![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
50 Cards in this Set
- Front
- Back
|
Enterobacteriaceae
|
- Gram (-) rods
- Glucose-fermenting - Oxidase (-) - Catalase (+) - Motile or non-motile - Non-sporeformers - Nitrate-reducing (nitrate → nitrite) - Heat stable lipopolysaccharide (LPS) (doesn't denature by heat) |
|
|
Indole test
|
The amino acid tryptophan can be broken down by enzyme tryptophanase to form indole, pyruvic acid and ammonia as end products. Tryptophanase differentiates indole-positive enterics, such as E. coli and P.vulgaris from indole-negative enterics, such as S. marcescens.
*Media and Reagents:* SIM with tryptophan and Kovac's reagent. *Expected Results:* Positive test : Kovac's reagent combines with indole and turns the surface red. Negative test: No red color or copper color development |
|
|
Voges-Proskauer Test (IMViC)
|

It is used to identify enteric bacteria based on their pattern of glucose metabolism. The enterics that produce neutral end-products, such as acetoin are detected by VP test.
*Media and Reagent:* MR-VP medium and Barritt's Reagent A (contains alpha-naphthol) and Barritt's Reagent B (contains KOH). *Expected results:* Positive test: acetoin + alpha-naphthol + KOH = red color Negative test: alpha-naphthol +KOH = copper color |
|
|
Citrate Utilization (IMViC)
|
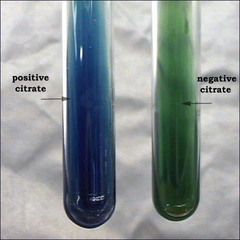
Citrate is an organic molecule that can be utilized by bacteria that produce the enzyme citrase. Citrase is produced by some bacteria such as E. aerogenes but not by others like E. Coli
*Media and Reagent:* Simmon's Citrate Agar. It has citrase as the only carbon source and PH indicator bromothymol blue *Expected results:* Positive test: Growth and color changes to blue Negative test: No growth and color remains green |
|
|
oxidase test
|
This test is used to identify microorganisms containing the enzyme cytochrome oxidase (important in the electron transport chain).
It is commonly used to distinguish between oxidase negative Enterobacteriaceae and oxidase positive Pseudomadaceae. Cytochrome oxidase transfers electrons from the electron transport chain to oxygen (the final electron acceptor) and reduces it to water. In the oxidase test, artificial electron donors and acceptors are provided. When the electron donor is oxidized by cytochrome oxidase it turns a dark purple. *Expected Results:* This is considered a positive result. In the picture above the organism on the right (Pseudomonas aeruginosa) is oxidase positive. |
|
|
Mac Results
|
o gram-negative Enterobacteria Escherichia coli and Enterobacter aerogenes ferment lactose
o E. coli produces pink to red colonies often with a reddish bile precipitate surrounding colonies on MacConkey's agar o E. aerogenes produces pink to red mucoid colonies on MacConkey's agar o gram-negative bacteria Proteus vulgaris and Salmonella typhimurium grow on MacConkey's agar, but do not ferment lactose (media appears yellow to light pink in color & colonies are colorless; swarming of Proteus is inhibited |
|
|
Hydrogen Sulfide Test (H2S) (IMViC)
|
(left is negative for H2S and right is positive for H2s)
Bacteria use enzyme cysteine desulfurase to hydrolyze the amino acid cysteine, forming hydrogen sulfide as end-product. *Media and Reagent:* SIM with cysteine and ferrous sulfate (detects H2S) *Expected Results: * Positive Test: H2S production = Black Negative Test: No H2S production = No blackening of medium |
|
|
Motility
|
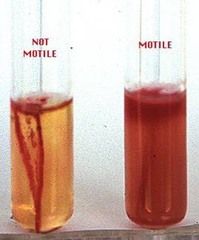
This is not a biochemical test, but it can distinguish bacteria. It determines presence of flagella.
*Media and reagent:* Deep agar *Expected results:* Positive test: Growth spread away from the line of inoculation = motile Negative test: Growth only occurred at the line of inoculation = Non-motile |
|
|
Escherichia coli
|
+ + - -
Gram negative BA Growth Beta Mac LF XLD LF HE LF Motility pos Citrate neg urea neg **selective Colorless (NEG) Mac Sorbitol for EHEC. Serotyping O, H Shiga toxin for EHEC MacConkey- reddish growth |
|
|
Enterobacteriaceae Overt Pathogens
|
Typhoid fever = Salmonella
- Dysentery = Shigella - Bubonic plague = Yersinia pestis |
|
|
Pseudomonas aeruginosa
|
Gram Stain Negative - small, clustered bacillus
aerobic oxidase POS BA growth MacConkey Plate- NFL, Yellow growth XLD NFL HE NFL Motility Pos Citraite Pos Urea Variable SPREADING metallic sheen pigment Odor is fruity grape smell Growth at 42 degree celcius |
|
|
Proteus vulgaris
|
+ +- -
Motility- pos Citrate neg Urea pos oxidase neg BA growth Mac NLF XLD NLF H2S HE NLF H2s Gram- negative ** H2S producer, ecoli is not** Temp- incubator showed small growth, should grow around 23 degrees |
|
|
Enterobacter cloacae
|
- - + +
Gram negative oxidase neg BA=Growth mac =LF He =LF Motility neg citrate pos Urea neg Bact. O2- obligate aerobe |
|
|
Acinetobacter baumannii
|
- - Gram (-) cocobacilli
- Non-fermenting - Saccharolytic (glucose oxidizer), non-hemolytic** - Most frequent Acinetobacter isolate** - Responsible for most nosocomial infections - Respiratory infections, pneumonia - Increasing resistance |
|
|
Enterobacteriaceae Opportunistic pathogens
|
Urinary tract infection = E. coli, Enterobacter, Proteus,
- Diarrhea, dysentery = Shigella, EIEC - Nosocomial infections = E. coli, Enterobacter, Proteus, Serratia |
|
|
Escherichia coli
|
+ + - -
Gram (-) rods - Glucose fermenter - Oxidase (-) - Indole (+) ** - MR (+) - VP (-) - Citrate (-) - β- hemolysis ** - Motile, pos |
|
|
Escherichia coli Clinical Disease
|
Normal bowel flora (~10% of intestinal flora)
- Most common Gram (-) rod in sepsis - Cause of 80% of community-acquired UTI - Gastroenteritis in developing countries (poor hygiene) - Most infections are endogenous (deep tissue) - Urinary tract infection (most strains can cause this) - Specific uropathogenic strains, adhesins - Septicemia - Neonatal meningitis: |
|
|
Enterohemorrhagic (EHEC)
|
Virulence factor: toxin similar to Shiga toxin which disrupt protein synthesis and A/E lesions that destroy intestinal microvillus leading to decreased absorption
- Disease: Initial watery diarrhea followed by grossly bloody diarrhea (hemorrhagic colitis) with abdominal cramps; little or no fever; may progress to hemolytic uremic syndrome (HUS) (kidneys get knocked out) - Large intestine - Jack-In-the-Box: uncooked hamburgers - Serotype 0157:H7= NEg Mac Sorbitol, OH ag, shiga toxin |
|
|
Salmonella
|
Widely disseminated in nature and associated with various animals
- Animal-to-animal, animal-to-human - Animal pathogens, human pathogens, animal-human pathogens - Contaminated food, fecal-oral spread - S. typhi is only found in humans at times of infection |
|
|
Salmonella Gastroenteritis
|
Diarrhea caused by a wide variety of serotypes that produce infections limited to the mucosa and submucosa of the GI tract
- 6-48 hrs post ingestion, 2-7days duration - Nausea, vomiting, non-bloody diarrhea**, fever, cramps, myalgia, headache Characterized by prolonged fever and multisystem involvement, including lymph nodes, liver and spleen. - Typhoid fever: S. typhi - Paratyphoid fever: other salmonellae - Transported to liver, spleen, bone marrow - 10-14 days post-ingestion: rising fever, myalias, headache, malaise, anorexia → gastrointestinal symptoms |
|
|
Salmonella
|
- + - v
Oxidase neg Growth on BA NLF on Mac NLF h2s on XLD NLF h2s on HE Motility Pos Citrate Pos Urea NEg Selective agar SS Tetrath Selenite Serotyping OKH ag (ABC1,C2, D,E, Vi) |
|
|
Shigella Epidemiology
|
Humans and other large primates are only reservoirs
- Found in humans only at time of infection - Not part of normal bowel flora - Person-to-person spread by fecal-oral route by ingestion of contaminated food, water - Pediatric disease, low personal hygiene |
|
|
Shigella Clinical Diseases
|
Shigellosis, bacillary dysentary (acute inflammatory colitis)
- 1-3 days post ingestion - Watery diarrhea in S. sonneir (due to Shiga toxin) - Lower abdominal cramps, tenesmus, pus & blood in stool - Self-limiting but treat to prevent spread - Carrier state possible |
|
|
Yersinia General characteristics
|
Smaller, slower-growing rods
- Motile at room temp, non-motile at 37°C ** - Bipolar staining in direct Giemsa stains |
|
|
Yersinia pestis Epidemiology
|
Carried by urban/domestic rats and wild rodents such as squirrel and prairie dog
- Is the only Enterobacteriacea spp that is transmitted from animals by the bite of an insect vector (flea) |
|
|
Yersinia enterocolitica Epidemiology
|
Carried by dogs, cats, rodents, rabbits, pig, sheep
- Not part of normal flora - Only inhabit the bowel at the time they are causing infection due to contaminated meat, milk, water - Enterocolitis in cooler regions - Not common |
|
|
Bubonic plague
|
Yersinia pestis
- Flea - Characterized by high fever and painful inflammatory swelling of axilla and groin lymph nodes - Infection rapidly progresses to fulminant bacteremia and lead to pneumonia that is often fatal if untreated |
|
|
Pneumonic plague
|
Yersinia pestis
- Involves the lungs - Characterized by malaise and pulmonary signs - The respiratory infection can occur as consequence of bacteremic spread assoc with bubonic plague - Can also be acquired by the airborne route during close contact with infected victims (Aerosols) - Rapidly fatal |
|
|
Proteus mirabilis
|
Normal human GI tract flora
- 2nd most common cause of UTI - Swarmer (waves) |
|
|
Enterobacter, Citrobacter, Morganella, Serratia
|
Normal human GI tract flora
- immunocompromised or nosocomial infections |
|
|
Klebsiella Pneumoniae
|
Normal human GI tract flora
- Nonmotile rod-shaped gram (-) enterobacteria - Prominent capsule - K. pneumoniae, |
|
|
Enterobacteriaceae Culture Media
|
Most grow well on SBA, BA, and MAC
- Non-fastidious - Selective/differential media - XLD, HE, SS (Salmonella-Shigella agar), CIN agars |
|
|
Enterobacter Media & Colony Appearance
|
MAC: Lactose fermenter; may be mucoid
- HE: yellow - XLD: yellow |
|
|
E. Coli Media & Colony Appearance
|
MAC: Lac fermenter; flat, pink colonies with surrounding darker pink area of precipitated bile salts
- HE: Yellow - XLD: Yellow |
|
|
Proteus Media & Colony Appearance
|
MAC: Non lac fermenter; swarming; foul smell
- HE: Colorless - XLD: Yellow or colorless, with black centers |
|
|
Salmonella Media & Colony Appearance
|
MAC: Non lac fermenter
- HE: Green - XLD: Red with black center (due to H2S production) |
|
|
Shigella Media & Colony Appearance
|
MAC: Non lac fermenter
- HE: blue-Green - XLD: Colorless |
|
|
E.coli
|
-a coliform i.e. ferments lactose
-gram -ve rod -cat +ve, oxi -ve -facultative anaerobes -IMViC ++-- -motile -Urease and H2S -ve -Lysine decarboxylase +ve |
|
|
Salmonella
|
-a non-coliform i.e. does not ferment lactose
-gram -ve rod -cat +ve, oxi -ve -facultative anaerobes -IMViC -+-+ -motile -Urease -ve -H2S and lysine decarboxylase +ve -need sal-specifc agar and sal-selective broth - would be over-grown by other bact on normal plate -black centered colonies on XLD agar |
|
|
Klebsiella IMViC
|
--++
|
|
|
What is the theory of the TSI test?
|
Term
What is the theory of the TSI test? Definition TSI is a differential medium for Gram-negative enteric organisms. It differentiates organisms based on their ability to ferment the lactose and or sucrose present in the media. (Note: all Gram-negative enteric organisms will ferment the glucose.) The TSI media contains disaccharides lactose and sucrose in concentrations of 1% and glucose at a concentration of 0.1%. The lower concentration of glucose allows for the detection of utilization of this substrate alone. Since glucose is a monosaccharide, it will be used first. The small amount of acid produced in the slant of the tube during glucose fermentation is oxidized rapidly, causing the medium to remain red or revert to an alkaline pH. In contrast, the acid reaction (yellow) is maintained in the butt of the tube because it is under lower oxygen tension. After the depletion of the limited glucose, organisms able to do so will begin to utilize the lactose and or sucrose resulting in an acid slant and butt. H2S production (indicated by the blackening in the butt of the tube) is detected by the sodium thiosulfate in the media, which is reduced by some organisms to hydrogen sulfide, which then reacts with ferrous sulfate in the media yielding the typical black iron sulfide. Cracked or elevated media is the result of production of CO2 from the fermentation of sugars. |
|
|
Salmonella IMViC
|
-+-+
|
|
|
How is media inoculated for the TSI test?
|
stab the butt of the tube and streak the surface of the slant
|
|
|
How long do you incubate the TSI test?
|
18-24 hours. Incubate no longer than 24 hours because of the acid reaction in the slant may revert to an alkaline reaction. This is called reversion.
|
|
|
How do you interpret the results of the TSI test?
|
Red slant/yellow butt (K/A) = glucose fermentation only
Yellow Slant/yellow butt (A/A) = glucose, lactose and/or sucrose fermentation Red slant/red butt (K/NC) = no carbohydrate fermentation hydrogen sulfide production results in a black precipitate in the butt. CO2 production is indicated by cracking or elevation of the media. NOTE: some hydrogen sulfide producing organisms may produce so much of the black precipitate, ferrous sulfide, that the acidity produced in the butt is completely masked. However, H2S is reduces, an acid condition does exist in the butt even if not observable and should be recoded as such. |
|
|
Explain the purpose of the phenol red in the medium for the TSI test.
|
To detect the fermentation of carbohydrates by change of the medium from an orange-red to a yellow color.
|
|
|
3.
Acinetobacter Colony & Appearance |
- BA: Smooth, opaque, raised, creamy, smaller than Enterobacteriacea spp
- MAC: Non lac fermenter, but colonies exhibit purplish/pink hue that may be mistaken for a lac fermenter |
|
|
Acinetobacter Pathogenesis
|
- Clinical isolates are often colonizers
- True infections are usually nosocomial - Occur during warm seasons - Most commonly involve GI tract, respiratory tract, wounds, soft tissue, and bacteremia - Community-acquired infection: pneumonia & wound infection - Outbreak among soldiers in Iraq: had A. baumannii. |
|
|
Acinetobacter Epidemiology
|
Widely distributed in natural and hospital environments
- Dry surfaces, food, human skin - May become apart of respiratory flora of pts hospitalized for prolonged periods (ICU, surgery) - As many as 25% of healthy adults harbor these bacteria on skin, gastrointestinal tract - Medical instrumentation introduces organism to normally sterile sites |
|
|
Stenotrophomonas General Characteristics
|
Gram (-) rods
- Oxidase (-) - Oxidation neg - Dnase (+) - - MAC (+) |

