![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
55 Cards in this Set
- Front
- Back
|
What is soft tissue?
|
- Non-epithelial tissue (= mesenchymal)
- Excluding bone, cartilage, CNS, hematopoietic, and lymphoid tissues) |
|
|
How are mesenchymal tumors classified?
|
According to the tissue they "recapitulate" (imitate, e.g., fat, fibrous tissue, vessels and nerves)
|
|
|
How common are soft tissue sarcomas (malignant mesenchymal tumors)?
|
Rare, ~1% of all cancers
|
|
|
How common are benign soft tissue tumors?
|
Outnumber sarcomas (malignant) 100:1
|
|
|
What do soft tissue tumors arise from?
|
Pluripotent mesenchymal stem cells (NOT d/t malignant transformation of mature mesenchymal cells)
|
|
|
What is the cause of most soft tissue tumors?
|
- Most are unknown
- Rarely, some are associated with radiation, burn injury, toxins, or trauma - Small minority associated with genetic syndromes - Majority occur sporadically |
|
|
What is the cause of Kaposi Sarcoma?
|
Human Herpesvirus 8
|
|
|
What genetic syndromes are associated with soft tissue tumors?
|
- Neurofibromatosis Type 1 --> Neurofibroma or Malignant Schwannoma
- Gardner Syndrome --> Fibromatosis - Li-Fraumeni Syndrome --> Soft Tissue Sarcoma - Osler-Weber-Rendu Syndrome --> Telangiectasia |
|
|
Where in the body do soft tumors appear?
|
Any location, but ~40% occur in lower extremities, especially the thigh
|
|
|
How does the frequency of sarcomas relate to age?
|
- Increased incidence with age (15% in children)
- Some sarcomas appear in certain age groups: - Rhabdomyosarcoma (childhood) - Synovial sarcoma (young adulthood) - Liposarcoma and pleomorphic or undifferentiated sarcomas (later adult life) |
|
|
What features of a soft tissue sarcoma influence the prognosis?
|
- Diagnostic classification (histology, IHC, EM, cytogenetics, molecular genetics)
- Grading - Staging - Location |
|
|
How are soft tissue sarcomas graded?
|
- Scale of I - III
- Based on degree of differentiation, average number of mitoses per high-power field, cellularity, pleomorphism, and extent of necrosis (reflects rate of growth) - Helps determine prognosis (mitotic counts and necrosis most important factors) |
|
|
How does the staging of soft tissue sarcomas affect the prognosis?
|
- Size: <5 cm, 30% chance of metastases; >20 cm, 80% of metastases
- Depth (above or under fascia) - Stage (I-IV) |
|
|
How does the location of a soft tissue sarcoma affect the prognosis?
|
- Tumors from superficial locations (e.g., skin) have better prognosis than deep lesions
|
|
|
How are soft tissue sarcomas treated?
|
- Wide surgical excision (frequently limb sparing)
- Irradiation and systemic therapy reserved for large high-grade tumors |
|
|
What are the types of tumors of adipose tissue?
|
- Lipomas (benign)
- Liposarcomas (malignant) |
|
|
What is the most common soft tissue tumor of adulthood?
|
Lipomas (benign)
|
|
|
What kind of tumor is a lipoma? Who is most likely to get it?
|
- Tumor of adipose tissue
- Most common soft tissue tumor of adulthood |
|
How many lesions typically occur in a lipoma?
|
Solitary lesions (most) - if there are multiple lipomas this suggests rare hereditary syndrome
|
|
|
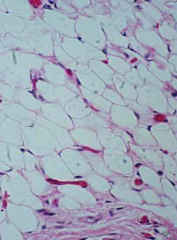
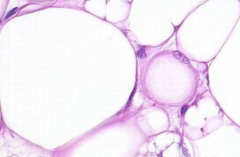
What are the characteristics of lipomas?
|
- Most are mobile, slowly enlarging, painless masses (except angiolipomas - local pain)
- Conventional lipomas are soft, yellow, and well-encapsulated - Histologically, consist of mature white fat cells w/ no pleomorphism - Conventional: 12q14-q15 |
|
How are lipomas treated?
|
Complete excision is usually curative
|
|
|
What kind of tumor is a liposarcoma? Who is most likely to get it?
|
- Malignant neoplasm with adipocyte differentation
- One of the most common sarcomas of adulthood (40s-60s) |
|
Where do liposarcomas frequently occur?
|
Deep soft tissues of proximal extremities (e.g., thigh) and retroperitoneum
|
|
|
How is the prognosis of liposarcoma dependent on type?
|
- Well-differentiated is relatively slow growing - more favorable outcomes
- Myxoid/round cell type more aggressive - Pleomorphic variant is usually most aggressive and may metastasize (to lungs) * All recur locally unless adequately excised |
|
|
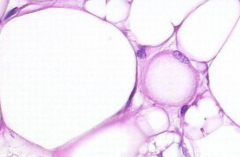
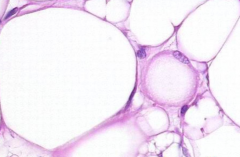
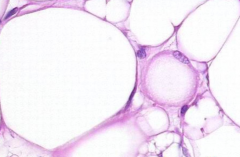
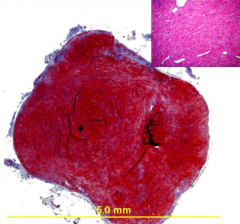
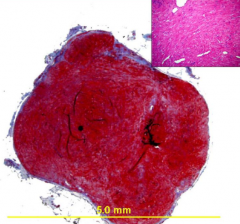
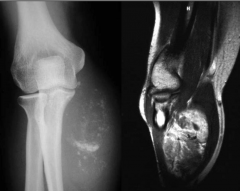
How does the appearance of lipomas compare to liposarcomas?
|
- Lipomas are more homogenous
- Liposarcomas are more heterogenous (as shown in image) |
|
|
What chromosomal abnormalities are associated with liposarcomas?
|
- Well-differentiated (WD-LPS) = supernumerary ring chromosomes (amplification of 12q14-q15, containing MDM2 --> binds and degrades p53)
- Myxoid/Round LPS = t(12;16)(q13;p11) --> interferes with adipocyte differentiation |
|
|
What are lipoblasts?
|
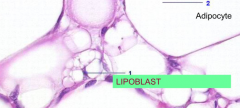
Cells that indicate fatty differentiation in soft tissue tumors; contain cytoplasmic lipid vacuoles that scallop the nucleus
(helpful for identifying poorly differentiated tumors as liposarcomas) |
|
|
What are "Pseudosarcomatous Proliferations"?
|
- Reactive non-neoplastic lesions that develop in response to some form of local trauma or are idiopathic (unknown cause)
- Develop suddenly and grow rapidly - Show hypercellularity, mitotic activity, and primitive appearance that mimics sarcomas |
|
|
What are the two types of Pseudosarcomatous Proliferations?
|
- Nodular Fasciitis
- Myositis Ossificans |
|
|
Where does Nodular Fasciitis occur? What kind of growth is it?
|
- Occurs in deep dermis, subcutis, or muscle (several cm w/ poorly defined margins)
- Pseudosarcomatous proliferation (fibroblastic) |
|
|
When/where does Myositis Ossificans occur? What kind of growth is it?
|

- Proximal extremities of young adults (following trauma >50% of time
- Pseudosarcomatous proliferation (fibroblastic) that contains metaplastic bone (eventually entire lesion ossifies and intratrabecular spaces fill w/ bone marrow) |
|

What does Myositis Ossificans resemble?
|
Extraskeletal Osteosarcoma
|
|
|
What are fibromatoses? Types?
|
- Fibroblastic proliferations
- Superficial fibromatoses - superficial fascia - Deep fibromatoses - abdominal wall and muscles of trunk and extremities and within abdomen |
|
|
What are some examples of superficial fibromatoses?
|
- Palmer = Dupuytren contracture
- Plantar - Penile = Peyronie disease |
|
|
What are some examples of deep-seated fibromatoses?
|
- Desmoid Tumors
- Component of Gardner syndrome |
|
|
What are Desmoid Tumors?
|
- Deep Fibromatosis
- Behavior lies between benign fibrous tumors and low-grade fibrosarcomas - Frequently recur after incomplete excision - Most frequent in teens to 30s - Mutations in APC or Beta-Catenin |
|
|
What is associated with mutations in APCs or Beta-Catenin genes?
|
Desmoid tumors / deep fibormatosis
|
|
|
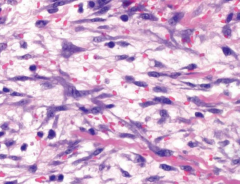
What kind of tumors are fibrosarcomas? Who do they affect and where?
|
- Malignant tumors of fibroblasts
- Affect adults mostly in deep tissues of thigh, knee and retroperitoneum |
|
|
How aggressive of tumors are fibrosarcomas?
|
- Aggressive
- Recur in >50% of cases after excision - Metastasize in >25% of cases (usually to lungs) |
|
|
What is the most common neoplasm in women?
|
Uterine leiomyomas (benign smooth muscle tumors)
|
|
|
What are the characteristics of leiomyomas?
|
- Benign smooth muscle tumors
- Commonly in uterus or skin - Usually <1-2cm - Solitary lesions are easily cured - Multiple tumors may be difficult to cure |
|
|
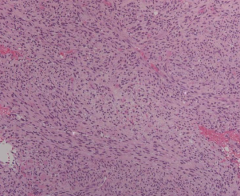
How common are leiomyosarcomas? Who do they affect?
|
- 10-20% of soft tissue tumors
- Adults, females > males |
|
|
Where do leiomyosarcomas occur?
|
- Skin
- Deep soft tissues - Extremities and retroperitoneum |
|
|
What is the typical prognosis of leiomyosarcomas?
|
- If superficial, usually small w/ good prognosis
- If deep in retroperitoneum, usually large and not capable of complete excision (local extension and metastatic spread) |
|
|
What is the most common soft tissue sarcoma of childhood and adolescence?
|
Rhabdomyosarcoma
|
|
|
Where does Rhabdomyosarcoma occur and in who?
|
- Commonly in head/neck or GU tract (usually at sites w/ little if any normal skeletal muscle)
- Commonly in those <20 yo |
|
|
What are the three subtypes of rhabdomyosarcoma?
|
- Embryonal (49%)
- Alveolar (31%) - Pleomorphic (20%) |
|
|
What are the characteristics of Embryonal Rhabdomyosarcoma?
|
- 49% of Rhabdomyosarcoma
- More frequent <10 yo - Head and neck (orbit and parameninges) - GU tract - Deep soft tissues of extremities, pelvis and retroperitoneum - Variants: sarcoma botryoides, spindle cell, anaplastic |
|
|
What are the characteristics of Alveolar Rhabdomyosarcoma?
|
- 31% of Rhabdomyosarcomas
- More frequent between 10 and 25 yo - Deep soft tissues of extremities - Less often in head/neck, perineum, pelvis, or retroperitoneum - 80-85% of cases have t(2;13)/PAX3-FKHR or t(1;13)/PAX7/FKHR translocations |
|
|
What are the tumors of unknown histogenesis?
|
- Synovial sarcoma
- Epithelioid sarcoma - Aloveolar soft part sarcoma |
|
|
How common are synovial sarcomas? Who do they affect?
|
- 5-10% of soft tissue sarcomas
- Affect young adults, more commonly males |
|
|
Where do synovial sarcomas occur?
|
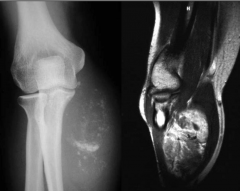
>80% in deep soft tissue of extremities, especially around the knee
|
|
What genetic abnormality is associated with synovial sarcomas?
|

t(X;18) (p11;q11)
|
|
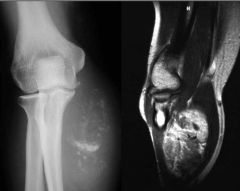
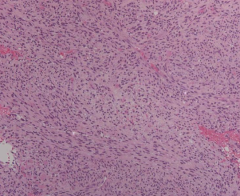
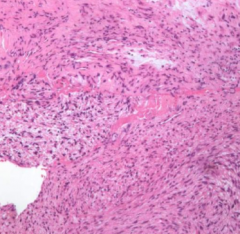
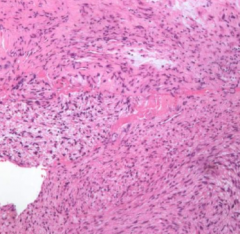
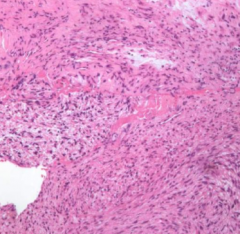
What are the histological characteristics of synovial sarcomas?
|
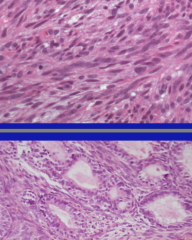
- Monophasic (spindle cell differentiation only) = toop
- Biphasic (epithelial-type cell and spindle cell differentiation) = bottom |
|
How are synovial sarcomas treated? Where can it metastasize to? Outcomes?
|
- Aggressively w/ limb-sparing surgery and chemotherapy
- Commonly metastasizes to lung, bone, and regional lymph nodes - 5-yr survival rates range from 25% to 62% and only 10-30% of patients live longer than 10 yrs |

