![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
572 Cards in this Set
- Front
- Back
|
In infant development, which comes first: bilaterality or unilaterality?
|
__________ precedes unilaterality in infant development
|
|
|
When does hand dominance begin to develop?
|
Hand dominance begins to develop at 3 to 6 years, and is not fully defined until 6 years
|
|
|
Can someone with receptive aphasia participate in sensory testing?
|
Individuals with this disorder cannot comprehend spoken or written words or symbols. Individuals cannot understand verbal directions or respond to sensory stimuli.
|
|
|
What is agnosia?
|
Agnosia is a category of defecits where the patient lacks recognition of familiar object as perceived by the senses. This could involve all the senses and manifests with problems in body scheme, such as somatognosia and anosognosia.
|
|
|
What is somatognosia?
|
Lack of awareness of one's body parts.
|
|
|
What is anosognosia?
|
Anosognosia: Transient, severe form of neglect. Patient does not recognize the presence or severity of his paralysis.
|
|
|
What is prosopagnosia?
|
Face blindness. Inability to identify an individual by their face.
|
|
|
What is visual-spacial agnosia?
|
Affects perception of spatial relationship between objects, or between objects and self.
|
|
|
What is auditory agnosia?
|
Inability to recognize sounds, words and non-words.
|
|
|
What is visual agnosia?
|
Lack of ability to recognize common objects and demonstrate their use in an activity.
|
|
|
What is apraxia?
|
Loss of the ability to execute or carry out learned (familiar) movements, despite having the desire and the physical ability to perform the movements
|
|
|
What is ideomotor apraxia?
|
Inability to imitate gestures or perform a purposeful motor task on command, even though the patient is able to fully understand the idea or concept of a task. This is often associated with left hemisphere damage.
|
|
|
What is ideational apraxia?
|
The disability of carrying out complex sequential motor acts. Caused by a disruption of the conception, rather than execution. (Loss of tool function knowledge)
|
|
|
What is constructional apraxia?
|
Unable to produce designs in 2 or three dimensions by copying, drawing, or constructing.
|
|
|
What is oral apraxia?
|
Difficulty in forming and organizing intelligable words, though the musculature required to do so is in tact. Differs from disarthria because no muscles are affected and speech is not slurred.
|
|
|
What is a neuroma?
|
A ______ is an unorganized mass of nerve fibers resulting from a laceration (either surgical or accidental) or amputation in which the nerve regrows in unorganized bundles. Results in sharp, radiating pain.
|
|
|
By what age does an infant sit erect and unsupported for several minutes?
|
By 8 to 9 months, an infant can sit erect and unsupported.
|
|
|
What is reflex sympathetic dystrophy?
|
__________ is caused by trauma, post-surgical inflammation, infection, or laceration to an extremity. Characterized by pain, edema, shiny skin, blotchy skin, and excessive sweating or dryness.
|
|
|
What is another name for reflex sympathetic dystrophy?
|
Complex regional pain syndrome.
|
|
|
What is a symmetric tonic neck reflex?
|
When an infant's neck is extended, the elbows extend and the hips flex. When the head is lowered, the elbows flex and the hips extend.
|
|
|
What is a bunny hop pattern?
|
A bunny hop pattern is a result of symmetric tonic neck reflex utilization in order to elicit movement at the hips and elbows for mobility.
|
|
|
What is a neuroma?
|
A complication of nerve structure or amputation. A traumatic ______ is an unorganized mass of nerve fibers resulting from accidental or surgical cutting of the nerve. Results in sharp, radiating pain.
|
|
|
What sensory region does the radial nerve innervate on the hand?
|
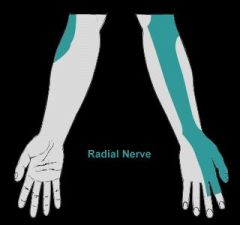
Radial Nerve
|
|
|
What sensory region does the ulnar nerve innervate in the hand?
|
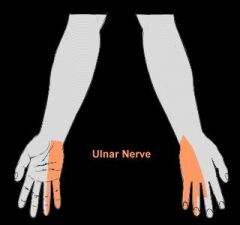
See image.
|
|
|
What sensory region in the hand is innervated by the median nerve?
|
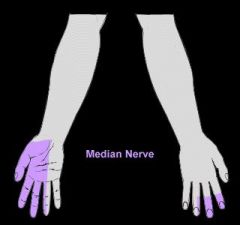
Median Nerve
|
|
|
What stage is initiated by looking at and reaching for food?
|
The oral preparatory phase.
|
|
|
What behavior would a child with poor modulation of tactile input display?
|
Children with autism often are unpredictable, both craving and avoiding sensory stimuli at various times.
|
|
|
After swallowing a pureed substance, you notice the individual has a wet, gurgling voice. What might this indicate?
|
Possible aspiration. A videoflouroscopy is often times needed to determine is this is the case.
|
|
|
In an acute care psychiatric setting, which group treatment is the most appropriate for individuals with disorganized psychosis?
|
Directive group treatment: a highly structured approach used in acute care for minimally functional individuals.
|
|
|
What type of group structure would be most appropriate for individuals with substance abuse?
|
A task group is appropriate for substance abuse disorders.
|
|
|
What group format is most appropriate for eating and adjustment disorders?
|
Psychoeducation groups
|
|
|
What is a Laissez-Faire leadership style?
|
Laissez-Faire is a "hands off" approach. Goals are not stated, the purpose is not clear, members are not discouraged or encouraged. This is for a high-functioning group.
|
|
|
What is the optimum number of members for a therapy group?
|
Five to six.
|
|
|
What is the optimum number of members for a counseling group?
|
No more than eight members.
|
|
|
What would you do if you had ten people assigned to your group?
|
Divide them into two subgroups.
|
|
|
What is autocratic leadership?
|
The leader exerts complete control.
|
|
|
What is democratic leadership?
|
This style can be a problem-solving style.
Group members feel safe to express views, thoughts, and feelings. |
|
|
According to the OT code of ethics, what is defined as beneficence?
|
Concern for the safety and well-being of the recipients of OT services.
|
|
|
According to the OT code of ethics, what is defined as nonmaleficence?
|
Ensure recipient’s safety and do no harm.
|
|
|
According to the OT code of ethics, what is defined as autonomy?
|
Respect patient rights, including confidentiality.
|
|
|
According to the OT code of ethics, what is defined as procedural justice?
|
Comply with laws
|
|
|
According to the OT code of ethics, what is defined as veracity?
|
Providing accurate information when representing the profession (don't lie)
|
|
|
According to the OT code of ethics, what is defined as duty?
|
Maintain credentials and continually learn craft
|
|
|
According to the OT code of ethics, what is defined as fidelity?
|
Treat colleagues and other professionals with respect, fairness, and integrity.
|
|
|
What are the normal ROM limits of cervical flexion, extension, and lateral flexion?
|
0-45 degrees
|
|
|
What are the normal ROM limits of cervical rotation?
|
0-60 degrees
|
|
|
What are the normal ROM limits of thoracic and lumbar spine flexion?
|
0-80 degrees
|
|
|
What are the normal ROM limits of thoracic and lumbar spine extension?
|
0-30 degrees
|
|
|
What are the normal ROM limits of lateral flexion of the spine?
|
0-40 degrees
|
|
|
What are the normal ROM limits of rotation of the spine?
|
0-45 degrees
|
|
|
What are the normal ROM limits of shoulder flexion?
|
0-170 degrees
|
|
|
What are the normal ROM limits of shoulder extension?
|
0-60 degrees
|
|
|
What are the normal ROM limits of shoulder abduction?
|
0-170 degrees
|
|
|
What are the normal ROM limits of shoulder adduction?
|
0 degrees
|
|
|
What are the normal ROM limits of horizontal adduction?
|
0-130 degrees
|
|
|
What are the normal ROM limits of horizontal abduction?
|
0-40 degrees
|
|
|
What are the normal ROM limits of shoulder internal rotation?
|
0-70 degrees in shd abduction
0-60 degrees in shd adduction |
|
|
What are the normal ROM limits of shoulder external rotation?
|
0-90 degrees in shd abduction
0-80 degrees in shd adduction |
|
|
What are the normal ROM limits of elbow flexion?
|
0-140 degrees
|
|
|
What are the normal ROM limits of elbow extension?
|
0 degrees
|
|
|
What are the normal ROM limits for pronation and supination?
|
0-80/90 degrees
|
|
|
What are precautions of neuroleptic medications?
|
Power tools and sharp instruments should be avoided, and sun exposure should be limited.
|
|
|
What is extrapyramidal syndrome?
|
Extrapyramidal syndrome is a neurological side effect of anti-psychotic medication that mimics the effects of Parkinson's disease. This can cause rigidity, bradykinesia, cogwheel and leadpipe rigidity, loss of postural mechanisms, and a resting, pill-rolling tremor.
|
|
|
What is tardive dyskinesia?
|
Tardive dyskinesia is a neurological syndrome caused by the long-term use of neuroleptic drugs. Tardive dyskinesia is characterized by repetitive, involuntary, purposeless movements. Features of the disorder may include grimacing, tongue protrusion, lip smacking, puckering and pursing, and rapid eye blinking. Involuntary movements of the fingers may appear as though the individual is playing an invisible guitar or piano.
|
|
|
What is ataxia?
|
______ describes a lack of coordination while performing voluntary movements. It may appear as clumsiness, inaccuracy, or instability.
|
|
|
What is bradykinesia?
|
Bradykinesia means "slow movement."
|
|
|
What is choreoathetosis?
|
____________ is a movement of intermediate speed, fluctuating between the quick, flitting movements of chorea and the slower, writhing movements of athetosis.
|
|
|
What is dystonia?
|
________ is a neurologic movement disorder characterized by sustained muscle contractions, usually producing twisting and repetitive movements or abnormal postures or positions.
|
|
|
What is Huntington's Disease?
|
The classic signs of HD include the development of chorea–or involuntary, rapid, irregular, jerky movements that may affect the face, arms, legs, or trunk–as well as the gradual loss of thought processing and acquired intellectual abilities (dementia).
|
|
|
What is adiadochokinesis?
|
The inability to perform rapid alternating movements such as pronation/supination.
|
|
|
What is dysmetria?
|
Dysmetria is the inability to estimate the ROM necessary to meet the target. Evident when the individual tries to touch the nose.
|
|
|
What is nystagmus?
|
Involuntary movement of the eyeballs in an up/down, back/forth motion. Interferes with head control.
|
|
|
What is dysarthria?
|
Explosive or slurred speech caused by incoordination of muscles involved in speech. Classified as a neuromotor problem.
|
|
|
What is ballism?
|
Rare symptom that is produced by continuous, abrupt contractions of the axial and proximal musculature of the extremity.
|
|
|
What are intention tremors?
|
Occurs during voluntary movement. Intensified at the termination of the movement and often associated with MS.
|
|
|
What are resting tremors?
|
Occurs at rest and subsides when voluntary movement is attempted.
Seen in Parkinson's disease. |
|
|
What is the first level of OT intervention?
|
Adjunctive methods. These are preliminary to the use of purposeful activities and may include exercise, facilitation and inhibition techniques, positioning, sensory stim, PAMs, and splints.
-OTs evaluate performance components (innate abilities) |
|
|
What is the second stage of OT intervention?
|
Enabling activities. May not yet be considered purposeful activities, but are steps toward performance of purposeful activities.
-Performance components and areas (Dressing using adaptive equipment) |
|
|
What is stage three of OT intervention?
|
Purposeful activities: Evaulate performance areas. Have inherent, autonomous goals and are relevant and meaningful to the patient, such as ADLs, IADLs, etc. Used to evaluate, facilitate, restore or maintain a person's ability to function in life roles. Can the person cook or work in a clinical setting?
|
|
|
What is stage four of OT treatment?
|
Occupations. The highest stage of treatment continuum engages the patient in natural occupations in their living environment and the community. Not all patients can achieve this stage.
|
|
|
What is the rehabilitation model?
|
The rehabilitation model goal is to help the patient learn to work arond or compensate for physical, cognitive, or perceptual limitations.
|
|
|
What is a FIM level of "Total Assistance," or level 1?
|
The person puts forth less than 25% of the effort necessary to do a task.
|
|
|
What is a FIM level of "Maximal Assistance," or level 2?
|
The person puts forth less than 50% of the effort necessary to do a task, but at least 25%
|
|
|
What is a FIM level of "Moderate Assistance," or level 3?
|
The person puts forth between 50% and 75% of the effort necessary to do a task, and requires no more than helping or touching.
|
|
|
What is a FIM level of "Minimal Contact Assistance," or level 4?
|
The person puts forth 75% or more of the effort necessary to do a task, and requires no more help than touching.
|
|
|
What is a FIM level of "Supervision or setup," or level 5?
|
The person only needs someone to standby and cue or coax him/her (without physical contact) so that he/she can do a task.
|
|
|
What is a FIM level of "Modified Independence," or level 6?
|
No helper is needed and the person needs an assistive device. This score can also be obtained when no help is needed but the person takes considerable time to do a task or may complete the task in an unsafe manner.
|
|
|
What is a FIM level of "Total independence," or level 7?
|
No helper is needed and the person performs the task safely, within a reasonable amount of time, and without assistive devices, aids, or changes.
|
|
|
What FIMS score would be given to a person who needs a helper to set up items or assistive devices?
|
A score of "5" or "Supervision or setup" can be obtained if a helper is needed to set up items or assistive devices for the person.
|
|
|
How tall should a door threshold be for wheelchair accessibility?
|
1/2" and should be bevelled-- should be removed if possible.
|
|
|
What is the standard height of a wheelchair seat?
|
18". Toilets are typically 15" and should be raised to accommodate transfers.
|
|
|
What is the minimum doorway width for a wheelchair?
|
32"
|
|
|
What is the National Alliance for the Mentally Ill?
|
Provides support groups open to clients & families with a focus on education and support for mental illness.
|
|
|
Which sensations return FIRST following a nerve injury?
|
Pain and temperature
|
|
|
What is occupational performance?
|
Ability to carry out ADLs. Evaluation looks at activity demands, client factors and environment.
|
|
|
What food consistency is most difficult to swallow?
|
Foods that have liquid and solid consistencies are hardest to chew and swallow.
|
|
|
In mental health, planning for discharge involves evaluating what?
|
Occupational performance
|
|
|
What is AC MRDD?
|
Accredidation Council for Services for Mentally Retarded and Developmentally Disabled
|
|
|
What is spinal shock?
|
Transient physiological reaction to depression of the cord below the SCI level. Associated loss of sensorimotor function and flaccid paralysis. Flaccid paralysis symptoms last several days.
|
|
|
What is functional skill training?
|
Focuses on mastery of a specific task. Requires client to repeatedly practice the substeps of a task with the # of cues for each task gradually faded out.
|
|
|
What is anterior cord syndrome?
|

Often associated with a lesion causing variable loss of motor and sensation function. Proprioception preserved.
|
|
|
When should continuous reinforcement be utilized?
|
When teaching new skills.
|
|
|
When should intermittant reinforcement be utilized?
|
When maintaining a behavior.
|
|
|
What is central cord syndrome?
|

Central injury to cervical spinal cord resulting in greater weakness in UEs than in LEs.
|
|
|
What is conus medullaris syndrome?
|
Assoc. with injury to the sacral cord and lumbar nerve roots. Patients present with areflexic bladder, bowel, and lower limbs. Sacral segments sometimes show preserved reflexes.
|
|
|
What is cauda equina syndrome?
|

Due to injury of lumbosacral nerve roots in spinal canal. Leads to areflexic bladder, bowel, and lower limbs.
|
|
|
What is Brown-Sequard syndrome?
|

A hemisection lesion of the cord resulting in ipsilateral motor loss and contralateral loss of sensitivity to pain and temp.
|
|
|
What is parasthesia?
|
Sensation of tingling, itching, numbness or burning caused by sustained nerve pressure or reduced blood flow.
|
|
|
What are the muscles of the rotator cuff?
|
Supraspinatus
Infraspinatus Subscapularis Teres Minor |
|
|
Should you pass a Level II fieldwork student if they are functioning below the minimal entry level?
|
Students functioning below entry level should be failed.
|
|
|
What is "close supervision" defined as?
|
Close supervision is defined as "daily, direct contact at the site of work"
|
|
|
What is a program evaluation?
|
A program evaluation is the compilation of the intervention results for a population of individuals.
|
|
|
What is Durable Medical Equipment (DME)?
|
Items that can withstand repeated use, such as a wheelchair, medical bed, and walkers.
|
|
|
Is a shower chair considered a DME?
|
Adaptive equipment is not covered under Medicare as a DME. Items not included are shower chairs, reachers, hand-held showers.
|
|
|
What are the main goals of work hardening?
|
To return the individual to work. Focus on pain management and proper body mechanics is key.
|
|
|
Allen Cognitive Scale
(External link) |
See http://www.flashcardexchange.com/flashcards/list/362121
|
|
|
Group Development
(External Link) |
http://www.flashcardexchange.com/flashcards/list/362658
|
|
|
Developmental Levels of Grasping
(External Link) |
http://www.flashcardexchange.com/flashcards/view/362966
|
|
|
Human Development and Aging
(External Link) |
http://www.flashcardexchange.com/flashcards/view/361913
|
|
|
Human Development Part 2
(External Link) |
http://www.flashcardexchange.com/flashcards/view/361728
|
|
|
In Hand Manipulation Skills
(External Link) |
http://www.flashcardexchange.com/flashcards/view/362983
|
|
|
Medicare Guidelines
(External Link) |
http://www.flashcardexchange.com/flashcards/view/363383
|
|
|
Rancho Los Amigos Cognitive Scale
(External Link) |
http://www.flashcardexchange.com/flashcards/view/362940
|
|
|
Spinal Cord Injury
(External Link) |
http://www.flashcardexchange.com/flashcards/view/362128
|
|
|
Splints
(External Link) |
http://www.flashcardexchange.com/flashcards/view/362646
|
|
|
Teaching Methods Occupational Therapy
(External Link) |
http://www.flashcardexchange.com/flashcards/view/362651
|
|
|
Types of Groups and Appropriate Clients
(External Link) |
http://www.flashcardexchange.com/flashcards/view/362952
|
|
|
What functionality does a person with C1-C3 SCI have?
|
-Individuals required to use a respirator
-Individuals might have limited head and neck movement -Able to use "sip and puff" wheelchair -Completely dependendent in ADLs and transfers |
|
|
What functionality does a person with C4 SCI have?
|
-Person has full mobility of the head and neck
-Able to breathe independently with low stamina -Complete body paralysis below neck -Possibility of autonomic dysreflexia -"Sip and puff" wheelchair required -Completely dependent in ADLs and transfers |
|
|
What functionality does a person with C5 SCI have?
|
-Good elbow flexion in order to self feed (with a mobile arm support)
-Supination available -No finger or wrist movement -Breathes independently with low stamina -Electric wheelchair may be used with hand control |
|
|
What functionality does a person with C6 SCI have?
|
-Complete paralysis of legs and torso.
-Able to extend wrist and flex the elbow. -Independent in transfers from toilet to wheelchair. -Able to reach forward. -Benefits from splint to promote wrist tenodesis. -Able to do some ADLs, such as shaving and dressing upper body. -Assistance may be required to dress lower body. -Needs assistance to transfer from bed to wheelchair. |
|
|
What functionality does a person with C7 SCI have?
|
-Elbow extension available
-Wrist flexion available -Finger extension available -Mod I feeding -Dress Mod I to min assist -Bathing & Grooming Mod I -Toileting Mod I -Transfers Independent |
|
|
What is Guillain-Barre syndrome?
|
An autoimmune disease in which the peripheral nerves become inflammed. Results in numbness and paralysis in the legs, upper body, and face. Level of independence depends on extent of paralysis.
|
|
|
What is the best way to obtain detailed information about an individual's job requirements?
|
By examing a job analysis. A job analysis is a detailed description of the physical, sensory, and psych demands of a job.
|
|
|
What postural stability must an individual demonstrate before being able to use a mobile arm support?
|
Lateral trunk stability
|
|
|
What is rotation?
|
A type of in-hand manipulation that is displayed when an individual turns a nut on a bolt.
|
|
|
What functionality does a person with C8-T1 SCI have?
|
-Full UE control, including fine coordination and grasp
-ADLs, mobility and communication are Mod I |
|
|
What functionality does a person with T6 SCI have?
|
-Increased endurance
-Larger respiratory reserve -Pectoral girdle stabilized for heavy lifting -ADLs Independent (No assistive devices) -Uses braces with great difficulty for ambulation |
|
|
What functionality does a person with T12 SCI have?
|
-Improved endurance and trunk control.
-ADLs and IADLs and independent -Mobility: Ambulates with long leg braces and crutches -Uses wheelchair for energy conservation |
|
|
What functionality does a person with L4 SCI have?
|
-Hip flexion and knee extension
-Independent in all activities plus ambulation -Bowel and bladder control is not voluntary |
|
|
What is Pes Valgus?
|

Pes Valgus (Pronated Foot)
|
|
|
What is pes varus?
|
Club foot (Supinated foot)
|
|
|
What is Ranchos Los Amigos Cognitive Scale Level I?
|
NO RESPONSE
Person does not respond to sounds, sights, touch or movement. |
|
|
What is Ranchos Los Amigos Cognitive Scale Level II?
|
GENERALIZED RESPONSE
-Begins to respond to sounds, sights, touch or movement -May open eyes, but does not focus on anything in paricular -Respond slowly, inconsistently, or after a delay -Responses may include chewing, sweating, breathing faster, increased BP, etc. |
|
|
What is Ranchos Los Amigos Cognitive Scale Level III?
|
LOCALIZED RESPONSE
-Patients begin to move their eyes and look at specific people and objects -Turn heads in the direction of loud voices of noise -Can follow simple commands, such as "Squeeze my hand" |
|
|
What is Ranchos Los Amigos Coma Scale Level IV?
|
CONFUSED AND AGITATED
-Patient is confused and agitated about where they are and what is hapening in the surrounding -At the slightest provocation, patient may become restless, agressive, or verbally abusive |
|
|
What is Ranchos Los Amigos Cognitive Scale Level V?
|
CONFUSED AND INAPPROPRIATE
-Patient is confused and does not make sense in conversations, but may be able to follow simple directions -May get upset when stressed, but agitation is no longer a major problem -Frustration as elements of memory may return |
|
|
What is Ranchos Los Amigos Cognitive Scale Level VI?
|
CONFUSED BUT APPROPRIATE
-Speech makes sense -Able to perform self care -Poor initiation and termination in activities -Learning difficult |
|
|
What is Ranchos Los Amigos Cognitive Scale Level VII?
|
AUTOMATIC APPROPRIATE
-Patients are usually coherent -ADLs independent -Difficulty remembering recent events and discussions -Difficulty with calculations, problem solving, judgment -Aware of deficits |
|
|
What is Ranchos Los Amigos Cognitive Scale Level VIII?
|
PURPOSEFUL AND APPROPRIATE
-Patients are independent and can process new information -Able to remember distant and recent events, and can figure out complex and simple problems |
|
|
At what Ranchos Los Amigos level do individuals begin to recognize family and friends?
|
Level III
|
|
|
At what Ranchos Los Amigos level do individuals begin to follow simple directions like "Squeeze my hand?" or "Look at me"?
|
Level III
|
|
|
At what Ranchos Los Amigos level do individuals begin to engage in simple, routine activities such as self feeding and dressing?
|
Level IV
|
|
|
At what Ranchos Los Amigos level do individuals begin to begin to remember events before the accident better than their daily routine?
|
Level V. At this level, patients also confabulate in order to fill in gaps in memory
|
|
|
An individual needs step-by-step instruction to perform self care. What Ranchos level are they at?
|
Level V
|
|
|
At what Ranchos level can a patient follow a schedule, but get confused by changes in the routine?
|
Level VI
|
|
|
You have a patient who is unable to step off of a curb or watch for cars. What Ranchos level are they at?
|
Level VI
|
|
|
At what Ranchos level can a patient pay attention for up to 30 minutes?
|
Level VI
|
|
|
At what Ranchos level are patients aware of the month and year?
|
Level VI
|
|
|
At what Ranchos level can an individual perform self care with minimal assist?
|
Level VI
|
|
|
At what Ranchos level is a patient independent in self care, but continues to need supervision because of safety awareness and judgment?
|
Level VII
|
|
|
At what Ranchos level is an individual ready for vocational and/or driving training?
|
Level VIII
|
|
|
What is retrograde amnesia?
|
Inability to remember events that occurred before the incidence of trauma or the onset of the disease that caused the amnesia
|
|
|
What is anterograde amnesia?
|
Inability to remember ongoing events after the incidence of trauma or the onset of the disease that caused the amnesia, but able to remember incidents that happened before the incident
|
|
|
What is the post-traumatic amnesia classification tool?
|
A classification tool used by clinicians to assess the severity of injury.
|
|
|
What is the Glasgow Coma Scale?
|
-A brain injury severity scale that assesses depth and duration of impaired consciousness and coma.
-Used by clinicians to gauge deterioration or improvement at the emergent and acute stages of brain damage or lesions. -Predicts ultimate functional outcome. |
|
|
What are the subtests of the Glasgow Coma Scale?
|
-Eye opening (E)
-Best Motor Response (M) -Best Verbal Response (V) -Minimum score of 1 in each subtest = 3 -Maximum score is 15 E+M+V=3-15 |
|
|
How is the Glasgow Coma Scale interpreted?
|
3-8: Severe injury (In a coma)
9-12: Moderate injury 13-15: Mild or no injury |
|
|
What are the brain behavioral characteristics of temporal lobe damage?
|
Temporal lobes contain auditory reception and visual processing areas. Damage to temporal lobes may affect:
-Sound discrimination -Voice Recognition -Language and Comprehension -Auditory and visual memory storage -Wernicke's Aphasia |
|
|
What are the brain behavioral characteristics of occipital lobe damage?
|
Occipital lobe contains visual reception areas. Damage can result in:
-Anopsia/quadrantanopsia -Object recognition and visual scanning deficits |
|
|
What are the brain behavioral characteristics of damage to the parietal lobe?
|
Contains reception areas for touch and body position. Damage includes deficits in:
-Sense of touch, proproception, temperature and pain -Disorganization -Distorted self perception |
|
|
What are the brain behavioral characteristics of damage to the frontal lobe?
|
The frontal lobes order information and sort out stimuli. Damage to the frontal lobe affects:
-Concentration and attention -Abstract thinking -Concept formation -Foresight -Problem solving -Broca's Aphasia |
|
|
What is Broca's Aphasia?
|
-Characterized by frontal lobe damage resulting in speech apraxia and agrammaticism
-The individual has good auditory comprehension, but reading and writing are severely affected |
|
|
What is Wernicke's Aphasia?
|
-Characterized by temporal lobe damage resulting in impaired auditory comprehension and feedback
-Have fluent, well-articulated paraphasic speech (word substitution errors) |
|
|
What are the behavioral charcteristics of damage to the thalamus?
|
-Communications relay station for all sensory information
-Damage can alter states of arousal, memory defect, speech deficits, apathy, and disorientation |
|
|
What are the behavioral characteristics of damage to the hypothalamus?
|
The hypothalamus regulates bodily functions such as thirst, hunger, body temperature, emotion, and circadian rhythm. Damage can result in:
-Uncontrolled eating or drinking -Mood alteration -Sleep disorder |
|
|
What are the behavioral charcteristics of damage to the cerebellum?
|
The cerebellum regulates balance, and posture. Damage can cause problems with:
-Fine motor control -Coordination |
|
|
What are the behavioral characteristics of damage to the reticular formation?
|
The reticular formation is in the core of the brainstem. Contains fibers en route to and from the brain. Damage to the reticular activitating system results in:
-Sleeping longer periods at a time |
|
|
What are the behavioral characteristics of damage to the limbic system?
|
Plays integral part in the expression of emotion. Damage can affect:
-Emotional behavior |
|
|
Of Broca's and Wernicke's, which is expressive and which is receptive aphasia?
|
-Broca's: Expressive Aphasia
-Wernicke's: Receptive Aphasia |
|
|
What can someone with an IQ range of 55-69 accomplish? What classification of MR is this?
|
Mild retardation:
-Social/verbal skills to 6th grade level -Able to take care of self |
|
|
What can someone with an IQ range of 40-54 accomplish? What classification of MR is this?
|
Moderate MR: 40-54:
-Can communicate & get vocational training -Can only do unskilled or semi-skilled work in sheltered workshops -Can handle routine daily functions -Can only learn up to a second-grade level -Require supervised living or group home |
|
|
What can someone with an IQ range of 25-39 accomplish? What classification of MR is this?
|
Severe Retardation:
-Learns to communicate through gestures and some words -Trained in basic health habits -Require supervised living or group home |
|
|
What can someone with an IQ range below 25 accomplish? What classification of MR is this?
|
Profound Retardation:
-Need caregiver assistance for basic survival skills -Often have neuromuscular, orthopedic, or behavioral deficits |
|
|
What falls under the umbrella of Pervasive Development Disorders (PDD)?
|
-Autism
-Asperger's Syndrome -Rett's Syndrome -PDD, not otherwise specified (Usually when autism is suspected, but not proven) |
|
|
What is autism?
|
Symptoms include:
-Impairments of social interaction, social communication, social behavior -Inability to relate to others -Echolalia -Flat affect and poor eye contact -Aversion to physical contact -Ritualistic and repetitve behaviors -Intolerance to changes in routine |
|
|
What is Asperger's Syndrome?
|
Has similar characteristics to autism. Sometimes referred to as high functioning autism.
|
|
|
What is cerebral palsy?
|
A permanent impairment affecting automatic postural control and movement as a result of a non-progressive brain disorder
|
|
|
What are the different types of cerebral palsy?
|
-Spastic CP
-Athetoid CP -Flaccid CP -Ataxic CP |
|
|
What characterizes severe spastic CP?
|
Characterized by:
-Severe increased tone -Flexion and extension cocontraction -High tone always -More proximal than distal |
|
|
What characterizes moderate spastic CP?
|
-Near normal tone at rest
-Tone increases with excitement, movement, emotion, and speech -More distal than proximal |
|
|
What characterizes mild spastic CP?
|
-Has normal tone at rest
-Tone increases with effort and movement |
|
|
What characterizes pure athetoid CP?
|
-Tone fluctuates from low to normal
-No or little spasticity -No coactivation |
|
|
What characterizes athetoid CP with spasticity?
|
-Tone fluctuates from normal to high
-Proximal stability -Proximal spasticity -Distal athetosis (slow, writhing, continuous, and involuntary mvmt of the extremities) |
|
|
What characterizes athetoid CP with tonic spasms?
|
-Unpredictable tone
-Changes from low to very high -All flexion or all extension |
|
|
What is chorea?
|
Irregular, purposeless, involuntary, quick, jerky, and dysrhythmic movements of variable distribution.
|
|
|
What characterizes choreoathetosis CP?
|
-Constant fluctuation from low to high tone
-No cocontraction -Jerky, involuntary movement -More proximal than distal |
|
|
What are the two types of chorea?
|
-Tardive dyskinesia
-Huntington's disease |
|
|
What characterizes flaccid CP?
|
-Markedly low tone
-Seen at birth or toddler -Later classified as spastic, athetoid, or ataxic |
|
|
What is ataxic CP?
|
-Ranges from near normal to normal
-Increased tone usually involves lower extremity flexion -Most functional form of CP |
|
|
What is pulled elbow syndrome?
|
- common injury in children under five years
- dislocation of the elbow by a sudden jerk upwards of the arm |
|
|
What is Valgus Stress Symdrome?
|
- valgus overload or overstress injury to the medial elbow
- occurs as a result of repetitive throwing motions |
|
|
Brachial Plexus injury?
|
- Types are Traumautic and Obstetric
- Traumatic (Road Traffic Injuries/falling a motorcycle) - signs * a weakness in the arm * diminished reflexes * corresponding sensory deficits |
|
|
What muscles does C5 innervate?
|
C5: Shoulder abduction, extension, and external rotation; some elbow flexion and supination
|
|
|
What muscles does C6 innervate?
|
C6: Forearm pronation and supination, some wrist extension
|
|
|
What muscles does C7 innervate?
|
C7: Consistently supplies the latissimus dorsi. Elbow extension, wrist flexion, finger extension
|
|
|
What muscles does C8 innervate?
|
C8: Finger extensors, finger flexors, hand intrinsics
|
|
|
What muscles does T1 innervate?
|
T1: Hand intrinsics
|
|
|
What is pronator teres syndrome?
|
- numbness in median nerve distribution
- entrapment (compression or pinching) of the median nerve at or about the level of the elbow - Symptoms: median nerve compressed at or just above the elbow results in weakness of the pronator teres muscle - Median nerve entrapment at the elbow is a rare, more commonly seen in children |
|
|
What is medial epicondylitis?
|
-AKA Golfer's Elbow
-Caused by forceful and repeated flexion of the wrist and fingers |
|
|
What is rotator cuff tendonitis?
|
-Acute, painful condition affecting the supraspinatus and sometimes infraspinatus tendons
-Pain with external rotation and mid-range abduction |
|
|
What is a rotator cuff tear?
|
-Often requires surgical repair
-Tear to the supraspinatus tendon -Surgery not usually performed unless more than 50% of the muscle is torn |
|
|
What is bursitis and tendonitis of the shoulder complex?
|
-Affects the shoulder when the bursa and synovial sheaths become inflammed from overuse
|
|
|
What is adhesive capsulitis?
|
-AKA Frozen shoulder
-Painful condition caused by immobility and disuse -Condition lends itself to formation of fibrous tissue inside joint capsule |
|
|
What is cubital tunnel syndrome?
|
-Compression or entrapment of the ulnar nerve as it courses around the medial epicondyle of the elbow
-Cubital is behind the "funny bone" -Numbness and tingling in the ring and small fingers |
|
|
What is olecranon bursitis?
|
-When the olecrenon bursa of the elbow becomes inflammed due to contact pressure or overuse
|
|
|
What is lateral epicondylitis?
|
-AKA Tennis Elbow
-Insertion point of the extensor carpi radialis brevis becomes inflammed -If left untreated, can tear requiring surgical repair |
|
|
What is De Quervain's Syndrome?
|
-Tendonitis of the first dorsal compartment near the anatomical snuffbox
-Caused by overuse of the thumb -Tested with finklestein's |
|
|
What is carpal tunnel syndrome?
|
-Caused by inflammation of the median nerve at the wrist
-Causes numbness, tingling, and pain in thumb, index, and middle fingers -May result in thenar atrophy |
|
|
What is the Tunnel of Guyon?
|
-Similar to CTS
-Ulnar nerve becomes entrapped between the hook of the hamate, and the pisiform bones |
|
|
What is trigger finger?
|
-Caused by a nodule or thickening of the flexor tendons of the finger or thumb as they pass through the digital pulleys
-Hinders gliding motion, resulting in catching or "triggering" during flx/ext |
|
|
Which joint do you assess first?
|
Always check uninvolved joint first to establish a baseline.
|
|
|
If active ROM is less that passive ROM, what does that indicate?
|
Muscle weakness
|
|
|
When should isometric exercises be avoided?
|
-Cardiac patients
-Burns -Rheumatoid arthritis -Casts |
|
|
When should sensory testing be avoided?
|
-Receptive aphasia
-Atrophic (aptropy) skin |
|
|
What is Tinel's sign?
|
-Tapping skin over damaged peripheral nerve to elicit tingling or pins and needles
|
|
|
What is the Phalen's test?
|

Phalen's Test
|
|
|
What are the methods used to treat hypersensitivity, such as burns, amputations, PNS injuries, etc?
|
-Desensitization
-Compensation (Such as testing hot water with other hand) |
|
|
What are the methods used to treat hyposensitivity?
|
-Sensory retraining
-Compensation (Such as testing hot water with the other hand, padding objects) |
|
|
How do you treat anesthesia?
|
-Anesthesia is complete loss off sensation
-Precautionary techniques -Compensatory techniques |
|
|
How do you treat spinal cord patients with anesthesia?
|
-Pressure relief equipment
-Changing position throughout the day using timer -Inspect skin with mirrors |
|
|
What are the components of a goal?
|
-Person
-Behavior -Condition -Criterion -Function |
|
|
What is the first component of a goal?
|
Person: The person who will do the behavior
|
|
|
What is the second component of a goal?
|
Behavior: What the individual is expected to perform.
-Must be observable, measurable and functional behavior |
|
|
What is the third component of a goal?
|
Condition: The environmental situation in which the behavior is performed (when, where, what, in what manner)
-Focus on what most affects function (ie - if a child cannot sit, "in sitting" would be the condition |
|
|
What is the fourth component of a goal?
|
Criterion: Standard the client must meet.
-How well they must perform in order to achieve goal/objective. -Has to be quatifiable (number or responses, degree of ROM, length of time, amount of assistance provided, etc.) |
|
|
What is the fifth component of a goal?
|
Function: Similar to behavior, but justifies the reason for treatment. (ie - to open a door, use a computer, etc)
|
|
|
What are components of a biomechanical activity analysis?
|
-What is the activity?
-Positioning -Precautions -Steps -Repetition -ROM required -Minimal muscle strength required -Type of contraction -Appropriate for short term or long term goal |
|
|
What are SOAP notes?
|
-Subjective
-Objective -Assessment -Plan |
|
|
What is the Subjective component of a SOAP note?
|
-What a patient or significant other states
-What the patient or significant other states about their medical history, emotions, lifestyle, home situation, -Patient-stated goals "I want to work again" -Complaints -Patient's assessment of treatment |
|
|
What is the Objective component of a SOAP note?
|
-Result of the therapist's objective measurements or observations
-IE: ROM, MMT, FIMs, evaluate speed of transfers and the movement of each body part and assistance required |
|
|
What is the Assessment component of a SOAP note?
|
-Involves professional judgment
-Provides opportunity for OT to draw conlcusions from S and O -Inconsistencies between patient's complaints and the objective findings can be discussed -Comments can be made regarding patient's progress in therapy (ie - Pt. refused to participate in tx.) -Reasoning for information not obtained can be listed (ie - too much pain to complete session) |
|
|
What is the Plan component of a SOAP note?
|
- The Plan states the frequency of treatment (per day or week)
- Tx plan LTG & STG - Discharge plan - Referral to other disciplines - DME & AE needed to order - Plans for further assessment |
|
|
What are orthosis?
|
Orthosis are permanent devices that replace or substitude for loss of muscle function
|
|
|
What are the general considerations of splinting?
|
- Comfort
- Function - Cosmesis - Patient acceptance and compliance - Patient education - Tratment plan integration |
|
|
What are the objectives of static splinting?
|
The main purporse of splinting is to help the individual perfom ADLs through:
- positioning and maintaining alignment - protecting or supporting or immobilizing - inhibiting tone by positioning the extremity in a reflex inhibiting position |
|
|
What are supportive splints?
|
Supportive splints are static splints used to:
- relieve pain - position and maintain join alignment - prevent adaptive shortening of soft tissues |
|
|
What are corrective splints?
|
Corrective splints are static splints used to:
- maintain improvement obtained through therapy - correct soft tissue contractures |
|
|
What are protective splints?
|
Protective splints are static splints used to:
- immobilize a joint or limb following trauma are fracture and some post-surgical conditions |
|
|
What are the objectives of dynamics splints?
|
- prevent progressive deforming changes as a result of muscle imbalance
- substitute for or assist lost or weakened muscles - increase ROM - minimize formation of adhesions |
|
|
What are static progressive splints?
|
Static progressive splints apply low-load prolonged stress at the end range to soft tissue through static positioning to increase ROM and correct contractures
|
|
|
What are seral static splints?
|
Serial static splints hold the tissue in end range until it adaps to its new length to increase ROM and maintain improvement obtained
|
|
|
What is the functional position of the hand?
|
-Wrist: 30 degrees in extension
-Phalanges: Slight flexion -Thumb: Opposed to index finger |
|
|
What is intrinsic plus grasp?
|
Characterized by:
-All the MPs in flexion -DIPs and PIPs, full extension -Thumb in opposition to MF & RF (ie-holding a plate) |
|
|
What splint is used to subtitute for loss of intrinsic plus grasp?
|
-Use figure eight or dynamic flexion splint
-Loss of intrinsic plus is associated with median and ulnar nerve dysfunction |
|
|
When is the intrinsic plus splinting position used?
|
-For individuals with burns and traumatic hand injuries
|
|
|
What are the common splinting precautions?
|
-Preexisting skin problems
-Bony prominences -Friction -Pressure spots |
|
|
What are the warning signs of inflammatory arthritis?
|
-Swelling in one or more joints
-Early AM stiffness lasting more than one hour -Recurring pain or tenderness in any joint -Inability to move the joint -Redness and warmth in the joint -Unexplained weight loss, fever, or weakness |
|
|
What is osteoarthritis?
|
-Non-inflammatory
-Cartilage destruction -Progressive -Usually occurs due to old age |
|
|
What is a Heberden's node?
|
Osteophyte formation in the DIP
|
|
|
What is a Bouchard's node?
|
Osteophyte formation on the PIP
|
|
|
What is the difference between rheumatoid and osteoarthritis?
|
-RA is an inflammatory, systemic, autoimmune disorder
-OA is regionalized to specific joints and can be caused by trauma, overuse, and old age |
|
|
When does stiffness occur in rheumatoid and osteoarthritis?
|
-Rheumatoid: Morning stiffness lasts longer than one hour
-Osteo: Morning stiffness lasts less than one hour, but stiffness returns after overuse at end of day |
|
|
What are the deformaties related to rheumatoid arthritis?
|
-Swan neck
-Boutonniere Deformity -Zig-Zag Deformity |
|
|
What characterizes a Swan-Neck deformity?
|
-MCP flexion contractures
-PIP hyperextension -DIP flexon |
|
|
What characterizes a Boutonniere's deformity?
|
-PIP flexion
-DIP hyperextension (Memory hint-Push your finger into the table in order to replicate this) |
|
|
What are the treatment goals for osteoarthritis?
|
-Address patient's pain and inflammation
-Splinting -Increase functional (not optimal) ROM -Increase functional mobility and independence in ADLs -Education on joint protection techniques |
|
|
What are the classic signs and symptoms of osteoarthritis?
|
-Diffused pain
-In cases of advanced OA, pain may be severe enough to wake individual -Synovial inflammation -Capsular distention places pressure on nerve endings -Muscle spasms around affected joint -Pain and tenderness in peri-articular structures -Mild to mod joint stiffness |
|
|
How is adhesive capsulitis (frozen shoulder) treated?
|
-Pain management (heat, cryotherapy, TENS, myofascial release)
-PROM, stretching -Strengthening exercises/activities |
|
|
What are the weight-bearing restrictions for hip arthroplasty?
|
-No weight bearing
-Toe touch (10% on the affected and 90% on the unaffected) -Partial weight bearing (50%) -Weight bearing as tolerated -Full weight bearing |
|
|
What are the hip precautions for an anterolateral hip arthroplasty?
|
-No hip extension
-No hip external rotation -No hip adduction (No crossing legs or feet) |
|
|
What are hip precautions for posterolateral hip arthroplasty?
|
-No hip flexion more than 90
-No hip internal rotation -No hip adduction (No crossing legs or feet) |
|
|
What are the precautions for total knee replacements?
|
-No internal or external rotation of the knee (via twisting the foot)
-No forced flexion -Prevent flexion contractures by extending |
|
|
Which side should a person with a recent hip replacement sleep on?
|
On the operated side to prevent accidental crossing of leg (adduction)
|
|
|
How does a patient with a recent total knee replacement sleep?
|
Patient should on unoperated, unaffected side
|
|
|
How does a person with hemiplegia doff a pullover shirt?
|
-First gather up shirt from top back with unafected hand
-Lean forward, duck head, and pull gathered back fabric over head -Remove first from normal arm, then affected arm |
|
|
How does a person with hemiplegia donn a pullover shirt?
|
-Lay shirt on lap
-With normal hand, roll up bottom edge of shirt until you reach sleeve of affected arm -Position sleeve opening as large as possible, and use normal hand to place affected hand into sleeve opening -Pull shirt past elbow and insert normal arm into sleeve -Complete putting on shirt |
|
|
How does a person with hemiplegia donn a button-up shirt?
|
-Put shirt on lap with inside up and collar towards the chest (upside down)
-Position sleeve opening on affected side -With normal hand, place involved hand into sleeve -Put normal arm into other sleeve, and bring arm out to 180 degrees of abduction -With normal hand, pull shirt over head, and it will be positioned correctly in order to button |
|
|
What are the clinical signs of a high radial nerve injury?
|
-Wrist drop
-Thumb in palmar abduction |
|
|
What are the clinical signs of a low level (posterior interosseus/deep branch of radial nerve)injury?
|
-Wrist extension is normal
-Sensation is normal -Posterior interosseus branch of radial nerve innervates only muscles, not sensory -Loss of finger and thumb extension |
|
|
What are the clinical signs of a low (distal) radial nerve injury?
|
-Occurs at or below level of wrist
-Incomplete extension of fingers and thumb MCP -PIP and DIP can be extended |
|
|
What is the splint for radial nerve palsy?
|
-Dynamic dorsal splint for wrist extension, MCP extension, and thumb extension
|
|
|
What are the clinical signs of a high-level median nerve injury?
|
-Loss of wrist flexion
-Loss of thumb flexion, palmar abduction, and opposition -Loss of active pronation |
|
|
What are the clinical signs of a low-level median nerve injury?
|
-Flattened thenar eminence
-Loss of thumb flexion, palmar abduction, and opposition |
|
|
What splint is used for median nerve palsy?
|
Splint to position the thumb in palmar abduction and opposition
|
|
|
What are the clinical signs of a high-level ulnar nerve lesion?
|
-Hyperextension of the MCP, ring and small finger (Bishop's hand)
-Absent hypothenar and interossei -Wrist flexion abnormal |
|
|
What are the clinical signs of a low-level ulnar nerve lesion?
|
-Clawing of the MCP, ring and small finger (Bishop's hand)
-Flexion of the PIP and DIP of the small finger -Wrist flexion normal |
|
|
How is ulnar nerve palsy splinted?
|
Splint to prevent MCP hyperextension of the ring and small finger
|
|
|
What should an OT do during the acute phase of therapeutic management in a nerve injury?
|
Early post-injury/surgery phase focuses on:
-Healing and prevention -Immobilization Post-immobilization focuses on: -Increasing ROM -Enhancing function through splints and assistive devices -Patient education |
|
|
What should an OT do during the recovery phase of therapeutic management in a nerve injury?
|
This defines the period of reinnervation. Focus is on:
-Motor retraining -Sensory reeducation -Desensitization |
|
|
What should an OT do during the chronic phase of therapeutic management in a nerve injury?
|
-No further reinnervation
-Patient has significant deficits -Focus is on compensatory skills |
|
|
What should an OT do during the acute phase of a spinal cord injury?
|
-The spine is immobilized with a halo brace of body jacket
-No flexion, extension, or rotary movements of the spine and neck -Positioning -Hand splinting -Active and active-assisted exercises -PROM of joints -Neuromuscular reeducation for wrist and elbows, if indicated -Begin discharge planning |
|
|
What should an OT do during the active rehabilitation phase of a spinal cord injury?
|
-Increase upright tolerance (Teach pressure relief methods)
-AROM/PROM -Contracture prevention -Promote tenodesis -ADL/Equipment needs -Strengthening/graded activities -Bowel/bladder training -Assess need for DMEs -Caregiver education -Home evaluation |
|
|
What should an OT do during the extended rehabilitation phase of a spinal cord injury?
|
-Driving
-Leisure activities -Prevocational assessment -Home modifications -Community reentry -Technology use |
|
|
What elbow exercises are needed for an individual with spinal cord injury?
|
-Engage triceps in activity to prevent flexion contractures
-Elbow extension is needed for transfers and weight shifting |
|
|
What shoulder exercises are needed for an individual with spinal cord injury?
|
Focus on promoting proximal stability by engaged:
-Shoulder depressors (lower traps, latissimus dorsi, and pectoralis minor) -Work shoulder flexors, abductors, and extensors |
|
|
What wrist exercises are needed for an individual with spinal cord injury?
|
-Wrist extension
-Focus on maximizing tenodesis with ROM of finger flexion with wrist extension and ROM of finger extension with wrist flexion |
|
|
What are the signs of a Deep Venous Thrombosis (DVT)?
|
-Edema
-Increased venous pattern -Pain and tendernous -Low-grade, idiopathic fever |
|
|
What is a postural or orthostatic hypotension?
|
-Common in T6 and above injuries
-Light headedness, dizziness, and/or fainting when moving from reclined to upright position -Patient must recline quickly |
|
|
What are the signs of a pulmonary embolism?
|
-Sudden shortness of breath (SOB)
-Hyperventilation -Cardiac Arrhythmias |
|
|
What is heterotrophic ossification?
|
-Abnormal deposition of osseous material in the hip, knee, elbow, and shoulder
-Symptoms include: heat, pain, swelling, decreased ROM, and fever -Usually appears 1-4 months post traumatic injury, such as TVA -Sometimes requires joint replacement surgery |
|
|
What is ankylosis?
|
-Fixation or fusion of a joint, often in an abnormal position
-Usually results from destruction of articular cartilage, as in RA |
|
|
What ankylosing spondylitis?
|
-A chronic inflammatory disease of ideopathic origin
-First affects the spine in adjacent structures and commonly progresses to eventual fusion (ankylosis) of involved joints |
|
|
What is a C-bar splint used for?
|

-Used to maintain webspace
-No joint stabilization |
|
|
What is a first-degree burn?
|
-Superficial burn involving the epidermis
-Caused by sunburn and minor flash injuries -No edema, no blisters |
|
|
What is a superficial partial-thickness burn?
|
-Second degree burn
-Involves epidermis and papillary dermis -Skin is moist, weepy, and blistered -Edema is present -Very painful type of burn -No scarring |
|
|
What is a deep partial-thickness burn?
|
-Deep second degree burn
-Involves epidermis and the dermis -Mottled areas of red and white eschar (dead tissue that sloughs off of healthy skin) -May be painful -Hypertrophic scarring and contractures -May need skin grafting |
|
|
What is a full-thickness burn?
|
-Third-degree burn
-Destruction of epidermis, dermis, and subcutaneous tissues -Adipose tissue may be exposed -Skin appears dry and leathery -No pain -Require skin grafting |
|
|
How is a wheelchair seat measured?
|
-Across the widest point of the hips of thighs
-Add half an inch to one inch on each side |
|
|
How is wheelchair back height measured?
|
-From the bottom of the buttocks to the top of the shoulder
-Subtract four to three inches, depending on trunk control and UE strength -Head rest may be required if no trunk control present |
|
|
How do you measure a wheelchair armrest?
|
From the buttocks to the bent elbow, add one inch
|
|
|
How do you measure seat depth?
|
From the buttocks to the popliteal fossa (behind the knee), subtract one to two inches
|
|
|
How do you measure footrest height?
|
-From the bottom of the heel to the popliteal fossa when individual is in 90 degrees of knee flexion
-Subtract two inches for floor clearance |
|
|
What are common cardiac precautions?
|
-Don't push and pull with UEs
-Don't lift weights -Perform transfers using mostly LE strength -Don't lean below level of the heart -Don't raise both arms at same time |
|
|
What splint is used for median nerve compression (CTS)?
|
Dorsal, volar, or ulnar gutter splint
|
|
|
What splint is used for a carpal tunnel release surgery?
|
Volar splint with the wrist in a neutral, or slightly extended wrist position
|
|
|
What immobilizing splint is used for radial nerve palsy?
|
Volar or dorsal, 15-30 degrees of wrist extension
|
|
|
What immobilizing splint is used for tendinitis/tenosynovitis?
|
Volar or dorsal, 20-30 degrees of wrist extension
|
|
|
What immobilizing splint is used for rheumatoid arthritis?
|
-Volar in extension up to 30 degrees, based on the person's comfort level
-Ulnar drift close to neutral during early stages |
|
|
What immobilizing splint is used for wrist fracture?
|
-Volar, dorsal, or circumferential.
-Maximum passive extension up to 30 degrees. |
|
|
What immobilizing splint is used for reflex sympathetic dystrophy (CRPS)?
|
-Volar in extension, as tolerated
-Circumferential wrist might be used to avoid edema |
|
|
What is a resting hand splint used for?
|
-RA, Burns, Dupuyten's, and RSD
-Supports the hand and wrist joint so that they heal without contracting and so that a deformity does not develop |
|
|
When are thumb immobilization splints used?
|
-DeQuervain's Tenosynovitis
-Rheumatoid arthritis -Osteoarthritis -Traumatic injuries of the thumb |
|
|
When is a thumb spica used?
|
-Immobilizes the thumb while allowing other digits freedom to move
-A long thumb spica splint also immobilizes the wrist -Immobilizes 1st CMC and sometimes 1st MP and IP -Hand based (short opponens splint) |
|
|
What is the difference between oral apraxia and dysarthria?
|
Dysarthria is a neuromotor disorder affecting the muscles of the face, whereas oral apraxia (such as Broca's aphasia )is purely neurological.
|
|
|
What is the main goal during the acute phase in mental health?
|
Stabilization
|
|
|
What is the main goal during the subacute phase in mental health?
|
-Enabling activities
-Performance components |
|
|
What is the main goal during the rehab phase of mental health?
|
-Functional activities
-Performance components |
|
|
What is the main goal during the chronic phase of mental health?
|
-Focus on compensatory techniques and environmental adaptations
|
|
|
What is the diagnostic criteria for major depressive disorder?
|
Must present with either depressed mood or loss of interest or pleasure. Can be a single episode.
|
|
|
What is the diagnostic criteria for dysthymic disorder?
|
More than two years depressed for most of the day.
|
|
|
What are the characteristics of bipolar disorder type I?
|
-Full manic episodes
-Promiscuity |
|
|
What are the characteristics of bipolar disorder type II?
|
-Hypomanic
-Depressed -Symptoms not severe |
|
|
What characterizes dementia?
|
-Patient is cooperative, but frustrated
-Onset is insidious -Cognition is prominently impaired -Symptoms worsen as day progresses |
|
|
What is a reasonable accomodation?
|
-Undue hardship in relation to company's assets
-Applies to companies with 15+ employees |
|
|
Is a person who is considered a risk to themselves or others eligible for ADA protection?
|
No. The person must be able to perform the job task safely without risk of harming patients.
|
|
|
What is the role of OT in the ADA?
|
-Prepare clients for disclosure
-Identify qualifications -Focus treatment to identify limitations -Educate client -Advocate and educate employer/public |
|
|
What are the steps in determining reasonable accomodation?
|
-Job analysis
-Disability-related limitations -Identify potential accomodations -Select and implement |
|
|
What can an individual accomplish at Allen's Cognitive Level 1?
|
Automatic actions
|
|
|
What can an individual accomplish at Allen's Cognitive Level 2?
|
Aware of large objects an can accomplish very simpl tasks
|
|
|
What can an individual accomplish at Allen's Cognitive Level 3?
|
-Patients use hands for simple, repetitive tasks
-Unlkely to produce consistent end product |
|
|
What can an individual accomplish at Allen's Cognitive Level 4?
|
-Patients are able to copy demonstrated directions (ie - visual and verbal cues) presented one step at a time
-Individuals can copy a sample plan to follow directions |
|
|
What can an individual accomplish at Allen's Cognitive Level 5?
|
-Patients perform tasks involving three familiar steps and one new one
-New learning occurs at this level |
|
|
What can an individual accomplish at Allen's Cognitive Level 6?
|
-Patients can anticipate errors and plan ways to avoid them
-Can follow written directions -Operate at normal capacity |
|
|
What is the remotivation approach?
|
-Using memories from pictures and music to remotivate patients
|
|
|
What is reality orientation?
|
Awareness of date and time
|
|
|
What is rationalization?
|
Making excuses for behaviors that are considered unacceptable
|
|
|
What is identification?
|
Taking on the character of another person
|
|
|
What is projection?
|
Blaming others for one's behaviors
|
|
|
What is level one of meal preparation?
|
Very simple
Example: Pouring glass of OJ |
|
|
What is level two of meal preparation?
|
Preparing simple step meals
Example: Peanut butter jelly and instant pudding |
|
|
What is level three of meal preparation?
|
Soups, frozen dinners, hot beverages
|
|
|
What is level four of meal preparation?
|
Hot, one dish meals
Example: Macaroni and cheese |
|
|
What is level five of meal preparation?
|
Two hot meals
Example: Chicken and mashed potatoes |
|
|
How much should a ramp be graded?
|
Maximum slope of 1 foot of ramp per every inch of rise in height
|
|
|
What is alexia?
|
Inability to understand written language
|
|
|
What is a utilization review?
|
Process of analyzing the provision of services to promote the most economical delivery service
|
|
|
What is close OT supervision?
|
Reporting once per day
|
|
|
What is routine OT supervision?
|
Reporting every two weeks
|
|
|
What is general OT supervision?
|
Once a month?
|
|
|
What is minimal OT supervision?
|
As needed
|
|
|
What is Title 1 of the ADA?
|
Addresses reasonable accomodation and employment discrimination
|
|
|
What is Title 2 of the ADA?
|
Addresses public services, constructed buildings, state and local gov't business
|
|
|
What is Title 3 of the ADA?
|
-Public accomodations
-Accessible design |
|
|
What does Title 4 of the ADA address?
|
Telecommunications for hearing and speech impaired
|
|
|
What is underlying premise of Rood technique?
|
Facilitory/inhibitory
|
|
|
What is underlying premise of Bobath (NDT) technique?
|
-Normal movement (ie - weight bearing)
|
|
|
What is the underlying premise of PNF technique?
|
Uses functional patterns of stretching in order to elicit proprioceptive awareness of one's body parts
|
|
|
What is a parallel group?
|
-Has a directive leader
-Focuses on task completion -No interaction -Indiv's are low level -Work on trust, awareness, comfort |
|
|
What is a developmental project group?
|
-Has a directive leader
-Focus is on group interaction -Individuals work on initiation, sharing, short-term tasks (ie - collage) and working with two people |
|
|
What is an egocentric-cooperative group?
|
-Facilitative leadership
-Focuses on acquiring skill -Not focus on task completion -Long-term tasks (ie-mosaics) |
|
|
What is a cooperative group?
|
-Facilitative leadership
-Goal is to acquire skills -Not focused on completing task -Feeling expression encouraged -Therapist acts as advisor |
|
|
What is a mature group?
|
-Therapist acts as equal group member
-Advisory type of leadership -Goal is for members to self direct -Requires end product and time limit |
|
|
What is an evalutation group?
(Type of activity group) |
-Purpose is to assess skills and limitations regarding group interaction
-For indiv's who lack group interaction skills -The therapist does not participate or intervene (only acts as observer) |
|
|
What is a thematic group?
(Type of activity group) |
-Purpose is to acquire knowledge and skills to perform a specific activity
-For indiv's who have minimal interaction skills -Therapist selects, structures, and grades activities -Therapist acts as advisor -Activities directly relate to skills (ie-cooking group, parallel group) |
|
|
What is a topical group?
(Type of activity group) |
-Purpose is to discuss activities engaged outside of group
-For individuals who share similar problems in functioning (ie-egocentric cooperative level) -Therapist acts as a role model and shares leadership -Activities include verbal discussion and roleplay |
|
|
What is a task-oriented group?
(Type of activity group) |
-The purpose is to increase awareness of needs, values, ideas, feelings, behaviors
-Intended for indiv's with disfunction in cognition and social-emotional areas (psych or physical trauma) -Used for substance abuse -Therapist is initially active and provides structure -Activities create an end product |
|
|
What is a developmental group?
(Type of activity group) |
-Purpose is to develop interaction skills for parallel, project, egocentric cooperative, cooperative, mature groups
|
|
|
What is an instrumental group?
(Type of activity group) |
-Purpose is to help functioning at highest level and meet mental health needs
-Intended for individuals who have an ability to change or progress -Therapist acts as supporter and is unconditional -Activities focus on maintaining function |
|
|
What is Axis I in the DSM-IV?
|
Clinical disorders/psych diagnoses
|
|
|
What is Axis II in the DSM-IV?
|
MR & personality disorders
|
|
|
What is Axis III in the DSM-IV?
|
General medical conditions
|
|
|
What is Axis IV in the DSM-IV?
|
Psychosocial & environmental problems
|
|
|
What is Axis V in the DSM-IV?
|
GAF Score
|
|
|
What is the GAF scale?
|
The Global Assessment of Functioning (GAF) scale is a numeric scale (0 through 100) used in mental health to rate the social, occupational and psychological functioning of adults. (DSM-IV)
|
|
|
What is a GAF scale of 0?
|
0: Not enough information available to provide GAF.
|
|
|
What is a GAF scale of 91 - 100?
|
91-100: Superior functioning in a wide range of activities, life's problems never seem to get out of hand. No symptoms.
|
|
|
What are cluster A personality disorders?
|
Paranoid, schizoid, schizotpal (odd/peculiar behavior)
|
|
|
What are cluster B personality disorders?
|
Antisocial, borderline, histrionic, narcissistic (dramatic/implusive)
|
|
|
What are cluster C personality disorders?
|
Avoidant, dependent, obsessive compulsive (anxiety/fear)
|
|
|
What are the characteristics of paranoid personality disorder?
|
-Feelings of being threatened or persecuted
-Indiv is withdrawn, suspicious -Have dillusions/hallucinations |
|
|
What is the difference between a hallucination and a dillusion?
|
-During hallucinations, indiv's sense (see, hear, etc) a non-existent external stimulus and with a compelling sense of their reality
-Dillusions are misinterpretations of external stimuli |
|
|
What is schizoid personality disorder?
|
-Characteristics are limited emotional range
-Absense or indifference to social activity -Withdrawn -Self absorbed |
|
|
What is schizotypal disorder?
|
-Same features as schizophrenia, but to lesser degree
-Cognitive impairment, primarily in working memory, verbal learning, and sustained attention |
|
|
What is antisocial personality disorder?
|
-Must be at least 18 years or older
-Engage in illegal activity -Unemployed, aggressive, impulsive, irresponsible -Lack of remorse |
|
|
What is borderline personality disorder?
|
-Impulsive
-Mood instability -Inappropriate affect -Suicidal ideations -Self mutilation -Fear of abandonment |
|
|
What is histrionic personality disorder?
|
-Theatrical
-Center of attention -Extreme emotionality -Approval seeking -Low frustration tolerance -Unable to delay gratification |
|
|
What is narcissistic personality disorder?
|
-Grandiosity
-Attention seeking -Lack of empathy -Egomaniac with inferiority complex |
|
|
What is avoidance personality disorder?
|
-Social discomfort
-Avoidance of interpersonal relationships is common -Fear of disapproval |
|
|
What is dependent personality disorder?
|
-Most common personality disorder
-Individuals believe they can not survive without relationships -Desire to win approval and avoid abandonment -Submissive -Difficulty making decisions -Fear of being alone |
|
|
What is obsessive-compulsive personality disorder?
|
-Potentially most disabling
-Perfectionistic -Rigid -Ritualistic behavior |
|
|
What is the comprehensive occupational therapy evaluation (COTE)?
|
Evaluates general, interpersonal, and task behaviors pertenent to OT
|
|
|
What is delirium?
|
-Impairment of consciousness with global cognitive impairments
-Lability -Hallucinations |
|
|
What is dementia?
|
-Commonly seen in Alzheimer's, head trauma, Parkinson's and Huntington's
-Multiple cognitive deficit including memory loss and impaired consciousness |
|
|
What psychiatric symptoms can be present in Huntington's
|
Psychotic Features
|
|
|
What psychiatric symptoms are present in epilepsy?
|
-Psychosis (hallucinations)
-Fear and anxiety |
|
|
What psychiatric symptoms are present in brain tumors?
|
-Hallucinations
-Depression -Psychosis -Personality changes |
|
|
What are the psychiatric symptoms of head trauma?
|
-Psychosis
-Disturbances of mood -Personality changes -Agitated/withdrawn |
|
|
What is the Kohlman Evaluation of Living Skills? (KELS)
|
Assesses basic living skills using interview and test
|
|
|
What are the four types of mental health service delivery?
|
-Traditional
-Partnership -Supportive -Seperatist |
|
|
What is the "traditional" type of mental health service delivery?
|
-Professionals provide the service
-Clients receive the service |
|
|
What is the "partnership" type of mental health service delivery?
|
-Clients are informed that they are partners in the service
-The distinction between professionals and clients remain clearly defined |
|
|
What is the "supportive" type of mental health service delivery?
|
Professionals are excluded, except in external roles
|
|
|
What is the "separist" type of mental health service delivery?
|
-Ex-patients provide the support and run the service
-Non-patients and professionals are excluded |
|
|
What is dyspraxia?
|
Difficulty in planning new motor tasks
|
|
|
What is dysgraphia?
|
Inability to print or write
|
|
|
What is a conduct disorder?
|
Conduct disorders often involve aggression toward people or animals and property destruction
|
|
|
What is a Volkmann's contracture?
|
A fracture of the distal end of the humerus that interferes with blood supply of the forearm
|
|
|
What muscle is affected in an axillary nerve injury?
|
The serratus anterior muscle
|
|
|
What domains are included in the Practice Framework?
|
1) Performance Areas
2) Performance Skills 3) Performance Patterns 4) Context 5) Activty demands 6) Client Factors |
|
|
What is included in the Performance Areas of Occupation (Practice Framework)?
|
-ADLs
-IADLs -Education -Work -Play -Leisure -Social Participation |
|
|
What is included in Performance Skills (Practice Framework)?
|
-Motor Skills
-Process Skills -Communication/Interaction Skills |
|
|
What are Process Skills (Practice Framework)?
|
-energy
-knowledge -temporal organization (time) -organizing space & objects |
|
|
What is included in the Performance Patterns (Practice Framework)?
|
-Habits
-Routines -Roles |
|
|
What is included in the Context of the Practice Framework?
|
-Cultural
-Physical (Environment) -Social -Personal(socioeconomic, age) -Spiritual -Temporal -Virtual |
|
|
What is included in the Activity Demands of the Practice Framework?
|
-Objects used and their properties
-Space Demands -Social Demands -Sequencing and Timing -Required Actions -Required Body Functions -Required Body Structures |
|
|
What is included in the Client Factors of the Practice Framework?
|
-Body Function
-Body Structure |
|
|
What are IADLs?
|
Activities that are oriented toward interacting w/the environment and that are generally optional
|
|
|
Give examples of IADLs?
|
-Care of pets
-Care of others -Child rearing -Communication devices -Financial management -Meal preparation and cleanup |
|
|
What are the steps in an activity analysis?
|
1) Break down componens of activity
2) Determine performance components 3) Assess therapeutic value of activity |
|
|
What methods are used to analyze an activity?
|
1) Specify exact activity
2) Idenitify procedures, materials and tools 3) Analyze standard performance of activity 4) Use AOTA uniform terminology 5) Select frame of reference |
|
|
What is defined as therapeutic use of self?
|
The therapist's conscious, planned interaction with the individual, family members, significant others, and/or caregivers
|
|
|
What are the stages of group development?
|
1)Origin phase
2)Orientation phase 3)Intermediate phase 4)Conflict phase 5)Cohesion phase 6)Maturation phase 7)Termination phase |
|
|
What are the styles of group leadership?
|
-Directive
-Facilitative -Advisory |
|
|
What is a directive leadership style (groups)?
|
-Therapist is responsible for planning and structuring
-Members have limited cognitive, social, and verbal skills -Used in parallel and project group levels -Goal: Task accomplishment |
|
|
What is a facilitative leadership style (groups)?
|
-Therapist shares responsibility with the members
-Members' skill level is moderate -Used in egocentric cooperative or cooperative groups -Goal: Skill acquisition through experience |
|
|
What is a advisory leadership style (groups)?
|
-Therapist functions as a resource
-Members set the agenda and structure -Members have a high skill level -Used in mature groups -Goal: Have members understand and self-direct the process |
|
|
According to Mosey, what are the major types of activity groups?
|
-Evaluation group
-Thematic group -Topical group -Task-oriented group -Developmental group -Instrumental group |
|
|
What is the purpose of an evaluation group?
|
-Assess client's skills, assets, and limitations regarding group interaction
|
|
|
What is the purpose/focus of a therapeutic group?
|
-Assist members in acquiring the knowledge, skills, and/or attitudes needed to perform a specific activity
-Members must have interaction skills equal to a parallel group skill level |
|
|
What is the purpose/focus of a topical group?
|
-Discuss activities outside of group
-Members must be at an egocentric-cooperative group skill level -Therapist shares leadership and acts as role model |
|
|
What is the purpose/focus of a task-oriented group?
|
-To increase clients' awareness of their needs, values, ideas, feelings, and behaviors as they engage in a group task
-Members' primary dysfunction is cognitive and socioemotional due to psychological or physical trauma |
|
|
What is a developmental group?
|
A continuum of groups consisting of parallel, project, egocentric cooperative, cooperative, and mature
|
|
|
What is the purpose/focus of a (developmental) parallel group?
|
-To enable members to perform individual activities in the presence of others
-Leadership: directive -Members' cognitive level: low |
|
|
What is the purpose/focus of a (developmental) project group?
|
-To develop the ability to perform a shared, short-term activity in a cooperative manner
-Members' cognitive level: low -Leadership: directive -Goal: group interaction |
|
|
What is the purpose/focus of a (developmental) egocentric-cooperative group?
|
-Enables members to select and implete a long-range activity (i.e.: grout with tiles drying)
-Requires group interaction -Members' cognitive level: Medium -Leadership style: facilitative Goal: acquire skills |
|
|
What is the purpose/focus of a (developmental) cooperative group?
|
-Enables members to engage in group activity to facilitate expression
-Members' cognitive level: Medium -Leadership style: facilitative Goal: acquire skills |
|
|
What is the purpose/focus of a (developmental) mature group?
|
-Enable members to assume all functional, socio-emotional and task roles within a group
-Members' cognitive level: high -Leadership: advisory -Goal: help members self-direct |
|
|
What is an instrumental group?
|
-To help members function at their highest possible level
Goal: prevent regression, maintain function, and meet mental health needs Type of member: high functioning |
|
|
What is conceptual age of a fetus?
|
Age of fetus or newborn in weeks since conception
|
|
|
What is gestational age of a fetus?
|
Age of fetus or newborn in weeks from first day of mother's last normal menstrual period
|
|
|
What is the development of sensorimotor integration in the prenatal period?
|
1) responds to tactile stimuli
2) reflex development |
|
|
What is the development of sensorimotor integration in the neonatal period?
|
-Tactile, proprioceptive and vestibular input needed for body scheme
-Vestibular defines arousal level -Visual system develops as infant responds to faces and items placed 10" from face |
|
|
What is the development of sensorimotor integration in the first six months?
|
-Infant movement patters progress from reflexive to voluntary and goal directed
-Vestibular, proprioceptive, and visual integrate for postural control -Visual and tactile systems become integrated to lay foundation for eye-hand coordination |
|
|
What is the development of sensorimotor integration in the six to twelve month period?
|
-Fine motor and motor planning develop due to refinement of tactile and proprioceptive senses
-Midline skills and crossing midline -Primitive self-feeding |
|
|
What are the components of motor development?
|
-Crossing midline
-Laterality -Bilateral integration -Fine coordination and dexterity -Visual-motor integration -Oral-motor control |
|
|
What is exploratory play?
|
-0 to 2 years
-play experience develops body scheme -child explores properties and effects of actions |
|
|
What is symbolic play?
|
-2 to 4 years
-Play helps to formulate, test, classify, and refine ideas |
|
|
What is creative play?
|
-4 - 7 years
-Child participates in cooperative peer groups |
|
|
What are games?
|
- 7-12 years
-Rules, competition -Friends become important for validation |
|
|
What are the dressing skill milestones at 1 year?
|
-Cooperates with dressing
-Pulls off shoes and socks |
|
|
What are the dressing skill milestones at 2 year?
|
-Helps pull down pants
|
|
|
What are the dressing skill milestones at 2 1/2 years?
|
-Unbuttons large buttons
-Assists in putting on socks |
|
|
What are the dressing skill milestones at 3 years?
|
-Puts on shirt w/ Min A
-Zips and unzips -Pulls down pants I -Buttons large buttons |
|
|
What are the dressing skill milestones at 3 1/2 years?
|
-Works snaps or hooks in front
|
|
|
What are the dressing skill milestones at 4 year?
|
-Removes pullover I
-Laces shoes -Identifies front and back |
|
|
What are the dressing skill milestones at 5 years?
|
-Ties and unties knots
-Dresses I |
|
|
At what age is a child I in toileting?
|
4 to 5 years
|
|
|
What should you do if you have questions about potential ethical violations that could cause harm?
|
Call the State Regulatory Board (SRB). NBCOT and AOTA should be contacted if offender falls under their licensing jurisdiction
|
|
|
Who should you report client/patient abuse to?
|
Immediate supervisor
|
|
|
What is the SEC?
|
Standards and Ethics Commission: a component of AOTA responsible for the code of ethics and standards of practice of the profession
|
|
|
Can OT Assistants be activities directors in skilled nursing facilities?
|
Yes and they can also supervise OT aids
|
|
|
What persons are eligible for medicare coverage?
|
-65 years or older
-Permanent kidney failure -Black lung disease -Persons on SS program for 24 months |
|
|
What does Medicare Part A cover?
|
-Pays for hospital, inpatient SNF, home health, and hospice care
-Requires annual deductible fees -Automatically provided by all cover in Social Security system that meet criteria |
|
|
What is cover under Medicare Part B?
|
-Covers hospital outpatient physician and other professional services including OT
-Consider supplemental -Must be purchased as a monthly premium |
|
|
What is the difference between Medicare Part A and B?
|
-Inpatient Part A requires service for a minimum of 5 days per week
-Part B covers 3 days of outpatient |
|
|
What are the 4 basic steps of program development?
|
-Needs assessment
-Program planning -Program implementation -Program evaluation |
|
|
What is a Needs Assessment?
|
-Describes community factors and populations at risk
-Target population, demographics, functional levels, disorders |
|
|
What is Program Planning?
|
-Defines focus for a program based on needs assessment results
|
|
|
What is Program Implementation?
|
-Initiates program according to time table and steps set forth in the program plan
-Promote program to ensure it reaches target population |
|
|
What is Program Evaluation?
|
-Systematic review and analysis of care provided to determine if care is at an acceptable level of quality
|
|
|
What are the types of approaches used in program evaluation?
|
-Continuous quality improvement (CQI): limitations and problems used to improve quality
-Utilization review: reviews use of resources in facility -Peer review -Professional review organization -Risk management |
|
|
What is spina bifida with myelomeningocele?
|
Protrusion of a sac through the spine, containing CSF and spinal cord/nerve roots
|
|
|
What is spina bifida with meningocele?
|
Protrusion of a sac through the spine, containing CSF and meninges; does NOT include spinal cord
|
|
|
What type of spina bifida presents with the most symptoms?
|
SB with a myelomeningocele results in sensory and motor deficits below the level of the lesion and may result in paralysis
|
|
|
What is Arnold-Chiari Syndrome?
|
-Cerebellum and medulla oblongata slip through foramen magnum of skull
-Typically results from spina bifida |
|
|
What is Duchenne's Muscular Dystrophy?
|
-Progressive disorder in which weakness occurs in all voluntary muscles, including the heart
-With Duchenne's, individuals rarely survive beyond early 20s -Focus on energy conservation, breathing techniques, I in ADLs, maintaining/increasing ROM |
|
|
What is Huntington's Chorea?
|
Characterized by choreiform movements and progressive intellectual deterioration
|
|
|
What is delirium?
|
A disoriented reaction with restlessness and confusion that may be associated with fear and hallucinations
|
|
|
What is affect?
|
The observable component of emotion
|
|
|
What are the subtypes of schizophrenia?
|
-Paranoid type
-Disorganized type -Catatonic type -Undifferentiated type -Residual type |
|
|
What is undifferentiated type schizophrenia?
|
Used to classify individuals who do not fit clearly into another subcategory of schizophrenia
|
|
|
What is disorganized type schizophrenia?
|
Primitive, disinhibited, and disorganized behavior
|
|
|
At what SCI level can a person use a universal cuff?
|
C6
|
|
|
What is sundowning?
|
Occurs in the late afternoon and at night in older individuals. Characterized by drowsiness, confusion, ataxia, and falling.
|
|
|
What is echopraxia?
|
The meaningless imitation of another person's movements
|
|
|
What is astereognosis?
|
The inability to identify objects through touch
|
|
|
What is the global assessment of functioning scale (GAF)?
|
A numeric scale from 0 to 100 that rates the social, occupational and psychological functioning of adults. This is axis five of the DSM-IV
|
|
|
What is the diagnostic criteria for a major depressive episode?
|
A two-week period of depressed mood or loss of interest or pleasure
|
|
|
What should a typical substance abuse OT intervention focus on?
|
Intervention should focus on developing skills for a substance-free lifestyle. This includes interpersonal relationships, socialization, and vocation. Assistance with practical services, such as obtaining Social Security, housing, and food stamps should also be a focus
|
|
|
What should a typical anxiety disorder OT intervention focus on?
|
OT interventions with anxiety disorders such as panic disorder, OCD, and PTSD should utilize skills training and cognitive behavioral approaches as well as teaching relaxation and stress management skills
|
|
|
What is schizoid personality disorder?
|
Individuals who display a lifelong pattern of social withdrawal. Marked by this cover with human interaction in conversion and bland constricted affect. Often seen by others as eccentric, isolated, or lonely
|
|
|
What is histrionic personality disorder?
|
Characterized by colorful, dramatic, extroverted behavior in excitable, emotional persons. Inability to maintain deep, long-lasting attachments with accompanying flamboyant presentation is often characteristic
|
|
|
What is oppositional defiant disorder?
|
Negativistic, hostile, and defined behaviors that result in functional impairment
|
|
|
What is conduct disorder?
|
A disregard for the rights of others leading to aggression towards people and animals, destruction of property, deceitfulness, theft, or serious violation of rules
|
|
|
How are oppositional defiant disorder and conduct disorder treated?
|
OT intervention focuses on development and improvement of self-esteem/self-efficacy. A focus is placed on developing the skills needed for ADL's, social, leisure, and school behaviors
|
|
|
How are eating disorders treated?
|
Activities to promote a reality based body image, education and management of nutrition, and activities to improve communication skills and self-expression
|
|
|
What are symptoms of Rett's syndrome?
|
Characterized by repetitive movements of licking, biting, and slapping of one's hands
|
|
|
How is Rett's syndrome treated?
|
Treatment may involve adaptations to maintain the integrity of the skin such as dynamic elbow splints that inhibit a hand to mouth pattern by limiting full elbow flexion
|
|
|
What is validity?
|
Determines if the tool measures what it is intended to measure
|
|
|
What is reliability?
|
Establishes the consistency of the evaluation
|
|
|
What is an opponens splint?
|
-May be short or long
-Supports the thumb in a position of abduction and opposition -Used during functional activities |
|
|
What is a cock up splint?
|
This splint supports the user's wrist in 10° to 20° of extension to prevent contracture, but allows digits to function, such as in a case involving a flaccid wrist
|
|
|
What does a manual muscle test of (0) indicate?
|
Zero (Z): No muscle contraction can be seen or felt
|
|
|
What does a manual muscle test of (1) indicate?
|
Trace (T): Contraction can be felt or seen underneath the skin, but there is no motion
|
|
|
What does a manual muscle test of (2-) indicate?
|
Poor Minus (P-): Individual is only able to move joint through incomplete range of motion with gravity eliminated
|
|
|
What does a manual muscle test of (2) indicate?
|
Poor (P): Part moves through complete range of motion with gravity eliminated
|
|
|
What does a manual muscle test of (2+) indicate?
|
Poor Plus (P+):
-Part moves through incomplete range of motion (less than 50%) against gravity -OR through complete range of motion with gravity decreased against slight resistance |
|
|
What does a manual muscle test of (3-) indicate?
|
Fair minus (F-): Part moves through incomplete range of motion (more than 50%) against gravity
|
|
|
What does a manual muscle test of (3) indicate?
|
Fair (F): Part moves through complete range of motion against gravity
|
|
|
What does a manual muscle test of (3+) indicate?
|
Fair plus (F+): Part moves through complete range of motion against gravity and slight resistance
|
|
|
What does a manual muscle test of (4) indicate?
|
Good (G): Part moves through complete range of motion against gravity and moderate resistance
|
|
|
What does a manual muscle test of (5) indicate?
|
Normal (N): Part moves through complete range of motion against gravity and full resistance
|
|
|
How should sensation testing be conducted in a spinal cord injury?
|
-Tested proximal to distal
-Vision occluded -Test uninvolved side first |
|
|
How should sensation testing be conducted in a peripheral nerve injury?
|
-Tested distal to proximal
-Vision occluded -Test uninvolved side first |
|
|
What is the protocol for a contrast bath?
|
-Begin in warm water for 10 minutes
-Move hand to cold water for 1 minute, then back to warm for four minutes -Continue for 15 to 30 minutes and end in warm water -In severe case of edema, end in cold water for 1 minute |
|
|
How are cold packs most effectively placed?
|
In an elevated position
|
|
|
What type of split would be crafted for a brachial plexus injury?
|
A flail arm splint
|
|
|
What type of split would be crafted for a median nerve injury?
|
An opponens splint or C-Bar splint
|
|
|
What type of split would be crafted for an ulnar nerve injury?
|
A dynamic/static splint to position MPs in flexion
|
|
|
What type of split would be crafted for a combined median/ulnar nerve injury?
|
A figure of eight splint or dynamic MCP flexion splint
|
|
|
What type of splint would be crafted for someone with a C6-C7 spinal cord injury?
|
A tenodesis splint
|
|
|
What type of split would be crafted for someone with the skiers thumb injury?
|
A hand-based thumb splint
|
|
|
What type of split would be crafted for someone with CMC arthritis?
|
A hand-based thumb splint
|
|
|
What type of split would be crafted for someone with a flexor tendon injury?
|
Kleinert or Duran dorsal protection splint
|
|
|
What type of splint would be crafted for someone with swan neck?
|
Silver rings or buttonhole splint
|
|
|
What type of split would be crafted for someone with a Boutenniere deformity?
|
Silver rings or dynamic PIP extension splints
|
|
|
What type of split would be crafted for someone with arthritis?
|
A functional splint or safe splints, depending on stage
|
|
|
What type of split would be crafted for someone with flaccidity?
|
A resting splint
|
|
|
What type of split would be crafted for someone with spasticity?
|
A spasticity splint or a cone splint
|
|
|
What is the position of deformity?
|
-Wrist flexion
-MCP hyperextension -IP joints flexed -Thumbs adducted |
|
|
What is the functional position of the hand?
|
-Wrist 20 to 30° of extension
-MCPs 45° flexion -IPs 20 to 30° of flexion -Thumb in palmar abduction |
|
|
What is agraphia (a.k.a. dysgraphia)?
|
The inability to write
|
|
|
What is an intervention strategy for motor/ideomotor apraxia?
|
Provide hand over hand tactile-kinesthetic input, and utilize visual cues
|
|
|
What is a blocking splint used for?
|
Used to isolate tendon and joint range of motion
|
|
|
What is an appropriate approach to take with a child with behavioral problems?
|
Provide enjoyable activities in a safe and accepting environment
|
|
|
What are intervention strategies for ideational apraxia?
|
Provide step-by-step instructions and hand over hand guiding
|
|
|
What are intervention strategies for perseveration?
|
Bring the perseveration to a conscious level and train the person to inhibit the behavior
|
|
|
What are intervention strategies for spatial neglect?
|
-Provide graded scanning activities
-Use external cues such as colored markers and written directions |
|
|
What are intervention strategies for body neglect?
|
Provide bilateral activities, guide the affected side through the activity, and increase sensory stimulation to the affected side
|
|
|
What are intervention strategies for aphasia?
|
-Decrease external auditory stimuli
-Give individual increase response time -Use concise sentences -Use visual cues and gestures |
|
|
What are intervention strategies for sequencing and organization deficits?
|
-Use external cues such as written directions and daily planners
-Use graded tasks that increase in complexity in terms of number of steps required |
|
|
How is desensitization done?
|
-Grade stimulus from soft to hard to rough
-Grade force of application from touch to: rub->tap->prolonged Ex: -rub: pet cat, fingerpaint, sandcastles -tap: juggle cotton balls, ping pong balls, or tennis balls -prolonged: flour, rice, beans, macaroni -Compensation- Ex: padding objects |
|
|
How is sensory retraining done?
|
-Sensory Retraining- learn the meaning of new sensation
1. vigorous, generalized cutaneous stimulation (Ex: rub affected area briskly with terrycloth) 2. cognitive cueing (Ex: OT & pt. discuss stimuli) 3. feedback (Ex: visual feedback) -Compensatory Techniques: visual, thermometers |
|
|
What is a Colles' fracture?
|
Fracture to the distal radius
|
|
|
What splint is used for a 5-year old child with spastic quad CP how shows bilateral thum-in-palm deformities?
|
A neoprene hand-based splint w/thumbs in opposition
|
|
|
A 15 year-old with arthrogryposis undergoes serial casting of the right wrist, with weekly cast changes. After four weeks, upon cast removal, the therapist notes both a small open area 1/4cm. by 1/4cm. and a red rash over the ulnar styloid. The therapist's best response is to?
|
-refer the individual to the physician to dx the finding
|
|
|
What is Arthrogryposis?
|
Arthrogryposis, or arthrogryposis multiplex congenita, comprises nonprogressive conditions characterized by multiple joint contractures found throughout the body at birth
|
|
|
An individual diagnosed with bipolar disorder of the manic type, begins an OT activity group. For the first experience in the group setting, the therapist should suggest:
|
A structured project, w/ easily-completed steps to increase self-esteem (i.e.: making a leather wrist band w/client's name)
|
|
|
What are the charateristics of individuals with oppositional defiant disorder?
|
Impulse contral, attention span, and short-term memory
|
|
|
Several adolescents with behavior problems attend an after-school program in a mental health outpatient program. They work at an egocentric-cooperative level in a group dealing with issues related to peer pressure. The participants would be most likely to:
|
Focus on the group tasks rather than the feelings of the participants.
|
|
|
A five year-old with moderate spastic cerebral palsy works on ambulation with a walker in physical therapy. The OT evaluation reveals problems in lower extremity dressing, transitional skills, self-feeding, and grasp and release skills. To facilitate the child's goal of ambulation, the occupational therapist elects to work on:
|
-donning and doffing shoes and socks in bench sitting with one leg externally rotated and placed on the opposite knee: encourages dynamic trunk balance, LE external rotation, and dissociation
|
|
|
Ten members of the community resource group are not working well together and show decreased levels of trust. The COTA's goal is to enhance the level of cohesiveness in the group. The best choice for the COTA is to:
|
Verbally reinforce the goals and purposes of the group.
|
|
|
In a mature group level, what is the role of the therapist?
|
To act as a member of the group
|
|
|
In a cooperative level, what is the role of the therapist?
|
-The therapist intervenes to promote cohesiveness and group problem-solving
|
|
|
An individual functions at level five according to the Allen Cognitive Test. The highest level task that the individual can perform is to:
|
-Carry out a task with three familiar steps and one new step
|
|
|
An individual with schizophrenia continues to experience periods of hallucinations after two changes in medications. During the OT project group, the individual begins to actively hallucinate. The COTA should:
|
-Redirect attention back to the project, and reinforce all misinterpretations of enviromental noises and events, use a calm tone, focus on reality
|
|
|
What functional activity can a person at Allen's Cognitive Level II do?
|
Poor imitation of posture
|
|
|
What functional activity can a person at Allen's Cognitive Level III do?
|
Sand wood
|
|
|
What functional activity can a person at Allen's Cognitive Level IV do?
|
Matching colors of clothing
|
|
|
What functional activity can a person at Allen's Cognitive Level V do?
|
Understand cause and effect
|
|
|
In an activity group of an inpatient unit, how should activities be done?
|
On an inpatient unit, activities should be structred, easily completed in one session, and provide a concrete result to reinforce reality
|

