from father - Hypothalamic dysfunction includes hyperphagia (increased eating) --> obesity - Also causes narcolepsy and short stature |
|
|
Where do sympathetic neurons originate? Where do the fibers go?
|
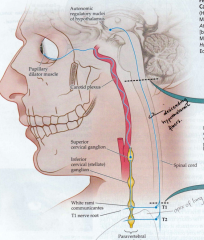
Hypothalamus (posterior region) --> descend in Descending Hypothalamic Fibers (DHF) - lateral part of brainstem
|
|
|
What can cause a lesion of the Descending Hypothalamic Fibers (DHF)? What kind of fibers are in here?
|
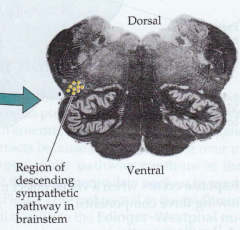
- Brainstem stroke (e.g., lateral medullary stroke)
- Sympathetic neurons |
|
|
What do the Descending Hypothalamic Fibers (DHF) synapse on?
|
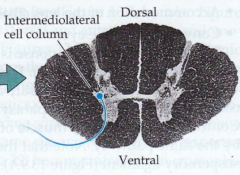
Cell bodies in the Intermediolateral cell column (IML) in the thoracic cord (pre-ganglionic cells)
|
|
|
What can cause a lesion of the Intermediolateral (IML) cell column? What kind of fibers are in here? Effect?
|
- Spinal cord injury (stroke, compression, tumor)
- Descending hypothalamic fibers (DHF) are synapsing on pre-ganglionic cells - Decreased sympathetic output to various target organs |
|
|
What leaves the Intermediolateral cell column? Path?
|
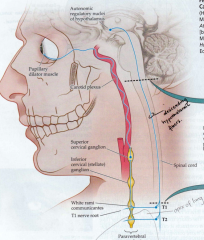
- Pre-ganglionic neurons exit cord
- Enter sympathetic chain and synapse onto several ganglia (including superior cervical ganglia = SCG, inferior cervical ganglia, celiac ganglia, etc.) - Synapse on post-ganglionic neurons that send axon to target |
|
|
How do sympathetic fibers reach the eyes?
|
- Preganglionic fibers exit Intermediolateral cell column
- Enter sympathetic chain - Ascend into Superior Cervical Ganglion (SCG) - Synapse onto post-ganglionic fibers - Post-ganglionic fibers ascends ICA --> cavernous sinus - Sends axons to dilator muscle of pupil |
|
|
What happens in Klumpke's Palsy?
|
- Damage to lower trunk of brachial plexus
- May cause disrupted sympathetic output (ipsilateral Horner's) - Ipsilateral finger paralysis (all directions of movement) w/ normal proximal arm muscle strength |
|
|
In a Klumpke's Palsy, what side do you see the symptoms of Horner's syndrome? Why?
|
- Ipsilateral
- Decreased sympathetic output |
|
|
What is Pancoast syndrome? Effects?
|
- Infiltration of Superior Cervical Ganglion (SCG) or lower brachial plexus by cancer
- E.g., lung cancer on apex of either lung - Disrupts ipsilateral sympathetic output (ipsilateral Horner's syndrome) |
|
|
What happens in a dissection of the ICA?
|
- Separation of the various layers of an artery
- Blood dissects through layers and may travel through a false lumen and reconnect with the true lumen more distally - Expands the artery - Stretches the sympathetic fibers traveling on surface of artery - Causes a decrease in sympathetic output - Also exposes blood to regions of artery not lined with endothelium --> more prone to clot formation --> embolize (shoot-off) distally into the MCA and cause strokes |
|
|
What happens in Cavernous Sinus Thrombosis?
|
- Inflammation of cavernous sinus (can occur in people with chronic sinusitis (infection or inflammation of adjacent sinuses)
- Clot formation --> compress cranial nerves and sympathetic fibers traveling with ICA resulting in multiple cranial neuropathies and sympathetic dysfunction |
|
|
How can you determine if pupils are reacting appropriately?
|
- Determine dilation in darkness
- Determine constriction in light - Even if their pupils are naturally different sizes the ratio should stay the same; if not it is pathological |
|

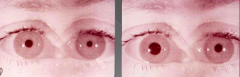
What is the diagnosis?
|

Horner's Syndrome (on L)
- Ipsilateral: - Miosis - small pupil - Ptosis - weakness of superior tarsal muscle (Müller's) - Anhidrosis - decreased facial sweating |
|
|
What causes Horner' syndrome? Symptoms?
|
- Lesion of the sympathetic pathways anywhere along its axis (DHF, SCG, etc)
- Miosis, ptosis, anhidrosis |
|
|
Where is the intermediolateral cell column in the spinal cord?
|
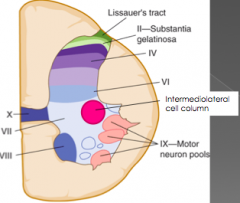
T1-L2
|
|
|
What mediates the pupillary light reflex?
|
- Parasympathetic innervation
- Information travels to pretectal nucleus in midbrain --> - Bilateral innervation of Edinger-Westphal nucleus --> - Neurons travel to ciliary ganglion --> - Parasympathetic neuron travels to ciliary constrictor muscle |
|
|
What do you learn in the swinging flashlight test?
|
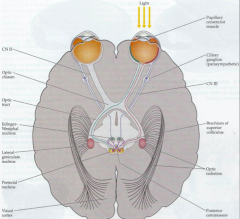
- Both eyes should dilate when light shines on either eye
- If when you shine it one one eye, both eyes dilate, there is an optic n. lesion / afferent pupillary defect |
|
|
How does the SNS affect the bladder?
|
- Detrusor relaxed
- Internal urinary sphincter contracted ** Store = SNS ** |
|
|
How does the PNS affect the bladder?
|
- Detrusor contracts
- Internal Urinary Sphincter relaxes ** Pee = PNS ** |
|
|
During urinary continence, how are the SNS and PNS affected?
|
- PNS inhibited (PNS = pee)
- SNS stimulated (SNS = store) |
|
|
During urination, how are the SNS and PNS affected?
|
- PNS stimulated (PNS = pee)
- SNS inhibited (SNS = store) |
|
|
How is sensation of the bladder sent to the brain?
|
- Sensory afferents from detrusor muscle convey information about fullness of bladder via S2-S4 nerve roots
- Information ascends to primary sensory cortex where sensation of bladder fulness in perceived |
|
|
What is the pathway of preventing urination to the detrusor and internal urinary sphincter?
|
- Micturition inhibitory center (medial frontal cortex) provides voluntary inhibition of flow of urine
- Neuron travels from medial frontal cortex to inhibit the pontine micturition center - Descends to lower thoracic/lumbar sympathetic region (T11-L1) to activate it - Inhibits parasympathetic region - Stops urination b/c internal urinary sphincter is contracted and detrusor is relaxed |
|
|
What is the pathway of preventing urination to the external urinary sphincter?
|
- Neurons from medial frontal cortex travel to Onuf's nucleus (alpha-motor neurons in S2-S4, ventral horn of spinal cord)
- Travel via pudendal nerve - Mediates contraction of EUS |
|
|
What is the pathway of urination to the detrusor and internal urinary sphincter?
|
- Inhibition of sympathetic pathway
- Neurons from pontine micturition center are not inhibited --> Intermediolateral cell column in T11-L2 sympathetic region - Preganglionic neurons travel out cord to inferior mesenteric ganglion - Postganglionic neruons travel via pudendal nerve to internal urinary sphincter (not stimulated --> relaxed) and detrusor (inhibition is lessened --> contracts) - PNS is stimulated --> neurons from sacral spinal cord (S2-S4) stimulate detrusor to contract and IUS to relax |
|
|
What can cause urinary incontinence?
|

- Hyperactive "spastic" bladder or underactive sphincter --> bladder spasms at low urine volume
- Hypoactive "flaccid" bladder or overactive sphincter --> prevents complete emptying |
|
|
What causes a "spastic" bladder? How do you treat it?
|

- Hyperactive bladder (detrusor)
- Underactive sphincter - Due to lesions of sympathetics - Treat with anti-cholinergics to relax bladder walls |
|
|
What causes a "flaccid" bladder? How do you treat it?
|
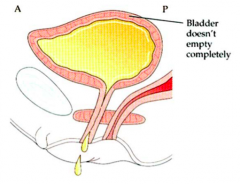
- Hypoactive bladder (detrusor)
- Overactive sphincter - Due to lesions of parasympathetics - Treat with anti-adrenergics to relax sphincter; self-catheterization |
|
|
CASE 1: 42 yr old female experiences weight gain of 100 lbs over a 3 month period of time, along with episodic hot flashes with unexplained fevers, and a visual field cut.
Which is the most likely pattern of her visual field deficit? What does this patient have? |

- Bitemporal field cut (due to proximity to optic chiasm)
- Hypothalamic tumor (craniopharyngioma) |
|
|
CASE 2: 69 yr old woman reports diminished sweating over her left face. She also has ptosis of the left, and anisocoria with the left pupil being smaller than the right. The left pupil also does not dilate appropriately in darkness. The other cranial nerves are normal.
What is wrong? |
- L ptosis, L miosis, and L anhidrosis --> Horner's syndrome --> L sympathetic chain to eye affected
- Lack of other long tract signs, lesion unlikely to be in brainstem * Neoplasm in the apex of the left lung |
|
|
CASE 3: 23 yo RH F presents with acute onset L sided numbness. She c/o R neck pain but attributed it to “whiplash” after riding roller coasters all day 2 days ago.
EXAM: - In darkness, L eye dilates, no change in R eye - With lightboth eyes constrict - L sided f/a numbness to PP, proprioception - Awkward when asked to pantomime ability to comb hair, brush teeth with L hand - No weakness - Reflexes symmetric, toes downgoing What is wrong? |
- R Horner's syndrome --> R sympathetic chain lesioned
- L hand apraxia --> R parietal lesion * Stroke of R parietal cortex due to dissection of R ICA from whiplash due to rollercoaster riding; R ICA dissects --> lesions R sympathetics --> thrombus from R ICA embolizes into R MCA division --> Stroke in R parietal cortex |
|
|
CASE 4: 24 yo M was drinking heavily with friends on the 4th of July and fell from a 2nd story balcony. He landed on his back in a seated position. Since then he has not been able to move legs. It has been 3 months since accident.
EXAM: Spastic paraparesis. 0/5 strength in legs. Reflexes 4+ with clonus. Absent rectal & bulbocavernosus reflex. He c/o of incontinence. After emptying bladder, catheterization shows no further urine in the bladder. Which is true about his bladder? |
**He has parasympathetic overactivity to bladder
- T10 spinal cord compression (affects SNS and PNS control of urination) - Sx more consistent w/ spastic bladder b/c self-catheritization failed to remove any trapped urine - Incontinence is due to detrusor contracting (excess PNS activity) - Cannot sense bladder fullness b/c afferent information traveling via sacral cord is lesioned |

