![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
242 Cards in this Set
- Front
- Back
|
What is Eithovin's Triangle?
|
A representation of the placement of the three standard ECG limb leads
|
|
|
Where are the leads placed for Lead I?
|
Leads are placed with left arm positive, right arm negative, left leg ground
|
|
|
Where are the leads placed for Lead II?
|
Leads are placed with right arm negative, left leg positive, left arm ground
|
|
|
Where are the leads placed for Lead III?
|
Leads are placed with left arm negative, left leg positive, right arm ground
|
|
|
Where are leads placed for Lead V5?
|
Positive electrode is placed between midclavicular line and lateral chest line in the 5th ICS
|
|
|
What two monitors detect cardiac dysrhythmias?
|
Stethoscope and ECG
|
|
|
Size and corresponding value of smallest squares on ECG paper
|
Smallest unit is 1mm tall by 1mm wide, corresponds to 0.04 seconds
|
|
|
Where is Lead V1 placed for a 12 lead ECG?
|
Placed over the 4th ICS on Right Sternum, over the junction of the RA and the RV
|
|
|
Advantages of a 5 lead ECG over a 3-lead ECG?
|
3-lead is limited in detecting myocardial ischemia, with 5-lead the myocardium can be monitored in all leads simultaneously for ischemia, 5 lead can better distinguish between atrial and ventricular dysrythmias
|
|
|
Which lead best detects LV myocardial ischemia?
|
V5 lead best detects
|
|
|
Which ECG lead best detects ischemia resulting from occlusion of the RCA?
|
Leads II, III, and aVF monitor this area - Inferior area
|
|
|
What ECG leads best detect myocardial ischemia in the myocardium resulting from occlusion of the left circumflex artery?
|
Leads I, aVL, V5-V6 monitor this area- the lateral myocardium
|
|
|
What ECG leads best detect ischemia resulting from occlusion of the LCA?
|
Leads I, aVL, V1-V4 monitor this area- the anterior myocardium
|
|
|
What ECG leads best detect ischemia resulting from occlusion of the LAD branch of the LCA?
|
Leads V1-V4 monitor this area, the anteroseptal myocardium
|
|
|
Characteristic EKG change with digitalis?
|
Causes downsloping of the ST segment
|
|
|
Best standard limb lead for detecting arrythmias
|
Lead II, b/c it displays large P waves
|
|
|
ECG changes with hyperkalemia
|
Prolongation of PRI, widened QRS, peaked T waves
|
|
|
ECG changes with hypokalemia
|
Prolongation of PRI, prolonged QTI, flattened T waves, appearance of U waves
|
|
|
ECG changes with hypercalcemia
|
Shortening of QTI, slight prolongation of QRS comples, widened T wives
|
|
|
Pt has prolonged PRI, widened QRS, and peaked T waves. What electrolyte abnormality would you suspect?
|
Hyperkalemia
|
|
|
Pt with Prolonged PRI, prolonged QTI, flattened T wave, and appearance of prominent U waves. What electrolyte abnormality?
|
Hypokalemia
|
|
|
ECG shows shortened QTI, slightly prolonged QRS, and widened T wave. What electrolyte abnormality?
|
Hypercalcemia
|
|
|
ECG shows prolonged QTI, increased ST segment duration, and flat T waves. What electrolyte abnormality?
|
Hypocalcemia
|
|
|
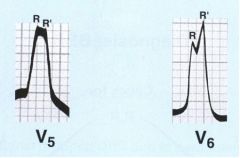
Hypertrophy of LV causes the QRS to be exaggerated in height and depth especially in what leads?
|
Large (high) R waves in V1 and V6
|
|
|
Diphasic P wave is characteristic of what?
|
atrial hypertrophy
|
|
|
Causes of ST segment depression?
|
Subendocardial ischemia or infarction; Digitalis
|
|
|
Causes of ST segment elevation?
|
Transmural ischemia or infarction
|
|
|
Indications for using a CVC?
|
1. To measure CVP
2. Rapid infusions 3. Transvenous pacemaker insertion 4. Parenteral alimentation 5. Chemo 6. Remove air |
|
|
Which vessel is preferred for CVP?
|
Right IJ b/c of straight course to SVC
|
|
|
Risks of using left IJ for CVC insertion?
|
1. Vascular erosion
2. Pleural effusions 3. Puncture of throacic duct |
|
|
Where should the tip of the CVP catheter be located?
|
Above the junction of the SVC and the RA
|
|
|
When the CVP line is inserted via RIJ, tip of the catheter on x-ray will be seen where?
|
Below inferior border of the clavicles, at the T4-T5 interspace, above level of the third rib
|
|
|
What causes the a wave on the CVP tracing?
|
results from increased pressure from Right Atrial contraction
|
|
|
What causes the c wave on the CVP tracing?
|
Results from the slight elevation of the tricuspid valve into the RA during ventricular contraction, increasing pressure in the RA
|
|
|
What causes the v wave on the CVP tracing?
|
Blood flow into the right atrium before the tricuspid valve opens, increasing pressure
|
|
|
What does the x-descent represent on the CVP tracing?
|
Occurs during ventricular systole, represents atrial relaxation with downward displacement of the tricuspid valve
|
|
|
What does the y-descent represent on the CVP tracing?
|
Occurs during diastole, represents early ventricular filling through the open tricuspid valve
|
|
|
What pathological conditions may cause an elevated CVP?
|
Pulmonary hypertension, Right heart failure, Left heart failure
|
|
|
In what situations would the CVP reading be higher than the PCWP?
|
Right Ventricular failure, possibly secondary to pulmonary HTN.
Pulmonary embolus |
|
|
Most common complication of CVC?
|
Infection
|
|
|
Acceptable sites for insertion of PAC?
|
In order of ease of insertion:
1. R IJ 2. External Jugular 3. Femoral 4. Subclavian 5. Basilar |
|
|
What site should not be used for insertion of a PAC?
|
Left IJ
|
|
|
With right IJ insertion of a PAC, what is the distance to the RIGHT ATRIUM? What is the normal pressure there?
|
Distance: 18-22cm
Pressure: 6-8mmHg |
|
|
With right IJ insertion of a PAC, what is the distance to the RIGHT VENTRICLE? What is the normal pressure there?
|
Distance: 28-32cm
Pressure: 25/0 mmHg |
|
|
With right IJ insertion of a PAC, what is the distance to the PULMONARY ARTERY? What is the normal pressure there?
|
Distance: 40-50cm
Pressure: 25/12 mmHg |
|
|
With right IJ insertion of a PAC, what is the distance to the WEDGE POSITION? What is the normal pressure there?
|
Distance: 45-50cm
Pressure: 2-12mmHg |
|
|
Indications for a PAC
|
Known CV disease
Surgery where cross-clamping of aorta is anticipated Respiratory failure Pulmonary emboli Previous cardiac surgery Pneumonectomy is anticipated Significant fluid shifts anticipated Sepsis Continuous inotropes or vasodilators Pulmonary HTN Cor pulmonale Tx with bleomycin |
|
|
What EF and CI are suggestive of poor LV fxn? What would be indicated?
|
EF <40%, CI< 2.1L/min/m2
PAC indicated |
|
|
Actions to treat PA perforation and hemorrhage
|
1. Replace volume
2. Use PEEP 3. Isolate involved lung w/ double lumen ETT |
|
|
Most common complication with insertion of PAC. How is this treated?
|
arrythmias, tx with lidocaine
|
|
|
Range of normal PA pressures
|
15-30 / 4-12 mmHg
|
|
|
Your PAC is properly wedged and a large V wave appears. What is the cause?
|
Probably mitral regurgitation
|
|
|
What interferes with CO determinations using thermodilution?
|
Electrocautery
|
|
|
Relationship between area under thermodilution and cardiac output
|
CO is inversely proportional to the area under the thermodilution curve
|
|
|
What may lead to falsely high thermodilution CO reading?
|
Insufficiency (regurgitation) of either the tricuspid valve or the pulmonic valve
|
|
|
Pt with tricuspid valve regurg has thermodilution CO reading of 5L/min. Is this accurate, falsely high, or falsely low?
|
Falsely high b/c tricuspid or pulmonic valve regurge causes false elevation
|
|
|
What is the relationship between preload, LVEDV, PAOP, LVEDP, and LADP?
|
In the absence of mitral stenosis or pulmonary HTN, PAOP = LADP = LVEDP = LVEDV = preload
|
|
|
Does PCWP overestimate, underestimate, or accurately reflect LVEDP in pt w/ mitral valve STENOSIS?
|
PCWP overestimates LVEDP in this patient
|
|
|
Does PCWP overestimate, underestimate, or accurately reflect LVEDP in pt w/ mitral valve INSUFFICIENCY?
|
Mitral insufficiency is not a factor that can lead to false estimate of LVEDP by PCWP
|
|
|
When will PCWP be greater than LVEDP?
|
1. Pts who have mitral stenosis
2. Pts with elevated alveolar pressure 3. Pts with pulmonary venous obstruction |
|
|
Diastolic dysfunction
|
decrease in left ventricular compliance
|
|
|
Systolic dysfunction
|
decreased myocardial contractility, heart failure
|
|
|
How will arterial line tracing change if air gets into the line?
|
A line pattern will be dampened in this situation
|
|
|
In intra-arterial waveform monitoring, what is the dicrotic notch due to?
|
This represents closure of the aortic valve on the intra-arterial waveform.
|
|
|
What factors may cause damping of arterial pressure transducer system?
|
May be caused by air bubbles in the a line tubing, thrombus formation in the catheter, or kinking of the catheter
|
|
|
What effect does system damping have on ABP readings?
|
Results in underestimation of SBP and overestimation of diastolic pressure
|
|
|
Arterial Cannulation sites, in order of preference
|
1. Radial
2. Ulnar 3. Brachial 4. Axillary 5. Femoral 6. Dorsalis pedis |
|
|
Possible complication with femoral artery cannulation
|
Prone to pseudoaneurysm and formation of atheroma, and potential for retroperitoneal hemorrhage
|
|
|
How do you determine the correct width of a BP cuff?
|
Width of the BP cuff should be 40% of the arm's circumference
|
|
|
Where is the ideal placement of the esophageal stethoscope?
|
Placement is within the lower third of the esophagus
|
|
|
What is the frequent cause of EtCO2 tracing not reaching baseline during inspiration?
|
Caused by rebreathing of deadspace volume
|
|
|
What conditions could cause the EtCO2 to increase in a tubed pt under GA?
|
CO2 production exceeds ventilation
Exogenous source of CO2 is present Alveolar ventilation decreases |
|
|
What causes the "rippling" or "feathering" seen on the plateau of the capnogram?
|
Caused by cardiogenic oscillations
|
|
|
What will happen to EtCO2 if the pt develops a V/Q mismatch?
|
EtCO2 may decrease because the ability to blow off CO2 decreases
|
|
|
Where on the capnograph tracing is found dead space plus alveolar ventilation?
|
Found throughout expiration on the capnograph tracing
|
|
|
Gases measured by mass spectrometry
|
Measures CO2, O2, N2, and inhaled agents
|
|
|
What happens to the gas sample drawn from a side port into the analyzer compartment of the mass spectrometer?
|
Gas sample is ionized by electron beam and passed thru magnetic field
|
|
|
Can a mass spectrometer detect a V/Q mismatch?
|
No- b/c V/Q mismatch is a/w a decrease in PaO2, which isn't measured by a mass spec
|
|
|
Examples of low perfusion states that can cause pulse oximetry artifact
|
1. Low CO
2. Anemia 3. Hypothermia 4. Increased SVR |
|
|
Factors unrelated to low perfusion that interfere w/ accurate pulse oximeter reading
|
1. Carboxyhemoglobin
2. Methemoglobin 3. Low oxygen saturations 4. Excessive ambient light 5. Movement of pt 6. Dye |
|
|
Does either fetal hemoglobin or bilirubin interfere w/ pulse oximetry?
|
No, these do not interfere with pulse oximetry
|
|
|
What two alterations in hemoglobin will yield falsely high pulse oximetry readings?
|
1. Carboxyhemoglobin- b/c it absorbs light at 660nm like oxyhemoglobin
2. Methemoglobin- has same absorption coefficient at red and infrared wavelengths |
|
|
What wavelength of light is absorbed by oxyhemoglobin?
|
Absorbs Infrared light - 990nm
|
|
|
What wavelength of light is absorbed by deoxyhemoglobin?
|
Abosrbs red light - 660nm
|
|
|
The Lambert-Beer law is based on what observation and applies to what monitoring modality?
|
Based on observation that oxygenated Hgb and reduced Hgb differ in absorption of red and infrared light - law forms the basis of pulse oximetry
|
|
|
Can the pulse oximeter detect and V/Q mismatch?
|
Yes, this monitor can detect a V/Q mismatch b/c can detect decreased PaO2
|
|
|
What monitor can detect aspiration?
|
Pulse oximeter
|
|
|
Monitors to detect disconnection
|
1. Pulse oximeter
2. Mass spec 3. Capnograph 4. Stethoscope 5. Spirometer |
|
|
Monitors to detect esophageal intubation
|
1. Pulse oximeter
2. Mass spec 3. Capnograph 4. Stethoscope |
|
|
Monitors to detect bronchial intubation?
|
1. Pulse oximeter
2. Stethoscope |
|
|
Monitors to detect pneumothorax?
|
Pulse oximeter
|
|
|
Why would you monitor with an EEG?
|
Used generally to assess adequacy of cerebral perfusion during surgery
|
|
|
When would you use sensory evoked potential monitoring?
|
To continually assess the function and integrity of neural pathways
|
|
|
How are somatosensory evoked potentials elicited?
|
Elicited by electrically stimulating nerves, exciting low threshold sensory neurons
|
|
|
What area is monitored by SSEP's?
|
Monitors the integrity of the posterior (dorsal) spinal cord where the sensory tracts are located
|
|
|
What happens to the SSEP when the pt is paralyzed w/ a muscle relaxant?
|
These will not alter the transmission of AP's in the sensory tract
|
|
|
How are evoked potentials altered by VAA?
|
These produce dose-dependent increases in latency and decreases in amplitude of EP's
|
|
|
How does nitrous oxide affect latency and amplitude of SSEP?
|
This causes decreased amplitude without change in latency of the SSEP
|
|
|
Physiologic factors that may alter sensory evoked potentials
|
1. Temperature
2. Hypotension 3. Hypoxia 4. Hypocarbia 5. Isovolemic hemodilution |
|
|
Which physiologic factor has the greatest effect on sensory evoked potentials?
|
Altered temperature affects these the most
|
|
|
Flow through what spinal arterial vessel(s) is monitored by SSEP's?
|
These monitor flow through the posterior spinal arteries
|
|
|
Brainstem auditory evoked potential monitoring is useful during operations involving what CN?
|
Useful for operations involving CN VIII
|
|
|
Monitoring of what evoked potential may be useful during pituitary surgery?
|
Visual evoked potential monitoring may be used during this type of surgery
|
|
|
Which EP is most easily depressed by VAA, and which is most resistant to depression by VAA?
|
Visual evoked potentials are most sensitive to these drugs, while brainstem auditory evoked potentials are the most resistant to these drugs
|
|
|
Where are motor evoked potentials stimulated?
|
These are stimulated over or in the motor region of the cerebral cortex
|
|
|
Why is the wake-up test performed?
|
This test is used to assess integrity of spinal-motor pathways, found in the anterior (ventral) cord
|
|
|
Wake-up test monitors what region of spinal cord?
|
This test monitors the ventral cord
|
|
|
Decreased CVP, Decreased PAP, Decreased PCWP, Decreased CI/SV/CO = ?
What would the treatment be? |
Hypovolemia
Treatment would be volume |
|
|
Elevated CVP, Elevated PAP, Elevated PCWP, Elevated CI/SV/CO = ?
What would the treatment be? |
Fluid Overload / Hypervolemia
Treatment would be diuretics, fluid restriction |
|
|
Decreased/Normal/Elevated CVP, Elevated PAP, Elevated PCWP, Decreased CI/SV/CO = ?
What would the treatment be? |
Left Ventricular failure, CHF
Treatment: Inotropes, Vasodilators |
|
|
Elevated CVP, Elevated PAP, Normal/Decreased PCWP, Decreased CI/SV/CO = ?
What would the treatment be? |
Right Ventricular failure
Treatment: Vasodilators, B-2 adrenergic stimulators |
|
|
Elevated CVP, Elevated PAP, Elevated PCWP, Decreased CO/CI/SV = ?
What would the treatment be? |
Pulmonary Edema
Treatment: Inotropes, Vasodilators, Diuretics |
|
|
Elevated CVP, Elevated PAP, Decreased PCWP, Decreased CI/SV/CO = ?
Treatment? |
Pulmonary Emboli
Treatment: support BP, aspirate air, CBP, Embolectomy |
|
|
Normal/Elevated CVP, Elevated PAP, Normal/Decreased PCWP, Normal/Decreased CI/SV/CO =?
Treatment? |
Pulmonary Hypertension
Treatment: Vasodilators, Prevent hypoxia |
|
|
Equalization of all CVP, PAP, PCWP, and CI/CO/SV = ?
Treatment? |
Cardiac Tamponade
Treatment: Volume, Pressors |
|
|
Full vasodilation produces approximately _____-fold increase in heat conductance to skin
|
Eight-fold
|
|
|
Primary means of heat loss from skin
|
radiation
|
|
|
Sweating is regulated how?
|
Regulated by the ANS, specifically via the hypothalamus to SC to sympathetic outflow tract to skin
|
|
|
Output of what hormone long term will increase heat production? How?
|
Thyroxine- increases cell metabolism throughout the body
|
|
|
Primary means of thermoregulation in the neonate
|
This age group is dependent on chemical thermogenesis (brown fat metabolism) for heat production
|
|
|
How does GA affect thermoregulation?
|
This type of anesthesia affects the CNS regulation of temp, causes vasodilation and redistribution, and slows the metabolic rate
|
|
|
How does regional anesthesia affect thermoregulation?
|
This type of anesthesia causes vasodilation below the level of the block, lowering threshold for shivering, redistributes blood, and affects peripheral perception of temp on skin
|
|
|
Deleterious Effects of Hypothermia
|
Coagulopathies
Cardiac instability Wound healing Increased Peripheral Vascular Resistance L Shift of OHC Impaired renal fxn Shivering Post-op stress response ALOC |
|
|
Phase I Hypothermia
|
1-1.5 degree reduction in core temp in first hour of surgery
|
|
|
Phase I Hypothermia is due to what?
|
Redistribution of heat from core to skin via anesthesia induced vasodilation
|
|
|
Phase 2 Hypothermia
|
Slower, linear decrease of temp
|
|
|
What causes Phase 2 Hypothermia?
|
Caused by heat loss to environment
|
|
|
Phase 3 Hypothermia
|
Plateau- heat loss and heat production is balanced, with a steady state of heat loss
|
|
|
What is the best way to decrease Phase I hypothermia? Why?
|
Pre-operative warming- eliminates gradient between core and peripheral derangements
|
|
|
In MH, agents trigger an abnormal (increase/decrease) in what kind of ions' release?
|
Agents trigger an abnormal INCREASE in the amt of CALCIUM IONS released from the sarcoplasmic reticulum in muscle cell
|
|
|
Classic S/S of MH
|
Tachycardia, Dysrhythmia, Unstable BP, Hypercapnia, Tachypnia, Skeletal muscle rigidity, high body temp, increased EtCO2
|
|
|
What is the earliest and most sensitive sign of MH?
|
Dramatic increase in EtCO2
|
|
|
What percentage of pts exhibiting masseter muscle rigidity will be MH susceptible?
|
About 50%
|
|
|
What is the diagnostic test for MH?
|
Thigh muscle biopsy - aka Halothane-Caffeine contracture test
|
|
|
Acute phase MH treatment
|
D/C causative agents
Hyperventilate w/ 100% O2 Give dantrolene sodium Give bicarb if needed Cooling |
|
|
Dantrolene Sodium dose
|
2.5mg/kg IV q5 min until s/s of hypermetabolism subside, then 1mg/kg q6h x24hr
|
|
|
The Right Coronary Artery supplies:
|
This vessel suppplies:
SA Node AV Node Posteroinferior LBB Inferoposterior LV Posterior 1/3 of septum RA and RV muscle |
|
|
What leads monitor the areas supplied by the Right Coronary Artery?
|
Leads II, III, and AVF monitor the areas supplied by this vessel.
|
|
|
The Left Coronary Artery branches into what two divisions?
|
This vessel branches into the Left Anterior Descending artery and the Circumflex artery
|
|
|
The Left Anterior Descending artery is a branch of what other artery?
|
The Left Coronary Artery
|
|
|
The Circumflex artery is a branch of what other artery?
|
The Left Coronary Artery
|
|
|
The Left Anterior Descending supplies:
|
This vessel supplies the:
Anterior 2/3 septum Right bundle branch Anterosuperior division of LBB Anterior wall of LV |
|
|
Which leads monitor the areas supplied by the Left anterior descending artery?
|
Leads I, AVL, and V1-V4 monitor the areas supplied by this vessel
|
|
|
The Circumflex artery supplies:
|
This vessel supplies the:
SA Node Posteroinferior division of LBB Lateral wall of LV |
|
|
Which leads monitor the areas supplied by the Circumflex artery?
|
Leads I, AVL, and V5-V6 monitor the areas supplied by this vessel
|
|
|
The Inferior portion of the myocardium is monitored by which leads? Which Vessel supplies this area?
|
This area is monitored by Leads II, III, and AVF
The RCA supplies this area |
|
|
The Lateral portion of the myocardium is monitored by which leads? Which Vessel supplies this area?
|
This area is monitored by Leads I, AVL, V5-V6
The Circumflex artery supplies this area |
|
|
The Anterior portion of the myocardium is monitored by which leads?
|
This area is monitored by Leads V3-V4
|
|
|
The Anterior Septal portion of the myocardium is monitored by which leads?
|
This area is monitored by leads V1-V2
|
|
|
The Anterior Lateral portion of the myocardium is monitored by which leads?
|
This area is monitored by leads V5-V6
|
|
|
Which lead is best for detecting ischemia?
|
V5 is best for detecting this.
|
|
|
The presence of a U wave on an ECG is often associated with:
|
This wave is a/w:
Hypokalemia Digitalis Papillary muscle dysfunction |
|
|
How should the ECG gain be set up when evaluating the ST segment?
|
Gain should be set at 1cm/mV when evaluating this area of the ECG
|
|
|
Potential causes for a prolongation in the QT interval
|
Prolongation in this area may be caused by:
CHF, MI, Hypocalcemia, Drugs |
|
|
Potential causes for a shortening of the QT Intervel
|
Shortening in this area may be caused by:
Digitalis, Hypercalcemia, Hyperkalemia |
|
|
Factors that can precipitate or exacerbate arrythmias
|
Ischemia, Hypoxia, Acidosis/Alkalosis, Electrolyte abnormalities, Dig toxicity, Scarred or diseased tissue
|
|
|
What is the most common cause of PVC's under GA?
|
Light anesthesia
|
|
|
Potential causes of sinus tachycardia?
|
Increased sympathetic response - light anesthesia, hypoxia
Baroreceptor reflex- hypotension, hypovolemia, HF Increased metabolic needs- hyperthermia, anemia, hypercarbia |
|
|
Etiology of a 1st Degree AV Block
|
Can be caused by:
Athletes with high vagal tone Ischemic heart disease S/P CV surgery (esp valve) |
|
|
Where is the conduction delay with a Second Degree AV Block?
|
Delay is in the low AV node or in the Bundle of His
|
|
|
Where is the block in a Third Degree Heart Block?
|
May occur at the level of AV node, Bundle of His, or Bundle Branch level
|
|
|
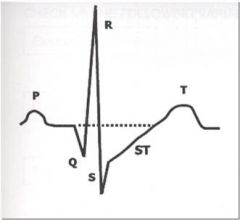
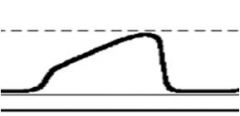
Digitalis effect
|
|
|
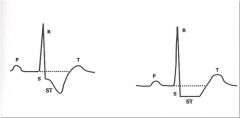
ST Depression
|
|
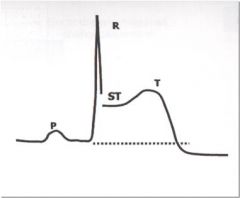
|
ST Elevation
|
|
|
An Anterior Infarction is usually a/w occlusion of what vessel?
|
Occlusion of Left Anterior Descending branch of the Left Coronary Artery
|
|
|
An Anterior Infarction is best seen in which leads?
|
This type of infarction is best seen in leads V1-V4
|
|
|
A Lateral Infarction is usually a/w occlusion of what vessel?
|
Occlusion of the Left Circumflex branch of the Left Coronary Artery
|
|
|
A Lateral Infarction is best seen in which leads?
|
This type of infarction is best seen in leads I, AVL, V5, V6
|
|
|
An Inferior infarction is usally a/w occlusion of what vessel?
|
Occlusion of the Right Coronary Artery
|
|
|
In which leads is an Inferior Infarction best seen?
|
This type of infarction is best seen in leads II, III, and AVF
|
|
|
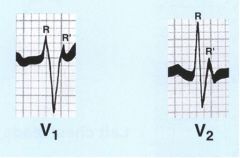
What does a posterior infarction look like on the ECG?
|
Tall, Broad R wave with ST Depression in V1 and V2
|
|
|
A Posterior Infarction is usually a/w occlusion of which vessel?
|
Occlusion of the Right Coronary Artery and/or the Left Circumflex Artery
|
|
|
In which leads is a Posterior Infarction best seen?
|
Leads V1 and V2
|
|
|
What does LVH or LAH look like on an ECG?
|
Large R waves in V1 and V6
|
|
|
How is Systolic BP affected by cuff placement?
|
SBP is increased as BP is measured more peripheral - i.e. SBP measures higher on calf than upper arm
|
|
|
How is Diastolic BP affected by cuff placement?
|
DBP is decreased as BP is measured more peripheral- i.e. DBP measures lower on calf than upper arm
|
|
|
What is the gold standard of BP monitoring techniques?
|
Intra-arterial monitoring
|
|
|
Indications for invasive arterial pressure monitoring
|
Induced hypotension
Rapid BP changes Large anticipated blood loss End-organ damage Frequent blood samples needed |
|
|
A normal Allen's test will have color return within how many seconds?
|
Less than 5 seconds
|
|
|
A dicrotic notch HIGH on the downslope of the dicrotic limb of an arterial waveform indicates what?
|
High SVR
|
|
|
A dicrotic notch LOW on the downslope of the dicrotic limb of an arterial waveform indicates what?
|
Low SVR
|
|
|
On an arterial waveform, a poorly defined or absent dicrotic notch with a slow rise in the anacrotic limb indicates what?
|
Aortic stenosis, Coarctation
|
|
|
On an arterial waveform, a poorly defined or absent dicrotic notch with a rapid rise in the anacrotic limb indicates what?
|
Aortic regurgitation
|
|
|
Factors affecting risk of complications a/w arterial lines
|
Prolonged cannulation, Hyperlipidemia, Repeated Insertion Attempts, Female gender, Use of pressors
|
|
|
Contraindications to CVP monitoring
|
Should not be done with:
Renal cell tumor extension into R Atrium Fungating tricuspid valve veg Ipsilateral Carotid End Receiving anticoagulants |
|
|
What danger is associated with cannulation of the Left Internal Jugular for placement of a CVC?
|
Danger of hitting the thoracic duct with cannulation of this vessel
|
|
|
What is indicated by elevated CVP with prominent A and V waves on the tracing?
|
Indicative of diminished Right Ventricle compliance (RHF)
|
|
|
Indications for insertion of a PA Catheter
|
Poor LV function
Assessment of intravascular fluid volume Evaluation of response to fluids or drugs Valve disease Recent MI ARDS Massive trauma |
|
|
Contraindications to placement of a PA catheter
|
Complete LBBB
WPW Syndrome Ebstein's Malformation Hypercoagulable |
|
|
Why is Zone III preferred for placement of the PA catheter?
|
This zone allows for uninterrupted blood flow and a continuous communication w/ distal intracardiac pressures
|
|
|
What does the dicrotic notch indicate on the PA trace?
|
Pulmonic Valve Closure
|
|
|
What does a large V wave on a wedge tracing indicate?
|
Mitral Valve Regurg is indicated by this wedge tracing
|
|
|
Normal Range for Cardiac Index
|
2.2 - 4.2 L/min/m2
|
|
|
Normal Range for Total Peripheral Resistance
|
1200-1500 Dynes*s cm5
|
|
|
What is the normal range for Pulmonary Vascular Resistance?
|
100-300 Dynes*s cm5
|
|
|
What is the normal range for stroke volume?
|
60-90 mL/beat
|
|
|
What is the normal range for Stroke Index?
|
20-65 mL/beat/m2
|
|
|
What is the normal range for RV stroke-work index?
|
30-35 g-m/beat/m2
|
|
|
What is the normal range for LV stroke-work index?
|
46-60 g-m/beat/m2
|
|
|
Normal pressures for RA/RAP/RVEDP/CVP
|
1-8mmHg
|
|
|
Normal pressures for RV/RVP
|
15-25 / 1-8 mmHg
|
|
|
Normal pressures for PAP
|
15-25 / 8-15 mmHg
|
|
|
Normal pressures for PW/PCWP/PAOP/LVEDP
|
6-12mmHg
|
|
|
Normal Mixed Venous Oxygen Saturation (SvO2)
|
65-75%
|
|
|
SvO2 is based on what equation?
|
Fick's- the amt of O2 consumed by an individual equals the difference between arterial and venous O2 content times CO
|
|
|
Causes of Elevation in SvO2
|
May be elevated by:
Sepsis, Pancreatitis, Continuous Wedged Balloon (most common) |
|
|
Causes of Decrease in SvO2
|
May be decreased by:
Low CO states, Low SaO2, Increased O2 consumption |
|
|
LVEDP is over or under- estimated with mitral stenosis?
|
OVERESTIMATION of LVEDP
|
|
|
LVEDP is over or under- estimated with aortic regurg?
|
UNDERESTIMATION of LVEDP
|
|
|
For every cm change in height, the SBP changes by how much?
|
Increases or decreases by 0.75mmHg
|
|
|
Bohr Effect
|
A Right Shift in the Oxy-Hb Curve: decreased affinity for O2, increased CO2 and temp
|
|
|
Haldane Effect
|
A Left Shift in the Oxy-Hb Curve: increased affinity for O2, O2 displaces CO2 from Hb
|
|
|
Isobestic Point
|
The absorption wavelength that is the same for both saturated and desaturated hemoglobin
|
|
|
What does the Beer-Lambert Law say in relation to pulse oximetry?
|
The concentration of a liquid is r/t the amt of light that will pass through it- oxygenated Hb absorbs a different wavelength of light than deoxygenated
|
|
|
SaO2 90% = PaO2 of what?
|
PaO2 of 60mmHg
|
|
|
When does cyanosis appear?
|
Appears at a SaO2 of 80% (PaO2 50mmHg)
|
|
|
Four things we have to monitor continuously
|
Oxygenation, Ventilation, Circulation, Temperature
|
|
|
Two most common methods of O2 analysis
|
Galvanic (Fuel) Cell Sensors
Paramagnetic Analysis |
|
|
Molecules may absorb infrared light if they are _____ and _______
|
Polymastic (2+ dissimilar atoms), asymmetric
|
|
|
What molecules will not be detected by infrared absorption? Why?
|
O2, N2, Helium won't be detected because they are symmetric
|
|
|
What are the main disadvantages to using mass spectrography?
|
Lag time (2-10min)
Cannot determine a V/Q mismatch May get false high readings |
|
|
Components of the Galvanic / Fuel Cell system
|
O2, anode, cathode, spontaneous electrical current, continuous consumption
|
|
|
Components of the Paramagnetic Oxygen Sensor
|
O2 magnetic field attraction, pressure difference, transducer
|
|
|
Phase 0 on the capnograph waveform represents what?
|
This phase represents inspiration, it is seen as the descending limb
|
|
|
What does the Beta Angle on the capnograph represent?
|
The angle between Phase III and the descending limb- it is at end tidal
|
|
|
What does Phase I on the capnograph represent?
|
Anatomical dead space- seen as the space just before the ascending limb
|
|
|
What does Phase II on the capnograph represent?
|
Mixture of anatomical and alveolar dead space, seen as a sharp upstroke
|
|
|
What does Phase III on the capnograph represent?
|
Alveolar plateau, the expiratory pause, designates ET concentration at the end
|
|
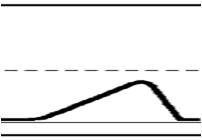
What condition would be expected to produce this type of capnograph?
|
Asthma
|
|
What condition may be expected to produce this capnograph?
|
COPD
|
|
|
What is the most common cause of diminished intraoperative renal output?
|
Hypovolemia
|
|
|
Slowed awakening with hypothermia correlates with what law?
|
Henry's Law
|
|
|
The BIS measures what?
|
The effects of anesthetics in the brain
|
|
|
Demonstrated benefits of using a BIS monitor
|
Less drug utilization
Faster wake-up and extubation More A&O in PACU |
|
|
Biggest clinical benefit of using the BIS?
|
Patient based titration of anesthetic agents, improving specificity of drug selection
|
|
|
What does the Wake-Up test evaluate?
|
Corticospinal tracts
|
|
|
Alpha EEG Waves
|
Pt is alert, relaxed, eyes open
|
|
|
Beta EEG Waves
|
Mental concentration in awake patient
|
|
|
Delta EEG Waves
|
Deep sleep or deep anesthesia
|
|
|
Theta EEG Waves
|
Seen in GA
|
|
|
Left Bundle Branch Block
|
|
|
Right Bundle Branch Block
|

