![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
18 Cards in this Set
- Front
- Back
|
Primary function of CV system? |
Transportation of nutrients, waste products, hormones, electrolytes, water and heat. |
|
|
Two modes of transport use in the CV system? |
bulk flow: rapid flow over long distances, basically taking blood throughout the body
diffusion: flow over a concentration gradient |
|
|
Ischemia vs Infarction vs Necrosis ? |
Ischemia: inadequate blood flow to any tissue
Infarction: persistent ischemia leading to permanent tissue damage
Necrosis: cell death |
|
|
What is primary cardiovascular dysfunction and what are some examples? |
Primary cardiovascular dysfunction: fundamental disturbance or disease process that affects the cardiovascular system directly
Two types: 1. Congenital (present at birth) - e.g. defective heart valves 2. Acquired (acquired after birth) - e.g. hemorrhage, myocarditis, heartworm |
|
|
What is secondary cardiovascular dysfunction and what are some examples? |
Secondary cardiovascular dysfunction: cardiovascular complications develop even though the cardiovascular system is not the primary target of the disease "It started somewhere else" - e.g. electrolyte loss associated with vomiting, endotoxic shock, anesthesia overdose |
|
|
What is perfusion pressure? |
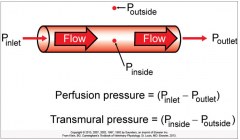
It's the pressure difference along the length of a blood vessel. Provides the energy for bulk flow. |
|
|
What is transmural pressure? |
It's the pressure difference across the wall of the blood vessel, or the distending pressure. |
|
|
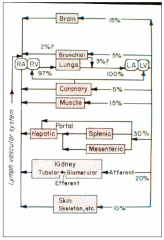
Name the three portal systems of the systemic circulatory system and why they are the exceptions. |

1. Splanchnic Circulation (digestive organs) - allows nutrients that have been absorbed in the GI tract to be directly delivered to the liver (Artery - Vein - Vein)
2. Kidneys - allows them to adjust the amounts of water and electrolytes that are in the blood (Artery - Artery - Vein)
3. Hypothalamic-hypophyseal portal system in the brain - allows for regulation of the amount of a specific hormone secreted in pituitary cells (Artery - Vein - Vein) |
|
|
What is meant by cardiac output (CO)? |
Volume of blood that is pumped each minute by one ventricle
CO of the left ventricle is the same as the CO of the right ventricle. |
|
|
Define systolic and diastolic pressure |
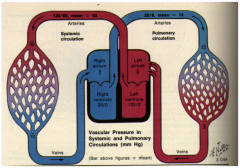
Systolic Pressure: pressure in both the systemic circulation and the pulmonary circulation during the ventricular contractions - e.g. 120/80 systemic circulation, 25/8 pulmonary circulation
Diastolic Pressure: pressure during ventricular relaxation - e.g. 120/80 systemic circulation, 25/8 pulmonary circulation |
|
|
Compare the perfusion pressures for the systemic and pulmonary circulations. How can the same volume of blood can flow through each system every minute when their perfusion pressures are so different? |
Systemic circulation: 98 - 3 = 95 mm Hg - high pressure due to high resistance
Pulmonary circulation: 13 - 5 = 8 mm Hg - low pressure due to low resistance
Explain: The systemic vessels are offering more friction to the blood flow which causes the higher pressure in the systemic system then in the pulmonary system. Not necessarily due to the further distance that it has to travel. |
|
|
How is blood distributed (percentage wise) between central and systemic circulation? |
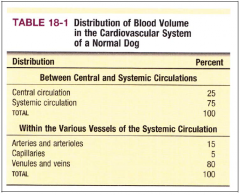
Central Circulation = 25%
Systemic Circulation = 75% - most of which is sitting in the veins |
|
|
Can you describe the path of a red blood cell (RBC) from the time it leaves the heart until it returns about one minute later? |
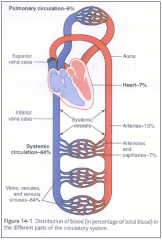
1. Aorta = leave heart 2. Arteries = high-pressure conduits 3. Arterioles = gates 4. Capillaries = exchange vessels 5. Venules = return from capillary 6. Veins = blood reservoirs 7. Vena Cavas = reenter heart |
|
|
Which vessels have the largest cross-sectional area, the slowest velocity of blood flow and largest surface area? Why? |
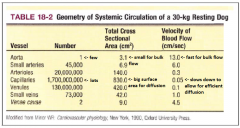
Capillaries and all because the blood needs time for diffusion to occur.
Needs the larger surface area to allow for higher capillary uptake, and needs the slower velocity so there are better odds that the blood will be fully processed. |
|
|
Be familiar with a hematocrit tube and the layers that are formed within it after centrifugation. |
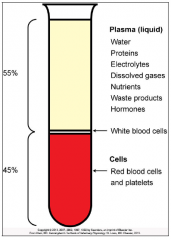
The fraction of cells in blood is called the hematocrit or packed cell volume (PCV).
Typical reference range in canines of 35 - 57% |
|
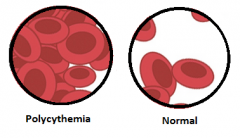
How does polycythemia effect viscosity and what is the effect on the heart? |
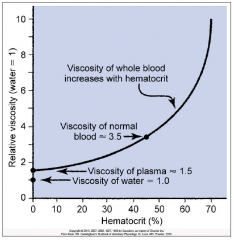
Polycythemia: an abnormally high hematocrit (RBC count)
It increases the viscosity of the blood which can cause high blood pressure due to the increase need to pump thicker blood through the circulatory system. |
|
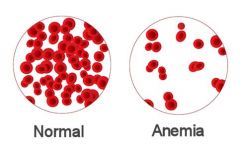
How does anemia effect viscosity and cardiac output? |
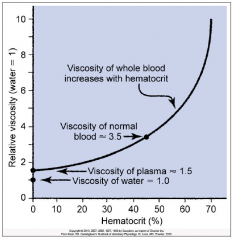
Anemia: an abnormally low hematocrit (RBC count)
Cardiac output is increased because the heart needs to compensate for the lowered oxygen concentration (due to the decrease in RBC count). |
|
|
Understand relative size and shape of the major constituents of blood. |
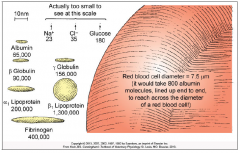
1. The plasma protein molecules are huge compared to the rest (especially to the electrolytes)
2. Blood cells (red and white) are huge compared to plasma proteins.
Electrolytes < Plasma Proteins < Blood Cells |

