![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
42 Cards in this Set
- Front
- Back
|
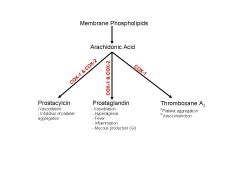
What does the flow diagram of the cyclooxygenase pathway look like?
|
|
|
|
What are the 3 main levels of pharmacological action of NSAIDs?
|
1) Analgesic effects (pain-relief)
2) Antipyretic (fever relief) 3) Anti-inflammatory (at high doses) |
|
|
Why is acetaminophen (AKA Tylenol) not considered a NSAID?
|
It has antipyretic and analgesic effects but it does not have an anti-inflammatory.
|
|
|
Which pathway in the Arachidonic Acid cascade is targeted by NSAIDs?
|
The cyclooxygenase (COX) pathway consisting of the COX-1, COX-2 and the newly discovered COX-3 enzymes
(Remember the other pathway? Lipoxygenase (LO) Pathway) |
|
|
Where does arachidonic acid come from?
|
The breakdown of phospholipids on the membrane of cells.
|
|
|
What are the three main products of the cyclooxygenase pathway?
|
1) Prostacyclins
2) Prostaglandins 3) Thromboxane A2 |
|
|
What enzyme(s) are necessary for prostacyclin a prostaglandin production?
|
COX-1 and COX 2
|
|
|
What enzyme(s) are necessary for TXA2 production?
|
COX-1 only.
|
|
|
What effect does prostaglandin production have on the body?
|
Hyperalgesia
Fever Pain Inflammation Vasodilation Mucous production |
|
|
What effect does prostacyclin production have on the body?
|
Inhibits platelet aggregation (thinning the blood)
Vasodilation |
|
|
What effects does thromboxane A2 have on the body?
|
Stimulate platelet aggregation (thrombosis)
Vasoconstriction |
|
|
What is the location, expression, role and specific function(s) of the COX-1 enzyme?
|
Constitutively expressed
Expressed in most tissues (including platelets) Plays a role in housekeeping (protection and maintenance) GI protection (prostalandins via mucous secretion) Maintains renal blood flow via vasodilation (prostaglandins acting on the AA) |
|
|
What is the location, expression, role and specific function(s) of the COX-2 enzyme?
|
Inducible via inflammatory mediators
Expressed in the KIDNEY, brain, bone and reproductive tissue (not platelets) Pro-inflammatory and mitogenic role therefore function in inflammation and carcinogenesis |
|
|
What is the MOA of NSAIDs?
|
Inhibit both the COX-1 and COX 2 enzymes of the cyclooxygenase pathway, thereby inhibiting prostacyclin, prostaglandin and TXA2 production.
|
|
|
What is the overall affect of NSAIDs?
|
Decreased pain and decreased platelet aggregation
|
|
|
What does a COX-2 inhibitor block?
|
Inhibits only prostaglandin and prostacyclin production via the cyclooxygenase pathway. TXA2 is still produced because it uses only COX-1 enzyme (therefore still have vasoconstriction and platelet aggregation occurring).
|
|
|
What are some example drugs that are NSAIDs?
|
Ibuprofen (Advil)
ASA Naproxen Diclofenac Indomethacin |
|
|
What is the protype drug for COX-2 inhibitors?
|
Celecoxib
|
|
|
How do NSAIDs have an analgesic effect?
|
By blocking COX-1&2, they block the production prostaglandins that sensitize nociceptors to inflammatory mediators (most sensitive against pain associated with inflammation or tissue damage).
Decreased prostaglandins = decreased vasodilation which may contribute to their effectiveness against headaches. |
|
|
How do NSAIDS cause an anti-inflammatory effect?
|
Decreased prostaglandin production, decreases vasodilation thereby decrease edema
|
|
|
Why is ASA not a good anti-inflammatory drug?
|
Because of its side effects (GI upset, tinnitus (ringing of the ears))
|
|
|
When is the use of ASA contraindicated?
|
1) In children with a fever– causes Reye’s syndrome (potentially fatal liver and brain disease that can arise when ASA is given when children are infected with a viral infection; causes fatty liver and encephalopathy). Give Tyelonol instead.
2) Asthmatics – may result in brochospasms/bronchoconstriction 3) GI bleed – ASA binds irreversibly to platelets |
|
|
What are the side effects of NSAIDs?
|
1) Gastrointestinal – nausea, heartburn, peptic ulcers, GI bleeds
2) Renal – prostacyclin causes vasodilation of the AA to the kidneys therefore NSAIDs decreased the ability to regulate renal flow 3) Increased chance of bleeding |
|
|
Biochemically, why do NSAIDs cause GI upset?
|
- Local damage of the organic acid of the drug damaging the epithelial cells (minimal)
- Systemic reduction of mucosal secretions (due to prostaglandin inhibition) which decreases the mucous layer and HCO3- secretion on the surface of the GI epithelium. This reduces the protective layer for the epithelium against acid. |
|
|
What are five factors that increase risk of getting ulcers when taking NSAIDs?
|
1) Previous ulcers/bleed
2) Eldery 3) Concomitant steroids 4) Cardiac disease 5) Choice of NSAID |
|
|
How would you manage someone that had GI effects from NSAIDs?
|
1) Gastroprotectants (antacids, H2-receptor antagonists, H+ pump inhibitors, prostaglandin analogs)
2) Choose agents with less GI side effects (Ibuprofen) 3) Administration of food 4) Avoid concomitant steroids 5) Consider COX-2 inhibitors |
|
|
What are some gastroprotectants you can use to help subside GI effects of NSAIDs?
|
Antacids
H2-receptor antagonists (Ranitidine) Misoprostol (prostaglandin analog) Omeprazole (H+ pump inhibitor) * Note – all of them will be effective for dyspepsia but only Misoprostol and Omeprazole will be gastroproctectant against ulcers. |
|
|
How do PPI decreased dyspepsia side effects of NSAIDs?
|
They inhibit the H+/K pump on the apical side of parietal cells thereby decreasing H+ (acid) secretion into the gastric lumen
|
|
|
What type of drug is Misoprostol?
|
Prostaglandin analog – will replace the prostaglandins being inhibited by the NSAIDs
|
|
|
What compounds regulate H+ release into the stomach?
|
1) ACh
2) Gastrin 3) Histamine |
|
|
In someone with a previous bleeding ulcer, is it better to treat with COX-2 specific inhibitors or Diclofenac + omeprazole?
|
No significant different in GI bleeds comparably.
|
|
|
Why should you never give someone with renal dysfunction, a NSAID or a COX-2 inhibitor?
|
Prostacyclins mediate vasodilation in renal medulla and glomerulus therefore, if you inhibit prostacylcins, you decrease the ability to regulate blood flow to the kidney. In someone with a failing kidney or on sodium depletion, this decrease in blood flow (and therefore GFR) can send them into renal failure.
|
|
|
Which NSAID(s) has the highest rate of toxicity?
|
Indomethacin
|
|
|
Which NSAID(s) have longer half lives and therefore less frequent dosing schedules?
|
Naproxen
Piroxicam |
|
|
What drugs interact with NSAIDs?
|
1) Lithium – due to decreased renal clearance
2) Warfarin – excessive thinning of already thin blood; bleeding risk 3) ACEi – reduces the anti-HTN effects |
|
|
Why do COX-2 inhibitors have an increased cardiovascular risks then NSAIDs?
|
Although NSAIDs affect all pathways of the cyclooxygenase pathway, the net platelet effect is decreased platelet aggregation.
With COX-2 inhibitors, TXA2 is still produces (via COX-1) whereas prostacylcins are reduced. This shifts the net effect towards the TXA2 effects which includes platelet aggregation. COX-2i therefore increases your risk of a thrombotic effect increasing your risk of MI. |
|
|
Why are NSAIDs not used as the 1st line of defense in OA therapy?
|
Because OA is considered a non-inflammatory process.
NSAIDs have more side effects then tylenol. |
|
|
What is the order of treatment for someone with OA?
|
1) Education - obesity, exercise, supports
2) Non-medical - PT and/or OT 3) Pharmacological a) Tyelonol (Acetominophen) b) NSAIDs c) Corticosteroid injection d) Viscosupplementation - glucosamine sulfate, chondroitin sulfate, Synvisc (HA injection) e) Surgery - arthroscopy or partial/total joint replacement/arthroplasty |
|
|
What are the two subtypes of corticosteroids and what physiological role do they play?
|
a) Glucocorticoids (cortisol) - control CHO, fat, protein metabolism and anti-inflammatory,
b) Mineralocorticoids (aldosterone) - control water and electrolyte level via the kidneys. |
|
|
Where in the cell do steroids exert their action?
|
Steroids bind a cytosolic receptor and translocate into the nucleus where they alter gene expression.
|
|
|
Why are steroids used for treating OA?
|
Steroids have a potent anti-inflammatory effect that if injected can be localized.
|
|
|
What is the anti-inflammatory MOA of steroids (glucocorticoids)?
|
1) Glucorticoids prevent Phospholipase A2 of cell membranes from coming into contact with its arachodonic acid substrate. This diminished eicosanoid production, decreasing leukotriene production
2) Cyclooxygenase expression is suppressed decreasing prostaglandin production Leukotriene and PG are the two main products in inflammation 3) Steroids also inhibits various inflammatory events such as, epithelial adhesion, emigration, chemotaxis, phagocytosis, respiratory burst, and the release of various inflammatory mediators. |

