![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
71 Cards in this Set
- Front
- Back
|
Protective and offensive factors that play a role in peptic ulcer disease? |
Protective - mucus andbicarbonate secretion, prostaglandins, blood flow, and the processes of restitution and regeneration after cellular injury Offensive - acid, pepsin, bile |
|
|
Cause of peptic ulcers? |
90% due to infection with h pylori or NSAID usage |
|
|
Describe the physiologic control of acid secretion in the stomach. |
Released from parietal cells Stimulated to secrete H+ by gastrin, ACh (M3R), Histamine (H2R). H+ secreted by H+/K+ ATPase proton pump into the gastric lumen Lumenal peptides or Vagal stimulation --> Antral G cells --> Gastrin --> Blood --> Gastrin/CCK-B receptor --> direct action and via ECL (enterochromaffin like cells) ECL --> activated by gastrin and ACh --> histamine release --> activate parietal cells Vagal stimulation - direct activation of parietal cells, activation of G antral cells (gastrin release), inhibition of Antral D cells (inhibit somatostatin), Activation of ECL (histamine release) |
|
|
Which of the following are incorrect regarding gastric acid secretion: 1. Inhibition of Acid release is via Inhibition of somatostatin release from antral D cells. 2. Gastric acid secretion is due to gastrin, ACh, histamine acting directly and indirectly on parietal cells 3. Antral D cells contain somatostatin and are inhibited by Vagal stimulation but are activated by CCK 4. Gastrin binds to Gastrin-CCK-B receptors on parietal cells and enterochromaffin like cells (ECL) 5. Gastrin release from antral G cells into blood vessels is due to intraluminal dietary peptides or vagal stimulation (via GRP -gastrin releasing peptide) |
1. Inhibition of Acid release is via Inhibition of somatostatin release from antral D cells. - Incorrect Inhibition of acid release is via STIMULATION of somatostatin release by increased H+ concentration in the lumen and via CCK release from the duodenum via the blood stream |
|
|
Describe the effects of Vagal stimulation of acid secretion in the stomach |
Vagal stimulation - 1. direct activation of parietal cells 2. activation of G antral cells (gastrin release) 3. inhibition of Antral D cells (inhibit somatostatin) 4. Activation of ECL (histamine release) All increase acid secretion from parietal cells in the fundus |
|
|
How does histamine activate acid secretion? |
Release from ECL cells Histamine binds H2 receptors on parietal cells Activation of adenylyl cyclase Increases cAMP Activated protein kinases that stimulate acid secretion by H+/K+ ATPase pump |
|
|
MOA of antacids. |
Antacids are weak bases that react with gastric hydrochloric acid to for a salt and water. Either particulate (mylanta) or non-particulate (sodium bicarb) Ie sodium bicarbonate, calcium carbonate --> both cause the formation of CO2 --> belching Excess alkali with calcium containing dairy products leads to hypercalcaemia, renal insufficiency and metabolic alkalosis (Milk alkali syndrome) |
|
|
Complication of antacids? |
Excess alkali with calcium containing dairy products leads to hypercalcaemia, renal insufficiency and metabolic alkalosis (Milk alkali syndrome) CO2 formation --> belching (calcium carbonate or sodium bicarbonate only) Excess alkali in absorption in renal insufficiency - metabolic alkalosis Excess NaCl absorption - fluid retention in heart failure, HTN, renal insufficiency (sodium bicarbonate) Can inhibit absorption of other medications - avoid during this period |
|
|
Benefit of magnesium hydroxide and aluminium hydroxide over sodium bicarbonate and calcium carbonate as antacids? |
magnesium hydroxide and aluminium hydroxide --> not gas production, no absorption of alkali Mg causes diarrhoea and Al causes constipation --> usually used together to balance out the effects BUT These are PARTICULATE substances and NOT helpful in the critical care situation as aspiration of these would be +++bad |
|
|
Examples of antacids? |
Particulate: magnesium hydroxide + aluminium hydroxide (combo - mylanta) Non-particulate: Sodium bicarb - baking soda calcium carbonate - tums Sodium Citrate - Best for crit care - no gas production and not a particulate |
|
|
Describe the pharmacokinetics of H2 antagonists. |
Rapid absorption 50% bioavailability Half life - varies between drugs 1-4hrs Metabolism - combination of hepatic, glomerular filtration and renal tubular secretion Dose reduction is required in mod/severe renal insufficiency |
|
|
Name commonly used H2 antagonists |
cimetidine ranititdine famotidine |
|
|
MOA of H2 antagonists? |
Selective H2 competitive antagonism Suppress histamine mediated basal and meal stimulated acid secretion Blocks the indirect pathway of gastrin and ACh via the ECL - histamine pathway and also the direct pathway as parietal cells are less sensitive to gastrin and ACh in the presence of H2 blockers |
|
|
Indications for H2 blockers? |
GORD with antacids (immediate effect); H2 (prolonged effecT) Less effective than PPIs in erosive oesophagitis PUD - usually treated with PPI now |
|
|
Which of the following are correct/incorrect regarding Gastric Acid associated disease: 1. H2 blockers are better at inhibiting nocturnal acid secretion than meal stimulated acid secretion 2. PPIs are far superior to H2 blockers in acid inhibition 3. Standard H pylori therapy involves PPI + 2 antibiotics 4. Both H2 blockers and PPIs can be given IV in situations of stress related gastritis/ulcers 5. H2 blockers are commonly associated with SE such s diarrhoea, headache, fatigue, myalgia, constipation |
5. H2 blockers are commonly associated with SE such s diarrhoea, headache, fatigue, myalgia, constipation Incorrect - these are the right side affects but they are uncommon < 3% |
|
|
T/ F Cimetidine can have endocrine effects resulting in gynecomastia and impotence with long term use |
TRUE via inhibition of binding of hydrydotestosterone to androgen receptors and inhibition of estradiol metabolism and increasing serum prolactin levels |
|
|
Which of the following are incorrect/correct regarding PPIs: 1. PPIs are given as the active drug 2. Formulations are given as enteric coated capsules or tablets 3. Absorption occurs in the instestine 4. Capsules may be opened and mixed with food or drink 5. Causes irreversible inhibition of H+/K+ ATPase - class effect |
1. PPIs are given as the active drug - incorrect --> are PRODRUG and is converted to the active form within the parietal cell |
|
|
MOA of PPI? |
Forms a covalent disulphide bond with H+/K+ ATPase irreversibly inactivating the enzyme Inhibition of acid secretion |
|
|
Describe the basic pharmacokinetics of PPIs |
Intestinal absorption as a prodrug in enteric coated capsules/tablets Distribution - rapid distribution as they are weak bases with a low pKa -- readily diffuses across lipid membranes Bioavailability - reduced by food by 50% Clearance - hepatic 3-4 doses for full effect to block all channels (or constant infusion) T 1/2 = 1.5 hrs but prolonged effects |
|
|
Indications for PPIs |
GORD - life long - symptoms recur on cessation PUD - Heals 90% duodenal ulcers in 4 weeks and gastric ulcers in 6-8 weeks H.pylori eradication with clarithromycin and amoxil or metronidazole for 14 days UGI bleeds - ulcers Non-ulcer dyspepsia symptoms Prevention of stress related mucosal bleeding Gastrinoma (surgery if possible) or other hypersecretory conditions |
|
|
ADRs of PPIs |
SAFE Minor - diarrhoea, headache, abdominal pain Nutrition - reduced B12, iron, calcium, magnesium absorption = bone fractures with long term use Infections - increased pneumonia, c diff, other enteric infections due to ? acid being protective against organisms Raised Gastrin levels - animal models carcinoid tumours due to ECL hyperplasia |
|
|
T/F PPIs may interact with the absorption/metabolism of a number of drugs due to decreased acid suppression as the main mechanism |
False Although this is one mechanism they also affect a number of P450 enzymes which can affect drugs such as CLOPIDOGREL, warfarin, diazepam, phenytoin Absorption of ketoconazole, digoxin and atazanavir may be affected |
|
|
MOA and indication of SUCRALFATE |
It is a salt of sucrose complexed to sulphated aluminium hydroxide If binds ulcers and erosions for 6 hrs and provides protection from further damage. IT also stimulates mucosal prostaglandin and bicarb secretion Indication - Limited - can be used in critically ill patients with UGI bleeds due to concern for PPI increasing nosocomial pneumonia May cause constipation Acid dependent MOA - cannot use with antacids |
|
|
Which of the following are correct/incorrect regarding Misoprostol: 1. It is an analog of PGE1 a prostaglandin produced in the GIT 2. Short half life required TDS/QID administration 3. Provides both acid inhibitory and mucosal protective properties 4. It has other effects including intestinal electrolyte and fluid secretion, intestinal motility and uterine contractions 5. Used for NSAID induced ulcers as well as those due to H. pylori |
5. Used for NSAID induced ulcers as well as those due to H. pylori - incorrect Although it would help it is generally not used due to dosing regime and side effects |
|
|
MOA of Bismuth? |
Unknown precise mechanisms Used in combination for H pylori eradication Coats ulcers and erosions creating a protective layer against acid and pepsin Stimulate prostaglandin, mucous and bicarb secretion Antimicrobial effects, binds enterotoxins, effective against H.Pylori |
|
|
Use of bismuth in travellers diarrhoea |
bismuth subsalicylate - the salicylate inhibits prostaglandin production and has an anti secretory effect and is useful in the prevention of travellers diarrhoea Also has antimicrobial effects and binds enterotoxins |
|
|
Number of gastric acid pumps active during the fasting state? |
10% |
|
|
ADRs of bismuth? |
darkening of tongue - harmless darkening of stools - may be confused with malena bismuth compounds mayrarely lead to bismuth toxicity, resulting in encephalopathy (ataxia,headaches, confusion, seizures). bismuth subsalicylate - over dosage may lead to salicylate poisoning |
|
|
Location of the enteric nervous system? |
Submucosa - submucosal plexus - meissener Musclularis propria - between the inner circular and outer longitudinal layers of muscle - myenteric plexus - Auerbach |
|
|
Which of the following are correct/incorrect regarding the enteric nervous system: 1. 5HT activated 5HT3R on extrinsic primary afferent neurons which travel via the DRG or vagus nerve to the CNS to stimulate N/V and abdominal pain 2. Enterochromaffin cells release serotonin 3. Intrinsic primary afferent neurons (IPANs) are stimulated by 5HT1P receptors which project to myeneteric interneurons and communicate via ACh and CGRP 4. 5HT4R is located at the presynaptic site on EPANs to enhance ACh and CGRP release 5. Myenteric interneurons control peristaltic reflex, promote release of excitatory mediators proximally and inhibitory mediators distally |
4. 5HT4R is located at the presynaptic site on EPANs to enhance ACh and CGRP release - incorrect on IPANs not EPANs - ie to the interneurons |
|
|
Function of dopamine in the enteric NS? |
inhibitory NT decreasing the intensity of oesophageal and gastric contractions |
|
|
Location of 5HT4 receptors ? |
presynaptic intrinsic primary afferent neurons - acts excitatory to increase ACh and CGRP release - promoting reflex activity |
|
|
Use of neostigmine as a prokinetic? |
the acetylcholinesterase inhibitor neostigmine = increase ACh concentration = increase PSNS function + increase in motility It enhances gastric, small intestine and colonic emptying. Can be used in patients with acute large bowel distension due to acute colonic pseudo-obstruction or Ogilvies syndrome 2mg = prompt colonic evacuation |
|
|
MOA of metaclopramide? |
Dopamine - D2 receptor antagonist 1. Blocks dopamine inhibition of cholinergic SM --> thus becomes a prokinetic Increase oesophageal sphincter pressure (good for GORD), enhance oesophageal peristalsis, enhance gastric emptying (good for gastroparesis) but have no effect on the SI or colon 2. Blocks D2 receptors in the chemotrigger zone (area postrema) - potent anti-nausea and anti-emetic actions |
|
|
MOA of Domperidone ? |
Dopamine - D2 receptor antagonist 1. Blocks dopamine inhibition of cholinergic SM --> thus becomes a prokinetic Increase oesophageal sphincter pressure (good for GORD), enhance oesophageal peristalsis, enhance gastric emptying (good for gastroparesis) but have no effect on the SI or colon 2. Blocks D2 receptors in the chemotrigger zone (area postrema) - potent anti-nausea and anti-emetic actions Same as metoclopramide |
|
|
Clinical uses of Metoclopramide and domperidone? |
GORD - prokinetic but PPI usually used Gastroparesis - ie post vagotomy, diabetic Anti-emetic Domperidone - PO formulation only |
|
|
ADRs of metoclopramide? |
CNS - restlessness, drowsiness, insomnia, anxiety, agitation 10-20% Extrapyramidal - dystonia, akathisia, parkinsonian features due to central dopamine blockade in 25% of patients with high doses or 5% with long term therapy Tardive dyskinesia - prolonged metoclopramide use High prolactin levels --> galactorrhoea, gynecomastia, impotence, menstrual disorders NOTE DOMPERIDONE is well tolerated because it does not cross the BBB to a significant degree and neuropsychiatric and extrapyramidal effects are rare. |
|
|
Side effects of domperidone? |
D2 antagonist High prolactin levels --> galactorrhoea, gynecomastia, impotence, menstrual disorders NOTE DOMPERIDONE is well tolerated because it does not cross the BBB to a significant degree and neuropsychiatric and extrapyramidal effects are rare.- unlikely metoclopramide which does |
|
|
MOA of macrolides as prokinetics? |
Direct stimulation of MOTILIN receptors on GIT smooth muscle and promote onset of migrating motor complex |
|
|
What can cause Nausea & vomiting? |
Systemic infections / disorders Pregnancy Vestibular dysfunction CNS infection Raised ICP Peritonitis Hepatobiliary problems Radiation or chemotherapy GI obstruction Dysmotility Gastroenteritis Poisoning |
|
|
Location of the vomiting center? Main inputs? |
Brainstem vomiting center = Lateral medullary reticular formation coordinated vomiting through interactions with CN VIII and X and Nucleus tractus solitarius (resp, salivation, vasomotor centers) Inputs: 1. Chemotrigger zone / area postrema - responds to blood and CSF 2. Vestibular system - motion sickness 3. Vagal and spinal afferents from the GIT via the nucleus tractus solitarius - 5HT3 - distention, radiation, gastroenteritis, gag reflex 4. CNS - psych, stress etc |
|
|
Main NTs at the chemotrigger zone? |
D2 Opioid ACh - M 5HT3 NK1 H1 |
|
|
MOA of ondansetron? |
5HT-3-R antagonist Mainly effect via blockade of peripheral 5HT3 receptors on extrinsic intestinal vagal and spinal afferents Also partly - central blockade at the vomiting center and chemotrigger zone 5HT3R |
|
|
Which of the following are correct/incorrect regarding anti-emetics? 1. Ondansetron works effectively against both vagal sources of vomiting (chemotherapy, PONV etc) and motion sickness 2. Ondansetron is metabolised mainly by the liver and excreted by both the liver and kidneys 3. Ondansetron causes constipation where as metoclopramide is a prokinetic 4. Ondanestron works synergistically with dexamethasone and NK1 receptor antagonists in chemotherapy induced N&V 5. |
1. Ondansetron works effectively against both vagal sources of vomiting (chemotherapy, PONV etc) and motion sickness - incorrect - poor effect on motion sickness |
|
|
What is the preferred antacid in critical care? |
Sodium citrate IT produces no gas and is not a particulate. Acts to neutralise stomach acid so that in the event of aspiration - less damage is done |
|
|
Drugs that reduce gastric acid secretion? |
H2 antagonists PPI Misoprostol |
|
|
H2 blockers inhibit which CYP enzymes |
CYP - 12A4 2C9 2D6 3A4 Resulting in creased levels of some important drugs SIGNIFICANT with CIMETIDINE - but much less with Ranitidine |
|
|
Enzymes involved with PPI metabolism? |
CYP 2C19 CYP 3A4 Theoretical risk of inhibition of activation of the prodrug clopidogrel |
|
|
Onset of action of PPI is delayed - why? |
PPI do not block already active proton pumps but inhibit further manufacture and bind inactive pumps But prolonged effect due to covalent binding - irreversible until PP is recycled |
|
|
Misoprostol MOA |
PGE1 - prostaglandin analog Reduces acid secretion Increases Bicarb production Enhances mucosal protective effects Promotes mucosal blood flow 100% Contraindication in pregnancy |
|
|
Regurgitation is ? |
the passive movement of stomach contents into the mouth |
|
|
Factors that increase PONV? |
Female History of PONV Young children > young adults > elderly Hx Motion sickness Non smoker Full stomach Surgery - prolonged, laparotomy, laparoscopy, middle ear/ENT, strabismus Anaesthetic - General anaesthesia, volatiles, N2O, opioids |
|
|
Usual rate of PONV? |
30% in general population but up to 80% with risk factors |
|
|
Give an overview of the vomiting center and inputs |
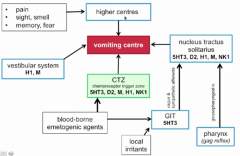
|
|
|
Side effects of ondansetron: |
Headaches Flushing Constipation QTc prolongation |
|
|
Examples of D2 Receptor antagonists? |
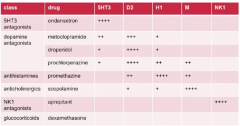
Benzamides: - Metoclopramide - Domperidone Butyrophenones - Droperidol Phenothiazenes - Prochlorperazine These drugs also work at other receptors - not selective for D2 |
|
|
Side effects of droperidol? |
Sedation Prolong QTc Extrapyramidal Exacerbate parkinsons Neuroleptic malignant syndrome |
|
|
MOA of droperidol? |
D2 antagonists Also 5HT3, H1 --> CTZ and NTS |
|
|
Prochloperazine MOA and Side effects? |
Phenothiazene - same as Chlorpromazine (largactil) MOA - D2 antagonist, also 5HT3, H1 - CTZ + NTS H1/M - vestibular system ADRs - sedation, long QTc, extrapyramidal, parkinson exacerbation, neuroleptic malignant syndrome, dry mouth, blurred vision |
|
|
Anti-histamine Anti emetics? |
H1 receptor antagonist Examples - promethazine, cyclizine (less sedating) MOA - H1 Indications: PONV, motion sickness, vertigo ADRs: sedation, anticholinergic (dry mouth, blurred vision, urinary retention, glaucoma) |
|
|
Common classes of anti-emetics? |
5HT3R antagonists - ondansetron D2 antagonists - metoclopramide, domperidone, droperidol, prochlorperazine Histamine H1 antagonists - cyclizine, promethazine Anticholinergics - uncommon Steroids - dexamethasone NK1 receptor antagonists - Aprepitant Also - propofol, midazolam, canabanoids |
|
|
Use of scopolamine? |
Skin patch for motion sickness Anticholinergic action - M1 |
|
|
MOA of dexamethasone for anti-emetic properties? |
Not known |
|
|
Aprepitant - MOA and ADRS |
MOA - NK1 receptor antagonist - at CTZ + NTS (Substance P receptor) ADRs - minor - fatigue, HA, diarrhoea, hiccups Tablet form Only approved in AUS for chemotherapy N&V |
|
|
Natural ligand for NK1 receptor? |
substance P |
|
|
Describe the main receptors involved in anti-emetic drug therapy. What are the main drugs ? |
|
|
|
Which of the following are correct/incorrect regarding ant-emetics? 1. Ondansetron routinely interacts with other drugs by inducing P450 enzymes 2. The MOA of dexamethasone as an antiemetic is unknown 3. Aprepitant is a selective NK1 receptor antagonist that crosses the BBB 4. Aprepitant is metabolised by CYP3A4 and thus may reduce metabolism of some chemotherapeutic agents such as paclitaxel, vincristine.... |
1. Ondansetron routinely interacts with other drugs by inducing P450 enzymes - incorrect Ondansetron is metabolised by P450 enzymes but does not usually affect other drug metabolism |
|
|
Examples of phenothiazines? |
prochlorperazine promethazine |
|
|
MOA of phenothiazines ? |
prochlorperazine + promethazine Antiemetic - Inhibition of dopamine and muscarinic receptors Sedation via antihistamine activity |
|
|
Example of butyrophenones and MOA? |
Droperidol Central dopamine inhibition Extremely sedating, extrapyramidal effects, long QT |
|
|
MOA of hyosine? Use? |
muscarinic antagonist ' transdermal patch for motion sickness prevention |

