![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
122 Cards in this Set
- Front
- Back
|
Body Defenses – 1st Line of Defense (desc --3 R's)
|
Reconnaissance, Recognition, and Response
–Detect invader/foreign cells –Communicate alarm & recruit immune cells –Suppress or destroy invader |
|
|
Two major kinds of defense have evolved that counter pathogens
|
–Innate immunity
--acquired immunity |
|
|
Innate Immunity
|
--broad defenses against infections, toxins
--nonspecific responses to pathogens; Non-selective --no previous exposure required; effective from the time of birth --immediate response; no lag time |
|
|
Phagocytosis
|
- cells engulf and digest recognized "foreign" cells – molecules
|
|
|
Inflammatory response -
|
localized tissue response to injury producing swelling, redness, heat, pain
|
|
|
Complement system –
|
activated proteins that destroy pathogen plasma membranes
|
|
|
Natural Killer cells –
|
special kind of lymphocytes-- that destroy virus infected cells and cancer cells
|
|
|
Interferon -
|
proteins that non-specifically defend against VIRAL infection
|
|
|
study of disease
|
Pathology
|
|
|
Etiology:
|
study of the origins of disease; the microbe causing a disease
|
|
|
Pathogenesis:
|
development of disease
|
|
|
Infection:
|
Colonization of the body by pathogens
|
|
|
Disease:
|
Abnormal body function
|
|
|
Where do Normal Microbiota reside on the Human Body?
|
Upper respiratory sys
eyes(conjunctiva) mouth skin large intestine urinary and reproductive system |
|
|
Normal Microbiota consist of these 3 types:
|
•Normal flora (permanently colonize)
•Transient flora •Opportunistic pathogens |
|
|
3 types of Symbiosis
|
•Commensalism—one organism benefits—other is unaffected
•Mutualism—both organisms benefit •Parasitism—One organism benefits at the expense of the other |
|
|
Microbial antagonism -
|
competition between microbes
|
|
|
Normal microbiota protect the host by (3 things)...
|
--Occupy niches pathogens might occupy
--Produce acids --Produce bacteriocins |
|
|
Live Microbes applied to the body or ingested---beneficial effect
|
Probiotics:
|
|
|
Classifying Infectious Diseases (6 terms)
|
Symptom
Sign Syndrome Noncommunicable disease: Communicable disease: Contagious disease: |
|
|
specific group of signs and symptoms that accompany a disease
|
Syndrome
|
|
|
change that can be measured or observed
|
Sign:
|
|
|
change felt by patient
|
Symptom:
|
|
|
disease that is spread from one host to another
|
Communicable disease:
|
|
|
disease that is easily spread
|
Contagious disease:
|
|
|
Noncommunicable disease:
|
Not transmitted from one host to another
|
|
|
Term for Occurrence of a Disease where there is...
a Fraction of a population that contracts a disease during a specific time; new cases |
Incidence:
|
|
|
Term for Occurrence of a Disease where there is...
a Fraction of a population having a specific disease at a given time |
Prevalence:
|
|
|
Term for Occurrence of a Disease where a disease...
Occurs occasionally in a population |
Sporadic disease:
|
|
|
Term for Occurrence of a Disease where a disease...
is Constantly present; baseline or expected |
Endemic disease:
|
|
|
Term for Occurrence of a Disease where a disease...
is Acquired by many in a given area in a short time |
Epidemic disease:
|
|
|
Term for Occurrence of a Disease where a disease...
is a Worldwide epidemic |
Pandemic disease:
|
|
|
Severity or Duration of a Disease is termed,
Acute disease: if.... |
Symptoms develop rapidly
|
|
|
Severity or Duration of a Disease is termed,
Chronic disease: if.... |
Disease develops slowly
|
|
|
Severity or Duration of a Disease is termed,
Subacute disease: if.... |
Symptoms between acute and chronic
|
|
|
Severity or Duration of a Disease is termed,
Latent disease: if.... |
No symptoms when inactive; reactivates
|
|
|
Local vs.Systemic infection:
|
Local infection:small area of body affected
Systemic infection: throughout the body |
|
|
Toxic inflammatory condition from the spread of microbes, especially bacteria or their toxins
|
Sepsis:
|
|
|
the presence of bacteria in the blood.
|
Bacteremia:
The blood is normally a sterile environment, so the detection of bacteria in the blood is always abnormal. |
|
|
Bacteria growing in blood
|
Septicemia:
|
|
|
Toxic inflammatory condition from the spread of microbes, especially bacteria or their toxins
|
Sepsis:
|
|
|
term for Initial illness
|
Primary infection:
|
|
|
Opportunistic infection after primary (predisposing) infection
|
Secondary infection:
|
|
|
Term for infection with No noticeable signs or symptoms
|
Subclinical disease:
(inapparent infection) |
|
|
Predisposing Factors...
Make the body more susceptible to disease list 7 of them: |
--Short urethra (in females)
--Inherited traits (such as the sickle cell gene) --Climate and weather --Fatigue --Age --Lifestyle --Chemotherapy |
|
|
Reservoirs (Continual Sources) of disease are...
|
***Living
1. Human: ex: AIDS, gonorrhea (Carriers may have inapparent infections or latent diseases) 2. Animal: ex: Rabies, Lyme disease (Some zoonoses may be transmitted to humans) ***Nonliving/Environmental 3. Soil, Air, Water, Food: ex: Botulism, tetanus |
|
|
3 types of contact transmission:
|
--Direct: Close association between infected and susceptible host
--Indirect: Spread by fomites (inanimate objects) --Droplet: airborne droplets |
|
|
Disease transmitted by a nonliving (environmental) reservoir
|
Vehicle Transmission
|
|
|
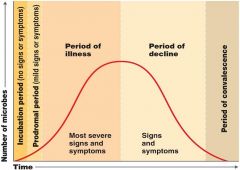
Stages of a Disease
|
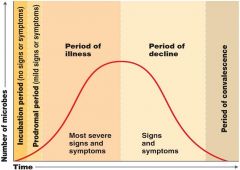
|
|
|
Define reservoir
|
A reservoir is simply the source of an infecting microorganism.
|
|
|
A zoonosis is...
|
a communicable disease which is transmitted from a non-human animal to a human.
note*Zoonotic reservoirs can be either unidirectional (e.g., transmitting only from non-humans to humans; ) or bi-directional (i.e., back and forth between non-human animals and humans). |
|
|
An endogenous infection is...
|
one which is caused by an opportunistic pathogen from an individual's own normal microbiota.
|
|
|
Transmission is...
|
the transfer of a disease-causing microorganism from one environment to another, particularly from an external environment to a susceptible individual.
|
|
|
There are three general categories of transmission:
|
contact
vehicle vector |
|
|
Fomites are...
|
basically almost anything an infected individual (or reservoir) can touch, upon which can be left a residue of contagious pathogen.
*note--Exceptions include the various inanimates referred to as vehicles: food air liquids |
|
|
Typically it is more difficult to avoid ________ contact transmission than it is to avoid _______ contact transmission.
|
indirect; direct
|
|
|
Droplet transmission is a form of contact transmission.
Basically it is the consequence of being: |
coughed on
sneezed on spit on *note--As a rule of thumb this is up to one meter post-mouth. Any further and this is considered airborne transmission. |
|
|
especially ______diseases that are transmitted by droplets.
|
respiratory
|
|
|
Vehicle transmission transmission is...
|
things routinely taken into the body.
|
|
|
Airborne transmission is a form of _____ transmission.
|
vehicle
*droplets are liquids that remain airborne whether as: aerosols (very small droplets) associated with dust particles |
|
|
Airborne transmission requires greater organismal durability than droplet transmission because...
|
of the length of time the microorganism is exposed to the air, before infecting a new host, is longer.
Increased durability is to the effects of dessication, exposure to sunlight, etc. |
|
|
Foodborne transmission is a form of______transmission
|
vehicle
*Generally pathogens that undergo foodborne transmission are either being transmitted from the: food preparer flora originally associated with the food product (ex: Salmonella spp. tends to be part of the normal flora of chickens) |
|
|
Waterborne transmission is a form of _____ transmission.
|
vehicle
*Generally, this is via sewage (i.e., fecal) contaminated water supplies. It is especially gastrointestinal pathogens that are present in feces and therefore which rely on waterborne transmission. |
|
|
an organism that does not cause disease itself but that transmits infection by conveying pathogens from one host to another
|
A vector
|
|
|
2 types of vector transmission:
|
1. Mechanical:
Carries pathogen ON bristles or feet 2. Biological: Pathogen reproduces in vector |
|
|
Nosocomial Infections
|
Acquired in hospital, clinic
Affect 5–15% of patients |
|
|
Nosocomial Infections
|
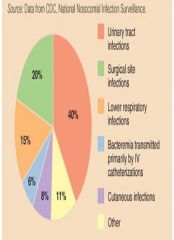
|
|
|
Which Procedure Most Increases the Likelihood of Infection?
|
|
|
|
Tapeworm, cat-scratch fever, toxoplasmosis, brucellosis, Q fever, typhus fever, and Western equine encephalitis are all examples of?
|
Zoonoses
|
|
|
Compare and contrast carrier with reservoir.
|
a reservoir is the source of an infecting microorganism while a carrier is a type of reservoir, particularly consisting of infected individuals of the same species. Note that a carrier need not be assymptomatic.
|
|
|
MRSA
|
Methicillin-resistant Staphylococcus aureus infection
|
|
|
New, increasing in incidence, or show potential increase in near future
|
Emerging Infectious Diseases
|
|
|
6 Contributing factors
of... Emerging Infectious Diseases |
1.Genetic recombination - E. coli O157, Avian influenza (H5N1)
2.Changes in weather patterns - Hantavirus 3. Modern transportation – West Nile Virus 4. Ecological disaster, war, expanding human settlement - Coccidioidomycosis 5. Animal control measures - Lyme disease 6. Public health failure - Diphtheria |
|
|
In US, what organization tracks... Where and when diseases occur and how they are transmitted
|
Centers for Disease Control and Prevention (CDC)
--Collect and analyze U. S. epidemiological information --Publish Morbidity and Mortality Weekly Report |
|
|
Pathogenicity:
|
ability to cause disease
|
|
|
Virulence:
|
extent or degree of pathogenicity
-- within a group or species of microorganisms or viruses as ---indicated by case fatality rates and/or the ability of the organism to invade the tissues of the host. --The pathogenic capacity of an organism is determined by its virulence factors. |
|
|
Measuring virulence:
What does "ID50" stand for? |
Infectious dose for 50% of test population
|
|
|
Measuring virulence:
What does "LD50" stand for? |
Lethal dose for 50% of test population (toxins)
|
|
|
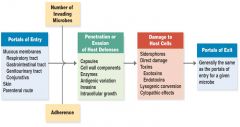
3 Portals of Entry
|
Mucous membranes
Skin Parenteral route |
|
|
5 Portals of Exit
|
1. Respiratory tract
ex-Coughing and sneezing 2. Gastrointestinal tract ex-Feces and saliva 3. Genitourinary tract ex-Urine and vaginal secretions 4. Skin 5. Blood ex-Biting arthropods and needles or syringes |
|
|
the route a pathogen takes to enter a host.
|
portal of entry
*Many pathogens are not able to cause disease if their usual portal of entry is artificially bypassed. |
|
|
Mucous membrane portals of entry
|
(Mucous membranes line or cover:)
the respiratory tract the gastrointestinal tract the genitourinary tract the eyes *The gastrointestinal and respiratory tracts are particularly common mucous membrane portals of entry. |
|
|
Microbes gain access to these mucous membranes by
|
during inspiration
upon ingestion touching the eyes touching the genitourinary tract |
|
|
Some pathogens are capable of entering through otherwise intact skin either via______ or by actually boring through
|
natural pores, exocrine glands, hair follicles
*Normally very impenetrable to most microorganisms, the skin can serve as an efficient portal of entry for many pathogens only when broken. |
|
|
A __________portal of entry is one of direct deposit of pathogens into body cavities or wounds.
|
parenteral
*a portal of entry through a break in skin is actually considered a parenteral portal of entry. |
|
|
A __________ is the route a pathogen takes out of an infected host.
|
portal of exit
*Portals of exit tend to be fairly well defined. |
|
|
A more ______ portal of exit occurs when an infected animal is butchered or an infected person undergoes surgery.
|
general
|
|
|
Blood-borne diseases tend to exit via:
|
arthropods
needles* bleeding *i.e., hyperdermic syringe. |
|
|
Almost every pathogen has a mechanism for attaching to host tissues at their _________.
|
portal of entry
|
|
|
Zoonotic reservoirs can be either __________ (e.g., transmitting only from non-humans to humans; ) or _________(i.e., back and forth between non-human animals and humans).
|
unidirectional; bi-directional
|
|
|
Adherence (of pathogen to host)
|
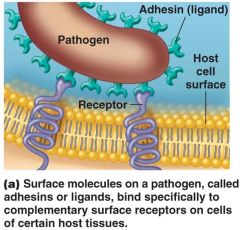
|
|
|
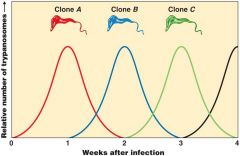
Invasiveness - Antigenic Variation
-Alter surface proteins |
|
|
|
Penetrating the Host Cytoskeleton
--Salmonella alters actin to enter host cell --Use actin to move from one cell to the next --Listeria |

|
|
|
What are Siderophores?
|
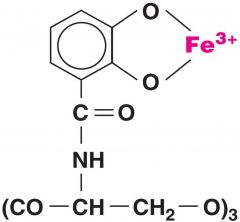
small, high-affinity iron chelating compounds secreted by microorganisms such as bacteria, fungi and grasses.
*Siderophores are amongst the strongest soluble Fe3+ binding agents known. |
|
|
Cell Damage - Endotoxins vs. Exotoxins
|

|
|
|
What are Endotoxins?
|
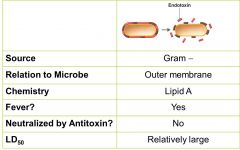
a toxin that is a structural molecule of the bacteria that is recognized by the immune system.
*examples of endotoxin are lipopolysaccharide (LPS) or lipooligosaccharide (LOS), found in the outer membrane of various Gram-negative bacteria and are an important component of their ability to cause disease.[ |
|
|
What are exotoxins? (G+)
|
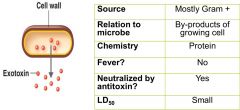
a toxin excreted or released during lysis of the cell by a microorganism,
including bacteria, fungi, algae, and protozoa. *Exotoxins are susceptible to antibodies produced by the immune system, but many exotoxins are so toxic that they may be fatal to the host before the immune system has a chance to mount defenses against it. |
|
|
A-B Exotoxin
|

group of intracellular toxins
The 'B'-subunit (binding) attaches to target regions on cell membranes, the 'A'-subunit (active) enters through the membrane and possesses enzymatic function that affects internal cellular bio-mechanisms. *The structure of these toxins allows for the development of specific vaccines and treatments. Certain compounds can be attached to the B unit, which is not, in general, harmful, which the body learns to recognize, and which elicits an immune response. |
|
|
Exotoxins & Lysogenic Conversion
|
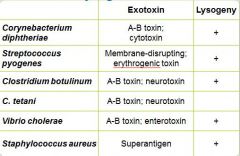
The process by which a virus induces change in the characteristics of a bacterial host.
**Lysogenic conversion is involved in scarlet fever, and in some botulinum and staphylococcal toxins responsible for food poisoning. * Different phages bring about different conversions |
|
|
Mechanisms of Pathogenicity
|
|
|
|
causes of specific diseases
|
Etiologies
|
|
|
Horizontal v Vertical transmission
|
Horizontal means transmission between individuals specifically who are not related as a parent is to its offspring
Vertical transmission occurs from parent to offspring |
|
|
Once entry has been accomplished, most microorganisms have mechanisms of host attachment,called________.
|
adherence
*For bacterial pathogens, successful adherence is usually a necessary prerequisite for virulence and even infection. *Such microbial structures as glycocalyx and fimbriae (i.e., attachment pili) are involved e. in adherence. |
|
|
5 structures of adherence
|
1. Adhesins/ligands bind to receptors on host cells
2. Glycocalyx: (Streptococcus mutans) 3.Fimbriae: (Escherichia coli) 4. M protein: (Streptococcus pyogenes) 5. Biofilms |
|
|
Capsules...
Prevent phagocytosis Name 3 bacteria w/capsules |
Streptococcus pneumoniae
Haemophilus influenzae Bacillus anthracis |
|
|
A cytotoxin is
|
an exotoxin that disrupts host cells.
|
|
|
An enterotoxin is
|
an exotoxin that disrupts the lining of the gastrointestinal tract
|
|
|
A neurotoxin is
|
an exotoxin that disrupts nerve cells.
|
|
|
Antitoxins are
|
antibodies that bind to exotoxins, thus inactivating the exotoxin.
|
|
|
A toxoid is a
|
physically or chemically inactivated exotoxin.
*Toxoids are employed as vaccines, such as against tetanospasmin, since they induce a host immune response (i.e., antitoxin) but have limited or nonexistent toxicity. |
|
|
The lipid A portion of lipopolysaccharide (LPS) is also known as ________.
|
endotoxin
|
|
|
Qualitatively, all endotoxins produce the same symptoms.
Why? |
This is because the symptoms are a consequence of the body reacting to the presence of endotoxin rather than endotoxins exerting some specific effect on the host.
Host responses include: fever chills weakness aches shock* death *septic shock. |
|
|
Immunology is
|
the study of specific immunity and the body's immune system that effects (i.e., causes) this specific immunity
|
|
|
Specific immunity is
|
that aspect of your body's defenses against pathogens (and other foreign material) that acts against specific molecules, usually requiring that your immune system "learn" the properties of specific molecules over a number of days or weeks before mounting an effective response against the foreign material
|
|
|
Specific immunity includes ______immunity and ___________immunity
|
humoral ; cell-mediated
|
|
|
specific immunity:
passive immunity occurs... |
when antibodies are produced by one individual and then acquired by another
ex- antibodies in colostrum *passive immunity is functional immediately upon reception |
|
|
specific immunity:
Active immunity occurs... |
when an individual's own immune system is induced to produce a specific immune response against an antigen/pathogen
*can last as long as the immune system cells, that mediate this immunity, survive within an individual; this can be for weeks, months, or years |
|
|
specific immunity is
|
that it is a means by which a body defends itself against the presence of specific antigens associated with, for example, pathogens
|
|
|
Antigens are the protein or polysaccharide components of pathogens
(c) (c) The reason that specific immunity is specific to specific pathogens (and their molecules) is because these molecules (antigens) are somewhat unique going from pathogen to pathogen (e.g., proteins with different amino acid sequences and therefore different structures, or polysaccharides made up of different sugars in different orders) |
the protein or polysaccharide components of pathogens
*The reason that specific immunity is specific to specific pathogens (and their molecules) is because these molecules (antigens) are somewhat unique going from pathogen to pathogen (e.g., proteins with different amino acid sequences and therefore different structures, or polysaccharides made up of different sugars in different orders) |
|
|
Nonspecific immunity includes
|
those defenses against pathogens, etc., that are not specific to each pathogen including such things as physical barriers, chemical barriers, some cellular defenses, inflammation, fever, and molecular defenses
|
|
|
specific immunity:
Naturally acquired immunity... |
is that immunity acquired upon exposure to a specific pathogen particularly in the course of an infection/disease
|
|
|
specific immunity:
Artificially acquired immunity... |
specifically refers to vaccination
|

