![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
292 Cards in this Set
- Front
- Back
|
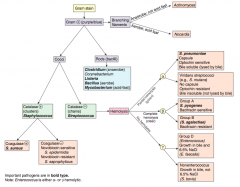
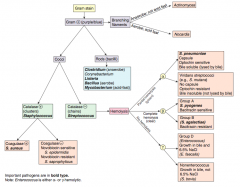
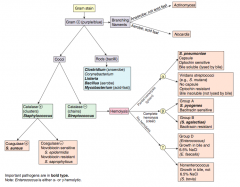
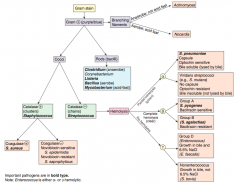
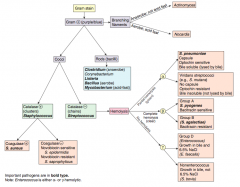
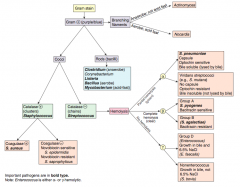
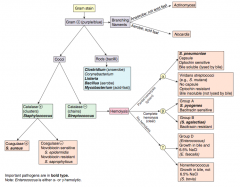
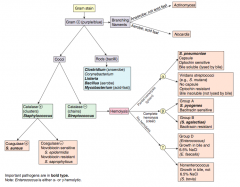
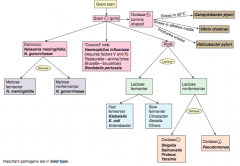
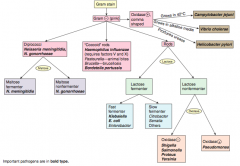
Which bacteria are G+ with branching filaments? How do you distinguish them? |
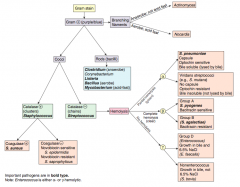
- Actinomyces (anaerobe, not acids fast) |
|
|
Which bacteria are G+ rods? How do you distinguish some of them? |
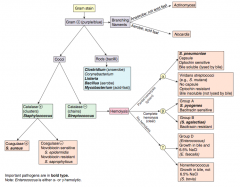
- Clostridium (anaerobe) |
|
|
How do you distinguish the G+ cocci? |
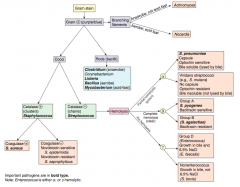
- Catalase test |
|
|
Which bacteria are G+ and catalase +? How do you distinguish them? |
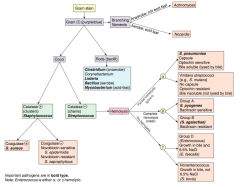
Staphylococcus (clusters) |
|
|
Which bacteria are G+ and catalase -? How do you distinguish them? |
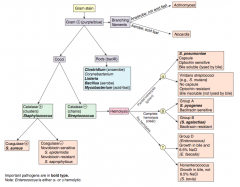
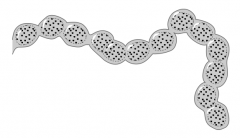
Streptococcus (chains) |
|
|
Which bacteria are G+, catalase +, and coagulase +? Organization? |
S. aureus - cocci in clusters |
|
|
Which bacteria are G+, catalase +, and coagulase -? Organization? |
Clusters of cocci: |
|
|
Which bacteria are G+, catalase -, and have partial hemolysis (green)? |
α-hemolytic Streptococcus (chains) |
|
|
Which bacteria are G+, catalase -, and have complete hemolysis (clear)? |
β-hemolytic Streptococcus (chains) |
|
|
Which bacteria are G+, catalase -, and have no hemolysis? |
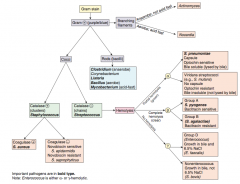
γ-hemolytic Streptococcus (chains) |
|
|
What are the types of hemolysis? |
- α-hemolysis: partial (forms green ring around colonies on blood agar) |
|
|
What does α-hemolysis mean? What are the types of bacteria that fall under this category? |
Partial hemolysis (green ring around colonies on blood agar) |
|
|
What does β-hemolysis mean? What are the types of bacteria that fall under this category? |
Comlete hemolysis (clear area around colonies on blood agar) |
|
|
What does γ-hemolysis mean? What are the types of bacteria that fall under this category? |
No hemolysis |
|
|
What does the "on the office's "staph" retreat, there was no stress" mnemonic mean? |
Staphylococcus - NO StRESs: |
|
|
What does the "overpass" mnemonic indicate? |
OVRPS: |
|
|
What does the "B-BRAS" mnemonic indicate? |
B-BRAS |
|
Which bacteria: |
Staphylococcus aureus |
|
|
Which virulence factor does Staphylococcus aureus use? Mechanism? |
Protein A: |
|
|
Where does Staphylococcus aureus colonize / infect? |
- Commonly colonizes: nose |
|
|
What does Staphylococcus aureus cause? |
Inflammatory Disease: |
|
|
What are the toxin mediated diseases of S. aureus? Toxin? |
- Toxic Shock Syndrome (TSST-1) |
|
|
What is an important cause of serious nosocomial and community-acquired infections? |
MRSA (Methicillin-Resistant S. aureus) |
|
|
What is TSST? Mechanism of action? What does it cause? |
Toxic Shock Syndrome Toxin → Toxic Shock Syndrome |
|
|
What predisposes to Toxic Shock Syndrome? |
Use of vaginal or nasal tampons |
|
|
Which bacteria causes rapid food poisoning? Mechanism? |
S. aureus food poisoning is due to ingestion of preformed toxin (enterotoxins) |
|
|
How does S. aureus form an abscess? |
Forms fibrin clot around itself → abscess |
|
|
Which bacteria is known for infection prosthetic devices and IV catheters? Mechanism? |
Staphylococcus epidermidis |
|
|
Characteristics of Staphylococcus epidermidis? |
Catalase (+), Coagulase (-) |
|
|
Which bacteria are the first and second most common cause of uncomplicated UTI in young women? |
1. E. coli |
|
|
Characteristics of Staphylococcus saprophyticus? |
Catalase (+), Coagulase (-) |
|
|
What does Streptococcus pneumoniae cause? |
Most common cause of: |
|
|
Characteristics of Streptococcus pneumoniae? |
Catalase (-), α-hemolysis (partial) |
|
|
What are the signs of Streptococcus pneumoniae? |
- Rusty sputum |
|
|
Which bacteria is a normal flora of the oropharynx and causes dental caries? |
Streptococcus mutans (Viridans group Streptococci) |
|
|
Which bacteria causes subacute bacterial endocarditis at damaged valves? Mechanism? |
Streptococcus sanguinis (Viridans group Streptococci) |
|
|
Characteristics of Viridans groups Streptococci? |
Streptococcus mutans & Streptococcus sanguinis |
|
|
What is the name of Group A Streptococci? |
Streptococcus pyogenes |
|
|
What does Streptococcus pyogenes cause? |
Pyogenic infections: |
|
|
What are the pyogenic infections caused by Streptococcus pyogenes? |
- Pharyngitis |
|
|
What are the toxigenic infections caused by Streptococcus pyogenes? |
- Scarlet fever |
|
|
What are the immunologic infections caused by Streptococcus pyogenes? |
- Rheumatic fever |
|
|
Characteristics of Streptococcus pyogenes? |
Group A, β-hemolysis: |
|
|
What enhances host defenses against Streptococcus pyogenes? |
Antibodies to M protein |
|
|
How can you detect a Streptococcus pyogenes infections? |
ASO titer detects recent S. pyogenes infection |
|
|
What are the diagnostic criteria for Rheumatic Fever? Cause? |
J♥︎NES criteria: |
|
|
Untreated pharyngitis caused by Streptococcus pyogenes can lead to what? |
- Rheumatic fever |
|
|
Impetigo more commonly precedes what immunologic manifestation of S. pyogenes? |
Impetigo more commonly precedes glomerulonephritis than pharyngitis |
|
|
What are the symptoms and cause of Scarlet Fever? |
Symptoms: |
|
|
Which bacteria causes pneumonia, meningitis, and sepsis mainly in babies? |
Streptococcus agalactiae (group B streptococci) |
|
|
Characteristics of Streptococcus agalactiae? |
Group B, β-hemolysis: |
|
|
Why does Streptococcus agalactiae (group B) commonly infect babies? Implications? |
- It colonizes the vagina - then it is spread to babies during a vaginal birth |
|
|
What is the mechanism of Streptococcus agalactiae (group B)? |
- Produces CAMP factor |
|
|
Which G+ bacteria is found in normal colonic flora and can cause UTIs, biliary tract infections, and subacute endocarditis (after GI/GU procedures)? |
Enterococci faecalis and faecium (group D) |
|
|
Characteristics of Enterococci? |
Group D Streptococci |
|
|
What kind of infections do Enterococci cause? |
- UTI |
|
|
What kind of bacteria are classified as Group D Streptococci? Difference? |
Enterococci (E. faecalis and E. faecium) |
|
|
What determines whether a bacteria is Group A/B/C/D? |
Lancefield grouping - based on differences in the C carbohydrate on the bacterial cell wall, variably hemolysis |
|
|
What is an important cause of nosocomial infection by Enterococci? |
VRE: Vancomycin-Resistant Enterococci |
|
|
Which G+ bacteria is found in normal colonic flora and can cause bacteremia and subacute endocarditis in colon cancer patients? |
Streptococcus bovis (group D) |
|
|
Characteristics of Streptococcus bovis (group D)? |
- Colonizes the gut |
|
Which bacteria causes pseudomembranous pharyngitis (grayish-white membrane) w/ lymphadenopathy? |
Corynebacterium diphtheriae - via exotoxin encoded by β-prophage, inhibits protein synthesis via ADP-ribosylation of EF-2 |
|
|
Which bacteria releases diphtheria exotoxin? Mechanism? |
Corynebacterium diphtheriae - exotoxin encoded by β-prophage, inhibits protein synthesis via ADP-ribosylation of EF-2 |
|
|
What are the symptoms of Corynebacterium diphtheriae infection? |
- Pseudomembranous pharyngitis (grayish-white membrane) |
|
|
How do you diagnose Corynebacterium diphtheriae infection? |
- G+ rods w/ metachromatic (blue and red) granules |
|
|
How can you prevent infection with Corynebacterium diphtheriae? |
Toxoid vaccine |
|
|
Which bacteria form spores? |
Spore-forming G+ bacteria in soil: |
|
|
What causes bacteria that form spores to make spores? Purpose? |
- Form spores at the end of the stationary phase when nutrients are limited |
|
|
What are the characteristics of spores? |
- Highly resistant to heat and chemicals |
|
|
How do you kill spores? |
Must autoclave (as is done to surgical equipment) by steaming at 121°C for 15 minutes |
|
|
Which bacteria are G+, spore-forming, obligate anaerobic bacilli? |
Clostridia |
|
|
What kind of toxin is produced by Clostridium tetani? |
Tetanospasmin / Tetanus toxin (exotoxin) |
|
|
What bacteria releases Tetanus toxin? Effects? |
Clostridium tetani |
|
|
What is trismus? Cause? |
Lockjaw - caused by Tetanus toxin from Clostridium tetani |
|
|
What is Risus Sardonicus? Cause? |
Spasm of facial muscles causing a grin - caused by Tetanus toxin from Clostridium tetani |
|
|
What kind of toxin is produced by Clostridium botulinum? |
Preformed, heat-labile toxin |
|
|
What bacteria releases a preformed, heat-labile toxin? Effects? |
Clostridium botulinum |
|
|
How does C. botulinum infect adults? Infants? |
"BOTulinum is from bad BOTtles of food and honey) |
|
|
Why shouldn't babies eat honey? |
- Honey can contain spores from C. botulinum |
|
|
What kind of toxin is produced by Clostridium perfringens? |
α-Toxin ("lecithinase" a phospholipase) |
|
|
What bacteria releases α-Toxin? Effects? |
Clostridium perfringens |
|
|
What kind of toxin is produced by Clostridium difficile? |
Produces 2 toxins |
|
|
What bacteria releases Toxin A? Effects? |
Clostridium difficile |
|
|
What bacteria releases Toxin B? Effects? |
Clostridium difficile |
|
|
What often precedes infection by Clostridium difficile? Symptoms? |
- Often secondary to antibiotic use, especially clindamycin or ampicillin |
|
|
How do you diagnose Clostridium difficile infection? Treat? |
Diagnose: |
|
|
What is the only bacterium with a polypeptide capsule (contains D-glutamate)? |
Bacillus anthracis |
|
|
Which bacteria causes Anthrax? Characteristics? |
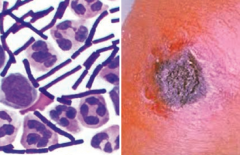
Bacillus anthracis |
|
|
What are the forms of infection caused by Bacillus anthracis? |
- Cutaneous anthrax |
|
|
What are the symptoms of Cutaneous Anthrax? |
- Boil like lesion → ulcer with black eschar (painless, necrotic) |
|
|
What are the symptoms of Pulmonary Anthrax? |
- Inhalation of spores → flu-like symptoms |
|
|
What is the term for Pulmonary Anthrax caused by inhalation of spores from contaminated wool? |
Woolsorters' Disease |
|
|
Which bacteria causes food poisoning commonly from reheated rice? |
Bacillus cereus |
|
|
What kind of infection is caused by Bacillus cereus? Source of infection? |
- Food poisoning: spores survive cooking rice, keeping rice warm results in germination of spores and enterotoxin formation |
|
|
What is responsible for the emetic type of food poisoning due to Bacillus cereus? How soon? |
Cereulide (preformed toxin) in rice and pasta, causes symptoms within 1-5 hours |
|
|
How quickly do diarrheal type symptoms from Bacillus cereus occur? |
Within 8-18 hours |
|
|
What bacteria can be found in unpasteurized dairy products and infected deli meats? |
Listeria monocytogenes |
|
|
Characteristics of Listeria monocytogenes? |
- G+ facultative intracellular microbe |
|
|
How can Listeria monocytogenes be acquired? |
- Ingestion of unpasteurized dairy products and deli meats |
|
|
How does Listeria monocytogenes avoid host defenses? |
- Avoids antibody by forming "rocket tails" (via actin polymerization) that allows them to move through the cytoplasm and into the cell membrane |
|
|
What can infection with Listeria monocytogenes cause? |
- Amnionitis, septicemia, and spontaneous abortion in pregnant women |
|
|
What does Listeria monocytogenes cause in healthy patients? How do you treat? |
Gastroenteritis (mild) - usually self-limited |
|
|
What does Listeria monocytogenes cause in pregnant patients? |
- Amnionitis |
|
|
What does Listeria monocytogenes cause in infants patients? How do you treat? |
- Granulomatosis infantiseptica |
|
|
What does Listeria monocytogenes cause in immunocompromised patients? How do you treat? |
Meningitis (treat empirically with Ampicillin) |
|
|
Which bacteria form long, branching filaments resembling fungi? |
- Actinomyces |
|
Which bacteria causes oral/facial abscesses that drain through sinus tracts forming yellow "sulfur" granules? How do you treat? |
Actinomyces - treat with Penicillin |
|
|
Characteristics of Actinomyces? |
- G+ anaerobe |
|
|
Which bacteria causes pulmonary infections in immunocompromised patients and cutaneous infections after trauma in immunocompromised patients? How do you treat? |
Nocardia - treat with Sulfonamides |
|
|
Characteristics of Nocardia? |
- G+ aerobe |
|
|
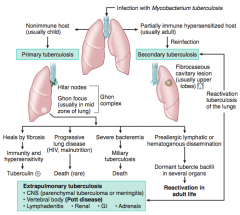
What causes Tuberculosis? Different forms of infection? |
Infection with Mycobacterium tuberculosis |
|
|
What are the signs of a Primary Tuberculosis? |
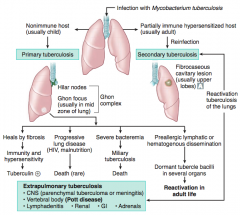
Occurs in a non-immune host (usually a child) |
|
|
What can Primary Tuberculosis lead to? |
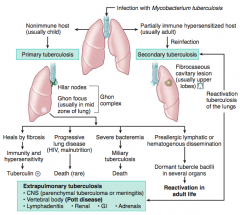
- Heals by fibrosis → immunity and hypersensitivity → Tuberculin (+) |
|
|
What are the signs of a Secondary Tuberculosis? |
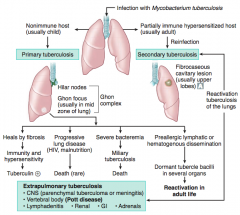
Fibrocaseous cavitary lesion (usually in upper lobes) |
|
|
What can Secondary Tuberculosis lead to? |
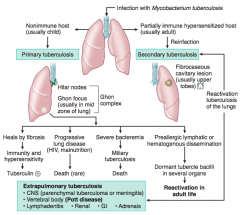
Extrapulmonary Tuberculosis |
|
|
What does a positive PPD test mean? |
Either: |
|
|
What does a negative PPD test mean? |
Either: |
|
|
Which test is more specific than PPD for Mycobacterium tuberculosis infection? |
Interferon-γ Release Assay (IGRA) |
|
|
Which vaccine is used to prevent Tuberculosis? |
BCG vaccine |
|
|
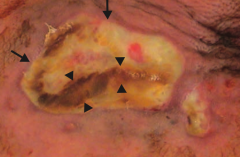
What is the appearance of a caseating granuloma in tuberculosis infection? |
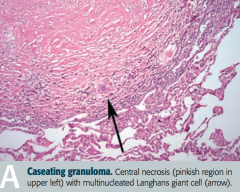
- Central necrosis (pinkish region in upper left) |
|
|
What are the symptoms of TB? |
- Fever |
|
|
What are the species of Myocbacterium? What disease do they cause? |
- M. tuberculosis (TB, often resistant to multiple drugs) |
|
|
What are the characteristics of all Mycobacteria? |
All are acid-fast organisms |
|
|
Which bacteria causes disseminated, non-TB disease in AIDS patients? Treatment / prevention? |
Mycobacterium avium-intracellulare |
|
|
What is released by virulent strains of Mycobacteria? Implication? |
Cord fator is found in virulent strains |
|

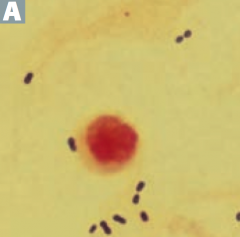
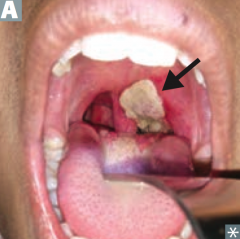
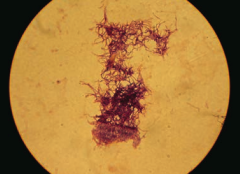
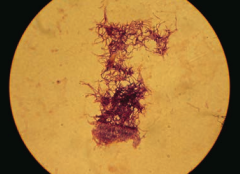
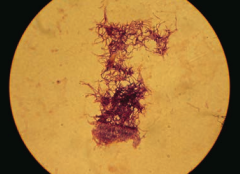
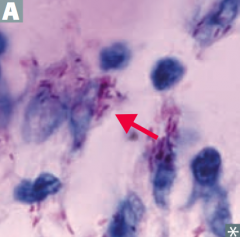
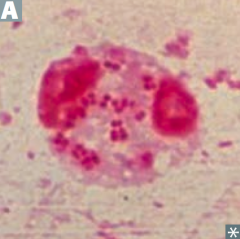
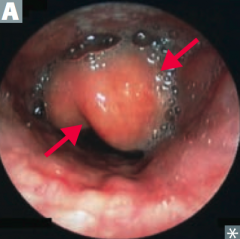
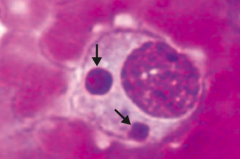
Which bacteria causes this appearance? |
Mycobacterium leprae (Leprosy / Hansen disease) |
|
|
Characteristics of Mycobacterium leprae? |
- Acid-fast bacillus |
|
|
What does Mycobacterium leprae infect? |
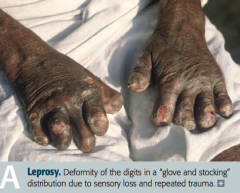
- Skin |
|
|
What are the forms of Leprosy / Hansen disease? Characteristics? |

Lepromatous: |
|
|
Which form of Leprosy has a LOW cell-mediated immunity with a humoral Th2 response? |
Lepromatous form |
|
|
Which form of Leprosy has a HIGH cell-mediated immunity with a largely Th1-type immune response? |
Tuberculoid form |
|
|
How do you treat the two forms of Leprosy / Hansen disease? |
Lepromatous form: |
|
|
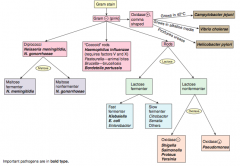
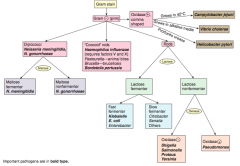
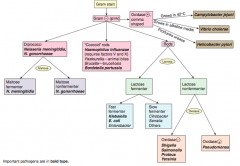
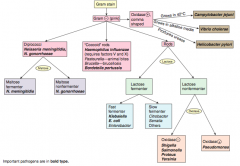
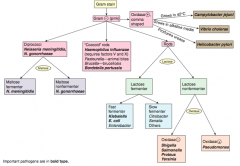
How should you first distinguish G- (pink) bacteria? |
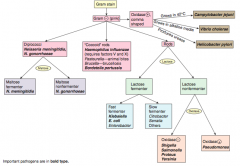
Shape |
|
|
Which bacteria are G- diplococci? How do you distinguish them? |
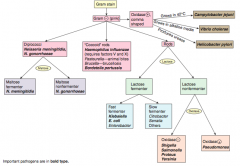
Distinguish based on ability to ferment maltose |
|
|
Which bacteria are G- coccoid rods? How do you distinguish them? |
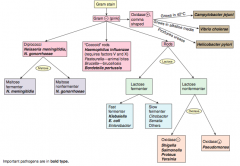
* Haemophilus influenzae (requires factors V and X) |
|
|
Which bacteria are G- rods? How do you distinguish them? |
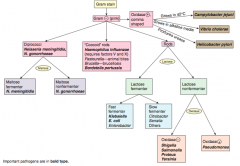
Distinguish based on ability to ferment lactose and distinguish non-fermenters by oxidase capability: |
|
|
Which bacteria are lactose fermenting G- rods? How do you distinguish them? |
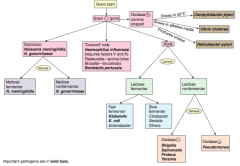
Fast fermenters: |
|
|
Which bacteria are non-lactose fermenting G- rods? How do you distinguish them? |
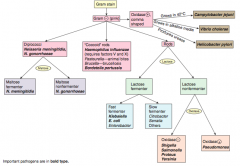
Oxidase (+): |
|
|
Which bacteria are oxidase (+), comma shaped G-? How do you distinguish them? |
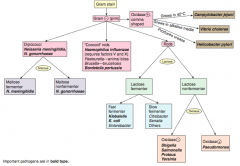
Grows in 42°C: |
|
|
How do you determine if a bacteria can ferment lactose? |

*If it can grow pink colonies on MacConkey agar |
|
|
Can E. coli ferment lactose? Why or why not? |
Yes - E. coli produces β-galactosidase, which breaks down lactose into glucose and galactose |
|
|
G- bacilli are resistant to what antibiotics? What are they susceptible to? |
- Resistant to Penicillin G and Vancomycin (G- outer membrane layer inhibits entry) |
|
|
Neisseria species are what type of bacteria? What can they ferment? |
G- diplococci |
|
|
What do Neisseria species produce? |
IgA proteases |
|
|
Which bacteria is sexually transmitted and can also cause septic arthritis, neonatal conjunctivitis, pelvic inflammatory disease (PID), and Fitz-Hugh-Curtis Syndrome? Treatment? |
Neisseria gonorrhoeae |
|
|
Characteristics of Neisseria gonorrhoeae? |
G- diplococci |
|
|
What can Neisseria gonorrhoeae infection cause? Prevention? |
Prevent sexual transmission w/ condoms |
|
|
Which bacteria is spread via respiratory and oral secretions, causing meningococcemia and meningitis as well as Waterhouse-Friderichsen syndrome? Treatment? |
Neisseria meningitidis |
|
|
Characteristics of Neisseria meningitidis? |
G- diplococci |
|
|
What can Neisseria meningitidis infection cause? Prevention? |

- Meningococcemia (picture) |
|

Which bacteria causes an infection that leads to the "thumbprint sign" on lateral neck radiograph? |

Haemophilus influenzae epiglottitis |
|
|
Characteristics of Haemophilus influenzae? |
Small G- coccobacillary rod |
|
|
Which type of Haemophilus influenzae causes the most invasive disease? What do the other types cause? |
- Most invasive disease caused by capsular type B |
|
|
What kind of infection is caused by Haemophilus influenzae? |
HaEMOPhilus causes |
|
|
How do you culture Haemophilus influenzae? |
On Chocolate agar, requires: |
|
|
How do you treat Haemophilus influenzae infections? |
- Mucosal infections (eg, otitis media, conjunctivitis, bronchitis) with Amoxicillin +/- Clavulanate |
|
|
How do you prevent spread / infection of Haemophilus influenzae infections? |
- Prevention in close contacts exposed to AEROSOL TRANSMISSION: Rifampin |
|
|
Which bacteria causes severe pneumonia, fever, GI and CNS symptoms? |
Legionella pneumophila (Legionnaire's disease) |
|
|
Characteristics of Legionella pneumophila? |
G- rod |
|
|
How do you diagnose Legionella pneumophila? Other signs? |
* Presence of antigen in urine is used clinically |
|
|
How does Legionella pneumophila get spread? |
- Aerosol transmission from environmental water source habitat (eg, A/C systems, hot water tanks) |
|
|
What disease states can Legionella pneumophila infection cause? Treatment? |
- Legionnaires' Disease: severe pneumonia, fever, GI and CNS symptoms |
|
|
Which bacteria is associated with wound and burn infections? |
Pseudomonas aeruginosa |
|
|
Characteristics of Pseudomonas aeruginosa? |
G- Rod: |
|
|
What toxins does Pseudomonas aeruginosa produce? Effects? |
- Endotoxin → fever and shock |
|
|
What color is Pseudomonas aeruginosa? How? |
Blue/green pigment called Pyocyanin |
|
|
What kind of infections does Pseudomonas aeruginosa cause? |
PSEUDOmonas associated with wound and burn infections: |
|
|
Which bacteria causes hot tub folliculitis? |
Pseudomonas aeruginosa |
|
|
How does Pseudomonas aeruginosa affect immunocompromised patients? |
Ecthyma gangrenosum |
|
|
What bacteria is associated with chronic pneumonia in cystic fibrosis patients? |
Pseudomonas aeruginosa (associated with biofilms) |
|
|
What are the virulence factors of E. coli? |
- Fimbriae |
|
|
What kind of infections are enhanced by the E. coli virulence factor "fimbriae"? |
- Cystitis |
|
|
What kind of infections are enhanced by the E. coli virulence factor "K capsule"? |
- Pneumonia |
|
|
What kind of infections are enhanced by the E. coli virulence factor "LPS endotoxin"? |
Septic shock |
|
|
What are the strains of E. coli? |
- EIEC |
|
|
Which bacteria causes invasive dysentery (severe diarrhea with the presence of blood and mucus in the feces)? Mechanism? |
EIEC (Invasive) |
|
|
Which bacteria causes Travelers' Diarrhea (watery)? Mechanism? |
ETEC (Travelers') |
|
|
Which bacteria causes diarrhea usually in children? Mechanism? |
EPEC (Pediatrics) |
|
|
Which bacteria causes non-invasive dysentery (severe diarrhea with the presence of blood and mucus in the feces)? Mechanism? |
EHEC (O157:H7 is the most common serotype) |
|
|
What are the components of Hemolytic Uremic Syndrome? Cause? |
- Anemia |
|
|
What is the difference between EIEC and EHEC? |
- EIEC: invasive, the microbe invades intestinal mucosa, causing necrosis and inflammation leading to dysentery |
|
|
Besides the presentation and mechanism, how does EHEC differ from other forms of E. coli? |
Does not ferment sorbitol |
|
|
Which form of E. coli does not ferment sorbitol? |
EHEC |
|
|
Which bacteria is associated with the 4 A's (Aspiration pneumonia, Abscess in lungs and liver, Alcoholics, and di-A-betics)? |
Klebsiella |
|
|
Characteristics of Klebsiella? |
G- Rod |
|
|
What does Klebsiella cause? Who is affected? |
*Causes lobar pneumonia (via Aspiration) |
|
|
Which bacteria causes patients to have a lobar pneumonia that leads to red "currant jelly" sputum? |
Klebsiella |
|
|
What are the similarities of Salmonella and Shigella? |
G- rods |
|
|
How do Salmonella and Shigella differ in movement? |
Salmonella: |
|
|
How do Salmonella and Shigella differ in dissemination? |
Salmonella |
|
|
How do Salmonella and Shigella differ in reservoirs? |
Salmonella |
|
|
How do Salmonella and Shigella differ in production of hydrogen sulfide? |
Salmonella |
|
|
How do Salmonella and Shigella differ in their response to antibiotics? |
Salmonella |
|
|
How do Salmonella and Shigella differ in their immune system response? |
Salmonella |
|
|
Which disease is characterized by rose spots on the abdomen, fever, headache, and diarrhea and can remain in the gallbladder causing a carrier state? Cause? |
Typhoid Fever (caused by Salmonella typhi) - only found in humans |
|
|
What are the symptoms of Typhoid Fever (Salmonella typhi)? |
- Rose spots on abdomen |
|
|
Characteristics of Salmonella? |
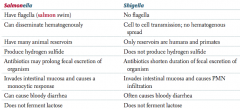
- Flagella (salmon swim) |
|
|
Characteristics of Shigella? |
- No flagella |
|
|
What bacteria is a major cause of bloody diarrhea (especially in children), and is spread through foods such as poultry, meat, and unpasteurized milk? |
Campylobacter jejuni |
|
|
Characteristics of Campylobacter jejuni? |
G- Comma or S-shaped |
|
|
How is Campylobacter jejuni acquired? |
Fecal-oral transmission through foods such as: |
|
|
What does Campylobacter jejuni cause? |
- Major cause of bloody diarrhea (especially in children) |
|
|
Which bacteria produces profuse "rice-water diarrhea"? Mechanism? Treatment? |
Vibrio cholerae |
|
|
Characteristics of Vibrio cholerae? |
G- comma shaped |
|
|
Where is Vibrio cholerae more common? Treatment? |
- Endemic to developing countries |
|
|
Which bacteria causes mesenteric adenitis that can mimic Crohn disease or appendicitis? Transmission? |
Yersinia enterocolitica |
|
|
What disease does Yersinia enterocolitica cause? Transmission? |
- Mesenteric adenitis that can mimic Crohn disease or appendicitis |
|
|
Which bacteria causes gastritis and peptic ulcers (especially duodenal)? |
Helicobacter pylori |
|
|
Characteristics of Helicobacter pylori? |
G- comma shaped rods |
|
|
What does Helicobacter pylori cause? |
- Causes Gastritis and Peptic Ulcers (especially duodenal) |
|
|
How do you treat Helicobacter pylori infection? |
Triple therapy: |
|

What is the name for spiral-shaped bacteria? Types? Visualization? |
Spirochetes: BLT - |
|
|
Which type of bacteria can be visualized with dark-field microscopy? |
Treponema (type of spirochete) |
|
|
Which type of bacteria is found in water contaminated with animal urine? |
Leptospira interrogans |
|
|
What diseases are caused by Leptospira interrogans infection? |
Leptospirosis |
|
|
What is the cause and symptoms of Leptospirosis? |
Leptospira interrogans |
|
|
What is the cause and symptoms of Weil Disease? |
Caused by Leptospira interrogans |
|
|
Who is more likely to get infected with Leptospira interrogans (which causes leptospirosis and Weil disease)? |
Prevalent among surfers and in tropics (eg, Hawaii) |
|
|
What causes Lyme Disease? |
* Borrelia burgdorferi, which is transmitted by the tick Ixodes (also vector for Babesia) |
|
|
Where is Lyme disease more common? |
NE United States |
|
|
What are the initial symptoms of Lyme Disease (Borrela burgdorferi)? |

- Erythema chronicum migrans - expanding bulls eye red rash (picture) |
|
|
What are the later symptoms of Lyme Disease (Borrela burgdorferi)? |
- Monoarthritis (large joints) |
|
|
What mnemonic can you use to remember the symptoms of Lyme Disease? |
FAKE a Key LYME pie: |
|
|
How do you treat Lyme Disease (Borrelia burgdorferi)? |
Doxycycline and Ceftriaxone |
|
|
What bacteria causes Syphilis? |
Treponema pallidum (spirochete) |
|
|
What are the stages of Syphilis? |
- 1° Syphilis |
|
|
What are the signs of 1° Syphilis? |

Localized disease, presents with PAINLESS chancre |
|
|
What are the microscopic and lab findings of 1° Syphilis? |
- Dark-field microscopy can visualize treponemes in fluid from chancre |
|
|
What are the signs of 2° Syphilis? |
- Disseminated disease / Systemic |
|
|
What are the microscopic and lab findings of 2° Syphilis? |
- Dark-field microscopy can visualize treponemes |
|
|
Following the systemic (2° stage) of syphilis, what happens? |
Latent syphilis stage |
|
|
What are the signs of 3° Syphilis? |
- Gummas (chronic granulomas) |
|
|
What are the lab findings of 3° Syphilis? |
For neurosyphilis: test spinal fluid with VDRL or RPR |
|
|
What are the signs of congenital syphilis? |
- Saber shins |
|
|
How do you prevent syphilis and congenital syphilis? |
*Treat with Penicillin G |
|
|
What is the "Prostitute Pupil"? AKA? Sign of? |
Argyll Robertson Pupil |
|
|
What is the VDRL test used for? Utility? |
Detects non-specific antibody that reacts with beef cardiolipin; widely used for syphilis (quantitative, sensitive, but not specific) |
|
|
What is the term for flu-like syndrome that begins after antibiotics are started? Why? |
Jarish-Herxheimer Reaction |
|
|
What is the Jarish-Herxheimer Reaction? |
- Causes flu-like syndrome that begins after antibiotics are started |
|
|
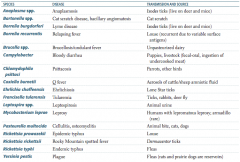
What is the term for infectious disease transmitted between animals and humans? |
Zoonosis |
|
|
Which zoonotic species is transmitted by Ixodes ticks? Source? Disease? |
Anaplasma species |
|
|
Which zoonotic species is transmitted by a cat scratch? Disease? |
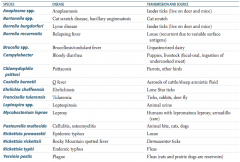
Bartonella species |
|
|
Which zoonotic species is transmitted by louse? Disease? |
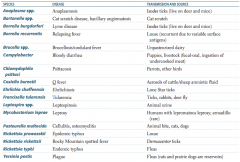
Borrelia recurrentis |
|
|
Which zoonotic species is transmitted by unpasteurized dairy? Disease? |
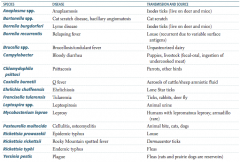
Brucella specia |
|
|
Which zoonotic species is transmitted by puppies and livestock? Source? Disease? |
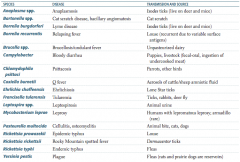
Campylobacter |
|
|
Which zoonotic species is transmitted by parrots and other birds? Disease? |

Chlamydophila psittaci |
|
|
Which zoonotic species is transmitted by aerosols of cattle / sheep amniotic fluid? Disease? |
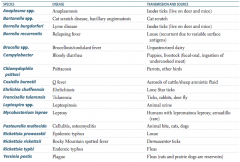
Coxiella burnetii |
|
|
Which zoonotic species is transmitted by lone star ticks? Disease? |
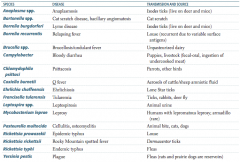
Ehrlichia chaffeensis |
|
|
Which zoonotic species is transmitted by rabbits? Disease? |
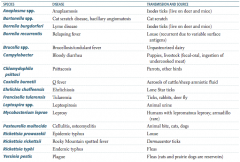
Francisella tularensis (also via ticks and deer fly) |
|
|
Which zoonotic species is transmitted by animal urine? Disease? |
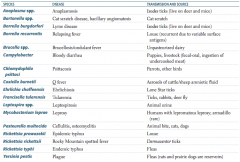
Leptospira species |
|
|
Which zoonotic species is transmitted by armadillos? Disease? |
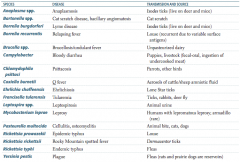
Mycobacterium leprae |
|
|
Which zoonotic species is transmitted by animal bites (cats, dogs)? Disease? |
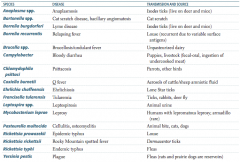
Pasteurella multocida |
|
|
Which zoonotic species is transmitted by Dermacentor ticks? Disease? |
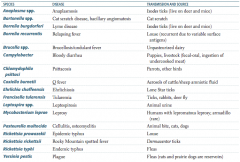
Rickettsia rickettsii |
|
|
Which zoonotic species is transmitted by fleas? Disease? |
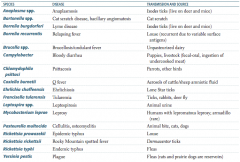
Rickettsia typhi |
|
|
Which zoonotic species has a reservoir in rats and prairie dogs? Disease? |
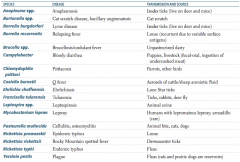
Yersinia pestis |
|
|
Which bacteria presents as a gray vaginal discharge with a fishy smell? |
Gardnerella vaginalis |
|
|
Characteristics of Gardnerella vaginalis? |
- Pleomorphic |
|
|
What causes Gardnerella vaginalis? |
* Not sexually transmitted |
|
|
How is Gardnerella vaginalis treated? |
Metronidazole or (to treat anaerobic bacteria) Clindamycin |
|
|
What are the vector-born illnesses? Vector? |
- Rocky Mountain Spotted Fever - tick is vector and carries Rickettsia rickettsii |
|
|
How do you treat all Rickettsial diseases and vector-borne illnesses? |
Doxycycline |
|
|
In which Rickettsial diseases and vector-borne illnesses is a rash common? |
Rash common: |
|
|
In which Rickettsial diseases and vector-borne illnesses is a rash rare? |
Rash rare: |
|

Which bacteria causes a rash that typically starts at wrists and ankles and then spreads to trunk, palms, and soles? Where is it more common? |
Rickettsia rickettsii (Rocky Mountain Spotted Fever) |
|
|
Characteristics of Rickettsia rickettsii? |
Obligate intracellular organisms |
|
|
What is the classic presentation of Rocky Mountain Spotted Fever? |
Triad: headache, fever, rash (vasculitis) |
|
|
In which infections is there a "palms and soles" rash? |
CARS = you drive CARS using your palms and soles |
|
|
What are the different causes of Typhus? How do they differ? |
Rickettsia typhi |
|
|
What are the symptoms of Typhus? |
Rash starts centrally (trunk) and spreads out, SPARING the palms and soles |
|
|
What are the characteristics of Ehrlichiosis? |
- Caused by Ehrlichia - vector is tick |
|
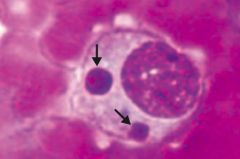
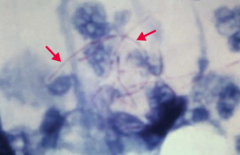
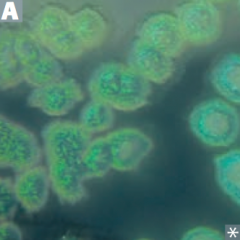
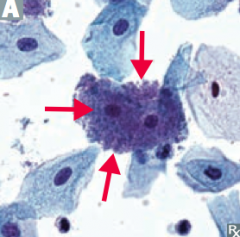
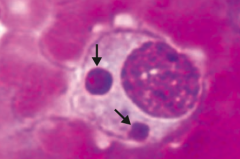
Which disease is pictured: monocytes with morulae (berry-like inclusions) in cytoplasm? |
Ehrlichiosis - caused by Ehrlichia (vector is a tick) |
|
|
What are the characteristics of Anaplasmosis? |
- Caused by Anaplasma, vector is tick |
|
|
Which disease is characterized by granulocytes with morulae in cytoplasm? |
Anaplasmosis - caused by Anaplasma (vector is tick) |
|
|
What are the characteristics of Q fever? |
- Caused by Coxiella burnetti (can survive outside in its endospore form) |
|
|
Which bacteria has Elementary bodies and Reticulate bodies? |
Chlamydiae |
|
|
What are the requirements of Chlamydiae? |
Obligate intracellular organisms - cannot make their own ATP |
|
|
What kind of infections does Chlamydiae cause? |

Mucosal infections |
|
|
What are the two forms of Chlamydiae? |
- Elementary Body (small dense) is "Enfectious" and "Enters" cells via "Endocytosis" where it transforms into a Reticulate Body |
|

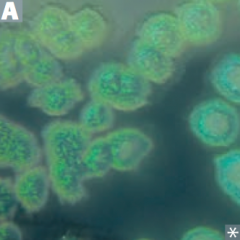
Which bacteria causes reactive arthritis (Reiter syndrome), follicular conjunctivitis (picture), non-gonococcal urethritis, and PID? |
Chlamydiae trachomatis |
|
|
Which bacteria causes atypical pneumonia and is transmitted by an aerosol? |
Chlamydiae pneumoniae and Chlamydiae psittaci (notable for an avian reservoir) |
|
|
How do you treat Chlamydiae infections? |
Azithromycin (favored because one time treatment) or Doxycycline |
|
|
How do you diagnose Chlamydiae infection? |
Lab: cytoplasmic inclusions seen on Giemsa stain or fluorescent antibody-stained smear |
|
|
What are the Chlamydiae trachomatis serotypes? |
- Types A, B, and C |
|
|
Which serotypes of Chlamydiae trachomatis cause chronic infection and can cause blindness due to follicular conjunctivitis? Other characteristics? |
Types A, B, and C |
|
|
Which serotypes of Chlamydiae trachomatis cause urethritis / PID, ectopic pregnancy, neonatal pneumonia (staccato cough), and neonatal conjunctivitis? |
Types D-K (everything else) |
|
|
Which serotypes of Chlamydiae trachomatis cause Lymphogranuloma Venereum? Symptoms? |
Types L1, L2, and L3 |
|
|
Which bacteria is the classic cause of atypical "walking pneumonia"? |
Mycoplasma pneumoniae (more common in patients < 30 years old; common outbreaks in military recruits and prisons) |
|
|
What are the symptoms of "walking pneumonia"? When is this more common? Cause? |
- Insidious onset |
|
|
What are the lab results for a patient with "walking pneumonia" caused by Mycoplasma pneumoniae? |
- X-ray looks worse than patient (patchy or diffuse interstitial infiltrate) |
|
|
How do you treat "walking pneumonia" caused by Mycoplasma pneumoniae? |
Macrolide, Doxycycline, or Fluoroquinolone |
|
|
Why will penicillin be ineffective in a case of walking pneumonia? |
Typical cause is Mycoplasma pneumoniae (which has no cell wall so penicillin will be ineffective) |
|
|
Characteristics of Mycoplasma pneumoniae? |
- No cell wall |

