![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
86 Cards in this Set
- Front
- Back
|
Simple/closed fracture
|
Fracture in which the skin surface is not penetrated.
|
|
|
Compound/open fracture
|
Fracture in which the skin surface is penetrated or broken and creates an open wound.
|
|
|
Spiral/torsion fracture
|

A fracture in which at least one part of the bone has been twisted.
|
|
|
Oblique fracture
|

A fracture in which the break has a curved or sloped pattern.
|
|
|
Compression fracture
|

A fracture in which the bone collapses on itself, seen in vertebral fractures.
|
|
|
Avulsion fracture
|

A fracture in which a fragment of bone is separated from the main bone mass.
|
|
|
Transverse fracture
|

A fracture at a right angle to the bone's axis.
|
|
|
Greenstick fracture
|

An incomplete fracture in which the bone is bent. This type occurs most often in children.
|
|
|
Comminuted fracture
|

A fracture in which the bone fragments are driven into each other.
|
|
|
Linear/fissure fracture
|

A fracture that is parallel to the bone's long axis.
Most common type of skull fracture and may not require any intervention. |
|
|
Displaced fracture
|
A fracture in which there is a loss of alignment.
Defined by the abnormal position of the distal bone fracture in relation to the proximal bone. |
|
|
Angulation displacement
|
Medial angulation - varus
Lateral angulation - valgus Ventral, volar and/or dorsal should also be used. |
|
|
Rotation displacement
|
Term usually used on long bones to describe internal or external rotation of the distal segment compared to the proximal.
|
|
|
Overlapped displacement
|
A fracture resulting in overlapping displacement of the two segments.
|
|
|
Distracted fracture
|
A fracture resulting in increased overall bone length, due to the distraction (widening) of the bone components.
|
|
|
Depressed skull fracture
|
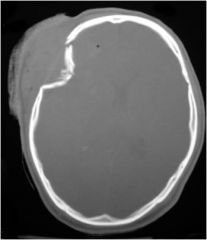
Fractured pieces of bone pushed inward.
|
|
|
Diastatic skull fracture
|
Fracture in which the sutures are widened, usually occurs in children under 3 years old.
|
|
|
Basilar skull fracture
|
Fracture of the bone at the base of the skull.
|
|
|
Battle's sign
|

Panda bear or raccoon eyes appearance that often occurs with a basilar skull fracture.
|
|
|
Multiple myeloma
|
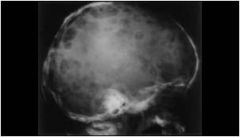
A plasma cell cancer that involves multiple organ systems. Bone pain is common due to destruction or osteolytic lesions.
|
|
|
Orbital/blowout fracture
|

Fracture of walls or floor of orbit, pushing contents into sinuses, trapping or damaging intraorbital.
Water's view (x-ray) or CT to diagnose. Caused by blunt trauma (fist fight). |
|
|
What are the most common cervical spine fracture x-ray views?
|
AP, lateral, odontoid
|
|
|
What is required to obtain a good cervical spine x-ray?
|
Adequate film
Alignment Bony landmarks Cartilaginous space Disc space Soft tissues |
|
|
What constitutes an adequate c-spine x-ray?
|
All 7 cervical vertebrae must be visible, including C7 on a lateral view.
Must also have correct density and show soft tissue as well as bony structures. |
|
|
What are the lines of alignment on a lateral c-spine x-ray?
|

Anterior vertebral line (r) -anterior vertebral bodies
Posterior vertebral line (br) -posterior vertebral bodies Spinolaminar line (g) -posterior spinal canal Posterior spinous line (bl) -tips of spinous processes Misalignment indicates ligament injury or fracture; immobilize the patient. |
|
|
What are the lines of alignment on an AP c-spine x-ray?
|

Should have a "bamboo appearance.
Height of vertebral bodies and joint spaces should be equal. Spinous processes should be midline and aligned. Misalignment indicates dislocation. |
|
|
C-spine bony landmarks
|

Pedicles - L/R should superimpose on lateral
Facets - double cortical lines, distance should be equal at all levels Lamina - posterior poorly seen on lateral Spinous processes - increase in size - Vertebral bodies should line up in arch - Each body should be rectangular, equal in size - Anterior height should equal posterior height |
|
|
What is the significance of cartilage on a c-spine x-ray?
|

Predental space should not be greater than 3 mm in adults and 5 mm in children.
Causes of an increased space include fracture. CT or MRI is recommended. |
|
|
What is the significance of disc space on a c-spine x-ray?
|

Disk spaces should be:
- symmetric - equal in height at anterior and posterior margins - equal height at all levels Degenerative disease in older patients may lead to spurring and loss of disc height. |
|
|
What constitutes an adequate odontoid view?
|
Should be able to view the entire odontoid (dens) and lateral borders of C1-C2.
Should have uninterrupted cortical margins blending with body of C2 (bony margin). |
|
|
What should the proper odontoid alignment be?
|
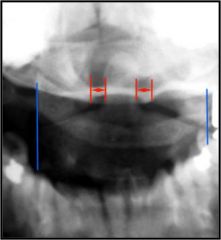
Occipital condyles should line up with the lateral masses and superior articular facet of C1.
Distance from dens to lateral masses of C1 should be equal bilaterally. If head is tilted, the vertebrae should be shifted out on the other side. Tips of lateral mass of C1 should line up with the lateral margins of the superior articular facet of C2. |
|
|
What soft tissues can be seen on a c-spine x-ray?
|

Nasopharyngeal space (C1) – 10 mm
Retropharyngeal space (C2-C4) – 6mm Retrotracheal space (C5-C7) – 22 mm --- 14 mm (children) |
|
|
Jefferson fracture
|

A fracture of C1 (atlas) anterior and posterior.
Caused by axial compression with or without extension or force. Posterior arch is more common and results from hyperextension, such as diving into a pool. |
|
|
Hangman's fracture
|

A fracture of the C2 (axis) pars interarticularis as a result of hyperextension with or without axial loading, as in a motor vehicle accident (MVA).
Anterior movement (spondylolisthesis) of C2 results. |
|
|
Clavicle fracture
|

Typically due to a fall on the arm or onto lateral shoulder.
|
|
|
Acromioclavicular (AC) dislocation
|

Typically due to direct downward blow to the tip of the shoulder (football, wrestling, hockey).
|
|
|
Shoulder/humerus fracture
|
Can occur at proximal end, midshaft or at distal epicondyle (medial/lateral).
|
|
|
Shoulder dislocation
|

Typically occurs anterior and inferior. Caused by external rotation abduction force on humerus, or posterior to posterior-lateral blow.
|
|
|
Shoulder osteoarthritis
|

Typically need three views - AP, axillary and lateral
|
|
|
Radius fracture
|

Typically due to fall with outstretched hand. Presents with pain and difficulty with supination/pronation.
|
|
|
Colles' fracture
|

Distal radius fracture with dorsal displacement of the hand/wrist caused by a fall on outstretched arm.
|
|
|
Nursemaid's elbow
|

Dislocation of the radial head.
|
|
|
Ulnar fracture
|

Mechanism is direct impact, as with a fall.
|
|
|
Elbow dislocation
|

Usually caused by fall on the outstretched arm, most commonly resulting in posterior displacement of the olecranon to the humerus. Arm is shortened and held flexed.
|
|
|
Boxer's fracture
|

Result of axial loading of the 4th and 5th metacarpal, as in hitting another person or hard object.
|
|
|
Scaphoid fracture
|

Can develop avascular necrosis if fracture occurs at the proximal pole.
|
|
|
Pelvis fracture
|

Result of direct trauma, can cause nerve blood vessel, bladder or bowel complications.
|
|
|
Hip/femur fractures
|
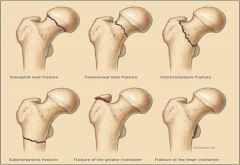
Most common in patients over 50 years of age.
Typically results from a fall. Can involve femoral neck or trochanter. |
|
|
Femoral neck fracture
|
The involved extremity is externally rotated and slightly shortened.
|
|
|
Femur trochanteric fracture
|
Intertrochanteric - involved extremity may be internally rotated and slightly shortened. More common at a later age than femoral neck fracture.
Greater trochanteric fracture |
|
|
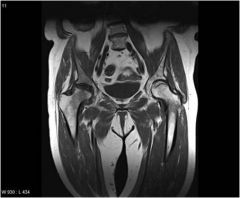
Hip dislocations
|

Posterior dislocation is more common.
Typically shortening, adduction and internal rotation of the extremity is seen. |
|
|
Slipped capital femoral epiphysis
|

A disorder in adolescents in which a fracture of the growth plate results in separation of the ball of the hip joint from the femur.
- More common in males - Causes painful limp and limited hip internal rotation and abduction - Change in ROM is usually diagnostic |
|
|
Avascular necrosis of the hip
|
Death of the bone tissue (necrosis) due to decreased or interrupted blood supply resulting in bone collapse and deterioration of the articular surface.
|
|
|
What three views should be obtained when evaluating the knee?
|
AP, lateral and sunrise/skyline view
|
|

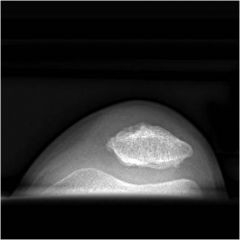
What diagnosis would you make based on this x-ray?
|
Osteoarthritis in knee
|
|
|
Chondromalacia patella
|
Abnormal tracking of the patella leading to inflammation and degeneration of the patella.
|
|
|
Tibia fractures
|

Can occur on plateau, shaft or malleolus.
|
|
|
Fibula fractures
|

Can occur on head, shaft or malleolus.
|
|
|
Ankle/foot malleolar fracture
|

Bimalleolar - both medial and lateral involved
Trimalleolar - medial, lateral and distal tibia involved |
|
|
Calcaneal fracture
|

Typically due to fall or jump from tall height.
|
|
|
What are the most important determinants in the analysis of a potential bone tumor?
|
- Morphology
--- well-defined or ill-defined osteolytic, sclerotic - Age of patient - most important - X-ray is most useful exam |
|
|
What morphology do most bone tumors have?
|
Osteolytic
|
|
|
What is the most reliable indicator in determining is lesions are benign or malignant?
|
Zone of transition between the lesion and adjacent normal bone - well-defined or ill-defined.
|
|
|
Criteria to diagnose Aneurysmal Bone Cyst (ABC)
|
- Well-defined osteolytic
- 10-20 years old |
|
|
Criteria to diagnose Chondromyxoid Fibroma (CMF)
|
- Well-defined osteolytic
- 10-20 years old |
|
|
Criteria to diagnose Eosinophilic Granuloma (EG)
|
- Well-defined or ill-defined osteolytic or sclerotic
- 0-20 years old |
|
|
Criteria to diagnose Giant Cell Tumor (GCT)
|
- Well-defined or ill-defined osteolytic
- 20-40 years old |
|
|
Criteria to diagnose Fibrous Dysplasia (FD)
|
- Well-defined osteolytic or sclerotic
- 10-20 years old |
|
|
Criteria to diagnose Hyperparathyroidism with Brown Tumor (HPT)
|
- Well-defined osteolytic
- 20-40 years old |
|
|
Criteria to diagnose Non-Ossifying Fibroma (NOF)
|
- Well-defined osteolytic
- 10-20 years old |
|
|
Criteria to diagnose Simple Bone Cyst (SBC)
|
- Well-defined osteolytic
- 0-20 years old |
|
|
Criteria to diagnose multiple myeloma
|
- Well-defined or ill-defined osteolytic
- Over 40 years old |
|
|
Small zone of transition
|
Results in a sharp, well-defined border and is a sign of slow growth. A sclerotic border especially indicates poor biological activity.
|
|
|
Wide zone of transition
|

An ill-defined border with a broad zone of transition is a sign of aggressive growth and is a feature of malignant tumors.
Infections and eosinophilic granuloma may mimic a malignancy. |
|
|
What is a periosteal reaction?
|
Non-specific reaction occurs when periosteum is irritated, resulting in benign or aggressive type.
Benign is seen with benign tumors or trauma. Aggressive is seen with malignancy, infections or eosinophilic granuloma. |
|
|
How do you detect a benign periosteal reaction?
|

Results in a thick, wave and uniform callus formation resulting from chronic irritation.
If slow-growing, the periosteum has time to lay down thick new bone and remodel it into a more normal-appearing cortex. |
|
|
How do you detect an aggressive periosteal reaction?
|

Multilayered, lamellated or demonstrates bone formation perpendicular to the cortical bone, may be spiculated and interrupted.
Codman's triangle may be present, referring to an elevation of periosteum away from the cortex and forming an angle where elevated periosteum and bone come together. |
|
|
Osteoid osteoma
|

Tumor of unknown etiology that is composed of osteoid and woven bone, usually smaller than 1.5 cm diameter. Can occur in any bone, but in 2/3 of patients, the appendicular skeleton is involved.
Classic presentation - Focal bone pain at site of tumor - Pain worsens at night, increases with activity - Pain dramatically relieved with aspirin - X-ray shows round lucency, with dense sclerotic central nidus |
|
|
Osteochondroma
|

Abnormal growth that forms on the surface of a bone near the growth plate that develops during childhood or adolescence.
It is an outgrowth of the growth plate and consists of both bone and cartilage. |
|
|
Enchondroma
|

Intramedullary cartilaginous cysts commonly found in the small bones of the hands and feet. Grow in childhood and remain present in adulthood, often found in patients 10-20 years old.
On x-ray, appears as small (less than 5 cm) lobe-shaped or oval with well-defined margins. Larger lesions have lucent defect with endosteal scalloping (erosin) and cortex is expanded and thinned. Calcifications can range from punctuate to rings. |
|
|
Aneurysmal Bone Cyst (ABC)
|

Lesions are located on the surface of bone, metaphysis and epiphysis and usually occurs in 20-30s. X-rays show striking expansile lesion with internal septae or longitudinal striations. If highly expansile and at end of bone, it may be referred as a "finger in a balloon."
|
|
|
Osteosarcoma
|

Peak age is 18-20 and males more commonly affected.
Most common presentation is pain and a mass, occurring near a joint. Located in metaphysis of long bones, appears as a mixed sclerotic and lytic lesion, that may permeate bone and nearby cortex, causing a soft tissue mass and periosteal reaction. Half of lesions are near knee joint. Has a "sunburst pattern" appearance. |
|
|
Chondrosarcoma
|

Slower growing than osteosarcomas and tumor produces cartilaginous matrix.
Metaphysis is most common location in long bones. More common in people over 60. Presents with pain and swelling in a bone. Fusiform, lucent defect with scalloping of the inner cortex and periosteal reaction. Extension into the soft tissue may be present. |
|
|
Ewing's sarcoma
|

Most common in pelvis, femur, tibia, and humerus, typically metaphysis.
More common in males and presents in childhood. Usually lytic and central, endosteal scalloping is often present. Lamellated or "onion skin" periosteal reaction, caused by and splitting and thickening of the cortex by tumor cells, followed with a "moth-eaten" or mottled appearance and extension into soft tissue. |
|
|
Benign bone tumors
|
Osteoid osteoma
Osteochondroma Enchondroma Aneurysmal bone cyst |
|
|
Malignant bone tumors
|
Osteosarcoma
Chondrosarcoma Ewing’s Sarcoma |

