![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
29 Cards in this Set
- Front
- Back
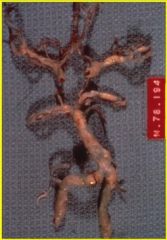
what pathology is this showing?
|
circle of willis with atherosclerosis (lipid in the wall of blood vessels)You get narrowing of lumen and eventually may get occlusion. A thrombus may form. Or develop emboli, which break off and clog up blood vessels down the line.
|
|
|
what is the major cause of ischemic stroke?
|
Atherosclerosis is Most common cause of stroke. Can be intracranial or extracrainial (in the bifurcation of carotid into int and ext. any branch point in a vessel is where you have turbulent flow and can get atherosclerosis.)
|
|

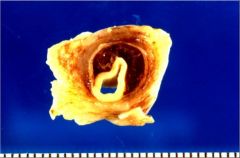
what is this? what is its pathogenesis?
|
this is a carotid endarterectomy showing atherosclerosis with complicated plaques. There is gradual encroachment of plaque. For most of its life, it lives beneath endolthelium. On a random day, it breaches the endothelium and then coagulation starts. Once this happens you can have occlusions or emboli. When you get atherosclerosis with breaching of the endothelium, this iscalled a “complicated plaque”
note: Carotid endarterectomy (CEA) is a surgical procedure used to prevent stroke, by correcting stenosis in the carotid artery. Endarterectomy is the removal of material on the inside (end-) of an artery. |
|
what pathology is this showing?
|
carotid dissection with accumulation in the adventitia. this squashes blood flow and can eventually lead to stroke
|
|
|
what is a "watershed" infarct?
|
area in the junctions of major arterial supply zones that have reduced pressure of perfusion bw the distal portions of arterial supply when there's low BP. classic borderzone is bw anterior and middle cerebral arteries distal territories
- causes weakness of shoulder/hip > leg/upper limb |
|

what is shown here?
|
global hypoperfusion = when the ischmic injury is severe enough to cause cortical atrophy of neuron containing structures like BASAL GANGLIA and causes HYDROCEPHALUS EX VACUO
|
|
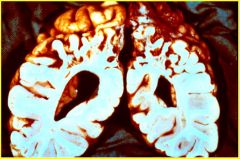
what is imaged here?
|
borderzone infarct in the parietal region. bilateral "man in a barrel" with arms. this can follow prolonged cardiac bypass or cardiac arrest.
|
|
|
what are the consequences of global ischemia?
|
if brief (minutes) = pt's neurological fxns may be restored with transient confusion
more severe injury may lead to dementia spasticity if protracted ischemia = pt may go into coma and be in persistent vegetative state |
|

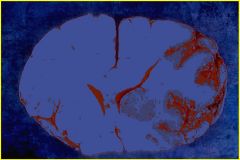
what's being shown here?
|
relative watershed; showing that the surface is better perfused than the depths. if a person experiences hypoperfusion, you will see bigger changes in the depths of the sulci (darker than normal tissue).
|
|
|
certain cell populations are more vulnerable to ischemic injury with ____>>____>>____. what are the 3 most sensitive populations?
|
neurons>>glia>>endothelium
3 most sensitive: 1. purkinje cells of cerebellum 2. large neurons in Sommer's sector of hippocampus (CA1) 3. middle layers of cerebral cortex - Laminar necrosis |
|
|
name the most sensitive portion of the hippocampus
|
pyrimidal neurons of CA1 - Sommer's sector
|
|

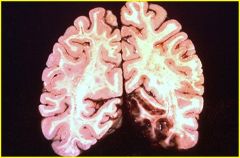
what pathology is being shown here?
|
global hypoperfusion in the brain leading to ischemia of hippocampus (CA1-Sommer's sector) due to selective vulnerability
|
|
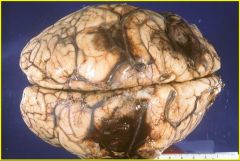
what pathology is shown here? what clinical sx's will result from such an event?
|
acute middle cerebral artery infarct with discoloration in MCA territory, squashing of the ventricles and cingulate herniation.
clinically, pt will have hemiparesis of contra face/upper limbs, sensory deficit in arms/face, with contra homonymous hemianopsia |
|
what pathology is shown here? how would this show up clinically?
|
posterior cerebral artery infarct; could occur from emboli/thrombus
-pt would have difficulty recognizing faces (ventral "what" stream compromised) with hemianopsia |
|
|
what is the pathological evolution of cerebral infarcts?
|
A dead neuron is a red neuron. Cytoplasm becomes eosinophilic and without contents. If you allow 6-8 hrs after hypoperfusion of brain, you’ll start to see this.
By day 2: perfusion will be restored by fibrillogeneis. Macrophages will come in and start cleaning up the mess. There’s not BBB, but still have vascular proliferation. Dead tissue is cleared out by macrophages. After months: cystic cavity from all the dead tissue being cleared out by macrophages |
|
what is the earliest light microscopic change in an infarct in brain tissue?
|
red neurons
|
|

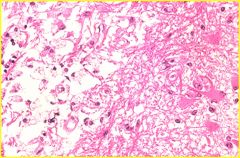
what pathology is shown here?
|
Remote MCA infarct. After macrophages cleared out tissue. This is the MCA infarct 6 months later. All the dead tissue is cleared out. Theres compensatory enlargement of the ventricles. There used to be neurons here…now theyr/e gone. So their axons are going to degenerate. If you look at cerebral peduncles and other parts of the brain grossly, you’ll see that they’re gone
|
|
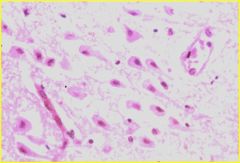
what is this? what is the difference bw left and right side of picture?
|
this is wall of remote infarct cavity.
Foamy macrophages on left. Glial cells on the right forming glial scar on the wall of infarct. |
|

what pathology is shown here?
|
left: atrophy of cerebral peduncle on the left
right: atrophy of medullary pyramid on left of brain stem BOTH FOLLOWING MCA INFARCT |
|

What pathology is shown here? how will this show up clinically?
|
remote pontine infarct in the CST/CBT area. this will lead to contra weakness, contra DC findings
|
|
what is going on with this brain?!?!
|
multiple hemorrhagic embolic infarcts. when you see multiple hemorrhagic strokes in varying vascular territories, you need to think EMBOLI!! (ie. emboli from the heart)
|
|
|
define CNS/systemic vasculitis. what is the one thing you must have in order to classify pathology as such?
|
vessels become inflammed themselves either systemically or witihn the wall of hte brain.
- inflammatory infiltrate MUST involve entire thickness of vessel wall (transmural inflammation)!! - when you see multifocal stroke, think about emboli or vasculitis! |
|

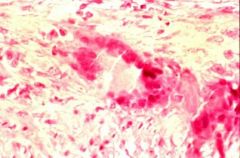
what is this?
|
vasculitis
REMEMBER IT MUST HAVE TRANSMURAL INFLAMMATION!!! aka... the inflammatory infiltrate must involve the entire thickness of the vessel wall |
|
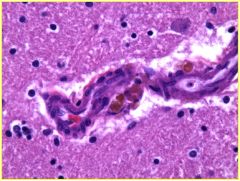
what is this?
|
granulomatous vasculitis; showing giant cell
|
|

what pathology is shown here? how did this happen? what are the Sx's?
|
this is a lacunar infarct that resulted from long standing hypertension which caused small, perforating vessels to become thick-walled...thus leading to ischemia.
Sx's depend on where infarct occurs |
|
what is this?
|
Microaneurysm = when there’s a pocket that forms from increased pressure (hypertension) and then it breaks to give a hypertensive intracerebral hemorrhage
|
|
|
what is the time frame in which you can give pt TPA for thrombolysis if there's a sudden onstem of thrombotic stroke? what is the other pre-requisite for administering TPA?
|
under 3 hours!
- this Tx can lead to recovery!! PATIENT CANNOT HAVE HAD A HEMORRHAGIC STROKE IN THE HEAD...so you have to get CT scan to check. |
|
|
besides administering TPA to a pt that just underwent thrombotic stroke, what else do you do (or not do)?
|
- do not allow hypotension
- protect airway if consciousness decreased - DVT (deep vein thrombosis) with low dose heparin so they won't get a pulmonary embolus down the line - anti-platelet (baby aspirin) |
|
|
what do you do for a pt with an embolic stroke? (2)
|
- remove source (if possible)
- consider anti-coaguulation (warfarin/heparin) try to give anti-coagulant to prevent the formation of new emboli... |

