![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
114 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
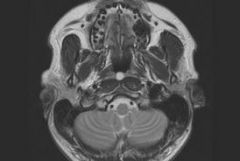
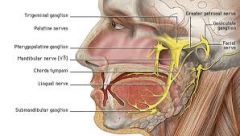
What is FALSE regarding juvenile nasopharyngeal angiofibroma?
a. Preoperative embolization may be helpful b. Erodes, remodels posterior wall of maxillary sinus c. Commonly involves sphenoid sinus at presentation d. More common in adolescent boys e. Arises from pterygopalantine fossa f. Frequently invades the orbit g. Commonly associated with epistaxis |

Arises from pterygopalatine fossa (FALSE)
-originates from sphenopalatine foramen in the lateral nasopharyngeal wall |
-most common benign tumor of nasopharynx
-adolescent males -recurrent epistaxis -bowing of the posterior wall of the maxillary antrum -grow through pterygopalatine foramina and fossa (widens the foramina) -supplied primarly by the internal maxillary artery -biopsy is contraindicated |
|
|
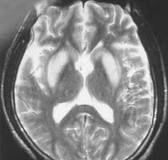
Luckenshadel (lacunar skull) is associated with which of the following:
a. Myelomeningocele b. Dandy-Walker c. Craniosynostosis d. Prematurity e. Increased ICP |

Myelomeningocele
|
Luckenshadel
-clusters of deep calvarial pits with steep edges and interspersed bony trabecular ridges that involve the inner table and diploe -always associated with meningomyelocele -commonly seen in Chiari II malformations -spontaneously disappear by 4-6 months old |
|
|
Myelination occurs in what direction?
a. Rostral to caudal b. Peripheral to central c. Dorsal to ventral d. Sensory to motor |
Dorsal to ventral,
caudal to rostral, central to peripheral, motor to sensory |
-T1 weighted images are useful in 1st 8 months of life and myelin follows fat on T1-weighted images given its high lipid content and hydrophobia.
In evaluating myelination, hyperintensity on T1 precedes hypointensity on T2 -Hyperintensity on T1 can be thought of as indicating active myelination whereas hypointensity on T2 indicates completed myelination. |
|
|
The spinal cord most commonly ends at normal level (has normal conus level) in the following:
a. Sacrococcygeal teratoma b. Imperforate anus c. Diastematomyelia d. Myelomeningocele e. Chiari II with lipomyelomeningocele |

Sacrococcygeal teratoma
|
-Sacrococcygeal teratomas usually show normal level of conus
-Imperforate anus as part as VACTERL is associated with tethered cord V-verterbral anomalies A-anal atresia C-CV defects T-tracheoesophageal fistula E-esophageal atresia R-renal anomalies L-limb anomalies -Diastematomyelia associated with tethered cord in 75% -Chiari II , associated lumbosacral meningocele or meningomyelocele that tethers the cord is nearly always present |
|
|
Midline facial defect/cleft are associated with:
a. Holoprosencephaly b. Septo-optic dysplasia c. Agyria d. Chiari II e. Dandy-Walker f. Schizencephaly |
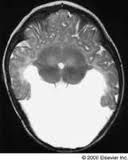
Holoprosencephaly
|
Causes of median facial cleft
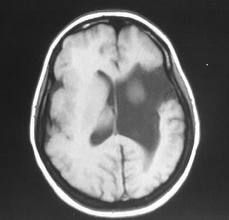
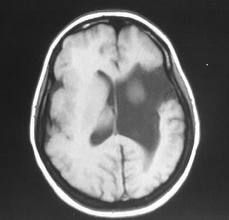
1. median cleft face syndrome 2. Holoprosencephaly Imaging of holoprosencephaly -Single ventricle -Absent or partial hemispheric and basal cleavage with absent interhemispheric fissure/falx - Azygous ACA -± associated facial defects -50% of patients with holoprosencephaly have trisomy 13 -Check for septum pellucidum; If present, it excludes the Dx of holoprosencephaly. Semilobar and Lobar HPE -less severe entities of HPE spectrum -semilobar - incomplete interhemispheric fissure, abnormal cc -lobar - interhemispheric fissure present |
|
|
Flat tire sign in orbit is indicative of what:
a. Ruptured globe b. Vitreal hemorrhage c. Dislocated lens d. Post septal hematoma |

Ruptured globe
|
Posterior collapse of the sclera causes flattening of the posterior contour of the globe
|
|
|
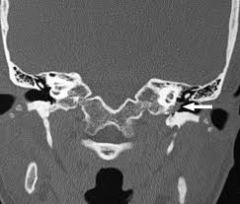
Amorphous calcification just below anterior arch of C1. Likely diagnosis?
a. HADD b. CPPD c. DISH d. Gout e. RA |
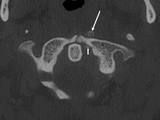
HADD (Calcium hydroxyappetite deposition disease)
|
-under-recognized cause of acute cervical pain
-occurs with longus colli muscle -Amorphous calcification anterior to C1-2 with associated asymmetric soft tissue swelling is pathognomonic -most commonly seen about the shoulder may disappear completely in 1 to 2 weeks -CPPD could also produce calcification in this region, but it would also involve other adjacent C1-C2 ligaments |
|
|
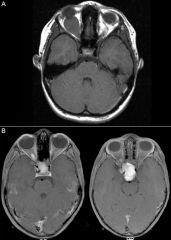
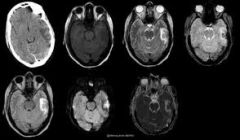
What is TRUE regarding metastasis to the brain?
a. Uncommon in posterior fossa in adults b. Papillary thyroid carcinoma commonly present with (hemorrhagic) metastasis c. Squamous cell mets solitary < 5% of the time d. Cystic metastases suggest (are seen with) mucinous adenocarcinoma e. Most commonly occur in the ventricles |
Cystic metastases suggest mucinous adenocarcinoma
|
Distal hematogenous dissemination is less common in papillary thyroid than with follicular cancer
|
|
|
Left occipital infarct. What visual field deficit?
a. A contralateral (right) homonymous hemianopsia b. Ipsilateral (left) homonymous hemianopsia c. Bitemporal hemianopsia d. Scotoma |
Contralateral (right) homonymous hemianopsia
-an injury beyond the chiasm, anywhere from optic tract, lateral geniculate, optic radiation or calcarine cortex, can result in homonymous hemianopsia |
Homonymous hemianopsia: most common cause is CVA in PCA territory
Bitemporal hemianopia: injury to middle part of optic chiasm: pituitary tumor or craniopharyngioma |
|
|
All of the following are associated with Chiari II EXCEPT:
a. Large posterior fossa b. Large mass intermedia c. Tectal beaking d. Myelomeningocele |

Large posterior fossa (NOT associated with Chiari II)
|
Chiari II:
callosal dysgenesis tectal beaking small posterior fossa vermian ectopia medullary kinking Also associated with: -enlarged mass intermedia (gray matter connecting thalami) -syrinx -fenestration of the falx cerebri with herniation of individual gyri across midline Chiari I malformation is generally clinically occult and consists of the cerebellar tonsils herniating by >5 mm below the foramen magnum. CSF flow dynamic alterations can give rise to cervical syrinx |
|
|
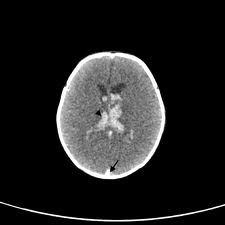
65 year-old man, normotensive, presents to ER with symptoms of CVA. Non-contrast CT demonstrates large irregular shaped hemorrhage in right frontal lobe. Most likely cause?
a. amyloid angiopathy b. hypertensive hemorrhage c. hemorrhagic metastasis d. dural venous sinus thrombosis |
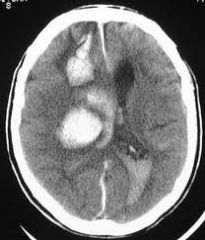
Amyloid angiopathy
|
Amyloid angiopathy hemorrhages
-characteristically lobar and spare the basal ganglia, brain stem, and cerebellum -frontal and parietal regions most common, involving cortex and subcortical WM |
|
|
Choroid plexus is seen in the following locations EXCEPT:
a. Body of the lateral ventricles b. Anterior and posterior horns of the lateral ventricles c. Atria of the lateral ventricles d. 3rd ventricle |
Anterior and posterior horns of lateral ventricles and cerebral aqueduct (NOT seen in these places)
|
present in all components of the ventricular system except for the cerebral aqueduct and the occipital and frontal horns of the lateral ventricles
|
|
|
Scanning with a 3 T MR vs. 1.5 T MR scanner?
a. Decreased susceptibility artifact b. Increased signal to noise ratio c. Increased energy deposition by 10% d. Bad quality MRA |
Increased signal to noise ratio
|
At higher magnetic fields, motion, flow, and susceptibility effects also increase.
|
|
|
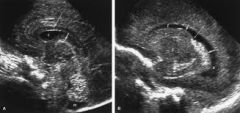
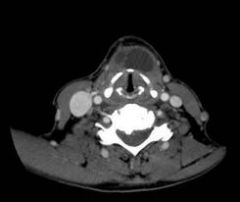
16 week-old fetus with cystic lesion in lateral neck most likely has which chromosomal abnormality:
a. Trisomy 13 b. Trisomy 18 c. Trisomy 21 d. Turner’s syndrome |
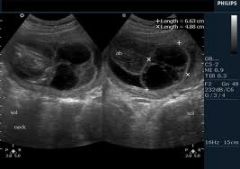
Turner's syndrome
|
Cystic hygromas
-lymphatic malformations which may be obstructed -most strongly associated with Turner's syndrome (XO) but also with trisomy 18 and 21 Prenatal cystic neck masses include: cystic hygroma cephalocele cervical teratoma cervical meningocele |
|
|
Staging of squamous cell cancer of the neck depends on the following:
a. size of LNs b. number of LNs c. laterality of LNs d. size (of lesion) and number of LNs e. size (of lesion), number of LNs, and laterality of LNs |
Size (of lesion), number of LNs, and laterality of LNs
|
|
|
|
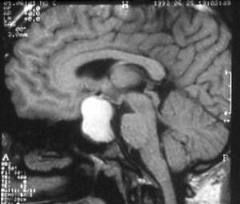
What is TRUE regarding normal pituitary gland? (two correct)
a. larger in males than females b. enhances like normal brain parenchyma c. enhances rapidly and prominently d. enlarges during menopause e. has a flat or concave superior border f. normal pituitary is hypoenhancing relative to adenoma |
enhances rapidly and prominently
has a flat or concave superior border, larger in females (during cycle and pregnancy) normal pituitary is hyperintense compared to adenoma |
-prompt enhancment of the anterior pituitary gland, the infundibulum, and cavernous sinuses
-enhances after the administration of intravenous contrast medium, because it lacks a blood brain barrier -posterior pituitary is already high intensity on T1WI -pituitary microadenomas are hypointense compared with the normal gland -superior border is flat or concave. If it is rounded, then suspect microadenoma -In females, the size of the gland varies with the menstrual cycle and pregnancy |
|
|
Which is FALSE regarding Thornwaldt cysts?
A associated with (midline) skull base (and C1) defect B notochord remnant C MRI T1 signal varies with protein content D located in posterior nasopharyngeal space E usually asymptomatic F midline abnormality |
Associated with skull base defect (FALSE)
|
Thorwaldt’s cysts
-midline congenital pouch/cysts lined by ectoderm -posterior wall of the nasopharyngeal mucosal space -asymptomatic, incidental -hypointense or hyperintense on T1 depending on the protein content -related to the embryogenesis of the notochord -NO bone erosion |
|
|
In neurofibromatosis (NF-1), what is the cause of pulsatile exophthalmos?
a. sphenoid wing dysplasia b. enlargement of optic/carotid canal c. carotid cavernous fistula d. bupthalmos e. choroidal hamartomas |
Sphenoid wing dysplasia
|
NF1 distinctive osseous lesions involve sphenoid wing dysplasia
Pulsatile exophthalmos is caused by herniation of subarachnoid space and temporal lobe into the orbit |
|
|
MR imaging in a 12 year old reveals an enlarged optic chiasm (optic nerve lesion) and a focus of increased T2 signal within the basal ganglia and cerebellum. Most likely represents?
A Neurofibromatosis 1 B Neurofibromatosis 2 C Tuberous Sclerosis D Sturge-Weber |
Neurofibromatosis I
|
NF-I:
-Plexiform neurofibroma (PNF) -Sphenoid dysplasia (SD) -Buphthalmos (BUPH) -Optic pathway glioma (OPG) |
|
|
Cerebellar lesion with T2 hyperintensity in the cerebral peduncles and optic nerves. Diagnosis?
a. Neurofibromatosis II b. Neurofibromatosis I c. Tuberous sclerosis |
Neurofibromatosis I
|
NF1:
-nonneoplastic hamartomas -hyperintense on T2 and not visible on T1 NF2: MISME Multiple Inherited Schwannomas Meningiomas Ependymomas Tuberous sclerosis -multiple hamartomas and tubers |
|
|
What is associated with neurofibromatosis type 2?
a) Meningioma b) Optic tract gliomas c) Chromosome 17 d) café au lait spots |
Meningioma
NF2 = MISME Multiple Inherited Schwannomas, Ependymomas and Meningiomas |
|
|
|
Identify anterior choroidal artery on an angiogram (shown a diagram of a carotid/ACA/MCA angiogram)
|
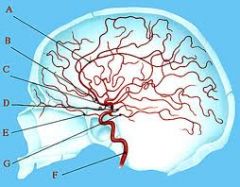
a: Pericallosal Artery; b: Anterior Cerebral Artery; c: Middle Cerebral Artery;
d: Anterior Choroidal Artery; e: Ophthalmic Artery; f: Internal Carotid Artery; g: Posterior Cerebral Artery |
The anterior choroidal artery comes off the supraclinoid carotid artery – last branch off ICA
|
|
|
30 yo male presents with confusion and seizures. High T2 signal (with mass effect) in the temporal lobes (and cingulate gyrus) without contrast enhancement. What is the etiology?
a. Herpes encephalitis b. PML c. Contusion d. Infarction e. MS |
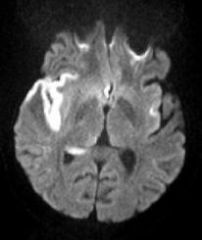
Herpes encephalitis
|
-T2/FLAIR hyperintensity of limbic system (medial temporal and inferior frontal cortex) with DWI restriction
-Patchy parenchymal or gyral enhancement |
|
|
Which is TRUE regarding herpes encephalitis?
a. More commonly seen in children than adults b. Patients are most often mmunocompromised c. Due to herpes zoster virus d. Involves the temporal lobes |
Involves the temporal lobes
|
Herpes enchephalitis
-in infants may be caused by genital herpes (HSV2) from the mother either from transplacental transmission -in adults, caused by Type 1 virus -is only occasionally seen in immunocompromised patient -as high PD/T2 signal in the temporal and inferior frontal lobes with progressive mass effect sparing the putamen |
|
|
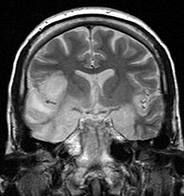
60 year old male with small cell lung cancer presents with asymmetric increased bilateral T2 signal in the mesotemporal regions. Diagnosis?
a. Limbic encephalitis b. Herpes encephalitis |
Limbic encephalitis
|
Paraneoplastic encephalomyelitis (PEM)
-a multifocal inflammatory disorder of the CNS associated with remote neoplasia -80% of cases are associated with bronchial cancer, typically small-cell lung carcinoma -MR usually is unremarkable, although T2 hyperintensity may be noted in mesial temporal lobes and associated limbic structures |
|
|
CN between PCA and superior cerebellar artery?
a. oculomotor nerve b. abducens nerve |
Oculomotor nerve
|
|
|
|
Patient presents with subarachnoid hemorrhage in the perimesencehpalic cistern. LP confirms blood. 4 vessel angiogram is normal. What is the etiology?
a. Subarachnoid hemorrhage not related to aneurysm b. ACOM aneurysm c. Basilar tip aneurysm d. Ruptured AVM |
SAH not related to aneurysm
|
|
|
|
What is true of venous angiomas (DVAs)?
A Related to cavernous malformation B Best seen on non-contrast T1 C Low on T2 |
Related to cavernous malformations
|
-Umbrella-like collection of enlarged medullary (white matter) veins ("Medusa head")
-At angle of ventricle -Numerous linear or dot-like enhancing foci -Converge on single enlarged "collector" vein -"Collector" vein drains into dural sinus/deep ependymal vein -15-20% coexisting cavernous &/or capillary malformations -Venouos angiomas show flow voids on T1 and T2 |
|
|
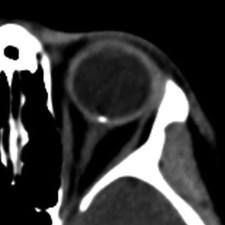
What is FALSE about hemangiomas of the orbit:
a. Prominent arterial supply b. Slowly enlarges c. Retrobulbar |

Prominent artery supply (FALSE)
|
Cavernous Hemangioma, Orbit
-venous malformation of orbit characterized by endothelial-lined cavernous spaces -slow growing -manifest as a painless, progressively proptotic eye - Well-demarcated, ovoid, enhancing intraconal mass -Heterogeneous early patchy central enhancement -CT usually diagnostic in appropriate clinical setting -Specific MR features include patchy enhancement, septations and pseudocapsule |
|
|
All have T1 hyperintense basal ganglia EXCEPT:
a. Neurofibromatosis b. Lehigh disease c. TPN (parenteral nutrition) d. Liver disease (hepatocellular degeneration) e. Calcifications |
Lehigh disease (NOT associated)
|
increased T1W signal in the basal ganglia:
-Ca2+ -NF -hepatic encephalopathy -manganese toxicity (long-term TPN) |
|
|
In a patient with hepatocerebral degeneration (hepatocellular encephalopathy), the basal ganglia demonstrate what signal pattern on an MRI?
a. Low intensity of basal ganglia on T1 b. Low intensity of basal ganglia on T2 c. High intensity of basal ganglia on T1 d. High intensity of basal ganglia on T2 |
High T1 signal in the basal ganglia
|
Chronic hepatic encephalopathy (HE)
-Bilateral T1WI hyperintensity in basal ganglia (BG), particularly globus pallidus (GP) Acute HE -High signal in most of cerebral cortex |
|
|
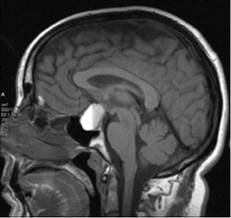
TRUE about pituitary sella masses in children:
A. .Majority of craniopharyngiomas are calcified B. Hamartomas of the tuber cinereum enhance C. Rathke cleft cysts are calcified |
Majority of craniopharyngiomas are calcified
|
-80% of craniopharyngiomas are calcified in pediatrics population vs 40% in adults
-Tuber cinereum hamartomas don’t enhance -Rathke cleft cysts are not typically calcified Craniopharyngioma -Cystic suprasellar mass with calcifications (Ca++) and enhancement of a mural nodule or cyst wall -90% are cystic -90% have calcifications -90% enhance (wall and solid portions) |
|
|
Maximum normal degree of rotation of C1 on C2:
a. 25 degrees b. 35 degrees c. 45 degrees d. 55 degrees |
45 degrees
|
|
|
|
What is associated with myelomeningocele on prenatal US?
a. hydronephrosis b. gastroschisis c. obliterated cisterna magna |

Obliterated cisterna magna (Chiari II malformation)
|
Chiari II malforamation:
callosal dysgenesis tectal beaking small posterior fossa vermian ectopia medullary kinking |
|
|
Which artery is associated with Wallenberg (lateral medullary) syndrome?
a) Ipsilateral PICA b) Contralateral PICA c) Superior cerebellar d) Branches off the basilar artery |
Ipsilateral PICA
|
PICA infarcts
-in loss of pain and temperature sense of the contralateral body and ipsilateral face -ipsilateral Horner’s syndrome PCA infarcts -typically affect vision and may affect memory, smell, and emotion |
|
|
What is the most likely etiology of a lytic skull lesion with well-defined sclerotic borders?
A. Metastasis B. Epidermoid C. Myeloma D. Eosinophilic granuloma E. Fibrous dyplasia F. Venous lake |

Epidermoid
|
Epidermoid inclusion cyst
-well-defined round osteolysis with sclerotic margin Metastasis, myeloma, and EG -multiple lesions and do not have sclerotic borders |
|
|
Woman is post partum, headache; labs show pan-hypopituitarism. MR: T1 hypointense pituitary mass with homogenous enhancement. Diagnosis:
a. Pituitary apoplexy b. Lymphocytic hypophysitis c. Rathke’s cleft cyst d. Craniopharyngioma |

Lymphocytic hypophysitis
Idiopathic inflammation of anterior pituitary |
Imaging:
-Thick stalk (> 2 mm + loss of normal "top to bottom" tapering) -± enlarged pituitary gland -75% show loss of posterior pituitary "bright spot" -Enhances intensely, uniformly Presentation: -Peripartum female with headache, multiple endocrine deficiencies -Middle-aged male with diabetes insipidus (lymphocytic infundibuloneurohypophysitis) |
|
|
Young woman with acute onset of headache, visual loss, and decreased level of consciousness. MR demonstrates a sellar and suprasellar mass with fluid-fluid levels and blood products within it. Statistically, this most likely represents what?
a) Craniopharyngioma b) Rathke's cleft cyst c) Pituitary adenoma d) Pituitary apoplexy e) Complex meningioma |
Pituitary apoplexy
-Acute clinical syndrome with headache, visual defects/ophthalmoplegia, altered mental status, variable endocrine deficiencies -Caused by either hemorrhage or infarction of pituitary gland -Preexisting pituitary macroadenoma common |
Sheehan syndrome is specific for a postpartum infarction of anterior pituitary gland
|
|
|
A 55 year old male undergoes brain MR: temporal lobe lesion which is very dark centrally and bright peripherally on T2. The entire lesion is isointense on T1 weighted images. This most likely represents:
a) Cavernous angioma b) Hemorrhagic contusion c) Herpes d) Abcess |
Hemorrhagic contusion
|
T1WI
-Acute: Inhomogeneous isointensity and mass effect FLAIR -Acute: Best for hyperintense cortical edema and subarachnoid hemorrhage (SAH) |
|
|
Brain MR demonstrates area of bright signal on diffusion, low signal on ADC and normal T2 in insular cortex. Diagnosis?
a. Herpes b. Acute infarct (minutes to hours) c. Subacute infarct (days to weeks) d. Chronic infarct (months to years) |
Acute infarct (minutes to hours)
|
|
|
|
The most medial CN in the cavernous sinus is:
a. II b. III c. IV d. VI |

CN VI
|
Lateral: III, IV, V1, and V2
Only CN VI runs medially next to the carotid artery ICA is even more medial than CN VI |
|
|
Which of the following conditions places a pediatric patient at high risk for latex sensitivity?
A. asthma B. myelomeningocele C. allergy to penicillin D. contrast allergy |
Myelomeningocele
|
-thought to happen secondary to the repeated surgeries
-also seen in spina bifida -higher risk for intraoperative anaphylaxis |
|
|
Patient has bilateral (optic globe) retinoblastomas. Patient most likely has a third lesion located in:
a) the hypothalamus b) the anterior (or posterior) portion of the pituitary c) the pineal gland d) the suprasellar region |

Pineal gland
Trilateral retinoblastoma = bilateral retinoblastoma plus pineoblastoma |
Pineoblastoma
-Highly malignant, primitive embryonal tumor (PNET) -Large, heterogeneous pineal mass - Lobulated with poorly delineated margins -Nearly 100% have obstructive hydrocephalus - Frequent invasion into adjacent brain |
|
|
Common location of intraventricular meningioma:
a. atria of lateral ventricles b. 4th ventricle c. posterior 3rd ventricle d. frontal horns of the lateral ventricles |

Atria of lateral ventricles
|
-Meningiomas are most commonly intraventricular in children
-2-5% of all meningiomas are intraventricular |
|
|
What is most characteristic of neurocystercercosis?
a. Seizures are a common complication b. Females are more often affected than males c. Associated with immunocompromised patients |
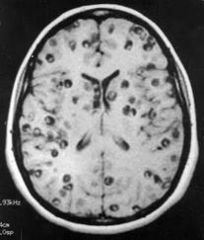
Seizures are a common complication
|
-Intracranial parasitic infection caused by the pork tapeworm Taenia solium
-Best diagnostic clue: Cyst with "dot" inside -Convexity subarachnoid spaces most common location |
|
|
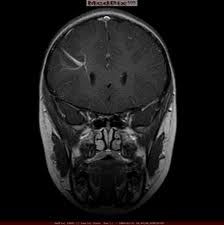
Which is NOT associated with pulsatile tinitus?
a) Jugular bulb dehiscence b) CC fistula c) Aberrant carotid d) Glomus tympanicum e) Cholesteotoma |
Cholesteotoma (NOT associated)
Pic - Glomus tympanicum |
Glomus tympanicum paraganglioma (GTP)
-Clinical profile: 50 year old female with vascular retrotympanic mass & pulsatile tinnitus -CT: Mass with flat base on cochlear promontory -MR: Enhancing mass with flat base on cochlear promontory -Aberrant jugular vein or ICA with associated dehiscence of the jugular/carotid canal may present as a pulsatile mass in the hypotympanum -Aberrant Carotid – enlarged inferior tympanic artery and enlarged aroticotympanic artery can cause pulsatile tinnitus |
|
|
Adult with unilateral papilledema and calcification at junction of globe and optic nerve. Diagnosis:
a. drusen b. retinoblastoma c. choroid osteoma d. hemangioma with calcified phlebolith e. rhabdomyosarcoma |
Drusen
|
If the patient were a child, the answer would be retinoblastoma
Drusen -disc mass with calcification at junction of nerve and globe Rhabdomyosarcoma -most common malignant orbital tumor in childhood Choroidal osteoma -benign tumor of young women -punctuate calcification in the posterior pole of the globe |
|
|
Most echogenic structure on a neonatal head US:
a. Corpus callosum b. Caudate head c. Cerebellar vermis d. Cingulate gyrus e. Choroid plexus glomus |
Choroid Plexus > Vermis > everything else
|
-glomus of choroids plexus is very echogenic-cerebellar vermis gives the appearance of a Christmas tree (also echogenic)
|
|
|
40 year old male w/ hx of GSW to T4 undergoing a cystourethrogram when he experiences increased pulse pressure, rapid breathing, decreased heart rate, flushed face, and pale cool torso. Diagnosis?
a. vasovagal reaction b. autonomic dysreflexia c. allergic response to latex d. allergic response to contrast e. detrussor sphincter dysfunction |
Autonomic dysreflexia
|
-headache, flushing, and diaphoresis
-process observed in queadriplegics |
|
|
Small choroid plexus cysts may normal on prenatal ultrasound. Which chromosomal abnormality is associated with large choroid plexus cysts?
a. Meckel-Gruber syndrome b. Kleinfelter’s syndrome c. Trisomy 21 d. Trisomy 13 e. Trisomy 18 |

Trisomy 18
>10cm; requires amnio |
Normal choroid plexus cysts:
-most resolve by the 3rd trimester. -<10mm Meckel-Gruber syndrome -occipital encephalocele -polycystic kidneys -polydactyly -Yemenite Jews -fatal at birth |
|
|
What lines the cleft in schizencephaly?
a. Gray matter b. White matter c. Germinal matrix d. Dura |
Gray matter
|
Can be result of acquired in utero insult affecting neuronal migration
-Transmantle gray matter lining clefts -Look for dimple in wall of ventricle if cleft is narrow/closed -Up to 1/2 of schizencephalies are bilateral -When bilateral, 60% are "open-lipped" on both sides -Gray matter lining clefts may appear hyperdense -Ca++ when associated with CMV -Prior to myelination T2WI more clearly defines lesion |
|
|
Schizencephaly represents which type of developmental abnormality?
A Induction defect B In-utero infection C Migrational abnormality D Neural tube closure defect |
Migrational abnormality
|
-developmental failure of cell migration to form cerebral cortex, or destruction of a portion of the germinal matrix
Associated with: -polymicrogyria, microcephaly, and gray matter heterotopia |
|
|
Patient who underwent chemotherapy and radiation therapy to brain. CT shows new white matter disease bilaterally. Most likely diagnosis?
a) ADEM b) PML c) Necrotizing leukoencephalopathy d) Adrenoleukodystrophy e) Subacute sclerosing panencephalitis f) Central pontine myelinosis |
Necrotizing leukoencephalopathy
|
-occurs primarily in patients undergoing chemotherapy (most commonly methotrexate)
-occurs with or without radiation -white matter lesions in the centrum semiovale ADEM is an -autoimmune disorder measles, mumps, varicella, pertussis, rubella infection/vaccination -Seizures and focal neuro signs 7-14 days after clinical onset of viral infection PML -usually immunocompromised such as in AIDS. |
|
|
Pediatric c-spine fracture considered stable?
A Flexion teardrop B Atlanto-axial dissociation C Posterior arch of C1 D Type II odontoid E Jefferson fracture |
Posterior (neural) arch of C1 (atlas)
|
Stable C-spine fractures:
-posterior neural arch fracture (C1) -type I odontoid fracture Unstable C-spine fractures -atlantooccipital subluxation/dislocation -flexion teardrop fracture -Hangman's fracture -Jefferson fracture -type II odontoid fracture |
|
|
40 yo male with lower extremity weakness and back pain. MRI shows enhancing mass in lumbar spinal canal which is insinuating around nerve roots and causing posterior scalloping of the vertebral bodies. Diagnosis?
a. Myxopapillary ependymoma b. Neurofibroma c. Arachnoiditis d. Astrocytoma |

Myxopapillary ependymoma
|
-Slow growing glioma arising from ependymal cells of filum terminale
Imaging Findings -Best diagnostic clue: Enhancing cauda equina mass with hemorrhage -Almost exclusively in conus, filum terminale, cauda equina -Well-circumscribed -Isodense intradural mass -+/- enlarging spinal canal & remodeling vertebral cortex (scalloping) -T1 C+: Intense enhancement -T2WI - predominantly hyperintense (mucin) with hypointsense regions (hemorrhage) |
|
|
Which of the following is MOST likely to cause drop metastasis to the spine (in a pediatric patient):
a. medulloblastoma b. choroid plexus papilloma c. juvenile pilocystic astrocytoma d. ependymoma e. lymphoma f. craniopharyngioma g. hemangioblastoma |
Medulloblastoma
|
Medulloblastoma (MB), posterior fossa PNET
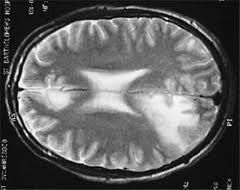
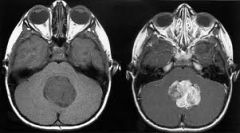
-4th ventricle tumor o Arises from roof (superior medullary velum) o Lateral origin (cerebellar hemisphere) more common in older children/adults -Spherical, pushes brain away on all sides -90% hyperdense on NECT -Small intratumoral cysts/necrosis in 40-50% -Hydrocephalus common (95%) -> 90% enhance -Restricted diffusion, low ADC -Up to 1/3 have subarachnoid metastatic disease at presentation Drop mets Ddx -medulloblastoma -PNET -ependymoma -anaplastic glioma -pinealoblastoma -lymphoma |
|
|
2003 What is the appearance of glomus vagale:
a. splays carotid arteries and internal jugular b. pushes internal jugular medial and carotids lateral c. pushes both internal jugular and carotids anteriorly d. pushes carotids (ICA and ECA) anteriorly and IJ posteriorly |

Pushes carotids (ICA and ECA) anteriorly and IJ posteriorly
|
Paraganglioma, Glomus Vagale
-Avidly-enhancing mass in nasopharyngeal CS -Ovoid carotid space mass -Pushes parapharyngeal space fat anteriorly, styloid process anterolaterally -Anterior and medial displacement of the ICA and ECA without widening of the carotid bifurcation -IJ displacement posteriorly -T1WI shows low signal serpentine or punctate foci ("pepper") secondary to high velocity flow voids if > 2 cm in diameter -T1 C+ MR reveals intense enhancement throughout mass -Glomus vagale and carotid body tumors can be differentiated based on displacement of ECA -Carotid body more common at carotid bifurcation (pushes ECA away from ICA) |
|
|
Huntington's disease affects which structure:
a. Substantia nigra b. Caudate nuclei c. Hippocampus d. Red nucleus e. Mammilary bodies |

Caudate nuclei
|
Huntington’s disease - caudate and putamen
Parkinson’s disease - substantia nigra, locus ceruleus Werncke-Korsakoff syndrome - mammillary bodies |
|
|
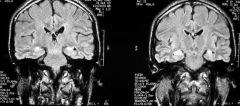
Bilateral T2 hyperintensity in the occipital lobes which resolves 2 weeks later is most likely due to:
a. Posterior reversible encephalopathy (eclampsia/ pre-eclampsia b. Tip of the basilar syndrome c. Progressive multifocal encephalomalacia d. Herpes |

Posterior Reversible Encephalopathy (PRES) seen with eclampsia/preeclampsia
|
PRES
-T2 hyperintensity in cortex and subcortical white matter of occipital parietal region |
|
|
What is the blood supply to the hippocampus:
a) ACA b) MCA c) PCA (in some versions) d) anterior choroidal artery e) pericallosal artery f) basilar artery g) pontine perforators |
Anterior choriodal (most), PCA (some)
|
-anterior choroidal artery arises from the ICA
-supplied by choroid plexus, hippocampus, portions of both pallidal segments, the entire retrolenticular part of the internal capsule, and a ventral part of the PLIC -PCA supplies the occipital and inferior temporal lobes including the hippocampus (which has dual supply |
|
|
Finding of Chiari I malformation on MR?
A. obliteration of the cisterna magna B. beaked tectum C. hydrocephalus D. enlarged massa intermedia E. abnormal corpus callosum |

Obliteration of the cisterna magna
=cerebromedullary cistern |
Chiari I malformation
-congenital tonsillar ectopia |
|
|
What is most commonly associated with Chiari I (or low lying cerebellar tonsils)?
a. Lambdoid-torcular inversion b. Syringohydromyelia c. Elongated and flattened fourth ventricle d. Beaked tectum e. Enlarged posterior fossa f. Hydrocephalus g. Myelomeningocele |

Syringohydromyelia
Synonyms: Hydromyelia, syringohydromyelia, syrinx |
-Expanded spinal cord with dilated, beaded, or sacculated cystic cavity
-Associated with scoliosis (↑ with left curve, high or low apex/end vertebra, male sex, Chiari I or II malformation) -A syrinx is present in about 30% of all Chiari I's, and about 70% of all symptomatic Chiari I's. |
|
|
What is TRUE regarding orbital anatomy?
a. Trochlear nerve innervates inferior oblique muscle b. Annulus of Zinn separates anterior & posterior compartments c.Trochlea of superior oblique muscle is in lateral wall d. Superior ophthalmic vein is superior to ophthalmic artery e. Superior orbital fissure contains the maxillary division of the trigeminal nerve |
Superior opthalmic vein is superior to ophthalmic artery
-Superior ophthalmic vein pursues the same course as the ophthalmic artery passes beween lateral rectus and through the medial superior orbital fissure, ending in the cavernous sinus |
-trochlear nerve (CN IV) innervates the superior oblique (SO)
-oculomotor nerve (CN III) innervates the inferior oblique (IO).] and medial rectus -abducens (CN VI) innervates the lateral recus -trochlea of superior oblique muscle lies superomedially -Annulus of Zinn: conic structure formed by the extraocular muscles (except IO) within the bony orbit -Anterior and posterior chambers are divided by the iris -Superior orbital fissure - CN III, IV, V(V1 branch), VI, and SOV -Foramen rotundum - passing - maxillary nerve and V2 |
|
|
What is the likeliest appearance of ischemic insult to the premature brain?
a. Hemorrhage b. Cystic changes in the periventricular white matter c. Ventriculomegaly d. Q waves on the EEG |

Cystic changes in the periventricular white matter (periventricular leukomalacia)
|
PVL
-white matter insult usually seen in premature infants because of watershed ischemia in the perforating arteries -posterior predominance with the most severe changes seen around the trigone of the lateral ventricle |
|
|
Patient has unilateral facial paralysis with preserved taste (in anterior 2/3 tongue). Where is the likely lesion?
a) pons b) IAC c) CP angle cistern d) petrous apex e) parotid gland |
Parotid gland
|
chorda tympani serves taste to 2/3 anterior tongue, which takes off just before the CN 7 exits the temporal bone before the parotid gland
|
|
|
What is NOT associated with tuberous sclerosis?
a) rhabdomyoma b) sphenoid wing dysplasia c) giant cell astrocytoma d) angiomyolipoma e) renal cysts f) cortical tubers g) calcifications along ventricles h) mass at foramen of Monroe |
Sphenoid wing dysplasia (NOT associated)
(associated with NF1) |
-cortical tubers,
-giant cell astrocytomas, -intrarcranial calcifications -periependymal nodules -angiomyolipomas of the kidney -aortic aneurysm -pulmonary LAM -cardiac rhabdomyomas -renal cysts |
|
|
Best MR sequence for brain shearing vessel injury (detect small hemorrhagic foci of remote DAI):
a. T2* b. T1 spin echo c. T2 spin echo d. Gradient Echo Imaging e. FLAIR |
Gradient echo imaging
80% of DAI are nonhemorrhagic |
-FLAIR: Nonhemorrhagic DAI → hyperintense foci
-GRE: Hypointense foci secondary to hemorrhage -SWI: Depicts significantly more DAI foci than GRE -May show restricted diffusion and ↓ ADC |
|
|
Most likely to be associated with precocious puberty in a female:
a. hypothalamic hamartoma b. craniopharyngioma c. hypothalamic adenoma d. Rathke's cleft cyst e. proactinoma f. hypothalamic glioma |

Hypothalamic hamartoma
-Nonenhancing hypothalamic mass contiguous with tuber cinereum -Mass located between mammillary bodies and infundibulum -Infant with gelastic seizures or precocious puberty -Older children with precocious puberty; tall, overweight, and advanced bone age |
Prolactinoma
-infertility, amenorrhea, and galactorrhea Rathke’s cleft cyst -visual disturbances, pituitary insufficiency, or diabetes insipidus |
|
|
Patient 7 days s/p SAH and aneurysm clipping develops bilateral lower extremity weakness and decreased alertness. Most likely diagnosis?
a. Vasospasm b. Recurrent SAH c. Subdural hematoma d. Hydrocephalus e. Wallerian degeneration |
Vasospasm
-in the setting of SAH, vasospasm is a common complication -blood in basal cisterns is associated with high risk |
Wallerian degeneration
-requires axonal transection -degeneration begins 4-10 days after the initial event |
|
|
Regarding pediatric cervical spine trauma films, which is TRUE?
A. Obliques increase detection of fracture by 20% B. Fractures at C1-2 are more common than at C6-7 C. Fracture is more common than ligamentous injury D. Most commonly missed fracture is flexion teardrop E. Unconscious patient requires flexion/extension |

Fractures at C1-2 are more common than at C6-7
-Children fracture the upper C-spine (atlas and axis) more often than the lower C-spine b/c they have BIG heads that weigh a lot -opposite in adults who tend to injure C6-7 |
Neural arch fracture
-longitudinal fracture through the posterior neural arch, usually bilateral. -caused by hyperextension, with the result that the neural arch of C1 is compressed between the occiput and C2. -best demonstrated on the lateral projection Burst (Jefferson) fracture -comminuted fracture, with bilateral disruption of both anterior and posterior arches -lateral displacement of both lateral masses -caused by axial compression -demonstrated on the open mouth view by Hangman’s fracture (traumatic spondylolisthesis) -hyperextension of the neck transmits the force through to the C2 pedicles -results in an oblique fracture -tension causes disruption of the anterior longitudinal ligament causing this injury to be unstable -demonstrated on the lateral view but may be undisplaced |
|
|
Woman presents with bilateral cheeks enlarging over time and complains of dry mouth. MR shows multiple small cysts parotids bilaterally. Diagnosis:
A. Sjogren's syndrome B. HIV with lymphoepithelial cysts C. Adenoid cystic carcinoma D. Warthin tumor E. Kinky hair Menke syndrome |

Sjogren's syndrome
-bilateral enlarged parotids with multiple cystic & solid intraparotid lesions ± intraglandular calcifications -Primary SjS: Dry eyes & mouth; no collagen vascular disease (CVD) -Secondary SjS: Dry eyes & mouth with CVD, most commonly RHEUMATOID ARTHRITIS |
|
|
|
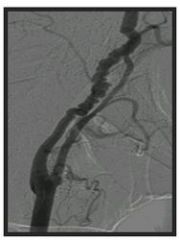
Most common site of extracranial carotid plaques?
A. Carotid bulb and proximal ICA B. Proximal ECA C. Origin of CCA D. Distal ICA at the skull base foramen |
Carotid bulb and proximal ICA
|
|
|
|
Which is TRUE regarding the intervertebral disc?
A. nucleus pulposis is made up of hyaline cartilage B. increased water content is seen with aging C. annular tear is hypointense on T2 weighted images D. annular tear will enhance with gadolinium |

annular tear will enhance with gadolinium
- Focal high intensity zone in the anulus on T2WI with low signal of parent disc -Contrast-enhancement on T1WI -T1 C+: Focally enhancing nidus in posterior disc margin |
-annulus fibrosis is made up of fibrous cartilage
-annulus fibrosis surrounds the nucleus polposus which contains loose fibers suspended in a mucoprotein gel (shock absorber) -With age inner anulus expands at expense of nucleus |
|
|
2 year old boy presents with dehydration and
decreased level of consciousness. Imaging demonstrates bilateral thalamic hemorrhages and associated edema. This most likely is related to: A. Herpes encephalitis B. Vein of Galen aneurysm C. Basilar artery thrombosis D. Bilateral infarcts E. Deep venous sinus thrombosis F. Superior sagittal sinus thrombosis |
Deep venous sinus thrombosis
-infarcts from straight sinus/vein of Galen thrombosis involve the thalami -in children, dehydration, infection, trauma and hematologic disease (protein C deficiency) cause sinus thrombosis |
-infarcts from sagittal sinus thrombosis involve parietal lobes
-infarcts from transverse sinus or sigmoid sinus thrombosis involve the temporal lobe -sagittal sinus is the most commonly occluded sinus followed by the transverse, sigmoid, and cavernous sinuses |
|
|
Which is TRUE regarding thyroglossal duct cysts?
A. they are always superficial to the strap muscles B. most are supra-hyoid C. when carcinoma exists, it is usually papillary type D. shows thick ring enhancement E. most often septated |
When carcinoma exists, it is usually papillary type
-<1% of TGDC have associated thyroid carcinoma -usually papillary -Midline cystic neck mass embedded in infrahyoid strap muscles ("claw sign") -20-25% in suprahyoid neck -Almost 50% at hyoid bone -About 25% in infrahyoid neck |
|
|
|
The vagus nerve accompanies what as it traverses the diaphragm?
a. IVC b. Thoracic duct c. Azygous d. Esophagus e. Aorta |
Esophagus
-aorta and thoracic duct travel together separate from the esophagus through a different opening -azygous and hemiazygous veins individually perforate diaphragm |
|
|
|
Which structure passes under the aortic arch?
a. Left recurrent laryngeal nerve b. Right recurrent laryngeal nerve c. Left vagus nerve d. Right vagus nerve e. Left phrenic nerve |
Left recurrent laryngeal nerve
The left recurrent laryngeal nerve loops under the ductus. |
|
|
|
What is the most common CNS infection in HIV?
A. HIV encephalitis B. PML C. toxoplasmosis D. cryptococcal meningitis |

HIV encephalitis
HIV encephalitis is the most CNS infection in AIDS patients, eventually developing in 60% and typically causing atrophy |
Toxoplasmosis
-most common radiologically discrete CNS lesion -20-40% of AIDS patients -almost always enhances PML -areas of demyelination occur because oligodendrogliocytes infected by JC virus lose their ability to maintain myelin Cryptococcal meningitis -commonly enlarges the perivascular spaces and may create "gelatinous pseudocysts" in the basal ganglia |
|
|
Adult has expansile, enhancing spinal cord lesion with regions of hemorrhage and adjacent cystic lesions. Most likely etiology is:
A. Intramedulary metastasis B. Astrocytoma C. Schwanoma D. Ependymoma |

Ependymoma
-most common cord tumor -often at cervicothoracic level -rim of hemosiderin (propensity for hemorrhage) -drop mets -reactive cysts above and below lesion -seen in NF2 |
Metastasis
-intramedullary are very rare -associated with edema -demonstrate enhancement Astrocytoma -looks just like an ependymoma -but more infiltrative, enhances less -hemorrhage is uncommon Schwannoma -extramedullary, intradural lesion -enhance |
|
|
All of the following are true regarding carotid fibromuscular dysplasia EXCEPT:
A. usually unilateral B. associated with aneurysms C. more common in ICA than ECA D. associated with string of pearls sign E. more common in women |
Usually unilateral (FALSE)
-bilateral carotid involvement is common (65%) -most commonly involves the ICA -medial fibroplasia is the most common associated histology -associated conditions include carotid dissection and saccular -one third of patients with carotid FMD also have renal artery FMDaneurysms -string of beads appearance is considered pathognomonic for medial fibroplasia |
|
|
|
Which lesion resembles multiple sclerosis?
a. Lyme disease b. Parkinson's c. Binswanger's d. HIV encephalitis e. Herpes |

Lyme disease
-high intensity lesions on PDWI/T2WI that enhance MS DDX (clinically and radiographically): Lyme disease Behcet’s disease Syphili Lupus |
|
|
|
Which of these is post-viral and immune-mediated?
a. extrapontine myelinolysis b. Guillain-Barré syndrome c. metachromatic leukodystrophy d. multiple sclerosis |
Guillain- Barre syndrome
-demyelination initiated by antibodies -after a respiratory or GI viral infection -marked enhancement of nerve roots of the conus medullaris and cauda equina |
Central pontine myelinolysis
-seen in chronic alcoholics and malnourished patients -extra-pontine lesions commonly seen in putamina and thalami -caused by osmotic shifts due to rapid correction of hyponatremia Metachromatic leukodystrophy -most common hereditary leukodystrophy -< 2 years -Death in childhood Multiple scelerosis -idiopathic demyelinating disease |
|
|
Which one of the following is the motor strip?
a. calcarine gyrus b. precentral gyrus c. frontal gyrus d. postcentral gyrus |
Precentral gyrus
Precentral gyrus (of the frontal lobe): The primary origin of the stimulus for motor function. Postcentral gyrus (of the parietal lobe): sensory reception ultimately received here. Calcarine gyrus/fissure is associated with the visual cortex. |
|
|
|
What is a ranula?
a. branchial cleft cyst b. submandibular gland c. blockage of the sublingual gland |
Blockage of the sublingual gland
A ranula is a cystic lesion that is due to obstruction of the sublingual gland duct The ranula’s wall usually enhances |
|
|
|
Which represents persistant embryonic connection between carotid and vertebral (basilar) arteries:
a. recurrent artery of Heubner b. tentorial artery c. otic artery |
Otic artery
The persistent otic artery, which is rare, connects the internal carotid artery to the vertebral artery The recurrent artery of Heubner supplies the anteroinferior portion of the head of the caudate (from the ACA). |
|
|
|
In a patient with SAH and known aneurysm, likeli-hood of having multiple intracranial aneurysms?
a. 5% b. 20% c. 45% d. 75-85% |
20%
Saccular aneurysms are true aneurysms where the sac consists of intima and adventitia. They are present in approximately 2% of the population; they are multiple in 20%. |
|
|
|
Which is NOT characteristic of arachnoiditis?
a. clumping of the nerve roots b. relatively empty thecal sac c. linear enhancement of conus d. obliteration of the thecal sac e. enlargement of nerve roots |
Obliteration of the thecal sac (NOT a characteristic)
Arachnoiditis can be caused by surgery, SAH, myelography, infection. In the lumbar spine, adhesion of nerve root to the dural tube giving an “empty sac” appearance, or clumping together of nerve roots leading to a “pseudofilum” appearance. Arachnoiditis may or may not enhance. |
|
|
|
Artery supply of posterior limb of internal capsule?
a. anterior choroidal b. recurrent artery of Heubner c. lenticulostriate d. ACA |
Anterior choroidal artery
The anterior choroidal artery and anterior thalamoperforators supply the posterior limb of the internal capsule. The medial and lateral lenticulostriate arteries and recurrent artery of Heubner supply the anterior limb of internal capsule. |
|
|
|
Which is FALSE concerning epidural hematoma?
a. can arise from dural veins b. can cross sutures c. can cross dura |
Can cross sutures (FALSE)
Epidural hematomas are arterial 90% (middle meningeal artery) and venous 10% (sinus laceration, meningeal vein). (1) 95% are unilateral, temporoparietal (2) biconvex, lenticular shape (3) do not cross suture lines (4) may cross dural reflections in contradistinction to subdural hematoma (5) commonly associated with skull fractures (6) heterogeneity predicts rapid expansion of EDH with areas of low density representing active bleeding |
|
|
|
Right paracentral/far lateral disc herniation at L4-5 cause what symptoms?
a. Right L4 radiculopathy, nerve root symptoms b. Right L5 radiculopathy, nerve root symptoms c. Left L5 radiculopathy, nerve root symptoms d. Right S1radiculopathy, nerve root symptoms e. Right L4 L5 radiculopathy, nerve root symptoms |
Right L5 radiculopathy, nerve root symptoms
Paracentral disk herniations in the lumbar region characteristically strike the root exiting below the interspace. This is because the disk space is inferior to the exiting root at that level. Thus, an L4-5 disk herniation most often compresses the L-5 root. Very lateral herniated disks may compress the upper root; that is, an L3-4 lateral herniation can compress the L-3 root; or, in the case of this question, a far lateral L4-5 herniation can compress the L4 root. |
|
|
|
Elderly male with cervical myelopathy. CT shows thick calcification/ossification at anterior aspect of the thecal sac immediately posterior to the C3-C5 vertebral bodies. This is most consistent with:
a. ankylosing spondylitis b. DISH c. Ossification of posterior longitudinal ligament d. calcification of a previous epidural hemorrhage e. arachnoiditis |
Ossification of posterior longitudinal ligament (OPLL)
Ossification of posterior longitudinal ligament (OPLL) is an inflammatory degenerative condition usually associated with degenerative disease of the cervical spine. often associated with ligamentum flavum calcification occurs along the full course of the posterior longitudinal ligament whereas osteophytes, in comparison, are present only at the disk space DISH - osteophytes occur at end plates at disk level. Ankylosing spondylitis - contiguous thracolumbar involvement (vertebral body “squaring”, syndesmophytes, bamboo spine) Arachnoiditis - blunting of nerve root sleeves without cord displacement. |
|
|
|
Which injury to the C-spine most likely to cause (devastating) neurologic symptoms:
a. Odontoid fracture b. Hangman’s fracture c. Jefferson fracture d. Flexion teardrop fracture e. Type II dens fracture |
Flexion teardrop fracture
Flexion teardrop fracture is the most severe C-spine injury. presents with clinical “acute anterior cord syndrome” (quadriplegia, loss of anterior column senses, retention of posterior column senses). Unstable. fracture through the anterior inferior aspect of the vertebral body with posterior displacement of the posterior aspect of the vertebral body. caused by compressive hyperflexion most common at the C5-6 interspace Odontoid fractures are classified in three types. Type I: fracture involving upper part of odontoid (rare); Type II: fracture at base of odontoid (unstable); Type III: fracture thru base and into body of axis (unstable though best prognosis for healing). Hangman's fracture - anterior subluxation of C2 through pedicles |
|
|
|
Most likely associated with a neurological deficit:
a) Fracture of the anterior and posterior arches of C1 b) Fracture of the lateral masses of C1 c) Hangman’s fracture d) Atlanto-occipital dissociation e) Fracture of the lamina of C3 f) Fracture of the odontoid |
Atlanto-occipital dissociation
Atlanto-occipital disassocation is usually fatal a hyperflexion injury craniocervical prevertebral soft tissue swelling, displacement of the occipital condyles relative to the lateral masses of C1, and displacement of the clivus |
|
|
|
All are associated with atlanto-axial subluxation EXCEPT:
a. Down's syndrome b. Spondyloepiphyseal dysplasia c. Trauma d. Hypothyroidism e. Juvenile rheumatoid arthritis (JRA) f. Morquio syndrome |
Hypothyroidism (NOT associated)
Associations with atlantoaxial subluxation: “JAMPCLAIRD” JRA, Ankylosis Spondylitis, Morquio syndrome, Psoriasis, Congenital Lupus, Accident, Infection (head and neck), Retropharyngeal abcess/Reiter’s/Rheumatoid, Down’s syndrome |
|
|
|
What cervical spine injury involves an exclusive hyperflexion mechanism?
a. Jefferson fracture b. Pillar fracture c. Hangman fracture d. Anterior subluxation e. Unilateral locked facet |
Anterior subluxation
Anterior subluxation ("hyperflexion sprain"): posterior ligament complex disrupted XR: localized kyphosis, widened interspinous/interlaminar space, widened disk space posteriorly Jefferson fracture: compression or hyperextension injury. Unilateral locked facet: flexion/rotation injury. Pillar fracture: hyperextension and rotation. Posterior arch of C1. Hangman's: fracture of both pedicles (pars) of C2, anterior subluxation of C2, hyperextension |
|
|
|
What cervical spine injury involves an exclusively hyperextension mechanism?
a. Jefferson fracture b. Flexion teardrop fracture c. Hangman’s fracture d. UIDx |
Hangman's fracture
Extension – Hangman’s; posterior arch C1 fx (posterior neural arch fracture); Extension teardrop Extension-rotation - Pillar Flexion - Bilateral facet dislocation, Wedge, Flexion teardrop, Clay shoveler’s, atlanto-occipital dissociation Flexion-Rotation – Unilateral facet dislocation, Compression – Jefferson fracture; Burst Complex—Odontoid; AOD |
|
|
|
Anterior longitudinal ligament discupted in which?
a. Pillar fracture b. Jefferson fracture c. Hangman fracture d. Unilateral locked facet e. Hyperflexion avulsion injury |
Hangman's fracture
Hangman's fracture: avulsion of the anteroinferior corner of C2 (bilateral pedicle fracture of C2) vertebral body (rupture of the anterior longitudinal ligament); caused by anterior subluxation of C2 on C3. Note that a hyperflexion avulsion injury would involve the posterior longitudinal ligament. You definitely get a tear of the ALL with extension teardrop (it’s the ALL that pulls off the teardrop bone avulsion) |
|
|
|
Trauma patient presents with conductive hearing loss and ipsilateral facial nerve (CN VII) palsy. This is most likely secondary to:
a. glomus tympanicum b. glomus jugulare c. meningioma at the cerebellar pontine angle d. transverse temporal bone fracture e. longitudinal temporal bone fracture |
Longitudinal temporal bone fracture
Longitudinal temporal bone fractures (middle ear fractures) are more frequent than transverse temporal bone fractures (80% vs 20%). The ossicles are involved (usually incus) which results in conductive hearing loss (no sensorineural hearing loss). Facial paralysis occurs in 20%. The tympanic membrane is involved, but the labyrinth is spared. Transverse temporal bone fractures (inner ear fractures) involve the labyrinth which results in vertigo and sensorineural hearing loss. The tympanic membrane is spared, but facial paralysis occurs in 50%. The most common non-traumatic cause of facial nerve paralysis AND hearing loss is a CPA tumor (acoustic neuroma, meningioma, epidermoid) However, the hearing loss will include both conductive and sensorineural elements. |
|
|
|
Which statement is FALSE regarding the position of the facial nerve in the IAC?
a. Anterior to the vestibular nerve b. Above the crista falciformis c. Below the crista falciformis d. Superior to the cochlear nerve e. Is located anterior-superior to the IAC f. Innervates taste in anterior 2/3 of tongue g. Exists through stylomastoid foramen h. Normally enhances on MRI with gadolinium |
Below the crista falciformis (FALSE)
The facial nerve runs in the anterior superior portion of the IAC, therefore superior to the crista falciformis, which divides the superior and inferior portions of the IAC. Taste from the anterior 2/3 of the tongue is carried by the corda typani a branch of the 7th cranial nerve The posterior 1/3 is supplied by cranial nerve IX. Enhancement in the IAC is always abnormal |
|
|
|
What is FALSE regarding the facial nerve?
a. superior to cochlear nerve b. can enhance on MR c. goes through stylomastoid foramen d. separates superficial and deep portions of parotid e. innervates post 2/3 of tongue |
: Innervates posterior 2/3 of tongue (FALSE)
Taste from the anterior 2/3 of the tongue is carried by the corda typani a branch of the 7th cranial nerve. The posterior 1/3 is supplied by cranial nerve IX. |
|
|
|
Brain MRI with a bleed that is bright on TI and dark on T2. Which phase of hemoglobin is it in?
a. oxyhemoglobin b. deoxyhemoglobin c. intracellular methemoglobin d. extracellular methemoglobin e. hemosiderin |
Intracellular methemoglobin
see chart on page 25, neuro |
|
|
|
Which of the following is the most likely cause of an enhancing suprasellar mass in a 1 year old?
a. Neuroblastoma metastasis b. Craniopharyngioma c. Pituitary adenoma d. Dysgerminoma |
Craniopharyngioma
Craniopharyngioma causes 50% of suprasellar tumors in children; most common suprasellar mass. Neuroblastoma is most common abdominal malignancy in the newborn but metastases to the brain are most often dural. Pituitary macroadenomas and some microadenomas enhance Dysgerminomas enhance strongly, and are the most common pineal tumor, although only 20% occur in the suprasellar region. |
|
|
|
NOT associated with Dyke Davidoff Mason?
a. unilateral cerebral atrophy b. unilateral (ipsilateral) calvarial thickening c. hyperpneumatization of the ipsilateral mastoids d. ipsilateral ventricle enlarged e. ipsilateral paranasal sinus hypoplasia |
Ipsilateral paranasal sinus hypoplasia (NOT associated)
Unilateral cerebral atrophy with homolateral hypertrophy of the skull and sinuses, compensatory enlargement of adjacent ventricle + sulci with midline shift. Insult to immature brain unilateral overdevelopment of sinuses |
|
|
|
Absolute contraindications to brain MR:
a. prosthetic hip b. CABG in past 7 days c. metallic surgical sutures d. cochlear implant e. Starr Edwards prosthetic valve (post 6000 series) f. metallic foreign body in the orbit |
Metallic foreign body in the orbit
Contraindications to MRI: ferromagnetic material in critical locations (e.g., within or behind the globe); pacemakers, internal defibrillators, thalamic/neural stimulators; temporary pacing wires, ferromagnetic aneurysm clips certain cochlear implants (Med-El model) have safely undergone scanning Usually safe to scan: Internal orthopedic hardware, surgical clips/wires/sutures/mesh; diaphragms, IUD’s, penile prostheses; intravascular stents, coils, filters (but generally wait 6 weeks if ferromagnetic); metal cardiac valves. |
|
|
|
TRUE regarding branchial cleft cysts:
a. usually type 1 b. at angle of mandible c. present at 5-10 yrs d. usually present as painful mass e. multiloculated |
At angle of mandible
Commonly presents as a solitary, painless mass in the neck of a child/young adult. History of intermittent swelling and tenderness during upper respiratory tract infection. Type II (most common, 95%): from 2nd branchial cleft, anterior triangle, angle of mandible; young to middle-aged adult, presents as multiparotid abscesses unresponsive to drainage or abx; cystic oval or round mass; insinuates between ICA and ECA (pathognomonic). |
|
|
|
Match following with their CT appearance:
1. Huntington's chorea 2. Wernicke’s encephalopathy 3. Dilantin therapy 4. Alzheimer’s disease 5. Mesial temporal sclerosis a. Atrophy of the caudate nucleus b. Mamillary bodies c. Cerebellar atrophy d. Cerebral atrophy e. Ammon’s horn |
1. A: Huntington’s chorea - basal ganglia atrophy
2. B: Wernicke’s encephalopathy - thiamine deficiency, medial thalami, mamillary bodies 3. C: Dilantin therapy - cerebellar atrophy (also with ETOH) 4. D: Alzheimer's disease - diffuse cerebral atrophy 5. E: Mesial temporal sclerosis--hippocampal disorder, dentate gyrus, Ammon’s horn |
|
|
|
The signal intensity of vertebral bodies on T1 weighted images is best described as?
A Isointense to the spinal cord B Hypointense to CSF C Hypointense to intervertebral discs D Isointense to intervertebral discs E Hyperintense to intervertebral discs |
Hyperintense to intervertebral discs
T1 of vertebral bodies is high because of fatty marrow, the nucleus pulposis is of relative low T1 signal intensity because it is hydrated. Tumor replacement of the fatty bone marrow is low signal intensity |
|
|
|
A vertebral hemangioma most commonly will have which pattern of signal intensity?
A Dark on both T1 and T2 B Bright on both T1 and T2 C Dark on T1 and bright on T2 D Bright on T1 and dark on T2 |
Bright on both T1 and T2
|
|
|
|
23-year-old patient presents with headache for 6 weeks, blurry vision, vomiting without nausea. Bilateral papilledema and mild truncal ataxia. Which imaging findings is consistent with history?
A Multiple infarcts B Massive subarachnoid hemorrhage C Obstructive hydrocephalus D Low CT attenuation in periventricular white matter |
Obstructive hydrocephalus
Colloid cysts are smooth spheric cysts third to fifth decade location is nearly constant in the anterior portion of the third ventricle |
|
|
|
Which of the following is true regarding post-traumatic vertebral body w/ Gibbus deformity:
a. Progressive increased density of remaining vertebral body b. Osteophyte formation c. Involvement of superior and inferior endplates d. Changes are seen in adjacent intervertebral disc e. Neurologic compromise |
Progressive increased density of remaining vertebral body
Gibbus is angular kyphotic deformity. Due to very compressed vertebral body, it would appear dense. |
|
|
|
Pediatric skull: which would you NOT see wormian bones in?
a. Pyknodysostosis b. Rickets c. Chiari II malformation d. Downs syndrome |
Chiari II malformation (NOT associated)
Chiari II: characteristic skull finding is Lückenschädel. Wormian bones are intrasutural ossicles in lambdoid, posterior sagittal, temporosquamosal sutures. Normal up to 6 months of age. Mnemonic: PORK CHOPS I: Pyknodysostosis, Osteogenesis Imperfecta, Rickets in healing phase, Kinky hair syndrome, Cleidocranial dysostosis, Hypothyroidism / Hypophosphatasia, Otopalatodigital syndrome, Primary acroosteolysis, Pachydermoperiostosis/Progeria, Syndrome of Down, Idiopathic |
|
|
|
Cystic area is seen peripheral to the thalamus in a neonatal US. The likely cause is:
a. infection b. post hemorrhage c. anoxia |
Post hemorrhage
Subependymal hemorrhage, germinal matrix hemorrhage, and grade I intraventricular hemorrhage, are all terms that refer to bleeding confined to the germinal matrix areas without intraventricular extension. |
|
|
|
Carotid-cavernous fistula on angiogram (T/F):
1. Reversal of flow in the ophthalmic vein 2. Early filling of the sagittal sinus 3. Filling of the contralateral cavernous sinus 4. Contralateral MCA injection will have cross-filling of the ipsilateral ACA across the ACOM 5. Early draining at the vein of Galen |
1-T, 2-F, 3-T, 4-T, 5-F
CCF represents abnormal communication between the veins of the cavernous sinus and the internal carotid artery. 1. True. There will be retrograde filling in the ophthalmic vein and any other veins that drain into the cavernous sinus, including the opposite cavernous sinus through the intercavernous sinus. 2., 5. False. The superior sagittal sinus nor the vein of Galen should not fill early as they do not communicate with the cavernous sinus until the level of the transverse sinus 3. True. Basically, everything that communicates with the cavernous sinus involved will attempt to decompress the fistulous blood. 4. True. Contralateral ICA injection is useful in determining extent of collateral flow |
|
|
|
What is a ranula?
a) branchial cleft cyst b) submandibular gland c) blockage of the submandibular gland |
Cystic lesion due to obstruction of the sublingual gland duct
Ranula's wall usually enhances |
|

