![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
38 Cards in this Set
- Front
- Back
|
The pathology of osteoarthritis can be defined in 4 dimensions. What are they?
|
1. gradual loss of articular cartilage
2. thickening of subchondral bone 3. osteophytes at the joint margins 4. mild, chronic non-specific synovial inflammation |
|
|
What are the 3 stages of cartilage (in general)?
|
1. stage I - normal cartilage
2. Stage II - aging cartilage 3. Stage III - OA cartilage |
|
|
What are the 2 main components of normal cartilage?
|
1. extracellular matrix - rich in collagens (**type II, IX, XI) and proteoglycans (mainly aggrecan)
2. Chondrocytes |
|
|
What is aggrecan?
|
Central core protein with GAGs attached (chondroitin sulfate, keratan sulfate) that are capable of retaining H20.
|
|
|
How does cartilage change as it ages?
|
1. contains less H20
2. contains fewer chondrocytes which decreases capacity to synthesize matrix 3. altered collagens |
|
|
How does the matrix change in aging cartilage?
|
1. GAGs become shorter
2. Type 6 keratan sulfate increases while type 4 decreases 3. Reduction in total total proteoglycan synthesis 4. Accumulation of advanced glycation end products (AGE's) leading to inferior mechanical properties |
|
|
How are chondrocytes affected in ageing cartilage?
|
AGEs trigger RAGEs on chondrocytes (= receptors for AGE's), leading to increased catabolic activity and therefore cartilage degradation.
|
|
|
What are the 3 histologic phases of OA?
|
1. Phase I: Edema and microcracks
2. Phase II: Fissuring and Pitting 3. Phase III: Microerosion |
|
|
What constitutes Phase I of OA?
|
- 1st recognizable change = edema of ECM
- cartilage looses smooth aspect -microcracks appear -focal loss of chondrocytes alternating with areas of chondrocyte proliferation |
|
|
What constitutes Phase II of OA?
|
-microcracks deepen perpendicularly
-vertical clefts form in subchondral bone cartilage -clusters of chondrocytes appear around these clefts and at the surface |
|
|
What constitutes Phase III of OA?
|
-fissures cause fragments of cartilage to detach and "fall into" articular cavity (= loose bodies/joint mice)
-loose bodies cause mild synovial inflammation -sclerosis of subchondral bone and osteophytes form around this zone (the surfaces of osteophytes are covered with fibrocartilage) -subchondral sclerosis increases with disease progression |
|
|
What drives the pathogenesis of OA?
|
- CHONDROCYTES!!!
- fail to synthesize a good quality matrix - fail to maintain the balance between synthesis and degradation of ECM |
|
|
What is the initiating factor in the development of OA?
|
We don't know!
-mechanical loading? -microtrauma? |
|
|
What is the pathogenetic sequence of OA development?
|
1. "insult" to chondrocyte
2. Chondrocyte releases IL-1, NO and Plasminogen activating factor (PAF) 3. increased release of NMP's (stromelysin & collagenase)by chondrocyte 4. these enzymes produce cartilage damage and thus altered biomechanics 5. secondary synovitis (due to joint mice) which cause the synoviocyte to release PGE2, NO, IL-1, and NMPs 6. this creates a feedback loop to the chondrocyte and further damage occurs |
|
|
What are TIMPs?
|
Tissue Inhibitors of Metalloproteases.
These enzymes oppose the metalloproteases. |
|
|
What is the role of TIMPs in osteoarthritis?
|
In OA, the balance between ECM synthesis and degradation is skewed.
- there is increased synthesis of NMPs -there is decreased synthesis of TIMPs |
|
|
How is OA characterized clinically?
|
1. joint pain
2. stiffness 3. decreased mobility and function |
|
|
How is OA characterized radiographically?
|
1. joint space narrowing
2. subchondral bone sclerosis 3. subchondral cysts (not always present) 4. osteophytes |
|
|
What are osteophytes?
|
Fibrocartilage extensions of "new bone" along margins of joint
|
|
|
Where might you see/feel osteophytes in physical exam?
|
-over DIP joints (Heberden's nodes)
-over PIP joints (Bouchard's nodes) -1st MCP -1st MTP (bunions) |
|
|
How can you classify the etiology of OA?
|
1. Primary
2. Secondary |
|
|
What is Primary OA?
|
Describes the condition in patients when no obvious underlying cause can be discerned.
-increasingly prevalent with advancing age. (Some arthritic changes are part of the normal aging process, as evidenced by the decreased range of motion of virtually all joints, even in people who are asymptomatic.) - after the age of 75 years, >80% of persons symptomatic and limited to some degree by OA in one or more joints. |
|
|
What is secondary OA, and what are some causes?
|
Secondary OA is degenerative joint disease that is secondary to specific conditions that cause accelerated erosion of articular cartilage:
1. trauma 2. inflammatory - following any chronic jt arthropathy (RA; Ank. Spon; etc) 3. neurologic 4. metabolic/endocrine: DM, acromegaly, hemochromatosis, ochronosis 5. Subchondral Bone too stiff (Paget's disease) 6. Subchondral Bone too weak (avascular necrosis) 7. Congenital: CHD 8. Mechanical: total menisectomy, etc. |
|
|
What is the significance of increased synthesis of NMPs in OA?
|
If the collagen arcade is interruped, then the NMPs can degrade the hydrophilic PG's and ECM loses its ability to retain H20.
|
|
|
Chondrocytes are hypermetabolic in OA. True or false?
|
True! They are just fighting a losing battle.
Chondrocytes in OA undergo a lot of cell division (not normal) and so increase in numbers and activity. |
|
|
Simple way of classifying pathogenesis of OA:
|
1. abnormal force on normal cartilage
2. normal force on abnormal cartilage 3. normal force on normal cartilage with WEAKENED subchondral bone 4. normal force on normal cartilage with STIFFENED subchondral bone |
|
|
What are some common sites of OA?
|
- DIP & PIP joints of the fingers
-carpometacarpal joint of the thumb -cervical and lumbar spine -the hip -the knee -metatarsophalangeal joint of the great toe. |
|
|
What is premature primary OA?
|
Premature primary OA is seen as severe degenerative changes in one or more joints by 50 to 60 years of age, without apparent predisposing events.
|
|
|
How is the early pathologic process of OA (ie. increased degradative and hypermetabolic processes demonstrated by early proteoglycan loss and subsequent increased proteoglycan synthesis) characterized with histologic staining?
|
-changes manifest as:
-loss of basophilic staining, -appearance of chondrocyte clones, -fibrillation of the superficial cartilage. The increased synthesis of functionally impaired building blocks ultimately fails to rescue and restore the diseased matrix. The altered and weakened hyaline cartilage is susceptible to further erosion under load-bearing conditions and becomes ineffective in buffering the subchondral trabeculae against impact loading and microfracture. Eventually, full-thickness loss of hyaline cartilage occurs from the combined effect of biochemical breakdown of the matrix and abnormal biomechanical forces. |
|
|
Collagen is relatively preserved in the early stages of OA. True or False?
|
True.
|
|
|
Catabolic enzymes such as interleukin-1, neutral proteases, and metalloproteinases are increased and are a factor in progressive OA. True or False?
|
True.
|
|
|
Patients with OA present with local signs and symptoms that are specific to the affected joint. True or False?
|
True.
|
|
|
What are the clinical symptoms of OA?
|
Of note, symptoms expressed by patients with arthritic disease are generally independent of etiology and generally focus toward pain, limitation of motion, and impaired function.
|
|
|
What causes pain in OA?
|
Pain is initially provoked by load-bearing activity, is relieved by rest, and then is aggravated on resumption of activity after rest.
As symptoms progress, the pain may become constant, being present even at rest and awakening the patient at night. Examination shows variable functional limitations and loss of joint motion. |
|
|
What is GOA (generalized osteoarthritis), and which joints are affected?
|
GOA is characterized by visible osteophytes at the DIP joints of the fingers (Heberden nodes) and other arthritic joints, specifically, the PIP joints of the fingers and the carpometacarpal joint of the thumb.
Involvement of the weight-bearing joints of lower extremities is less common but causes greater functional disability. Knee arthritis is associated with GOA and hand arthritis. Hip arthritis has only a weak association with GOA. |
|
|
Where does OA cause the greatest functional limitation?
|
OA of the knee is most likely to cause functional impairment. The reported incidence of OA of the knee is 30% or greater after the age of 65 years. Associated factors in knee OA include female gender and obesity.
In contrast, OA of the hip is less common than that of the knee and exhibits neither a female predilection nor meaningful association with obesity. |
|
|
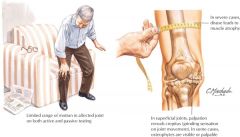
Pathology of OA.
|

|
|
|
Clinical signs of OA.
|
|

