![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
40 Cards in this Set
- Front
- Back
|
What are the 6 clues of a possible/probable fracture?
|
1. Hx of the circumstances of the injury (fall, forceful blow, etc.)
2. Pain 3. Obvious Deformity 4. Crepitus upon palpation 5. Loss of sensation distal to the injury 6. X-ray reveals the injury |
|
|
What are 7 things that keep a fracture from healing?
|
1. Movement
2. Fragments not being aligned 3. Decreased arterial blood supply from the injury 4. Excess edema 5. Infection from an opening in the skin of bloodborne from another infection 6. Decreased new bone growth, bleeding 7. Use of steroids (decreases inflammation that is the first step required for the healing process) |
|
|
What are the s/s of Compartment Syndrome?
|
**This is an EMERGENCY!
~Edema in the compartment ~Reduced arterial blood flow; pulses may still be present since arterial flow is the last to be obstructed due to pressure ~Severe PAIN that is not relieved by narcotics! Includes a burning sensation and numbness ~Rhabdomyolysis and decreased urine output |
|
|
What is Rhabdomyolysis?
|
Rapid muscle ischema causes massive amounts of protein (from the myosin) to go to the kidneys and plug up the glomerulus. This prevents potassium from being excreted, also.
|
|
|
What is done to treat Compartment Syndrome?
|
A Fasciotomy is performed to relieve the pressure. An incision is made down the length of the wound, which allows for a return of arterial blood to the site. Keep the injured area at heart level
|
|
|
What should the pressure be within a muscle/artery compartment? At what point does it damage blood vessels and at what point does necrosis begin?
|
Normal - 8 mm Hg
30-40 mm Hg damages blood vessels At 65 mm Hg necrosis starts |
|
|
What does a fat embolism come from concerning skeletal trauma? Where does it usually go and what irritates tissue at the site it lodges in?
|
Fat globules can be released from bone marrow when there is a fx of a long bone, multiple fractures, and especially with crush injuries. They usually turn into pulmonary embolisms and they break down into fatty acids that irritate the alveoli.
|
|
|
What syndrome does a fat embolism cause? What are the sx? Who is most at risk and what is the mortality rate?
|
It causes ARDS (adult respiratory distress syndrome).
The sx are: ~Altered mental status ~Low O2 sat ~Tachycardia r/t hypoxia ~Petechia over neck, arms, chest, and abdomen Mortality is 50% |
|
|
What are the two types of thromboembolitic complications of fractures and what are they related to? Who is at the highest risk?
|
#1 is DVT, #2 is PE r/t trauma, surgery, and immobility.
Increased risk: ~Previous DVT ~Smoker ~Obesity ~Heart Disease |
|
|
What can we do to prevent thromboembolitic complications from fractures?
|
~Administer anticoagulants
~Get the pt walking ~Good hydration ~Ted Hose ~Stool softener (straining increases venous pressure which dilates leg veins and the clot is released) |
|
|
What would an infection in the bone be called? What increases the risk of a pt getting an infection from fx complications?
|
Osteomyelitis
Increased risk from: ~Open fractures ~Implanted hardware ~Another infection that is present (ex. UTI, otitis media, infection of adjacent soft tissue, etc.) ~Decreased blood flow, which can lead to bone necrosis (bacteria can lodge in small vessels and prevent WBCs and antibiotics to get to the infection site) ~Can get drug-resistant bacteria present ~Can get an infection from avascular necrosis, hip fx's, injury to blood supply, etc |
|
|
What would the assessment criteria be for a person with an infection of the bone be? What are the treatments?
|
Assessments:
~Fever of 101° ~Bone pain at the site of injury ~Leukocytosis Treatments: ~Long-term antibiotics ~Surgical debridement since necrotic bone won't heal |
|
|
What is a Fracture Blister, what can it lead to, and how can we prevent it?
|
~It is extensive edema that separates the epidermis from the dermis
~It can lead to fx and nonunion ~Prevention can be through elevation to reduce edema and immobilization |
|
|
What 4 kinds of external fixation devices are there? Are they both used extensively? Why or why not?
|
~Cast or immobilizer - can use foam and metal supports, plaster, fiberglass, etc. Can not get plaster wet!
Traction - Can be skeletal (pins attached to the bone) or skin (a device is fitted to the extremity and the traction pulls on it). Not used much due to immobilization problems. Braces - Fit to a body part, like the thorax for spinal fx's Pins & a frame - Pins stick out through the skin from the bone and attach to an external frame - Need good skin care around pin sites! |
|
|
What is done for internal fixation?
|
ORIF - Open reduction & internal fixation - Insertion of hardware that stays in the body.
|
|
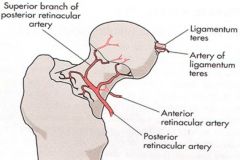
Label these hip arteries and one ligament
|
|
|
|
What is a problem that can result from a hip fx regarding circulation? What are fx's called when they are outside the joint vs inside the joint?
|
One problem concerning circulation is that the head of the femur loses it's blood supply.
Extracapsular - Outside the joint Intracapsular - Inside the joint |
|
|
What are 4 strong indicators that there may be a hip fracture?
|
1. The affected leg turns outward
2. The affected leg is shorter 3. Inability to put weight on that leg 4. Pain with swelling |
|
|
What are the 6 instructions given to pts who have just had a hip fx fixed?
|
1. Avoid hip flexion >60° for 10 days
2. Avoid hip flexion >90° for 2 months 3. Avoid adduction beyond midline for 2 months 4. Use partial weight-bearing supported by a walker, cane, etc 5. Don't position pt on the side of the surgery for comfort and pressure concerns 6. Keep a pillow between the knees to prevent crossing midline |
|
|
How do you assess for neurovascular status in a pt with a MS injury?
|
CMS - Mneumonic for 1st three
1. Circulation - Pulses, cap refill, temperature (check both limbs at once!) 2. Movement - Is there any distal to the site of the injury? 3. Sensation - Can the pt feel light sensation from a cotton ball distal to the injury? 4. Is there a lot of swelling and pain? |
|
|
What are 5 interventions for a fracture?
|
1. Immobilization
2. Ice to decrease edema (don't use for compartment syndrome!) 3. Prevent infection (use strict aseptic technique to open fx's) 4. Limit steroids to allow for edema, which is the first stage of healing 5. Prevent DVT through the use of stool softeners, SCDs, blood thinners, etc. |
|
|
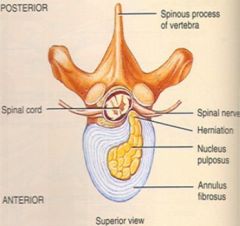
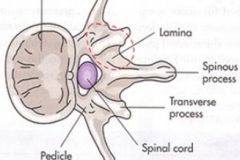
What is DJD (Degenerative Joint Disease)? What levels is it commonly located at? What can cause it and how is it fixed?
|
~It is where the Nucleus Pulposus herniates through the Annulus Fibrosis and pushes on the spinal cord and nerves
~It is commonly seen at levels C4-C7 and L4-S2. ~Results from trauma, carrying things that are too heavy, or even twisting that causes the muscles around the spine to cramp up ~A laminectomy is performed to get to the herniation and remove it |
|
|
What are the results of DJD? What are dermatomes? What is a general rule regarding dermatomes in the lower limbs?
|
DJD can result in:
~Pain along corresponding dermatomes ~Muscle weakness ~Paresthesia Dermatomes are the areas of the body that are served by the major nerves from the spine In general, the front of the legs are supplied by the lumbar nerves and the posterior is served by sacral nerves |
|
|
What are the 5 postop care principles for DJD?
|
1. Monitor neuro function - Sensation and muscle strength in toes
2. Check dressing for bleeding 3. Log roll the pt 4. No twisting or bending! 5. Fit a brace or corset to prevent twisting if ordered by Dr |
|
|
What are the characteristics of DJD osteoarthritis? What are the risk factors?
|
~Not inflammatory, even though it ends in "-itis"
~Due to 'wear and tear' ~Articular cartilage degenerates - first it becomes rough, frayed, and cracked, then it is worn away and there is bone-on-bone in the joint ~Subchondral bone becomes thickened ~Osteophytes develop (bone spurs) ~Risk factors are obesity, high impact activities, etc. |
|
|
Concerning osteoarthritis (OA), what are the nodules called that form at the distal joint of a finger, and what are the nodules called at the middle joint?
|
Distial - Heberden's nodes
Middle - Bouchard's nodes |
|
|
|
|
|
What are the risk factors for developing osteoarthritis? What are the clinical manifestations?
|
Risk factors:
~Obesity ~Genetics ~Over the age of 60 Manifestations? ~Pain relieved by rest ~Morning stiffness lasting <1 hour ~Joint swelling, increase in synovial fluid ~Decreased ROM r/t muscle spasms, osteophytes, loss of cartilage |
|
|
What is the treatment for osteoarthritis?
|
~NSAIDs to decrease inflammation
~Unload the joint using a cane, walker, weight loss, etc. ~Arthrodesis - Joint fusion ~Arthroplasty - Joint replacement |
|
|
What are the down sides to having a joint replaced?
|
Arthroplasty
~Finite life span - 10-20 years ~They can wear, break, loosen, get infected, etc. ~Revision has more blood loss and has a greater risk of infection |
|
|
What is the postop care for joint replacement?
|
~Prevent DVT using heparin, warfarin, LMWH, foot pumps, ambulation
~Prevent infection that can result from multiple channels in bone that can harbor bacteria, and from the increased amount of time required for the surgery ~Decrease pain and swelling using ice and medicate prior to PT and OT |
|
|
What treatments are no longer recommended for post op care of pts with a joint replacement?
Why is there a higher risk for DVT in pts that have just had a joint replacement? |
~Ted hose or elastic socks are not recommended
~Risk of DVT comes from tourniquets that are placed above the knee for TKA, and femoral vein compression for THA |
|
|
What post op care is specific to a hip replacement?
|
Prevent dislocation!!
~This would result in a sudden pop, pain, loss of movement ~Do not cross legs over midline ~Do not flex the joint past 90° - Use an elevated toilet seat, etc. |
|
|
What post op care is specific to a knee replacement?
|
~Do not kneel!! This is for the rest of the pt's life
~No pillow behind the pt's knee to prevent compression of the vessels ~Can use continuous passive motion (CPM), if ordered |
|
|
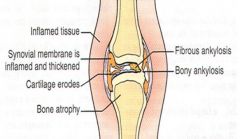
What is Rheumatoid Arthritis (RA)?
|
~It is a chronic inflammatory autoimmune collagen disease
~It results in a symmetric inflammations of synovial membranes ~There is a thickening of membranes ~Increased synovial exudate and swelling |
|
|
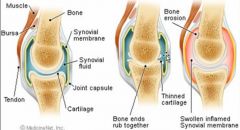
Normal, OA, RA
|
|
|
What are the symptoms of RA?
What are the treatments? |
Symptoms:
~Stiffness of the joint all of the time ~Pain with movement and rest ~Loss of motion ~Loss of strength ~Joint can be pulled into an abnormal position due to inflammation Treatment: ~Relieve sx - Heat, ice ~Prevent joint destruction - Meds ~Maintain function - PT/OT, braces, splints, assistive devices ~Swim programs for severe RA |
|
|
What are some medications available for tx of RA?
|
~General pain meds
~Steroids or inflammation ~Methotrexate - Inhibits folic acid & DNA synthesis of inflammatory cells ~Immunosuppressants - Imuran, Cytoxan ~TNF - alpha antagonist - Enbrel |
|
|
What is osteoporosis and what are the risk factors?
|
~It is the gradual thinning of bones that leads to increased risk of fx. It usually presents in the hips, spine, and wrists. A bump or strain can cause a fx.
Risk Factors: ~Female over 50 (post menopausal) ~Family hx ~Thin or anorexic ~Low lifetime intake of calcium ~Cigarette smoking ~Inactive lifestyle |
|
|
What are some medications and recommended lifestyle changes for osteoporosis?
|
Medications:
~Fosamax ~Boniva ~Actonel ~Calcitonin - Miacalcin Exercise: ~Weight-bearing - walking, jogging, dancing, etc. Diet: ~Supplemental calcium 1200-1500 mg/day divided into 3 doses ~Milk, yogurt, ice cream, cheese, tofu, salmon, sardines, leafy green vegetables Stop smoking! |

