![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
28 Cards in this Set
- Front
- Back
|
what are hypersensitivity reactions?
|
normal immune reactions that produce undesired results
|
|
|
Type 1 Immune Reactions: Characteristics
|
Antibody Mediated- IgE
soluble antigen mechanism: mast-cell activation |
|
|
name the type of allergy reaction the results from the allergen entering the body thru different routes
|
Systemic Anaphylaxis- blood
Acute Urticarial- skin Seasonal Rhino Conjunctivitis- eyes and nose Asthma- lungs Food Allergy- GI tract |
|
|
which hypersensitivity reactions are antibody mediated? which are cell mediated?
|
I, II, III are antibody mediated
IV is cell mediated (involves T cells in the immune response; does not involve antibodies) |
|
|
what makes types II and III different?
|
where they occur
Type II occurs on cell surfaces Type III occurs freely in fluid phase |
|
|
how do we develop sensitivity to a particular antigen?
|
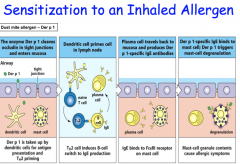
allergen must pass the barrier epithelium and be endocytosed by a DC, resulting in feeble activation
the feebly activated DC, along with help from TGF-beta polarizes a naive T-cell into a Th2 helper T cell this Th2 cell then drives a class switch in the B-cell to a IgE producing plasma cell the IgE antibodies attach to Fc receptors on the mast cells of the mucosa, preparing the body to mount an allergic response whenever it encounters that particular antigen the allergic response involves the allergen cross-linking IgE antibodies on mast cells, causing them to degranulate and release their pharmacologically active mediators |
|
|
TH2 polarization and sensitization
|
in NORMAL individuals, DC activation from an immunogen induces Treg production
in people with allergic predispositions, however, TH2 is produced, giving rise to IgE |
|
|
what facilitates TH2 polarization?
|
-intrinsic properties of the antigen (small, soluble, and stable)
-low antigen dose -route of presentation: skin and mucosa -cytokines: IL-4, 5, 9, 13 |
|
|
what signals facilitate class switching to IgE in B lymphocytes?
|
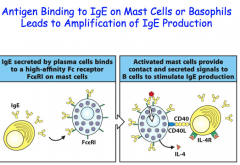
IL-4 and IL-13 (TH2 cells, mast cells, basophils)
CD40 (B-cell) - CD40L (T-cell) ligation |
|
|
effects of mast-cell activation
|
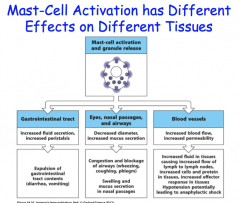
different effects in different tissues
-can actually amplify IgE production by interacting with plasma cells by releasing IL-4 and through CD40-CD40L interactions the 2 main targets of the pharmacologically active mediators released by granulocytes are smooth muscle and blood vessels, allowing for typical immune response (edema, mucous secretion, etc.) |
|
|
IL-4, IL-13
|
stimulate and amplify Th2-cell response
|
|
|
TNF-alpha
|
cytokine that promotes inflammation, stimulates cytokine production by many cell types, activates endothelium
|
|
|
role of eosinophils
|
type I reactions
similar role as mast cells release granule antimicrobials that have hydrolytic effects and cause significant tissue damage *secrete TH2-type cytokines (inducing further TH2 polarization, in addition to TH1 T-cell Toxic chemicals (IDO) -inhibits TH1 polarization |
|
|
IgE-Mediated Allergic Reactions Rapid and Chronic Responses
|
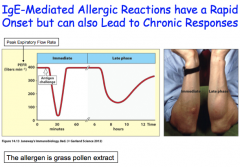
immediate onset- appears as a wheel and flair appearance on the skin, which are the effects of edema and inflammation
late onset- comes a few hours later; greater swelling of the area from increased cellular infiltrates (prostaglandins, leukotrienes, chemokines, and cytokines) -more dangerous, especially in the lungs, because it can lead to fibroids and decreased lung capacity |
|
|
chronic response in Type I
|
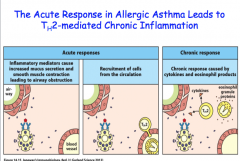
migration of TH2 cells and eosinophils to the site of inflammation from the increased permeability of the vascular tissue and the chemokines released by the mast celts
soluble Ag contacts IgE, facilitates cross-linking, releases, pro-inflammatory mediators from within mast cell, up regulates fluid secretion, and increases smooth muscle cell contraction |
|
|
type II hypersensitivity
|
cell surface IgG mediated
occurs when antigens bind to IgG antibodies on cell surfaces in the body, usually red blood cells and platelets, and trigger cellular damage in one of the following manners 1. complement-mediated cell lysis 2. phagocytosis and clearance 3. Antibody-Dependent Cell-Mediated Cytotoxicity (ADCC)- Arming of NK cells |
|
|
3 examples of Type II hypersensitivity reactions
|
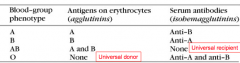
1. blood transfusion mismatch
2. erythroblastosis fatalis 3. drug-induced hemolytic anemia |
|
|
Erythroblastosis Fatalis
|
If an Rh- mother were to become pregnant with a Rh+ baby, theres a possibility that RBCs with the Rh antigen will travel into the maternal circulation during delivery.
-if this happened, the mom would produce memory and plasma B cells with IgG antibodies specific for the Rh+ RBC's In subsequent pregnancies with Rh+ babies, the mom's memory cells would recognize fetal Rh+ RBC's and IgG antibodies would cross the placenta to selectively attack the fetal RBCs, causing erythroblastosis fatal is |
|
|
how do we prevent erythroblastosis fatalis?
|
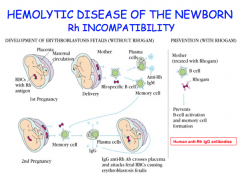
treat the mom with Rhogam, which is a passive therapy of IgG for thesis antigen during delivery
-these IgG antibodies bind and clear the Rh+ RBCs before the maternal immune system can recognize them and mount an immune response |
|
|
how can we determine if the mother is producing IgG antibodies against fetal Rh+ RBCs?
|

Coombs Test
Direct: Is there Ab bound to the fetal red blood cells? -look for fetal RBC with maternal Ab bound -add 2nd anti-human antibody, which is an antibody to human IgG -agglutination/clumping occurs if moms Ab's are present Indirect: Does mom have Ab's in her body that recognize Rh? -incubate her blood serum with Rh+ RBC -if she has Rh antibody, they will bind RBC -use Coombs reagent again to facilitate cross-linking and agglutination |
|
|
drug induced hemolytic anemia
|
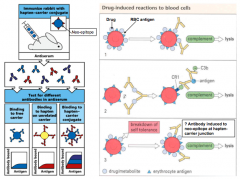
type II hypersensitivity reaction
hapten drugs, like penicillin, like to bind to large carrier proteins, particularly RBCs and platelets some individuals make IgG antibodies against these drugs, and since the metabolite is bound to a cell, the cell is damaged as a side effect |
|
|
type III hypersensitivity
|
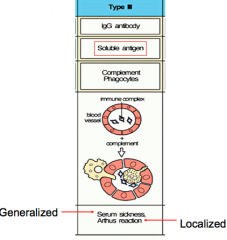
fluid-phase IgG mediated
also called the immune complex disease bc it forms immune complexes of soluble IgG antibodies bound to antigens type III hypersensitivity occurs when the antigen's are in excess because they form small immune complexes (small antibody:antigen complexes) |
|
|
Type III hypersensitivity and Immune Complexes
|
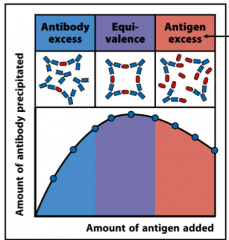
Type III hypersensitivity occurs when antigen's are in excess because they form small immune complexes
-these complexes are too small to precipitate so they get stuck in capillaries and cause damage small immune complexes tend to lodge where there are large amounts of blood flow -i.e., choroid plexus, glomerulus of the kidney, lung this provokes an immune response and damages the tissue the most efficient type of immune complex is when antibodies and antigens are in equivalency |
|
|
serum sickness
|
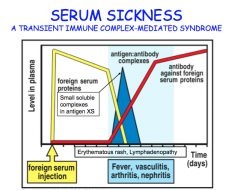
"generalized" type III reaction
when a bunch of foreign serum is injected into the body , IgG antibodies against the antigen begin the be made since antigen is in excess, it forms small immune complexes, which get trapped in the capillary beds the immune system response by phagocytosis and complement mediated destruction, which causes fever, vasculitis, arthritis, and nephritis -theses are all transient tho and disappear as the body is able to clear out the antigen |
|
|
arthus reaction
|
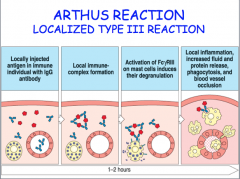
"localized" type III reaction
occurs when an individual is immunized and has high levels of antibodies against the vaccine at the site of vaccination, an IgG:Antigen immune complex forms, which then binds to the Fc receptor on mast cells -this induces mast cell degranulation, which amounts an immune response examples: -bee stings -farmers' lung from moldy sugar cane -bird fancier's lung from bird sh!t |
|
|
Type IV Hypersensitivity Reactions
|
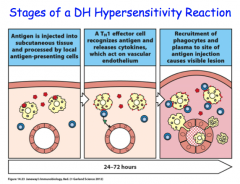
Cell Mediated
-the only type of hypersensitivity that doesn't involve antibodies; uses T-cells instead Takes MUCH longer bc DCs have to pick up the Ag, travel to the lymph node, present a peptide to a naive T cell, the T cell undergoes clonal expansion, and T-cell leaves the node to travel back to the site of infection ~24-38 hours after infection starts |
|
|
Tuberculosis skin test
|
uses the Type IV hypersensitivity
involves injecting purified protein derivative (PPD) into the skin to see whether the body has already produced T cells to combat tuberculosis from a previous infection if the T-cells are present, it will facilitate an immune reaction |
|
|
contact-sensitizing agents
|
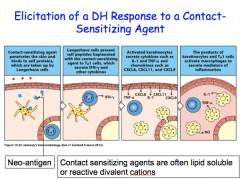
small, highly-reactive molecule that can easily penetrate skin
use T-cells poison Ivy |

