![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
51 Cards in this Set
- Front
- Back
|
what does MIC stand for
|
minimum inhibitory concentration
this is the lowest concentration of a drug that prevents growth |
|
|
what does MLC stand for
|
minimum leathal concentration of a drug that kills
|
|
|
what is a chemotherapeutic agent
|
any chemical that is used to treat a desease
|
|
|
what is an antimicrobial drug
|
any chemical used to treat a microbial infection
|
|
|
antibiotics
|
antimicrobial drugs naturally produced by microorganisms
|
|
|
what is selective toxicity
|
antimicrobial drugs must be selectively toxic againt microorganisms and not permanently harm the human host
|
|
|
what is the therapeutic dose
|
the level required for treatment
|
|
|
what is the toxic dose
|
the level at which the drug is toxic to the host
|
|
|
what is the therapeutic index
|
toxic dose/therapeutic dose
the larger this is, the better (more selective) the antimicrobial drug |
|
|
what is the mechanisms of action of beta-lactam drugs
|
inhibit cell wall synthesis
|
|
|
what are two beta lactam drugs
|
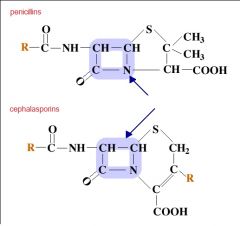
penicillins and cephalasporins
|
|
|
what is the specific mechanism of action in beta-lactam drugs
|
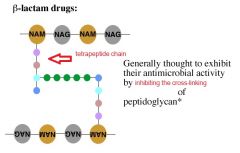
inhibiting the cross-linking of petidoglycan via the tetrapeptide chain
|
|
|
Beta-lactam drugs are only effective in these type of cells
|
cells that are actively synthesizing their cell walls. When the cell is actively growing
best time to treat is during initial log |
|
|
gram negative bacteria are more likely to produce this enzyme that can inactivate antibiotics
|
beta-lactamases (penicillinases)
|
|
|
other than this, beta-lactam antibiotics tend to have very few side effects
|
allergic reactions
|
|
|
because the peptidoglycan layer of gram negative bacteria is protected by this they tend to be more innately resistant to this type of antibiotic
|
protected by outer membrane
beta-lactam antibiotics |
|
|
what is the
Source effective against Examples for natural penicillins (beta-lactame antibiotics) |
peniciilium, chrysogenum
G+ bacteria and some G- Cocci Penicillin G, Penicillin V |
|
|
what is the
Source effective against Examples for Broad-spectrum penicillins |
Partially synthetic
G+ and G- bacteria ampicillin and amoxicillin |
|
|
what is the
Source effective against Examples for extended-spectrum penicillins |
partially synthetic
some tough G- bacteria (Pseudomonas) Ticarcillin and Piperacillin |
|
|
what is the
Source effective against Examples for cephalosporins |
Acremonium, Cephalosporium (more recent derivaties are partially synthetic)
some G+ and more recent derivatives are effective against G- Cephalexin and Cefepime |
|
|
because vacomycin cannot do this it is not a possible treatment for gram negative bacteria
|
cannot cross the outer membrane
|
|
|
this is good for treating G+ infections if the beta lactam antibiotics are ineffective
|
Vancomycin
example = antibiotic resistant Staphylococcus aureus |
|
|
how is vancomycin administered
|
intravenously (parenterally)
|
|
|
what is the mechanism of action of Vancomycin
|

binds to the peptide side chain of NAM and stops synthesis of peptidoglycan
|
|
|
what is the mechanism of action of Bacitracin
|
Inhibits cell wall synthesis by interfering with the transport of peptidoglycan precursors across the cytoplasmic membrane
|
|
|
when is bacitracin used
|
only in topical ointments
|
|
|
what is the
mechanism of action effective against and example for Aminoglycosides |
bind to 30S ribosomal subunit causing it to mis-translate proteins
mainly G- that respire (proteus, escherichia, Klebsiella) streptomycin, gentamicin, neomycin (do not take orally, non selective) |
|
|
can you take the aminoglycoside antibiotic neomycin orally
|
no, it is non-selective
|
|
|
do the aminoglycosides have a high or low therapudic index
|
low
|
|
|
what is the
mechanism of action effective against and example for tetracyclines |
reversibly bind to the 30s ribosomal subunit and stop protein synthesis
certain G+ and and G- (rickettsia and chlamydiae) tetracycline and doxycycline |
|
|
what is the
mechanism of action effective against and example for macrolides |
reversibly bind to the 50S ribosomal subunit and stop protein synthesis
a variety of bacteria, mainly G+, but also those that cause walking pneunomia erythromycin azithromycin |
|
|
what is the Mechanism of action for Aminoglycosides
|
bind to 30S ribosomal subunit causing it to mis-translate proteins
|
|
|
what is the Mechanism of action for tetracyclines
|
reversibly bind to the 30s ribosomal subunit and stop protein synthesis
|
|
|
what is the Mechanism of action for macrolides
|
reversibly bind to the 50S ribosomal subunit and stop protein synthesis
|
|
|
what are aminoglycosides effective against
|
mainly G- that respire (proteus, Escherichia, and Klebsiella)
|
|
|
what are the tetracyclines effective against
|
Certain G+ and G- (rickettsias and chlamydiae)
|
|
|
what is macrolides effective against
|
variety of bacteria, mostly G+, but also those that cause walking pneumonia
|
|
|
what is an example of an aminoglycoside
|
stretomycin
Gentamicin Neomycin (DO NOT TAKE ORALLY) |
|
|
what is an example of an tetracycline
|
tetracycline and doxycycline
|
|
|
what is an example of an tetracycline
|
erythromycin and Azithromycin
|
|
|
what type of antibiotic are the aminoglycosides, tetracyclines and macrolides
|
they all inhibit protein synthesis
|
|
|
what class of antibiotics inhibit protein synthesis
|
aminoglycosides, tetracyclines and macrolides
|
|
|
the plasma in micoplasma means
|
that the bacteria has no cell wall
|
|
|
what does arbo mean?
|
arthropod born bacteria
|
|
|
what class of antibiotics inhibit nucleic acid synthesis
|
quinolones
|
|
|
what is the mechanism of action of the quinolones
|
inhibit DNA topoisomerases and gyrases
|
|
|
what are the quinolones effective against
|
wide variety of G+ and G-
|
|
|
what is an example of a quinolone
|
Ciprofloxacin (cipro)
|
|
|
what is an example of an antibotic that interferes with cell membrane integrity
|
Polymyxin B
|
|
|
where should polymyxin B be used
|
only topically because it can damage eukaryotic cells
active ingrediant in topical first aid creams |
|
|
what type of cells are easier to kill/inhibit with antibiotics
|
grame positive because of the exposed peptidoglycan layer.
|

