![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
362 Cards in this Set
- Front
- Back
|
Which parts of the digestive tract are sheathed in adventitia?
|
esophagus, anus, and a small part of the large intestine
|
|
|
Blood vessels run in which layer(s) of the digestive tract?
|
lamina propria and submucosa
|
|
|
Contrast erosion vs ulceration.
|
Erosion - necrosis involving only mucosa; heals by regenerations without fibrosis/scar
Ulver - necrosis involving mucosa + deeper layers; heals with granulation tissue leading to fibrosis/scar |
|
|
The esophagus is lined by what kind of epithelium?
|
stratified squamous epithelium
|
|
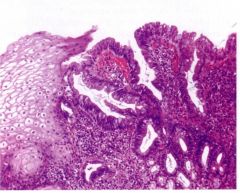
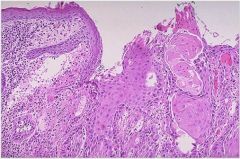
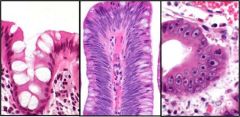
This is normal esophagus. Name the layers (lumen ->)
|
Epithelium (stratified squamous)
Lamina propria Muscularis Mucosa Submucosa Muscularis Propria (circumferential) Auerbach's plexus Musclurais Propria (longitudinal) Adventitia |
|
|
Most hiatal hernia are of what type?
|
sliding
|
|
|
Infectious esophagitis typically common in what class of patients? Name the principal etiologies. Which is most common?
|
immunosuppressed (transplant, chemo); AIDS
Candida, HSV, CMV; Candida is most common |
|
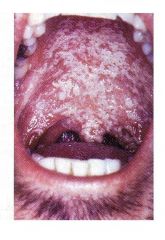
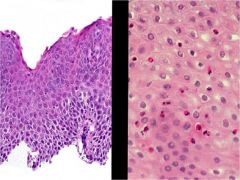
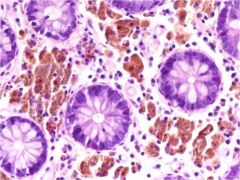
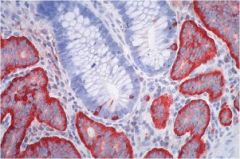
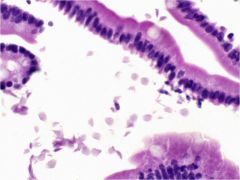
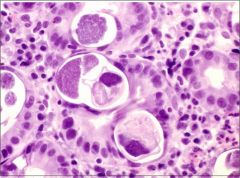
Name the organism.
Which histological stain would you use to definitively identify it? |
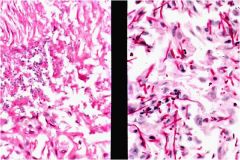
Candida
PAS stain (above: H&E on left, PAS on right) |
|
|
How is CMV acquired?
|
sexual contact
organ transplant |
|
|
What kind of lesions does Candida esophagitis produce?
|
superficial white plaques
|
|
|
What kind of lesions does CMV esophagitis produce? Which cells does the virus invade?
|
superficial ulcers
virus invades cells of the lamina propria (endothelial cells, fibroblasts) |
|
|
What kind of lesions does HSV esophagitis produce? Which cells does the virus invade?
|
superficial vesicles and ulcers
virus infects epithelial cells |
|
|
Which is worse to ingest, acid or alkaline solutions?
|
alkaline solutions are worse than acid solution
|
|
|
Contrast esophageal damage caused by ingestion of alkali vs. acid solutions.
|
alkali - causes liquefactive necrosis
acids - cause coagulative necrosis (which leads to a protective scar) |
|
|
Describe the histology of GERD.
|
Inflammation (eosinophils)
basal zone hyperplasia edema (spongiosis) |
|
|
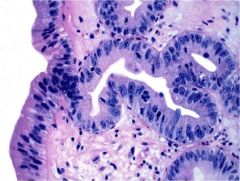
Describe the histology of Barrett Esophagus.
|
metaplasia of normal esophageal stratified squamous epithelium to intestinal columnar epithelium (with goblet cells)
|
|
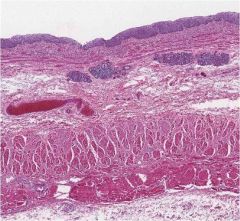
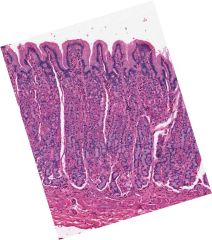
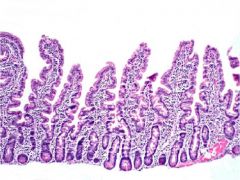
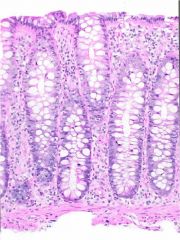
Sample from the distal 1/3 of the esophagus of a patient with 5y hx of reflux. What change is seen here?
|
Barrett Esophagus
stratified squamous -> simple columnar (intestinal) |
|
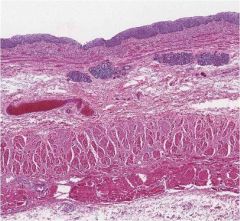
This sample is from a patient describing a 2y hx of heartburn. What is this?
|
GERD
note basal zone hyperplasia, spongiosis (edema), eosinophilia |
|
|
The top 1/3 of the esophagus is composed of ______ muscle while the lower 2/3 is composed of _________ muscle.
|
The top 1/3 of the esophagus is composed of striated muscle while the lower 2/3 is composed of smooth muscle.
|
|
|
Primary peristalsis
|
peristalsis associated with a swallow
|
|
|
How is the LES innervated?
|
vagal preganglionic (relaxation)
sympathetic post-ganglionic (constriction) |
|
|
Muscoal barrier defenses in the esophagus
|
tight junctions
bicarb production elevated blood flow transmembrane pumps salivary bicarb |
|
|
What commonly cited reason for GERD is RARELY the reason for GERD?
|
increased stomach acid production - this is rarely the reason for GERD
|
|
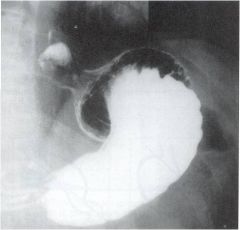
Barium swallow. What is the dx?
|
hiatal hernia
|
|
|
How does GERD normally present?
|
heartburn, dysphagia
|
|
|
Which condition is premalignant condition for adenoCA of the esophagus? Is it reversible?
|
Barrett Esophagus; this is irreversible
|
|
|
Is the risk of esophageal adenoCA high in reflux?
|
no
|
|
|
For patients with suspected GERD, which "alarm symptoms" indicate need for EGD or barium study?
|
alarm symptoms: weight loss, dysphagia, anemia, early satiety, bleeding
|
|
|
What is the best test for definitively diagnosing GERD?
|
24 hour pH proble via nasal tube
|
|
|
In the setting of reflux, a barium swallow is a good test for understanding _______ but bad at diagnosing _______.
|
In the setting of reflux, a barium swallow is a good test for understanding dysphagia but bad at diagnosing GERD.
|
|
|
In the setting of reflux, EGD is a good test for finding _______ but bad at diagnosing _______.
|
In the setting of reflux, EGD is a good test for finding complications but bad at diagnosing GERD.
|
|
|
In suspected GERD, in the absence of "alarm symptoms" what is first-line therapy?
|
non-pharmacologic approach:
-elevate head of bead -stop smoking, EtOH -reduce dietary fat -lose weight -avoid chocolate, peppermint, caffeine,citrus, tomato-based foods |
|
|
Describe the pharacological approaches to treating GERD.
|
Mild or non-erosive disease: prn treatment with baking soda, OTC antacids, H2 blockers
More severe disease: bid H2 blockers at doses up to 3x the recommended dose Erosive esophagitis and more severe disease: proton pump inhibitors |
|
|
omeprazole, lansoprazole, rabeprazole, pantoprazole, and esomeprazole belong to which class of drugs? How do they work?
|
proton pump inhibitors (PPI's)
irreversibly block the H/K ATPase |
|
|
The Nissen procedure is used to treat...
|
GERD
|
|
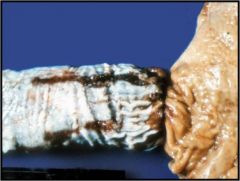
What kind of esophageal cancer is this?
|
adenocarcinoma
|
|
What kind of esophageal cancer is this?
|
squamous cell carcinoma
|
|
|
What are the 3 morphological categories of GI malignancies?
|
fungating (polypoid or exophytic)
infiltrating ulcerating |
|
|
Most esophageal carcinoma is of which type?
|
adenoCA
|
|
|
What percentage of patients with Barrett esophagus will develop adenocarcinoma? What determines the risk?
|
10%
risk of adenocarcinoma related to: -length of metaplastic segment -degree of dysplasia |
|
Describe the histological changes in Barrett Dysplasia.
|
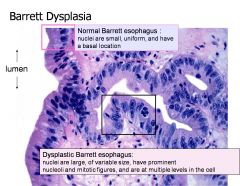
Elevated N/C ratio
Pleomorphic nuclei Hyperchromatic Prominent nucleoli Mitotic figures |
|
|
Adenocarcinoma of the esophagus is (fungating / ulcerating / infiltrating).
|
can be any of the three
|
|
|
Squamous cell carcinoma of the esophagus is (fungating / ulcerating / infiltrating).
|
can be any of the three
|
|
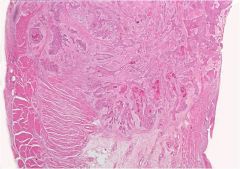
This is esophagus. What kind of cancer?
|
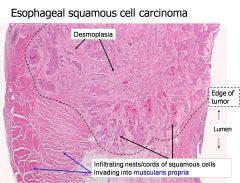
squamous cell carcinoma
|
|
|
The lymphatics of the proximal 1/3 of the esophagus drain to which nodes?
|
cervical and supraclavicular nodes
|
|
|
The lymphatics of the middle 1/3 of the esophagus drain to which nodes?
|
hilar and tracheal nodes
|
|
|
The lymphatics of the distal 1/3 of the esophagus drain to which nodes?
|
gastric and celiac nodes
|
|
|
Esophageal malignancies infiltrating and impinging on the recurrent laryngeal nerve will cause what symptoms?
|
hoarseness
|
|
|
Esophageal malignancies infiltrating te trachea will cause what symptoms?
|
cough
|
|
|
How does esophageal CA typically present?
|
dysphagia (almost always)
sometimes with weight loss (typically indicates metastatic disease) |
|
|
Describe the epidemiology of squamous cell CA.
|
more common in AA's
more common in lower SES associated with smoking associated with EtOH associated with toxin ingestion |
|
|
Describe the epidemiology of adenoCA.
|
more common in caucasians
strongly ass'd with reflux and Barrett Esophagus |
|
|
How is esophageal cancer diagnosed?
How is staged? |
diagnosed with endoscopy
staged with CT, MRI, EUS |
|
|
Esophageal cancer has what kind of survival? Why is this?
|
Dismal (1y = 18%, 5y = 5%)
This is mostly because they don't present until they have metastasized |
|
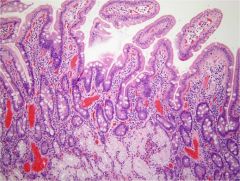
What part of the GI tract is this? What are the major features?
|
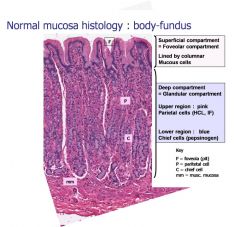
This is stomach (fundus and body).
|
|
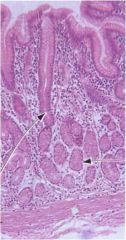
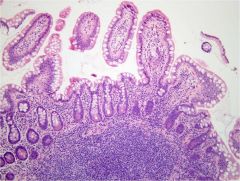
What part of the stomach is this? What are the major features?
|
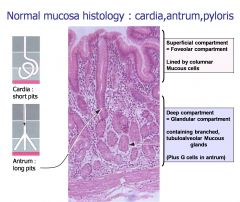
stomach (cardia, antrum, pyloris)
|
|
|
Which cells do H. pylori infect? Where do they concentrate?
|
H. pylori doesn't infect cells
H. pylori inhabits the layer of mucus adherent to gastric foveolar cells and does not adhere to intestinal cells; they concentrate at intercellular jxns where urea level is highest |
|
|
How does H. pylori adapt to the GI environment?
|
it has a urease that degrades urea into ammonia, buffering the local pH
|
|
|
H. pylori is a gram _______ rod.
|
negative
|
|
|
What is the pathogenesis of H. pylori.
|
uses proteases to degrade mucous barrier and indirectly injure epithelial cells
produces ammonia (urease) and cytotoxins which cause direct cell injury |
|
|
What are the etiologies of acute gastritis?
|
Drugs (NSAIDS, EtOH, CA chemo)
Infection (H. pylori) Trauma |
|
|
What are the "flavors" of acute gastritis?
|
Acute gastritis (inflammation)
Acute erosive gastritis (necrosis, erosion) Acute erosive hemorrhagic gastritis (erosis with hemorrhage) |
|
|
What are the etiologies of chronic gastritis?
|
Infection (H. pyrlori)
Autoimmune Other (diet) |
|
|
At the pathological level, what is the main difference between acute and chronic gastritis?
|
Acute: PMN involvement, acute onset
Chronic: lymphocyte and plasma cell involvement leading to atrophy, metaplasia, dysplasia, and cancer |
|
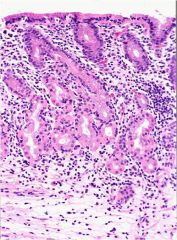
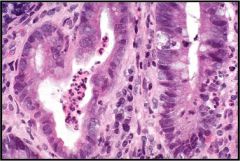
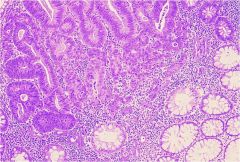
Stomach. Is this gastritis chronic or acute?
|
Chronic - note the infiltration by lymphocytes.
|
|
|
Describe the pathogenesis of autoimmune chronic gastritis.
|
Decrease in number of parietal cells leads to decreased HCL production, atrophy of gastric glands, and decreased IF production (pernicious anemia b/c B12 can't be absorbed).
|
|
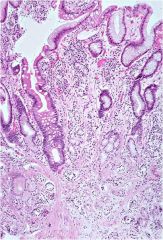
What kind of gastritis is this?
|
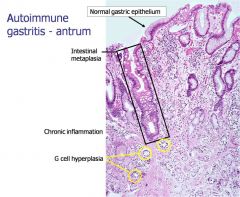
autoimmune gastritis
|
|
|
Peptic Ulcer disease primarily affects which parts of the GI tract?
|
stomach (lesser curvature and pre-pylorus) and duodenum (proximal) -regions exposed to pepsin and HCL
|
|
|
What is the etiology of Peptic Ulcer Disease?
|
H. pylori infection
NSAIDS increase in gastric acid (including ZE) |
|
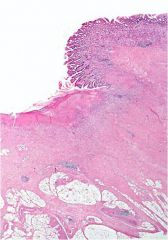
What are the four characteristic zones of a gastric peptic ulcer?
|
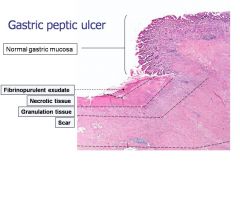
|
|
|
What are the major complications of Peptic Ulcer Disease?
|
perforation
hemorrhage obstruction from scarring |
|
|
Autoimmune gastritis is caused by antibodies to......
|
parietal cells and intrinsic factor
|
|
|
What is Menetrier's Disease?
|
hypertrophic gastropathy which causes vomiting, diarrhea, weight loss, and severe protein loss
|
|
|
How does gastritis present?
|
dyspepsia
nauseau vomiting |
|
|
What tests should be run if gastritis is suspected?
|
Consider EGD depending on "alarm symptoms"
Test for H. pylori Test levels of B12, IF, ab's to parietal cells and IF |
|
|
By definition, a gastric ulcer penetrates which layer of the gastric wall?
|
the muscularis mucosa
|
|
|
What role do prostaglandins play in gastric defense? What drugs inhibit prostaglandin synthesis?
|
prostaglandins:
stimulate mucous and bicard secretion increase mucosal blood flow inhibit acid secretion NSAIDS block COX1 and COX2, inhibiting prostaglandin synthesis |
|
|
How does peptic ulcer disease present?
|
burning epigastric pain, typically postprandial and nocturnal that is relieved with food or medication
|
|
|
How is peptic ulcer disease diagnosed?
|
endoscopy (+ biopsy)
radiography |
|
|
The Billroth procedure (both I and II) are used to treat....
|
peptic ulcer disease
|
|
|
What is Zollinger Ellison Syndrome?
|
a triad of findings:
-severe ulcer disease -gastric acid hypersecretion -non-beta islet cell tumors of the pancreas (gastrinoma) |
|
|
A gastrinoma is a tumor that secretes ________ and is associated with which disease?
|
gastrin; Zollinger-Ellison Syndrome
|
|
|
Gastric cancer is more predominant in (males / females).
|
males
|
|
|
What are the risk factors for H. pylori infection?
|
-childhood socioeconomic factors (household crowding, developing nation, water and food)
-sibling with H. pylori infection -age, race |
|
|
How is H. pylori transmitted?
|
primarily via vomit
|
|
|
How is an H. pylori infection definitively diagnosed?
|
-histology from a tissue biopsy is gold standard
-rapid testing (CLOtest, etc) -serology (IgG ELISA) -urea breath test -stool antigen test |
|
|
How do you treat an H. pylori infection?
|
PPI + 2 antibiotics
-PAC (PPI, amoxicillin, clarithromycin) -PMC (PPI, metronidazole, clarithromycin) -PBMT (PPI, bismuth, metronidazole, tetracycline) |
|
|
How does gastric carcinoma typically present?
|
Insidiously and non-specifically:
-dyspepsia -nauseau -early satiety -weight loss Advanced cancer may present with: -emesis from obstruction -GI bleeding -palpable mass -lymphadenopathy (Virchow's, SMJ nodes) |
|
|
How is gastric carcinoma diagnosed and staged?
|
Diagnosed: EGD
Staged: CT, EUS, PET, laparoscopy |
|
|
MALToma is what type of cancer?
|
gastric B-cell lymphoma
-ass'd with H. pylori infection -may have "B" symptoms |
|
|
What is a leiomyoma?
|
benign gastric smooth muscle tumor
|
|

This tumor, found on the gastric wall, forms from what kind of tissue?
|
This is a leiomyoma, a benign smooth muscle tumor (and thus of non-epithelial origin)
|
|
|
What are the two types of benign gastric polyps. How are they different?
|
Hyperplastic (non-neoplastic): occur following injury, common
Adenoma (neoplastic): benign proliferation of epithelium and stroma, uncommon |
|
|
Where is the most common site of gastric adenocarcinoma?
|
the lesser curvature of the antropyloric region
|
|
|
What is the difference between "early" and "advanced" gastric adenocarcinoma?
|
early - spread only in mucosa +/- submucosa
advance - spread into the muscularis propria +/- serosa |
|
|
What are the two types of gastric adenocarcinoma? How are they different?
|
Intestinal Type: arises from metaplastic intestinal epithelium -> dysplasia -> adenoCA; grows in expanding front
Diffuse Type: arise from poorly differentiated gastric mucous cells ("signet ring cells") - infiltrative spread causing desmoplasia (linitis plastica) |
|
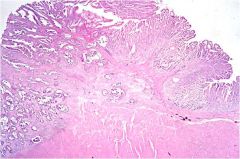
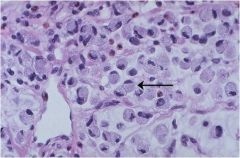
What type of gastric adenoCA is this?
|
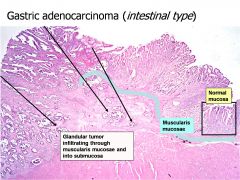
Intestinal Type
|
|
What type of gastric adenoCA is this?
|
Diffuse type gastric adenocarcinoma (note the signet ring cells)
|
|
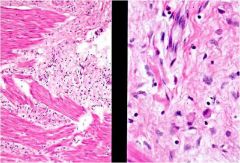
What type of gastric adenocarcinoma is this?
|
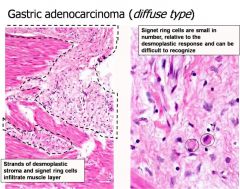
Diffuse type
|
|
|
Is the type of gastric adenocarcinoma (eg intestinal vs diffuse) have any prognostic value?
|
Not nearly as much as other factors like depth of invasion and nodal/distant mets
|
|
|
What is the pathogenesis of MALToma?
|
H. pylori infection -> chronic inflammation -> B cell influx -> low grade lymphoma
|
|
|
Does MALToma reverse with H. pylori eradication?
|
sometimes
|
|
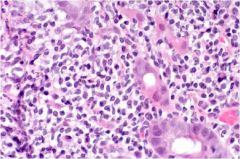
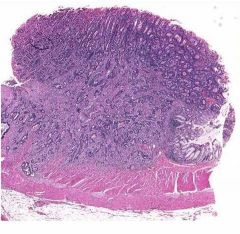
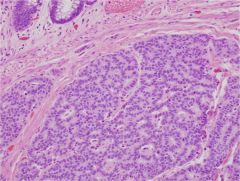
This is stomach tissue. What is the diagnosis? How do you know?
|
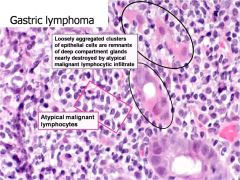
Gastric lymphoma (MALToma)
|
|
|
Achalasa is characterized by what two deficits?
|
incomplete relaxation of the LES
lack of peristalsis |
|
|
How does achalasia present?
|
increasing dysphagia to both liquids and solids with regurgitation, often with weight loss and chest pain
|
|
|
What is the etiology of achalasia?
|
Destruction of the ganglionic neurons in the esophagus
|
|
|
How is achalasia diagnosed?
|
-EGD performed to rule out mechanical obstruction
-barium swallow shows dilated esophagus with debris -manometry is diagnostic |
|

This is a barium swallow.
What's the likely diagnosis? |
achalasia
|
|
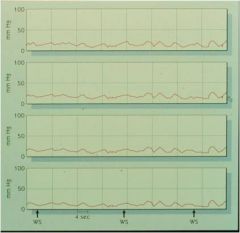
This is a manometer reading from a patient with a 6 month history of increasing dysphagia to liquids and solids and weight loss. "WS" indicates a swallow. What is the likely diagnosis?
|
achalasia
|
|
|
Describe therapy options for achalasia.
|
-Ca channel blockers and nitrates are mildly effective
-Pneumatic Dilation -Surgical Myotomy -Botox injections for pts who aren't surgical candidates |
|
|
How does Diffuse Esophageal Spasm present clinically?
|
chest pain, often with dysphagia
|
|
|
How is Diffuse Esophageal Spasm diagnosed?
|
-EGD will be normal
-Barium swallow will be normal or may show corkscrew appearance -E mano will show long, simultaneous waves |
|

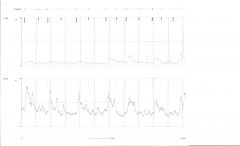
Patient presents with chest pain and mild dysphagia. What is the diagnosis?
|
Diffuse Esophageal Spasm
|
|

Patient presents with chest pain and mild dysphagia. What is the diagnosis?
|
Diffuse Esophageal Spasm
|
|
|
How is Diffuse Esophageal Spasm treated?
|
-Smooth muscle antagonists (Ca channel blockers and nitrates)
-Surgical long myotomy (intense) |
|
|
What constitutes Ineffective Esophageal Motility?
|
>30% of swallows without complete peristalsis
>30% of swallows having distal peristalsis of <30 mmHg |
|
|
What are the esophageal findings in scleroderma?
|
Decreased motility
Decreased LES pressure (hangs open) Typically presents with GERD or Esophagitis symptoms. |
|
|
How does scleroderma affect the GI tract?
|
Esophagus: decreased motility and weak LES -> GERD, esophagitis
Stomach: gastric stasis -> nausea and vomiting Small intestine: stasis, small bowel bacterial overgrowth -> bloating, nausea Colon: constipation |
|
|
Almost all stomach infections in young people that cause acute vomiting are of (bacterial / viral) origin.
|
viral (and drugs)
|
|
|
Which cause of chronic nausea and vomiting is associated with diabetes?
|
gastroparesis
|
|
|
How does bowel obstruction typically present clinically? How is the diagnosis made?
|
abdominal pain, distension, nausea, vomiting
diagnosis made by H&P + one or more of the following: plain film, CT, endoscopy, surgery |
|

25yo male present with abdominal pain, distension, and vomiting. Abdominal film above. What is the diagnosis?
|
Obstruction of small bowel
|
|
|
Which gender is more affected by constipation?
|
women
|
|
|
What is constipation?
|
-Decreased stool frequency
-Straining with defecation -Passage of hard stool -Incomplete evacuation |
|
|
Which rectal muscle distinguishes between gas / liquid / solid?
|
the internal anal sphincter muscle
|
|
|
Which rectal muscle is responsible for altering the angle of the rectum when defecating?
|
the puborectalis muscle
|
|
|
Which muscle must voluntarily relax to allow defecation? Which muscle is it attached to?
|
The external anal sphincter, which blends with the puborectalis muscle
|
|
|
Stool form correlates well with _______.
|
transit time through the bowel
|
|
|
Hard or lumpy stools indicate that a patient's intestinal transit time is too (fast / slow).
|
slow
|
|
|
A patient complains of constipation. Radiopaque markers are given to the patient and a plain film is taken 120 hours later. The radiopaque rings are found to be in the rectosigmoid colon. What is the diagnosis?
|
Functional outlet obstruction
|
|
|
4 day old infant has failed to pass meconium. Abdominal plain film above. What is the diagnosis?
|
Hirschsprung's Disease (note the distended rectum)
|
|
|
What is pelvic floor dyssynergia?
|
a paradoxical contraction of the pelvic floor with defecation that leads to outlet obstruction
|
|
|
In a patient with pelvic floor dyssynergia, manometry will show (elevated /depressed) anal pressure with (elevated / depressed ) rectal pressure on defecation.
|
In a patient with pelvic floor dyssynergia, manometry will show (elevated) anal pressure with (elevated) rectal pressure on defecation.
|
|
Top line is abdominal pressure.
Bottom line is anal pressure. What is the diagnosis? |
Pelvic floor dyssynergia.
|
|
|
Rectocele are more common in which gender?
|
Women
|
|
|
How is constipation due to slow transit treated?
|
laxatives
|
|
|
How is pelvic floor dyssynergia treated?
|
pelvic floor biofeedback: patient taught to isolate and relax puborectalis muscle with rectal sensor in place
|
|
|
How is a rectocele or enterocele treated?
|
surgically
|
|
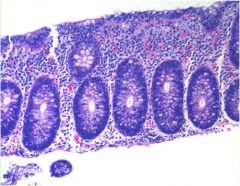
What part of the GI tract is this from?
|
small intestine
|
|
What part of the GI tract is this from?
|
colon
|
|
|
What is the prototype function bowel disease?
|
Irritable Bowel Syndrome (IBS)
|
|
|
Irritable Bowel Syndrome is predominantly a disease of which gender?
|
females
|
|
|
Patients with IBS have exaggerated motor response to __________ or ________ stimuli.
|
intrinsic (luminal); extrinsic (environmental)
|
|
|
Patients with IBS demonstrate (elevated / depressed) visceral hypersensitivity.
|
elevated
|
|
|
Patients with IBS demonstrate (larger / smaller) areas of referred pain in response to rectal distension.
|
larger
|
|
|
What is melena?
|
black, tarry stool usually associated with an upper bleeding source
|
|
|
What is hematochezia?
|
bloody stool, usually red or maroon in color, usually from a lower bleeding source
|
|
|
What is orthostasis?
|
drop in blood pressure and/or increase in pulse with a change in laying to standing position; usually indicates hypovolemia
|
|
|
Which part of the GI tract has the most sources of vascular supply and thus the least risk of ischemic disease?
|
the stomach
|
|
|
What are poor prognostic signs in an upper GI bleed?
|
-older age
-recurrent bleeding within the same hospital visit -variceal bleeding |
|
|
The vast majority of upper GI bleeds are from which cause?
|
peptic ulcers or erosions from the stomach and duodenum
|
|
|
Describe the inital steps in the management of a patient with a suspected upper GI bleed.
|
-Give patient blood while taking hx
-Get hx of liver disease, coagulopathy, NSAID use -May need NG aspirate -Assess orthostasis (hypovolemia) |
|
|
What diagnostic studies may be used in a suspected upper GI bleed?
|
NG aspirate
Upper endoscopy Arteriography (rare) NOTE: barium studies play NO role in evaluating upper GI bleeding |
|
|
How can upper GI bleeds be therapeutically managed endoscopically?
|
-inject site with epi, saline, alcohol
-use heater probe or laser -clipping of bleeding site -banding or sclerosis of varices |
|
|
Name some of the predictors of rebleeding in an upper GI bleed.
|
-older age
-shock/hemodynamic instability -comorbidities -anticoagulant use -high-risk lesions |
|
|
Describe pharmacological therapy for an acute GI bleed.
|
IV PPI (proton pump inhibitor) to stabilize clot (pepsin is inactivated at pH > 6.0)
IV octreotide if varices expected NOTE: NO role for antacids, iced saline lavage, H2 blockers |
|
|
What is the best predictor of variceal hemorrage?
|
size of varice
|
|
|
How is variceal hemorrhage treated?
|
-banding or sclerosis
-balloon tamponade -octreotide to decrease portal pressure -TIPS procedure |
|
|
What diagnostic tests are used in cases of suspected lower GI bleeding?
|
-colonoscopy (difficult with unprepped patient)
-bleeding scan -angiography |
|
|
If a bleeding scan performed on a suspected case of a lower GI bleed is positive, what is the likely next step?
|
angiography
|
|
|
Name the two most common sources of an upper GI bleed in the esophagus.
|
Varices
Mallory-Weiss tear |
|
Esophagus on L, stomach on R. What pathology is this?
|
Mallory-Weiss tear: severe retching leads to mucosal laceration and bleeding
|
|
|
Describe the various etiologies of Acute Hemorrhagic Gastritis.
|
Chemical (NSAID, EtOH, Steroids)
Ischemia Medical Stress (burns, elevated ICP, sepsis) |
|

Autopsy from patient with acute GI bleed. This specimen is from the stomach. What is the diagnosis?
|
Acute Hemorrhagic Gastritis (note the diffuse petechial mucosal hemorrhage)
|
|

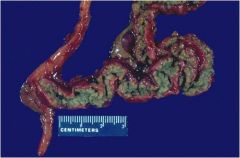
Small bowel. What is the diagnosis?
|
Ischemic bowel disease (volvulus) - note the point where the mesentery is twisted.
|
|
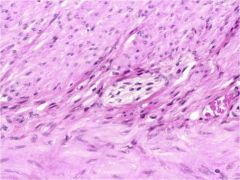
This kind of coagulative necrosis with ghost cell architecture seen in this specimen is a typical source of GI bleed. What is this?
|
ischemic bowel disease
|
|

Enlarged small bowel lymphoid tissue in children frequently causes this. What is the diagnosis?
|
intussusception of the small bowel
|
|
|
Why does intussusception of the small bowel cause ischemia, necrosis, and bleeding?
|

the mesentery is pulled into the intussusception, resulting in the ischemia and thus necrosis, infarction, and bleeding
|
|
|
A Meckel Diverticulum is the result of a persistent __________ and is a (true / false) diverticulum.
|
A Meckel Diverticulum is the result of a persistent vitelline duct and is a true diverticulum (3 layers: mucosa, submucosa, muscularis propria)
|
|
|
Why might a Meckel Diverticulum be a problem?
|
It can harbor ectopic gastric mucosa or pancreatic tissue that leads to peptic ulceration of adjacent small intestinal mucosa
|
|

The thin vascular walls of this finding are typically located in the cecum or right colon and cause a GI bleed. What is this?
|
angiodysplasia
|
|

This colonic carcinoma is on what side of the colon?
|

Left side - note the annular, ulcerated appearance with heaped up edges (this is more common on the left side)
|
|

This colonic carcinoma is found on which side of the colon?
|

Right side - carcinoma of the right colon tends to be more polyploid / fungating; note also the small bowel on the right
|
|

Where is this ulcer located?
|
duodenum
|
|
|
Which form of IBD does this describe:
-colon only -diffuse, contiguous -mucosal -not associated with smoking |
ulcerative colitis (UC)
|
|
|
Which form of IBD does this describe?
-any GI segment -focal, asymetric, skip lesions -transmural inflammation -ass'd with smoking |
Crohn's Disease
|
|
|
NOD2 allelic variants are associated with which bowel disease?
|
Crohn's disease
Some NOD2 (chr 16) variants ass'd with increased susceptibility |
|
|
Which organs besides the intestinal tract does Crohn's disease affect?
|
skin
liver eyes joints |
|
|
While Crohn's Disease can affect almost any part of the GI tract, which area does it most often affect?
|
the terminal ileum
|
|
|
How does Crohn's Disease present?
|
Abdominal pain
Diarrhea Weight Loss Growth retardation in children Fever Perianal disease |
|

This is a small bowel follow-thru of a 27yo female presenting with diarrhea, abdominal pain, and weight loss. What is the likely diagnosis?
|
Crohn's Disease
|
|
Skip lesions like the one seen above are a common presentation of which IBD?
|
Crohn's Disease
|
|

Transmural thickening of the bowel wall is associated with which IBD?
|
Crohn's Disease
|
|
|
Fistulas (bowel - bowel or bowel-bladder or bowel-skin) and perianal disease are associated with which IBD?
|
Crohn's Disease
|
|
|
IBD (both Crohn's and UC) tend to present with a _______ age distribution.
|
bimodal (~late 20's and 50's)
|
|
|
Describe the epidemiology of UC and Crohn's (geographic, age, gender, race, smoking)
|
UC: northern, 15-30yo, equal gender, white jewish, non-smokers
Crohn's: norther, 15-30yo, females more common, white jewish, smokers |
|

What frequent complication of Crohn's Disease is shown here? How does it present?
|
obstruction; presents with:
abdominal distension nausea vomiting |
|
|
What deficiencies are commonly associated with Crohn's Disease? Why is this?
|
the terminal ileum, where Crohn's is most likely to affect, is where B12 and bile salts are reabsorbed
|
|
|
How is Crohn's Disease managed?
|
First line: aminosalicylates / antibiotics
Second line: immunomodulators, corticosteroids Surgery for severe cases |
|
|
Ulcerative Colitis involves what part of the GI tract?
|
the colon only (and, more specifically, just the mucosa)
|
|
|
How does Ulcerative Colitis present?
|
Bloody diarrhea (contrast with Crohn's)
Tenesmus (inability to completely defecate) Crampy abdominal pain with BM's Weight Loss Fever Growth retardation in children |
|
|
Name some symptoms that allow differentiation between Crohn's Disease and Ulcerative Colitis.
|
In UC, diarrhea will be bloody while in Crohn's it will not
Perinanal disease is associated with Crohn's but not UC Tenesmus is associated with UC but not Crohn's |
|

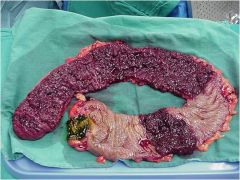
This is a frequent complication of Ulcerative Colitis. What is it? How is it treated?
|
Toxic megacolon; it is a surgical emergency
|
|
|
How will the following lab values appear in both Crohn's Disease and Ulcerative Colitis: CBC, CRP, Albumin
|
CBC will show anemia
CRP will be elevated (increased inflammation) Albumin will be depressed ("leaky gut") |
|
|
Why is a plain abdominal film needed in Ulcerative Colitis?
|
to rule out toxic megacolon, a frequent complication that is a surgical emergency
|
|
|
What is the relationship between Ulcerative Colitis and colorectal cancer?
|
After 10 years of UC, the risk of developing colorectal cancer increases by 0.5% - 1% per year. Regular dysplasia screening by colonoscopy is recommended.
|
|
|
What is the only cure for ulcerative colitis?
|
proctocolectomy (removal of the colon)
+ end ileostomy or J pouch |
|
|
50% - 70% of patients with Primary Sclerosing Cholangitis have _______.
|
IBD
|
|
|
Neutrophils located in intestinal crypts lumens are termed _______, while neutrophils located in intestinal crypt epithelium are termed _______. Both are signs of ___________.
|
Neutrophils located in intestinal crypts lumens are termed crypt abscesses, while neutrophils located in intestinal crypt epithelium are termed cryptitis. Both are signs of active colitis.
|
|
|
How does Chronic Colitis differ from Active Colitis? What is Chronic Active Colitis?
|
Chronic Colitis: altered intestinal crypt architecture and drop out; lymphocyte and plasma cells proliferate
Active Colits: PMN's in crypt lumens (crypt abscesses) and epithelium (cryptitis); crypt architecture is preserved Chronic Active Colitis is crypt abscesses, cryptitis, altered crypt architecture, and lymphocyte and plasma cell proliferation |
|
What kind of colitis is this?
|
active colitis - note the crypt abscess on L and cryptitis on R
|
|
|
What causes Colitis (active or chronic)?
|
anythig that causes disruption of colonic mucosa:
-infections -diverticulitis -ischemia -ibd |
|
|
"Creeping" mesenteric fat is associated with which form of IBD?
|
Crohn's Disease
|
|
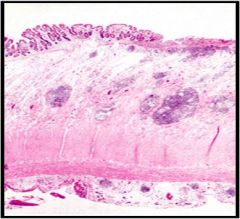
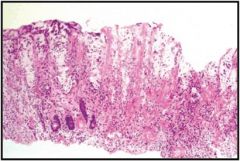
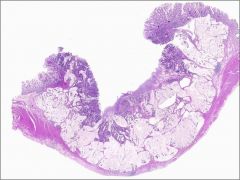
Which form of IBD is this?
|
Crohn's Disease - note the mucosal ulceration, transmural lymphoid aggregates, thickening of the wall
|
|
|
Pseudopolyps are associated with which form of IBD?
|
Ulcerative Cholitis
|
|

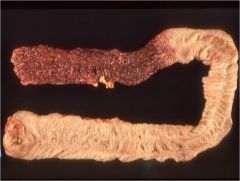
What form of IBD is this?
|
Ulcerative Cholitis - note the proximal, uninvolved colon and the distal colon with muscosal congestion, inflammation, and pseudopolyps
|
|

Pseudopolyps like these are associated with which form of IBD?
|
Ulcerative Cholitis
|
|
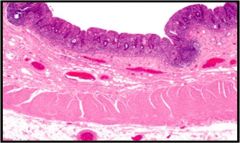
What form of IBD is this?
|
Ulcerative Cholitis - note that only the mucosa is inflamed
|
|
Which form of IBD is this?
|
Ulcerative Colitis
|
|
|
Describe the pathogenesis of appendicitis
|
Fecolith lodges in appendix
Continued secretion into lumen Elevated lumen pressure causes ischemia Ischemia causes necrosis Infection, perforation, peritonitis, sepsis |
|
|
Describe the 3 pains of appendicitis
|
Visceral pain in periumbilical region
Transmural and serosal inflammation – related pain in RLQ Diffuse abdominal / peritoneal pain if perforation occurs |
|
|
What are the symptoms of acute appendicitis?
|
Abdominal pain
Nausea / vomiting Mild fever, chills Anorexia |
|
|
What are the signs of acute appendicitis?
|
Tachycardia
Low grade fever RLQ pain (rebound) Rovsing sign Psoas sign Obdurator sign |
|
|
The Rovsing, Psoas, and Obdurator signs are all associated with which disease?
|
Acute Appendicitis
|
|
|
The majority of appendicitis is of the ________ variety.
|
Retrocecal
|
|
|
What is the key lab finding in a case of acute appendicitis?
|
Elevated WBC count (PMN’s)
|
|
|
Which radiologic study is most sensitive and specific for acute appendicitis?
|
CT (94% sens, 95% spec)
|
|
|
How is acute appendicitis managed?
|
Broad spectrum antibiotics + appendectomy
|
|
|
Which disease can often present like appendicitis?
|
Crohn’s Disease
|
|
|
What are the two main etiologies of diverticulosis?
|
age
low fiber diet |
|
|
The diverticulae of diverticulosis are (true / false) diverticuli.
|
False diverticuli – just a weakening of the wall
|
|
|
T/F: Diverticulosis occurs in the rectum
|
False
|
|
|
The majority of diverticulosis occurs in which part of the colon.
|
Left side
|
|

What is the diagnosis?
|
Diverticulosis
|
|
|
What is diverticulitis?
|
A state where diverticulae have perforated and inflammation ensues
|
|
|
Diverticulitis is by definition a ______ of a diverticulum.
|
perforation
|
|
|
How does diverticulitis present?
|
LLQ abdominal pain
Fever Constipation Leukocytosis Bowel obstruction Peritoneal signs |
|
|
A macroperforation in diverticulitis can lead to fistulas with what organs?
|
Bladder
Skin Vagina Intestine |
|
|
How is diverticulitis diagnosed?
|
CT scan
|
|

What is the diagnosis?
|
Diverticulitis?
|
|
|
Which diagnostic studies are absolutely contraindicated in diverticulitis?
|
colonoscopy
barium enema |
|
|
How is diverticulitis treated?
|
clear liquid diet
antibiotics surgery may be indicated verify etiology after resolution to rule out cancer, Crohn's, etc |
|
|
Which organisms cause bacterial enteritis by way of a pre-formed toxin?
|
Staph aureus
B. cereus |
|
|
Which organisms cause bacterial enteritis by way of direct tissue invasion?
|
Salmonella
Shigella Campylobacter E. coli |
|
|
How does bacterial enteritis present?
|
Diarrhea
Fever Dehydration Nausea Vomiting Abrupt onset |
|
|
What is the workup for bacterial enteritis?
|
CBC with differential
stool studies (+ occult blood) C. diff toxin if recently on antibiotics serum electolytes sigmoidoscopy may be indicated |
|
|
Pseudomembranous colitis is strongly associated with use of which antibiotic? What else is it associated with?
|
clindamycin
hospitalization |
|
|
Describe the 2 toxins of C. diff. What does infection with C. diff cause?
|
C. diff causes Pseudomembranous colitis and is strongly associated with clindamycin use.
Toxin A causes inappropriate colonic secretion. Toxin B is directly cytotoxic to enterocytes and is 100x more potent than Toxin A |
|

An inpatient develops a fever and diarrhea 7 days after stopping clindamycin. How would you treat this?
|
This patient likely has Pseudomembranous colitis caused by C. diff.
He needs to stop whatever antibiotics he might be on He needs to stop any anti-diarrheals he might be on Metronidazole po is first line (if it doesn't work, try metronidazole a 2nd time) Vancomycin po is second line |
|
|
In south america, achalasia often develops secondary to....
|
Chagas Disease (Trypanosoma cruzi)
|
|
This is an early sign of which disease?
|
CF - this is meconium ileus
|
|
This finding in the distal colon is suggestive of which disease?
|
Hirschsprung's Disease - due to defective neural crest cell migration leaving segment of distal colon aganglionic or with compromised ganglionic function and thus an inability to relax
|
|

What does this typically occur secondary to?
|
This is an extreme case of bowel adhesions which occur secondary to healing from peritoneal inflammation.
|
|
|
What are the three main forms of volvulus? What do they have in common?
|
Volvulus neonatorum: malrotation
Cecal volvulus: anomaly in mesenteric attachment Sigmoid volvulus: redundant sigmoid colon |
|
|
Is IBS a static or dynamic disorder? What does this mean?
|
IBS is a dynamic disorder, which means that the relative contribution of brain v gut changes over time and the symptoms change over time
|
|
|
Contrast acute versus chronic diarrhea.
|
Acute: < 2-3 weeks duration, self-limiting, most commonly infectious
Chronic: > 3 weeks duration, may be from non-infectious etiology like IBD |
|
|
Contrast the mechanisms of osmotic/malabsorption and secretory diarrhea.
|
Osmotic/Malabsorption - osmotic load in intestine results in retention of water in the lumen
Secretory - excess secretion of electrolytes and water into the intestinal lumen |
|
|
Osmotic diarrhea will decrease or resolve with __________.
|
fasting
|
|
|
Pancreatic insufficency will cause what kind of diarrhea?
|
osmotic diarrhea (fats and proteins no longer absorbed, increasing oncotic pressure in the lumen of the bowel, drawing water out)
|
|
|
Lactose intolerant individuals will have what kind of diarrhea upon ingestion of dairy products?
|
osmotic diarrhea
|
|
|
Celiac Disease, Whipple's Disease, and IBD cause what kind of diarrhea?
|
osmotic diarrhea
|
|
|
How "insufficient" does the pancreas have to become before symptom of fat and fat-soluble vitamin malabsorption becomes evident?
|
90% decrease in pancreatic function
|
|
|
The absorption of which vitamins will be affected by pancreatic insufficiency?
|
Vitamins D, A, K, and E
|
|
|
How does bacterial overgrowth of the small bowel cause diarrhea? What kind of diarrhea does it cause?
|
Bacterial overgrowth causes an osmotic diarrhea by interfering with deconjugation of bile acids, damaging mucosa, and interfering with absorption of vitamin B12.
|
|
|
What tests could you use to diagnose bacterial overgrowth of the small intestine?
|
Plain films w/ small bowel follow thru
Hydrogen breath test Culture of fluid from duodenum Empiric trial of antibiotic |
|
|
Hypokalemia is characteristic of what kind of diarrhea?
|
secretory diarrhea
|
|
|
How is a secretory diarrhea characterized?
|
substantially elevated stool volumes and hypokalemia that continues despite fasting
|
|
|
Describe the stool osmotic gap.
|
stool osmotic gap = plasma osmolality (290mosm) - [2 x (stool Na + stool K)]
if > 60, osmotic diarrhea |
|
|
Contrast secretory and osmotic diarrhea.
|
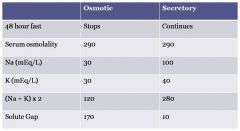
|
|
|
What features are associated with inflammatory diarrhea? Give some examples of inflammatory diarrhea.
|
WBC's / blood in stool
Fever With rectail involvement, tenesmus Examples: UC, Crohn's, E. coli, Shigella, Salmonella |
|
|
A sudan stain is applied to a stool sample to test for what?
|
fecal fat, indicating malabsorption
|
|
|
A hydrogen breath test can be used to assess what diseases?
|
lactose intolerance
small bowel bacterial overgrowth |
|
What is the diagnosis?
|
collagenous colitis
|
|
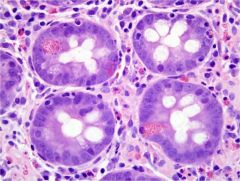
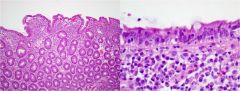
What part of the bowel?
|
duodenum (note the Brunner's Glands)
|
|
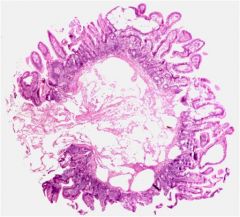
What part of the bowel?
|
ileum - note the peyer's patch
|
|
What role do the cells highlighted pink by the H&E stain play?
|
these are paneth cells, which provide host defense against microbes in the small intestine (similar function to neutrophils)
|
|
|
Name a vascular etiology of diarrhea.
|
Intestinal lymphangiectasia - dilated lymphatics in small bowel, most commonly due to retroperitoneal LN obstruction
|
|
|
Neuroendocrine tumors arising in the bowel wall can cause carcinoid syndrome, which can include a malabsorptive diarrhea. These tumors won't cause carcinoid syndrome unless....
|
they metastasize to the liver and secrete their products into the systemic circulation via the hepatic veins (if secreted in the bowel they are carried via the portal system and inactivated in the liver)
|
|
Pigementation in the bowel wall as seen here is the result of macrophages devouring dead cells. Grossly, this section of bowel would show melanin-like pigmentation. What is the diagnosis?
|
laxative abuse
|
|
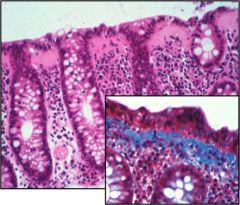
This kind of inflammatory process is common in patients with Celiax disease. What is it? If a thick collagen band was present in the mucosa, what would it be?
|
lymphocytic colitis - note that the colonic mucosal architecture is largely intact but infiltrated by lymphocytes.
If a thick collagen band was present, it would be called collagenous colitis. |
|
|
Foamy vacuolation of enterocytes and acanthocytosis of RBC's are characteristics of what congenital disorder?
|
Abetalipoproteinemia
|
|
Villous blunting, crypt hyperplasia, and intraepithelial lymphocytes in the distal duodenum and proximal jejeunum are characteristic of which disease?
|
celiac disease (sprue)
|
|
|
What is short bowel syndrome?
|
malabsorption secondary to anatomic loss of a segment of small bowel (Crohn's, Hirschsprung, Ischemia, etc)
|
|
|
The majority (90%) of bowel tumors are NOT in which segment of the bowel?
|
the small bowel
|
|
|
What is enterocyclis?
|
a diagnostic study in which as small tube is inserted through the nostril and then through the pyloric sphincter – tons of barium contrast is pumped into small bowel and images are taken
|
|
|
What is an octreotide scan?
|
give patient a synthetic hormone and a bowel tumor will preferentially take it up and this can be visualized
|
|
|
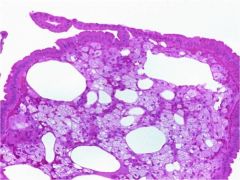
What are the three most common benign tumors of the small bowel? Which are submucosal?
|
adenoma (tubular or villous)
leiomyoma (stromal tumor, submucosal) lipoma (submucosal fat) |
|
|
A tumor projecting into the lumen of the intestine will show up on a barium study as a __________.
|
filling defect
|
|
|
What are the four most common malignant small bowel tumors?
|
adenocarcinoma
carcinoid lymphoma leiomyosarcoma |
|
|
Name this tumor:
50% of malignant small bowel tumors male predominance typically occurs at proximal small bowel associated with celiac disease, crohn's, and FAP |
small bowel adenocarcinoma
|
|
|
What is carcinoid syndrome? Which hormone causes it?
|
flushing, dyspnea, hypotension, diarrhea, telelangectasias, tachycardia
associated with serotonin secretion by carcinoid tumors |
|
|
Small bowel lymphoma associated with celiac disease is mediated by which kind of immune cells?
|
T-cells
|
|
|
What is the most common benign tumor of the distal colon and rectum? Do they have malignant potential?
|
hyperplastic polyps; they do NOT have malignant potential
|
|
|
Juvenile polyps are _________.
|
hamartomas
|
|
|
Juvenile hamartomas and mucocutaneous hyperpigmentation is associated with which syndrome?
|
Peutz-Jeghers Syndrome (autosomal dominant inheritance)
|
|
|
Colorectal cancer tends to arise from ________.
|
adenomas
|
|
|
What are some common protective measures against colorectal cancer?
|
CRC screening (colonoscopy)
Calcium Aspirin (although not routinely recommended due to risk of GI bleed) |
|
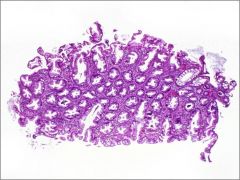
This histological section was taken from a patient's rectum. Was it pedunculated or sessile? Is it malignant or does it have malignant potential?
|
This is a hyperplastic polyp, the most common benign colon polyp. It has no malignant potential. It is sessile.
|
|
The change in colonic mucosa seen here is typical in which kind of colonic polyp?
|
Adenomatous polyp
Normal on left LG dysplasia in middle HG dysplasia on right |
|
|
What are the two kinds of adenomatous polyp? Which is more aggressive?
|
tubular; villous
villous is more aggressive |
|
This is a sample from an adenomatous polyp removed from a patient's colon. What is going on here.
|
This is high grade dysplasia that is in the very early stages in becoming invasive.
|
|
|
Where does adenocarcinoma of the colon typically metastasize to?
|
the liver (think portal system)
|
|
|
While adenocarcinoma is most common in the colon, it can occur in the small bowel. What 2 settings is it most likely to occur in the small bowel?
|
FAP
Crohn's disease |
|
|
Adenocarcinoma arises from what kind of tissue? Carcinoma?
|
Adeno - glandular tissue
Carcinoma - epithelial tissue |
|
|
How does colorectal carcinoma differ by site?
|
Right colon lesions tend to be fungating (polypoid)
Left colon lesions tend to be "apple-core" or "napkin-ring" annular lesions |
|
Where does this cancer tend to be located?
|
This is mucinous adenocarcinoma, which tend to be located in the R colon.
|
|

This disease is autosomal _______. Why was this colon removed?
|
This is FAP, an autosomal dominant disease. The colon was removed because virtually 100% of patients with FAP will develop adenoCA.
|
|
|
Carcinoid tumors in the bowel most often present at what location?
|
tip of the appendix
|
|
What kind of tumor is this? What kind of stain can be used to confirm this?
|
Carcinoid tumor - in previous image note the well rounded nodule with bland tumor in submucosa, salt and pepper chromatin pattern
To make the diagnosis we use a synaptophysin stain (pictured here) which highlights neuroendocrine cells red. |
|
|
Diagnosis of a stromal tumor depends on demonstrating expression of what oncogene?
|
c-kit
|
|
|
T/F: Secondary GI involvement by lymphomas of nodal origin is more common that primary GI lymphoma.
|
true
|
|

Diffuse infiltration of the bowel wall with no obvious gland formation is likely to be which kind of bowel cancer?
|
lymphoma
|
|
|
HPV infection (esp HPV 16) is associated with which kind of anal neoplasm?
|
squamous cell carcinoma
|
|

Where does this cancer occur? What kind of prognosis does it have?
|
This is anal melanoma which tend to invade the transitional zone above the dentate line. It has a poor prognosis.
|
|
|
The primary complication of leiomyoma is _______.
|
obstruction
|
|
|
Volvulus is a frequent complication of what kind of stromal tumor?
|
GI stromal tumor (GIST)
|
|
|
Candidiasis and Kaposi's Sarcoma can occur in an AIDS patient with a CD4 count as high as _____.
|
500
|
|
|
The CD4 count in a person with AIDS has to be below ______ in order to have symptomatic disease from MAC, CMV, and Crytosporidium.
|
100
|
|
|
Oral Hairy Leukoplakia is caused by ________ and typically manifests as _________.
|
Epstein-Barr Virus (EBV)
white lesions on lateral side of tongue that can't be scraped off |
|

AIDS patient presents with this.
What do you prescribe him? |
This is angular chelitis, a symptom of Candida infection. Therapy is Fluconazole (Amph-B is second line).
|
|

What virus causes this in an AIDS patient?
|
This is oral hairy leukoplakia, caused by the Epstein Barr Virus.
|
|
|
Dysphagia is a common symptom of which esophageal disease commonly found in AIDS patients?
|
Candida
Note: CMV, HSV, and IEU rarely cause dysphagia but will cause odynophagia |
|
|
Odynophagia is a common symptom of which esophageal disease(s) commonly found in AIDS patients?
|
CMV, IEU, HSV
Note: Candida rarely causes odynophagia but causes dysphagia |
|
|
Which esophageal disease(s) commonly found in AIDS patients cause multiple ulcers?
|
HSV
Candida doesn't cause ulcers CMV and IEU typically present with a single ulcer |
|

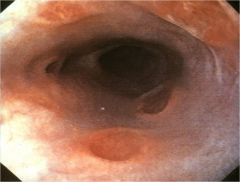
Endoscopic image of patient with AIDS and CD4 count <100. What would you prescribe for this?
|
This is CMV esophagitis. Note the deep punched out appearance. Treat with Ganciclovir or Foscarnet.
|
|

Endoscopic image of patient with AIDS and CD4 count <100. What would you prescribe for this?
|
This is HSV esophagitis. There are multiple "volcano-like" ulcers. Treatment is with acyclovir (valacyclovir, famcyclovir).
|
|
Endoscopic image of patient with AIDS and CD4 count <100. What would you prescribe for this? What would you want to do before writing this prescription?
|
There are Idiopathic esophageal ulcers. Not as deep or punched out as a CMV ulcer and note there are multiple ulcers here (CMV typically presents with a single ulcer). This is more common than HSV esophagitis. Treatment is with prednisone or thalidomide, so you better make sure it isn't CMV or HSV before you prescribe it.
|
|
|
What is the most common HIV gastric disease?
|
CMV gastritis
|
|
|
Which bacterial pathogens are common causes of diarrhea in AIDS patients with low CD4 counts?
|
Salmonella, Shigella, Campylobacter
MAC is very common when CD4 < 50 |
|
|
Which histological stain can be used to rule in / rule out MAC as a cause of diarrhea in an AIDS patient with a low CD4 count?
|
acid fast stain
|
|
|
Which protozoans are the most common causes of diarrhea in AIDS patients with low CD4 counts?
|
Microsporidia and Cryptosporidium
|
|
|
Koilocytes are a histological finding in........
|
HPV infection
|
|
|
Kaposi sarcoma is associated with which virus?
|
Human Herpes Virus 8 (HHV-8)
|
|
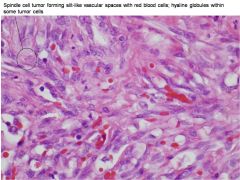
An AIDS patient with a low CD4 count undergoes a biopsy for a tumor of his bowel. The path report is above. What is this?
|
Kaposi's Sarcoma (caused by HHV-8)
|
|
What relatively rare systemic GI disease is characterized by a lamina propria expanded by foamy macrophages? What stain is used to identify it? What causes it?
|
This is Whipple Disease caused by Tropheryma whippelii, a gram positive bacilli. The macrophages stain with a acid-Schiff (PAS) stain.
|
|
|
What two systemic GI disease are characterized by macrophages expanding the lamina propria? How do you differentiate them?
|
Whipple Disease and MAC
In MAC the macrophages are NOT lipid filled (or foamy). MAC stains with an acid-fast (Ziehl-Neelsen) stain while Whipple Disease stains with a PAS stain. |
|

Patient presents with acute diarrhea. Stool sample is examined with light microscopy above. What is the diagnosis?
|
giardiasis - note the "falling leaves" appearance
|
|
Patient presents with diarrhea. Stool sample is examined under light microscopy above. How does this organism cause diarrhea?
|
This is giardiasis.
Trophozoites adhere to mucosal surface and: 1) act as a physical barrier to absorption 2) damage the microvillus brush border leading to inhibited absorption |
|
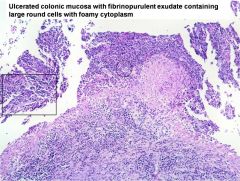
This disease is more common in the immunocompromised, is transmitted via fecal-oral route, and grossly resembles IBD (erthematous mucosa and ulceration). What is the diagnosis?
|
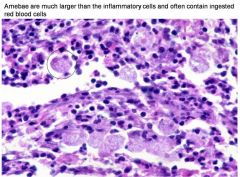
Amebiasis
|
|
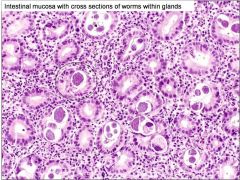
Unmanaged AIDS patient experiences vomiting, abdominal pain, and dyspnea. Stool sample is above. Lugoal iodine stain is applied. What is the diagnosis?
|
Strongyloidiasis
|
|
|
What are the exocrine cells of the pancreas? What do they do?
|
Duct cells - secretin-dependent bicarbonate secretion (neutralizes gastric acid, activates pancreatic enzymes)
Acinar cells - CCK-dependent secretion of pancreatic zymogens that are activated in duodenum by brush border enzyme enterokinase |
|
|
What are the two most common etiologies of acute pancreatitis?
|
alcohol
gallstones |
|
|
Which zymogen is implicated in the initial pathogenesis of acute pancreatitis caused by a gallstone?
|
trypsinogen - it is converted / activated to trypsin within the acinar ducts which stimulates the conversion of many other zymogens to their active forms - the result is autolysis of acinar cells
|
|
|
What genetic mutations have been associated with heriditary pancreatitis?
|
Cationic trypsinogen (PRSS1)
Pancreatic secretory trypsinogen inhibitor (PSTI; SPINK1) CFTR |
|
|
What are the two forms of acute pancreatitis?
|
Edematous pancreatitis
Necrotizing pancreatitis (sterile v infected) |
|
|
Describe the clinical presentation and course of edematous pancreatitis.
|
presents with abdominal pain, nausea, vomiting, tender abdomen
it is usually self-limiting |
|
|
How is edematous pancreatitis diagnosed? How is it treated?
|
H&P
confirmed by hyperamylasemia or hyperlipasemia LFT's may be elevated in case of bile duct obstruction imaging is largely unnecessary treat with IV fluids and pain control if gallstone induced then cholecystectomy |
|
|
What is the most common cause of acute necrotizing pancreatitis?
|
gallstones
|
|
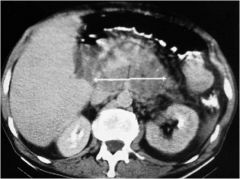
Patient presents with severe abdominal pain, nausea, vomiting, hypotension, tachycardia. CT image above. What is the diagnosis?
|
Acute necrotizing pancreatitis. Note the pancreatic phlegmon.
|
|
|
Flank (Grey-Turner's sign) and periumbilical (Cullen's sign) ecchymosis are associated with which disease?
|
acute necrotizing pancreatitis
|
|
|
What lab findings are typically associated with acute necrotizing pancreatitis?
|
Elevated amylase, lipase
Elevated Cr, BUN Leukocytosis, thrombocytosis Elevated LFT's Hypoxia Hypocalcemia |
|
|
In the case of acute necrotizing pancreatitis, is ECRP diagnostic or therapeutic? Is CT used to make the diagnosis?
|
both
CT is used to make diagnosis (contrast with edematous pancreatitis, in which imaging isn't necessary except to rule out other things) |
|
|
How is acute necrotizing pancreatitis managed?
|
pain control
IV fluids nutrition therapeutic ERC surgery |
|
|
What is the primary cause of chronic pancreatitis?
|
EtOH abuse
|
|
|
How does chronic pancreatitis present?
|
severe, unremitting epigastric pain
nausea, vomiting steatorrhea malnutrition endocrine insufficiency (diabetes) |
|
|
How is chronic pancreatitis diagnosed?
|
H&P
lab: poor nutritional status, decreased albumin, decreased transthyretin |
|
|
Calcification of the pancreas on a plain film is suggestive of what kind of pancreatitis?
|
chronic pancreatitis
|
|
|
How is chronic pancreatitis managed?
|
pain control
pancreatic enzyme replacement decrease gastric acid secretion nutrition, low fat diet endoscopic procedures: pancreatic duct stent, stone retrieval, etc surgical procedures: Puestow procedure, resection, Whipple |
|
|
What is the most common pancreatic cancer?
|
pancreatic ductal adenocarcinoma
|
|
|
What are some risk factors for developing pancreatic adenocarcinoma?
|
chronic pancreatitis
hereditary pancreatitis EtOH and tobacco use coffee dietary habits (fat) |
|
|
How does pancreatic adenocarcinoma typically present?
|
painless jaundice
pruritis weight loss malaise early satiety palpable gallbladder |
|
|
How is pancreatic adenocarcinoma treated?
|
Resection when possible (Whipple procedure)
Palliative therapy (stent) Chemo: 5-FU or gemcitabine XRT |
|
|
Does pancreatic adenocarcinoma have the potential to metastasize?
|
Yes - early potential for mets
|
|
|
Saponification is characteristic of which GI disease?
|
acute necrotizing pancreatitis
|
|
|
The majority (60%) of pancreatic adenocarcinoma is found in which part of the pancreas?
|
head of pancreas
|
|
|
The majority of islet cell tumors of the pancreas are of what type?
|
75% insulinomas
(23% are gastrinomas) |
|
|
How is a diagnosis of Irritable Bowel Syndrome defined?
|
Recurrent abdominal pain or discomfort at least 3 days / month in past 3 months associated with 2 or more of:
-improvement with defecation -change in frequency -change in appearance |
|
|
What are the most common "dominant" symptoms in making a diagnosis of Irritable Bowel Syndrome?
|
Pain
Diarrhea Constipation Bloating/Gas |
|
|
Can stress cause irritable bowel syndrome?
|
No, but it can make it the symptoms more severe.
|
|
|
What lab and diagnostic tests should be completed when the dominant symptom of a patient with Irritable Bowel Syndrome is identified?
|
CBC w/ sedimentation rate
Serum electrolytes Stool studies Endoscopy |
|
|
What general categories of medications are used to treat painful Irritable Bowel Syndrome?
|
Smooth muscle relaxants
TCA's SSRI's |
|
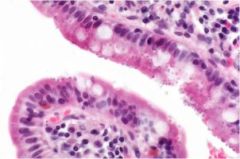
This protozoan parasite colonizes the brush border of columnar epithelia causing diarrhea in AIDS patients with depressed CD4 counts. What is it?
|
Cryptosporidium
|

