![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
117 Cards in this Set
- Front
- Back
|
Lymphocytes include:
|
Include T and B-lymphocytes
Also NK cells |
|
|
Lymphocytes in Chronic inflammation:
|
Arrive approximately 5 days post injury
Prominent in chronic inflammation Essential 4 normal tissue repair Enhance macrophage function |
|
|
Lymphocytes can be associated with:
|
repetitive microtrauma, autoimmune responses, chronic conditions
**Does not have the cardinal signs of inflammation |
|
|
Histamine:
|
vasodilation, exudate formation, itching, capillary premablity
|
|
|
Kinin (Bradykinin Etc.)
|
vasodilate, form pain, exudate formation
|
|
|
Prostaglandin:
|
sensitize blood vessels to inflammatory mediators and nocirecptors
|
|
|
Complement:
|
Kills cell lyosis, non-specific, and specific , enhances defense
|
|
|
The Four Components of Repair Phase are:
|
1. Granulation
2. Fibroplasia 3. Angiogenesis 4. Re-epithelialization |
|

Granulation present indicates:
|
"normal" healing
**Named for its cobbled appearance** |
|
|
Fibroplasia are:
|
Fibroblasts drawn to wound from dermis by cytokines
Fibroblasts then change into myofibroblasts As new blood vessels are produced myofibroblast production slows |
|
|
Angiogenesis occurs by:
|
1. Sprouting of new pathway
2. Anastomosis with new and existing vascular paths A response to: Hypoxic environment Free edge effect Cytokines: platelets etc. |
|
|
Re-epithlization is important for:
|
providing barriers to infection and to decrease fluid loss
**Concurrent with the formation of granulation tissue |
|
|
Fibroplasia have:
|
Collagen (Type III) present in wound as soon as 2 days!!
|
|
|
Ground substance is:
|
Gelled material that forms the extracellular matrix &
Facilitates fibroblast production & absorbs large amounts of water **ADDS FLEXIBILITY** |
|
|
Angiogenesis is a response to:
|
1. Hypoxic environment
2. Free edge effect (wound is present) 3. Cytokines: platelets etc. |
|
|
Cellular Production is:
|
Contact inhibition is mediated by cytokines known as chalones
**NEED TO HAVE FREE EDGE EFFECT TO KNOW IT NEEDS TO OCCUR** |
|
|
Migration is the:
|
Process of cell movement from periphery to center &
occurs over granulation tissue |
|
|
3 stages of remodeling phase is:
|
1. Collagen conversion
2. Wound contraction 3. Scar formation |
|
|
Remodeling Phase is the:
|
Balance between tissue synthesis & degradation
**want both to occur |
|
|
Key Point to Collagen Conversion is that:
|
Oxygen is necessary for collagen cross-linking to occur
|
|
|
Wound Contraction is:
|
Process that closes wound after tissue loss
*Myofibroblasts connect with fibronectin which then connect with collagen fibers Actin in the cytoplasm draws the collagen closer together |
|
|
Wound Contraction results in:
|
faster healing since it decreases the amount of tissue that must be repaired & remodeled
Contraction decreases the size of full-thickness wounds by 40% & is associated with concurrent scarring |
|
|
Scar Formation has four stages, what are they?
|
Stage 1-4
|
|
|
Stage 1 of scar formation is:
|
2-4 days post injury
Type III collagen Prone to tear |
|
|
Stage 2 of scar formation is:
|
5-21 days post injury
Type III converted to type I collagen Less likely to tear Most receptive to intervention |
|
|
Stage 3 of scar formation is:
|
21-60 days post injury
More fibrous and strong Decreased response to intervention |
|
|
Stage 4 of scar formation is:
|
60 days on post injury
Scar maturation Final appearance Unresponsive to treatment, surgical intervention considered |
|

What kind of scar is this?
|
Hypertrophic scar
|
|

What kind of scar is this?
|
Keloid Scar
|
|
|
Keloid scars are:
|
Typically extend outside of wound bed
Seen typically in Asian and African populations |
|
|
Hypertrophic scars:
|
Do not extend outside of wound bed
|
|
|
Type III is gradually lysed by collagenase and converted to Type I in what length of time:
|
300 days
**The stimulus for this conversion is stress and strain Ex. Tension, compression |
|
|
In collagen conversion, Type III converted to:
|
Type I
|
|
|
Type III is synthesized during the first:
|
48-72 hours
|
|
|
Collagen Conversion tissue breaks strength to pre wound values by:
|
20% by third week prior to being damaged
70-80% in several months down the road |
|
|
Pain is defined as:
|
Unpleasant sensation
Unpleasant emotional response Actual or potential tissue damage Warning signal so appropriate response evoked |
|
|
What is pain perception?
|
Establish cognitive value & response priority
Based off of experience & involves sensory, emotional, motor, and cultural components |
|
|
Pain usually helps with:
|
tissue healing by preventing us from further aggravating our pathological and painful conditions.
|
|
|
What are the two sources of pain?
|
1. Peripheral Nociceptive
2. Peripheral Neurogenic |
|
|
Peripheral Nociceptive pain is:
|
Pain transmitted via A delta and C fibers to dorsal horn & to brain
**Its a sharp, acute pain that is localized to that injured tissue |
|
|
Peripheral Neurogenic Pain is:
|
Creates abnormal impulse generator sites (AIGS)
Nerve can be stripped of myelin **Its an Injury to the nervous system |
|
|
Central Pain source creates:
|
abnormal pain states
|
|
|
Allodynia is:
|
pain provoked by stimulus that doesn’t normally cause pain
Ex. Someone brushing up against you |
|
|
Hyperalgesia is:
|
heightened response to a painful stimulus, should hurt but "reaction" is GREATER than you would expect
|
|
|
Chronic Pain is:
|
1. Pain that last longer than 6 months
2. People sleep less (can’t sleep) & truly depressed 3. It never truly goes away, too much damage was done 4. Pain can “go away” but comes back **Physical therapy can helpmanage pain & symptoms |
|
|
Neuroanatomy
|
GET FROM MELISSA DONT HAVE IN NOTES!! :(
|
|
|
What are the 3 Afferent Types?
|
1. Interoceptors
2. Exteroceptors 3. Proprioceptors |
|
|
Interoceptors are:
|
Found within the system
Monitor blood pressure internally Blood o2 levels |
|
|
Exteroceptors are:
|
anything that responds outside the body
Ex. Eyes, Ears, Mouth, Etc. |
|
|
Proprioceptors can be:
|
a mixture of both Interoceptors & Exteroceptors
|
|
|
A Delta Fibers are:
|
1.Primarily mechanical nociceptors which are Sensitive to pressures intense enough to cause damage
2. Sensation is sharp, pricking & last 4 a short duration 3. Localized & tolerated well |
|
|
C Fibers make up:
|
1.Majority of nociceptors
2.Sensitive to very intense mechanical & temperature **Some are Specific to chemical (acid, irritants, inflammatory mediators) or mechanical pressure only |
|
|
Non-Nociceptive Afferents are mechanoreceptors which include:
|
1. Meissner’s corpuscles
2. Pacinian corpuscles 3. Merkel’s discs 4. Ruffini ending **Should not cause pain! |
|
|
Meissner's Corpuscles are:
|
very sensitive to light touch
**Found most places on the body |
|
|
Pacinian Corpuscles are:
|
found to be more adapt to changes in pressure & vibration
**Juries still out if research can tell the difference between smooth and rough |
|
|
Merkel discs tend to:
|
pressure and texture
Ex. Smooth and Rough |
|
|
Ruffini Endings have:
|
1. No adaptation in general (Alot Deeper)
2. SUSTAINED PRESSURE 3. Deals with mechanical deformation of joints *Can act as thermoreceptors (DEEP BURN,not good) |
|
|
Proprioceptors in Non-Nociceptive Afferents exist in:
|
Joint capsules, Muscles & Tendons
Ex. Ruffini endings, Muscle spindles & Golgi tendon organs |
|
|
Thermoreceptors in Non-Nociceptive Afferents sense:
|
Change in temperature in the skin, Joint capsules and Ligaments
Ex. Krause’s end bulb & Ruffini |
|
|
Krause's End Bulb is:
|
more adapt to cold temperature than hot temperature
|
|
|
Thermal Nociceptors deal with:
|
1. Both A delta and C fibers
2. Some are sensitive to changes that barely vary from the norm (depending the severity of the burn) 3. Others require extreme temps to fire |
|
|
Some A Delta and C Fibers respond to __________, in the interoceptors category:
|
1. Molecules of local metabolism
2. Mast cell activation 3. Hormonal activity |
|
|
Homeostatic Receptors have:
|
Low threshold A delta fibers & can send signals of weak mechanical stimuli
**It Evoke feelings of sensory touch &Emotional response comes into play (Ex. Pleasure Memory) |
|
|
Chemical Nociception is:
|
1. Tissue trauma causes a release of multiple chemicals from the damaged cells
2. These elicit a response from nociceptors to release various neuropeptides 3. Then Enhances the sensation of pain |
|
|
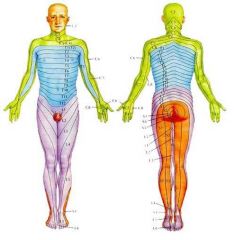
Name the Different Levels of Dermatones:
|
???? GET FROM LAB PAPERS!!!
|
|
|
Parallel Ascending Pathways of Pain goes from:
|
From spinal cord to higher centers & have mult. pathways.
|
|
|
The most important pathway of the Parallel Ascending Pathways of Pain is:
|
**Spinothalamic Tract**
Other Tracts: Spinomesencephalic , Spinoparabrachial, Spinoreticular, Spinohyphothalamic-limbic |
|
|
All the Parallel Ascending Pathways of Pain make up what system?
|
Anterolateral System
|
|
|
Spinothalamic Tract consists of:
|
1. Discrimitive pain
2. Temperature 3. Crude touch 4. Pressure **STOPPED HERE FOR QUIZ THURSDAY!!!** |
|
|
Spinomesencephalis Tract consists of:
|
1. Pain modulation
2. Sensorimotor integration of pain 3. Motor reflex to pain |
|
|
Spinoparabrachial Tract consists of:
|
the affective component of pain
|
|
|
Spinoreticular Tract consists of:
|
1. Modulation of pain
2. Motivational, emotional, unpleasant component of pain |
|
|
Spinohypothalamic-Limbic Tract consists of:
|
Autonomic adjustments to pain
|
|
|
Anterolateral Systems "Take Home" message is that is has:
|
1. Multiple ascending pathways
2. Ipsilateral, contralateral, bilateral 3. Redundant system |
|
|
Names the Different States of pain:
|
1. Acute Pain
2. Referred Pain 3. Persistent Pain |
|
|
Acute Pain is:
|
Sharp
Localized Rapid onset Short duration (usually) Warning of tissue damage (actual or potential) |
|
|
Referred Pain is:
|
Pain at a site remote from the source of pathology & occurs due to convergence
Brain unable to decipher or determine where pain is coming from |
|
|
Persistent Pain is:
|
Pain that is recurrent or episodic
May accompany a re-injury or associated chronic condition |
|
|
You can assess pain by:
|
1. Numerical
2. Verbal rating scale 3. Visual analog scale |
|
|
Assessment Scales should include:
|
Severity
Location Quality Observation of non verbal cues Mode, duration of onset Provocating and relieving factors |
|
|
Numerical Pain Scale Is:
|
Give pt 0 to 10
Qualify numbers What is zero, what is ten |
|
|
Verbal Rating Scale is:
|
No pain, mild, moderate, etc.
|
|
|
Visual Analog Scale is:
|
Number line, or Faces for Kids!
|
|
|
Abnormal Pain can be:
|
1. Allodynia
2. Hyperalgesia 3. Neuropathic 4. Chronic Pain |
|
|
C Fibers temperatures ranges are from:
|
< 59 deg F > 123 deg F
|
|
|
How large are A Delta and C Fibers?
|
Aδ: Diameter = 1-5 µm; velocity = 2-30 m/sec
C: Diameter = 0.2-1.5 µm; velocity = no more than 2 m/sec |
|
|
C Fibers are:
|
1. Unmylinated & free nerve endings (STRONGER intensity with the stimuli)
2. Stronger Intensity, slow deeper pain &unspecificed area 3. Associated with Chronic Pain 4. Are second to A delta fibers 5. Kick in after a “MONTH” |
|
|
A Delta is:
|
1. Faster than C Fibers
2. Very Fast Onset of Action 3. Mylinated 4. Tolerated Pretty Well Ex. Touching a Hot Stove |
|
|
Dorsal Horn (Dorsal Root Ganglion-DRG) afferents enter:
|
The spine via the dorsal portion of the spinal nerve
Two point discrimination & proprioception enter through the medial portion of the dorsal root Nociception (Pain) enters the lateral portion of the dorsal root |
|
|
DRG (Dorsal Root Ganglion) afferent terminates on:
|
The appropriate laminae! They then ascends one to two spinal levels via Lissauer’s tract
Crosses in anterior white commissure Goes up the spinothalamic tract |
|
|
Nociception means:
|
PAIN!!!
|
|
|
7 to 8 Times more likely to go into chronic pain if _________ gets injured?
|
Dorsal Root Ganglion (DRG)
|
|
|
DRG (Dorsal Root Ganglion doesn't produce pain for up to:
|
2 - 3 weeks
**This is where Work Comp patients get a bad wrath |
|
|
Examples of Sensory Evaluations are:
|
Touch (light touch, discrimination)
Pain: sharp/dull Temperature Vibration |
|
|
Why Do We Need to Assess Sensation?
|
1. Determine areas of sensory loss
2. Following nerve damage (either peripheral or CNS) 3. Before using modalities that could potentially cause harm 4. SAFETY |
|
|
Sensation is:
|
All sensory neuron cell bodies are in the dorsal root ganglia
Considerable overlapping of one area to another Superficial or Deep |
|
|
The Receptors Activated by Touch are:
|
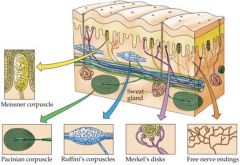
Free nerve endings (FNE)
Hair follicle receptors Meisner Corpuscles Merkel’s Discs Ruffini Endings Krause Endbulbs |
|
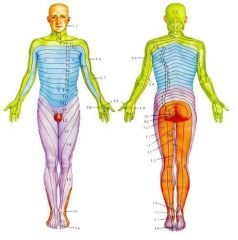
Name all the Dermatone Levels:
|
FINISH
|
|
|
When testing Touch on the Sensory Test, you need to:
|
Use piece cotton or tissue
Ask patient to say “yes” each time they are touched- “I want you to tell me when you feel me touch you” Eyes closed Soles and palms need heavier stimulus-hairier areas need less stimulation Test on known innervated area first |
|
|
Tonic Stimulation is:
|
Some sensory receptors respond to tonic activity like Pacinian Corpuscles
|
|
|
Nociceptor is:
|
Nerve fiber that fires in response to damaging or potentially damaging stimuli
|
|
|
Noxious Stimuli include:
|
Mechanical
Temperature Chemical Electric |
|
|
When testing Pain in the Sensory Test, you need to:
|
Use pinprick; unfolded paper clip
Eyes closed Deliver stimulus in random fashion Don’t deliver more then 1 stimulus per second If find decreased sensation, determine boundaries |
|
|
With Temperature, Warm Fibers are:
|
Increase firing with increased temperature
Fire for duration of stimulus Stop firing when warm stimulus removed Do not respond to mechanical stimulus |
|
|
With temperature, Cold Fibers are:
|
Increase firing with decreased
|
|
|
When do pain receptors begin to fire?
|
Below 20°C and above 45°C
|
|
|
When testing Temperature in Sensory Test, what do you need to do?
|
Expose area of skin to be tested
Use 2 test tubes one with hot water, one with cold water Eyes closed Randomly apply tubes to body part in question Ask if feels “less hot or less cold” in comparison to normal side |
|
|
Vibration uses:
|
Pacinian corpuscles and deep afferent nerves
Rarely affected by lesions of single nerves Involved with polyneuritis & dorsal column disease Commonly lose vibration & position sense together |
|
|
When testing Vibration in the Sensory Test, you need to:
|
Use tuning fork
Place tuning fork over bony prominence and compare to other side |
|
|
Two-point Discrimination is:
|
Involves sensory cortex and sensory projections from thalamus
Measures the smallest separation between 2 points on the skin that is perceived as 2 stimuli Use compass or 2 point aesthesiometer |
|
|
When testing Two-Point Discrimination, you need to:
|
Eyes closed
Apply 2 stimuli to skin-ask if feels 1 or 2 points Varies depending on body location EX: 2-3 mm lips, 3-5 mm fingertips, 20-30 mm on dorsum of hands and feet, 4-8 cm on trunk |
|
|
Proprioceptors are:
|
Provide information on joint position and muscle tone (Muscle Spindle, Golgi Tendon Organ)
Free Nerve Endings (Pain, Touch) Pacinian Corpuscle (Deep Pressure) |
|
|
Stereoaugnosis Testing is:
|
Place Familiar Object In Hand and Ask to Identify
|
|
|
Tactile Location Testing is:
|
Touch Patient, where the Pressure is Placed
|
|
|
Barloaugnosis Testing is:
|
Two Objects - - > One in each hand, different weights of Objects, Ask which object is heavier
|
|
|
Graphesthesia Testing:
|
Recognizes Letter Or Design Traced On Skin
Ex. Dram "R" on back or any part of body |
|
|
Texture is:
|
Telling the Difference between:
Smooth Vs. Rough Silk Vs. Scrubber Pad |

